Abstract
Objective Patient-clinician communication has been associated with increased patient satisfaction, trust in the clinician, adherence to prescribed therapy, and various health outcomes. The impact of health information technology (HIT) on the clinical encounter in general and patient-clinician communication in particular is a growing concern. The purpose of this study was to review the current literature on HIT use during the clinical encounter to update best practices and inform the continuous development of HIT policies and educational interventions.
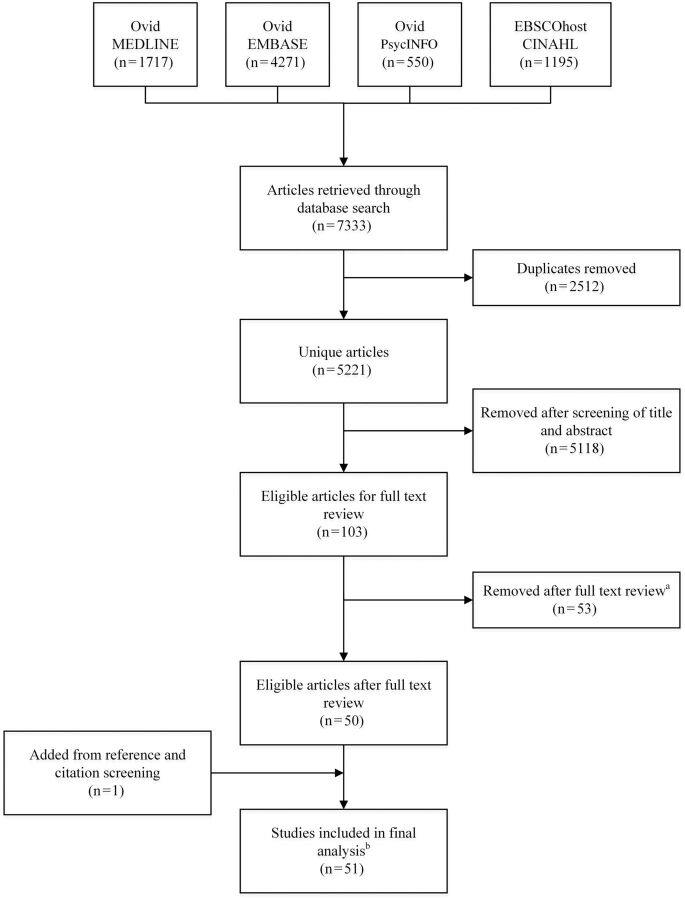
Methods We conducted a literature search of four databases. After removing duplicates, reviewing titles and abstracts, performing a full-text review, and snowballing from references and citations, 51 articles were included in the analysis. We employed a qualitative thematic analysis to compare and contrast the findings across studies.
Results Our analysis revealed that the use of HIT affects consultations in complex ways, impacting eye contact and gaze, information sharing, building relationships, and pauses in the conversation. Whether these impacts are positive or negative largely depends on the combination of consultation room layout, patient and clinician styles of interaction with HIT as well as each other, and the strategies and techniques employed by clinicians to integrate HIT into consultations.
Discussion The in-depth insights into the impact of HIT on the clinical encounter, especially the strategies and techniques employed by clinicians to adapt to using HIT in consultations, can inform policies, educational interventions, and research.
Conclusion In contrast to the common negative views of HIT, it affects the clinical encounter in multiple ways. By applying identified strategies and best practices, HIT can support patient-clinician interactions rather than interfering with them.
Keywords: professional-patient relations, health information technology, patient-clinician communication, electronic health record, templates
INTRODUCTION
Patient-centered care (PCC) has been widely acknowledged as an important component of health system quality.1 This concept emerged from the works of Balint in the 1960s, which contrasted PCC with the traditional model of “illness-centered care,”2,3 and from Engel’s Biopsychosocial Model, which places suffering, disease, and illness in the broad context of biological, psychological, and social dimensions.4 One of the most significant components of PCC is patient-clinician communication,5 which is considered one of the core competencies of medicine.6 Positive communication behaviors have been associated with patient satisfaction, trust, understanding, utilization of health system resources, and adherence to prescribed therapies.7–10 Although its impact is often indirect,8 there is evidence that good communication can positively affect various health outcomes, such as physical and emotional health status, performance of daily life activities, severity of symptoms, disease states, and clinical markers.9,11,12
With the increasingly ubiquitous use of health information technology (HIT), its impact on patient-clinician communication has become a common concern.13–15 In 2009, we published a literature review on the impact of electronic medical records (EMRs) on patient-clinician communication during the clinical encounter,16 identifying several themes including the positive and negative impacts of using HIT on patient-clinician communication, clinician styles of interaction with the computer and the patient, and factors that affect communication in computerized healthcare settings.
Since the publication of that review, several changes in the HIT landscape have occurred that warrant revisiting the topic. First, adoption rates for HIT have increased substantially, especially in North America. More than 75% of non-federal US hospitals and 80% of clinicians in Canada now use electronic health records (EHRs) and other health information systems17,18 – and, in other developed countries, these rates are even higher.19 Clinicians in many countries now have years of experience using HIT in the clinical encounter. Second, our previous literature review focused only on the use of EMRs by clinicians in outpatient settings and clinician offices. However, HIT is increasingly being used at the bedside in acute care settings as well as in primary care, outpatient clinics, and patient homes, and by healthcare professionals other than clinicians. Much of this use is enabled by technological developments, especially of mobile devices such as smartphones and tablets, and there is a growing body of literature that links these hardware, as well as clinical applications other than EMRs, and patient-clinician communication.32 Finally, specific tools to assess patient-clinician-computer communication are now available,20,21 and educational programs and modules are increasingly added to curricula to teach healthcare personnel effective communication skills.20,22
Thus, the purpose of this article is to update our previous review16 by analyzing recent literature on various HIT applications and hardware and patient-clinician communication. Specifically, it expands on previous work in that: 1) we included other clinicians in the literature search strategy and analysis, not just clinicians; 2) we have broadened the scope of the literature search from studies specifically on EMRs/EHRs to those on HIT in general; and 3) we specifically searched for and included studies that used platforms other than laptop or desktop computers (primarily smartphones and tablets). Our goal is to update best practices and inform the continuous development of policies, educational tools, and interventions to better support patient-clinician interactions in computerized healthcare settings.
METHODS
We first conducted a scoping review of the literature. Consistent with the approach suggested by Arksey and O’Malley,23 and unlike systematic reviews, we included a wide variety of research designs and did not assess the quality of the studies included in the literature review, in an attempt to cover the breadth of literature on HIT use during clinical encounters. We followed the process for scoping reviews outlined by Arksey and O’Malley,23 which includes four stages: 1) identifying relevant studies; 2) study selection; 3) charting the data; and 4) collating, summarizing, and reporting the findings.
Identifying Relevant Studies
To identify relevant studies, we searched for journal articles and papers in conference proceedings, published from 2007–2014 (inclusive), in four databases: MEDLINE, EMBASE, PsycINFO, and the Cumulative Index to Nursing and Allied Health Literature (CINAHL). For this purpose, we developed a comprehensive search strategy that included a combination of index terms and free text words (Supplementary Data). We included specific search terms to retrieve studies involving clinicians other than physicians and studies involving platforms other than laptops or desktop computers – especially smartphones and tablets.
The purpose of this literature search was to capture as many relevant studies as possible. Therefore, we designed the search strategy for high recall (sensitivity), while compromising on precision (the equivalent of positive predictive value in information retrieval), because there is often a trade-off between the two.24,25 To assess the recall of the search strategy, we first used it to search for articles published from 1997–2007, which is the period covered in our previous literature review. All of the articles included in the previous review were retrieved by the search strategy, except for one that had originally been retrieved from the references of other articles in the literature review and not from a database search. The authors are well-versed in the topic, so we also compared the search results for the period of 2007–2014 to our personal libraries. All of the articles we were familiar with were retrieved by the database search. Thus, we concluded that the search strategy had good recall.
A total of 7731 articles were retrieved: 1717 from MEDLINE, 4271 from EMBASE, 550 from PsycINFO, and 1195 from CINAHL. Upon pooling all of the articles together, 2512 duplicates were removed using EndNote X5 software, for a total of 5221 unique articles (Figure 1).
Figure 1:
PRISMA flow diagram of the article screening process. (a) Reasons for exclusion: 1) The study assessed clinician interaction with the computer alone – 12 articles; 2) The study assessed clinician interaction with the patient alone – 14 articles; 3) The study assessed patient interaction with the computer alone – 9 articles; and 4) Other (eg, not an empirical study, an implementation study that did not involve any communication aspect; use of the computer for communication with patients outside of the clinical encounter) – 18 articles. (b) Qualitative studies – 24, Quantitative studies – 24, Mixed methods – 3.
Study Selection
The titles and abstracts of the articles retrieved in the literature search were manually screened. Inclusion criteria for the final analysis were articles published in English and empirical investigations (quantitative or qualitative) of HIT use in face-to-face patient-clinician encounters. In an attempt to be as inclusive as possible, studies were included even if only a small component of the overall study was related to communication (eg, included questions related to communication on surveys administered to the study population). Studies related to virtual encounters (eg, telehealth), virtual communication (eg, e-mail), and purely methodological or viewpoint articles were excluded. This led to a total of 103 articles eligible for full text review, after which 50 papers met the criteria for final analysis. The titles of the references of these 50 articles were reviewed, upon which 1 article was added to the final analysis. Collectively, 51 articles were analyzed (Figure 1).
Charting the Data
Charting involves the systematic collection and recording of both “general information about the study and specific information relating to, for instance, the study population, the type of intervention, outcome measures employed and the study design.”23 For this purpose, we used six categories from the faceted classification system proposed by the International Medical Informatics Association Primary Care Informatics Work Group (IMIA PCI WG), for reporting observational studies on the use of technology during patient-clinician consultations.26 We first pilot tested the applicability of the framework by using it for charting and characterizing a convenience selection of 10 papers. We concluded that, although it was not designed for this purpose, with some modifications, the faceted classification system would provide a useful framework for charting the data, and then used it to summarize and characterize all 51 studies.
Collating, Summarizing, and Reporting the Findings
We adopted a thematic analysis approach to collating and summarizing the findings using the following process to identify recurrent and unique themes. First, one researcher (A.S.) read all the articles, annotated them, and identified broad topic categories (Supplementary Data). As additional articles were read, they were mapped to previously identified categories, based on the topics discussed in them, and more categories were added as new topics emerged. Topic categories are not mutually exclusive, and each article could be mapped to multiple categories, based on its contents. Next, the same researcher re-read all of the articles listed under each topic category, reviewed the annotations from the previous round, and compared and contrasted the various studies’ findings to identify recurrent themes, discrepancies, and unique findings. To establish trustworthiness, a second researcher (S.R.) independently performed this phase of the analysis for the articles listed in two categories. We then compared our analyses and discussed disagreements between them, in order to reach a consensus.
RESULTS
The complete characterization of the 51 studies we identified according to the modified IMIA PCI WG framework is presented in Supplementary Data. Of the 51 studies, 24 were qualitative, and used approaches such as linguistic analysis, grounded theory, cognitive task analysis, hermeneutics, dramaturgy, and thematic analysis. Twenty-four studies were quantitative, of which seven articles involved only cross-sectional or pre-/post-implementation surveys of patients or healthcare providers. Others employed quantitative communication assessment tools, such as the Roter Interaction Analysis System,27 or used time measurements of various behaviors – most commonly eye gaze. Finally, three studies used mixed (quantitative and qualitative) methods. Data collection methods most commonly involved video observation (25 studies) and surveys (13 studies). Other data collection methods included interviews, shadowing, and direct observations. The majority of the studies (37) were conducted in primary care settings.
A number of themes emerged from the analysis – some of which have been described in previous literature reviews and are reinforced and elaborated on here, and some of which are new. These topics are described in detail below.
Previously Identified Themes
Patient Attitudes Toward Clinicians’ Use of HIT
Sixteen studies looked at patients’ attitudes toward the use of computers in the clinical encounter, including for various aspects of communication (Table 1). Most patients reported having positive attitudes (10 studies), mixed attitudes, or no change in attitude about technology’s impact on patient-clinician communication (4 studies). One study28 found that, generally, patient satisfaction with their clinical experiences before and after EHR implementation were similar; however, scores for survey items related to patient-clinician communication significantly declined after EHR implementation. Another study, conducted in Kuwait,29 reported more negative attitudes with 50% of patients who agreed or strongly agreed that with the computer, physicians focused on the screen rather than the patient.
Table 1:
Patient Attitudes Toward the Use of Computers During Clinical Encounters and Its Impact on Communication
| Study | Details |
|---|---|
| Positive attitude | |
| Barker and Court30 | Patients perceived note typing as practical, time-saving, accurate, and comprehensive. They felt that “clinicians listened well” and noted positive clinician communication skills. |
| Baysari et al.31 | Most patients felt engaged or very engaged when clinicians used an iPad on ward rounds. |
| Freeman et al.32 | Patients reported that EMR use did not interfere with the patient-clinician relationship, did not affect visit time, and improved office efficiency and access to information. |
| Kushnir et al.33 | Patients reported having generally positive attitudes toward computer use during the clinical encounter; there was no significant difference in these attitudes between Jewish and Bedouin populations in Israel. |
| Lelievre and Schultz34 | Patient attitudes toward computer use were mostly positive. Most thought that it had a positive or very positive impact on their overall satisfaction with the visit (57%), their ability to voice concerns to the clinician (54%), the ability of the clinician to explain conditions to them (57.2%), and the ability of the doctor to write prescriptions (53.7%) and to access information in the record (56%). 61.1% of patients thought the computer had no effect on the doctor’s level of distraction. |
| Montague and Asan35 | High scores for patient satisfaction with clinicians’ EHR use (4.43–4.67 on a 5-point scale, depending on clinician style of interacting with the computer and with patients). |
| Piper and Hollan36 | Elderly patients thought that a large horizontal touch screen (surface computer) would facilitate information sharing, their ability to review the record for accuracy, and improve their understanding of medical information. |
| Rosen et al.37 | Greater parent satisfaction with the EHR than with paper records in a pediatric rheumatology clinic, including higher quality of care, better communication, and better understanding of test results. The authors noted that, “Satisfaction with communication [was] significantly correlated with reporting better understanding of medical tests and improved quality of care.” |
| Shield et al.38 | After full EHR implementation, patient reactions to it were mostly positive (including regarding communication); some patients expressed concerns about privacy. |
| Strayer et al.39 | Patients reported having positive attitudes toward using tablet computers in the consultation; most did not think it made the encounter with the clinician less personal. Older age and higher education level were associated with dislike of using tablets in patient-clinician consultations. |
| Mix of positive and negative attitudes/no effect on attitude | |
| Chen et al.40 | Patients expressed both positive and negative views on the impact of COWs on communication. These views were affected by whether they could see the screen or not. |
| McCord et al.41 | Generally, PDA use had no effect or only a small positive effect on patients’ perceptions of various aspects of patient-centeredness. Patient-clinician communication was rated significantly higher when the clinician explained their use of the PDA. |
| Stewart et al.42 | No significant difference in patient satisfaction with patient-psychiatrist relationship before and after EHR implementation. |
| Ratanawongsa et al.43 | Patients had mostly positive attitudes toward clinicians’ use of the EHR; however, 20% felt that the provider listened less because of the EHR. Non-English speakers and Asians were more likely to report that the EHR helped clinicians understand their health problems and remember their concerns, respectively. |
| Negative perceptions | |
| Al-Jafar29 | 50% of patients agreed or strongly agreed that clinicians focused on the screen rather than the patient. |
| De Leon et al.28 | Scores for survey items related to communication (“doctor listened to you,” “doctor gave clear instructions,” and “enough time with doctor”) significantly declined from pre- to post-implementation of an EHR. |
COW, computer on wheels; EHR, electronic health record; EMR, electronic medical record; PDA, personal digital assistant.
Impact of HIT on Visit Time and the Time Spent on Various Tasks
Ten studies reported that HIT use during patient visits had various impacts on time (the length of the visit as well as the time spent on various tasks). As presented in Table 2, clinicians perceive that the use of computers increases visit time,44–46 and some observational studies support this notion, especially if decision aids are being used or if information is documented after the patient’s visit.47–49 Other studies describe HIT’s impact on the relative time spent on various tasks. Although there is a wide range of reported values for time spent using HIT during a consultation, studies consistently report that clinicians spend at least 20% of their time with the patient looking at a computer screen or engaging with the computer in some way (Table 2). There is also some evidence that, with a computer in the consultation room, clinicians spend less time looking at the patient than they do when using paper records.50
Table 2:
Time-Related Aspects of Computer Use During Clinical Encounters
| Study | Time-related aspects of computer use |
|---|---|
| Adams et al.44 | Nurses reported that consultations were longer when e-health technology was being used during consultations. |
| Al Alawi et al.45 | Clinicians believed that EMR use takes more time and “identified the long time required to do the documentation in the system as a factor that affects their practice and communication.” |
| Anderson46 | Home-care occupational therapists believed that computer-based documentation increased patient visit length. |
| Asan and Montague51 | Average screen gaze and average typing time were 26.5–37.58% and 7.4–12.18% of the total patient visit time, respectively, and depended on the clinician’s information-sharing style. |
| Asan and Montague50 | Time the clinician spent looking at a computer screen accounted for 35.2% of the total patient visit time – significantly higher than time spent looking at paper records (22.1%). |
| Time the clinician spent looking at or interacting with patients during the consultation was 45.6%, which is significantly less than when the clinician was using paper records (52.6%). | |
| Dowell et al.52 | Total computer work accounted for at least 20% of the total visit time; average split attention time and time totally focused on computer were 27% and 12%, respectively. |
| Fiks et al.49 | Total computer work accounted for 27% of the total patient visit time. |
| Post-visit documentation was associated with patient visits that were 11% longer. | |
| Johnson et al.47 | Use of a mouse or keyboard accounted for, on average, 27% of the total patient visit time. |
| Visits were ∼5 min longer when the clinician used a computer during the consultation (compared to paper records). | |
| Kaner et al.48 | Consultations in which the clinician used computer-based decision aids took longer (an average of 31 and 44 min, depending on the tool) than a paper-based guideline (an average of 21 min). |
| Kumarapeli and de Lusignan53 | 61% of patient visit time involved direct patient-clinician interaction (including physical examination), 25% involved computer use with no patient interaction, and 14% involved interaction with both the patient and the computer. |
| Montague and Asan54 | Time the clinician spent looking at the computer screen accounted for, on average, 30.7% of the total patient visit time. |
| Time the clinician spent interacting with patients accounted for, on average, 46.5% of the total patient visit time. | |
| Shachak et al.55 | Time the clinician spent looking at the computer screen ranged from 25–55% of the total patient visit time. |
| Shield et al.38 | Time the clinician spent on computer/looking or writing in chart increased significantly after EMR implementation – on average, from 2.8–4.4 min (average consultation length was 25.6 and 23.8 min, respectively). |
| Street et al.56 | Time the clinician spent looking at the computer screen accounted for, on average, 39.4% of the total patient visit time. |
E-Health, electronic health; EMR, electronic medical record.
Effect of HIT on the Clinical Encounter
As we found in our previous review,16 studies continue to report a diverse range of impacts of HIT on patient-clinician communication, both negative and positive. Negative impacts include:
Difficulty dividing attention between the patient and the screen,55,57,58 distractions, interference with eye contact, dialogue, and rapport or patient-centeredness;31,35,40,44,45,50,56–58
Ignoring or deferring patient concerns,59 typing or looking at the computer screen while patients speak, sometimes even when patients bring up psychological and emotional issues;40
Disconjugate gaze, in which the patient continues to look at the computer screen while the clinician turns to the patient; the computer may be a distraction for some patients;54,60
Less information sharing than when paper records are used,57 negative relationship between computer use and the amount of information given by patients;61
Negative impact on patients’ ability to ask questions;58 and
Specifically for mobile devices, patients may be skeptical if personal digital assistants (PDAs) look too similar to the clinician’s personal device.57
Other studies have reported that HIT has no effect on communication, eg, there was no difference between paper and computerized decision aids in the proportion of technical and psychosocial conversation,48 no difference in provider/patient talk ratio during the consultation, and no difference in nonverbal communication.47
Positive impacts of HIT on patient-provider communication include:
More information-giving48 and a greater proportion of open-ended questions asked;47
More use of partnership strategies between patient and clinician, social and positive talk, and patient-centered interaction style;47
Patients can bring the computer into the conversation, thereby changing the nature of the consultation and power dynamics with the clinician.60
In particular, screen sharing may facilitate communication and patient education. Some clinicians used the computer to share information and explain results, eg, labs and imaging.40,51 In other cases, screen sharing was used to verify the accuracy of the patient’s information, eg, by collaboratively reviewing the patient’s list of medications40 or by allowing the patient to immediately correct and add to the information being documented during the consultation.55 In some cases, risk calculators and other decision aids, or information from the Internet, were used to explain conditions, disease processes, and potential interventions to patients.45,55,62
Finally, impacts of HIT on the patient-clinician encounter are not limited to communication. Additional impacts include reduced cognitive load associated with clinical tasks, due to the comprehensiveness, organization, and readability of information in HIT systems;55,57 the use of templates as reminders or checklists;55,59 and improved patient safety and care,45,55 including the ability of the computer to prevent errors and allow for making corrections.57 On the negative side, the computer may induce new types of errors, such as wrongly selected items from lists and documenting information in the wrong patient’s file.55 One study reported that use of an EHR increased patients’ waiting times.45
Physical Setting
A number of studies discussed the physical setting in which the patient, clinician, and computer interact. Most studies described family clinician or outpatient office settings. Office configurations range from inclusive layouts that allow patients to view the computer screen easily, to exclusive settings in which the computer screen is hidden from the patient’s view. In addition, there are semi-inclusive configurations in which the patient may be able to view the computer screen by changing position (patient-controlled) or if the clinician turns the computer monitor toward the patient (clinician-controlled).53 Various studies reported different prevalences of these configurations. Kumarapeli and de Lusignan,53 in the United Kingdom, reported that 62.5% of settings employed the clinician-controlled, semi-inclusive configuration; 25% employed the patient-controlled, semi-inclusive configuration; and only 1 in 16 (6.3%) employed the exclusive configuration. In Australia, Pearce et al.63 also reported that “more commonly [than the exclusive set-up], although the screen was facing the doctor, it could be partially viewed by the patient.” In contrast, Shachak et al.,55 in Israel, found that 22 of 25 clinician offices (88%) examined for the study used an exclusive configuration, and only 3 (12%) used an inclusive configuration. Different behavioral patterns were observed in different settings. In exclusive or clinician-controlled settings, clinicians did not actively share the computer screen with patients,53 while inclusive settings promoted more sharing of information from the patient’s medical record and from the Internet.63,64
A number of studies involved computers on wheels (COWs) or mobile technology (specifically, PDAs) in outpatient40 or simulated inpatient settings.57,58 Similar to desktop computers, COWs were found to pose a physical barrier that could interfere with eye contact. The physical size of the cart, as well as the need, in some settings, to plug the computer into a power outlet, made it hard to maneuver. Thus, COWs maintained a relatively fixed position in both outpatient examination rooms and simulated inpatient wards.40,58 In the simulated inpatient settings, clinicians had to turn away from the patient to work on the computer, which resulted in a loss of eye contact with the patient.58 In the outpatient settings, clinicians alternated between exclusive, inclusive, and patient-controlled views of the monitor by moving the cart, depending on the phase of the encounter.40
Compared to desktop computers or COWs, PDAs were found to cause no physical barrier to eye contact. Clinicians were able to position themselves so that they could easily re-establish eye contact with the patient after using the device. Because of the small size of the PDA, it could be easily put in a white coat’s pocket and carried around.57,58 However, PDA use resulted in a different type of barrier, ie, low visibility of actions. From the patients’ perspective, all actions performed on the device appear similar.57,58
Clinician Styles
Five studies classified clinician styles of using HIT during clinical encounters (Table 3). Although various attributes have been used for this classification, many similarities between clinician styles of interacting with HIT and patients can be drawn. For example, Pearce et al.’s65 unipolar and bipolar styles are equivalent to Rhodes et al.’s66 bureaucratic and participative/patient-centered styles, respectively. Montague and Asan’s35 technology-centered and human-centered styles share many similarities with Chan et al.’s67 continuous and end users, respectively. Similarities can also be drawn between clinician styles of interacting with HIT and patients based on body orientation,65 screen gaze,66 or amount of typing35 and those based on information-sharing behaviors,51 although the latter may be a result of a combination of clinician styles, the physical set-up of the consultation room, and patient styles of interacting with HIT and the clinician (see next section).
Table 3:
Clinician Styles of Interacting with HIT and the patient
| Study | Classification basis | Styles identified | Style characteristics |
|---|---|---|---|
| Pearce et al.65 | Lower body orientation | Unipolar | Maintains fixed lower body orientation toward the computer; often asks questions driven by the computer; enters data during the consultation; lower and upper body orientation often in different directions (eg, turning gaze toward the patient while maintaining lower body orientation toward the screen). |
| Bipolar | Alternates lower body orientation between the patient and the computer; indicates switching attention between the two by changing body orientation. | ||
| Montague and Asan35 | Amount of typing | Technology-centered | Extensive typing (>15% of visit time); types continuously throughout the patient-clinician encounter; spends the largest amount of time looking at the computer screen; often talks to the patient while typing and uses affirmative speech and nodding to indicate that the patient has their attention while they are working on the computer. |
| Optimizing | Intermediate amount of typing (5-15% of visit time); employs brief typing periods in which they focus on the computer; stops typing and shifts gaze to the patient when speaking with the patient; maintains posture that allows for facing the patient most of the time. | ||
| Human-centered | Least amount of typing (<5% of the visit time) and screen gaze time; characterized by slow “hunt and peck” typing style; often uses aids such as paper or dictation for data entry; “higher amounts of positive verbal and nonverbal communication style.” | ||
| Asan and Montague51 | Screen sharing | Active information-sharing | Inclusive office set-up (see ‘Physical Setting’ above); turns the screen toward the patient; verbally invites patients to look at the monitor; uses the computer to explain results and retrieve and share information with the patient; high percentage of conjugate gaze at the computer (see “Patient Styles” section, below). |
| Passive information-sharing | Semi-inclusive, patient-controlled setting; high amount of clinician typing and looking at the computer; shifts gaze back and forth between the computer and patient; patients tend to look at the computer while clinicians enter data. | ||
| Technology withdrawal | No screen sharing; minimal computer use, with clinician typing mostly toward the end of the visit; clinicians mostly focus on the patient, with brief gazes at the computer. | ||
| Chan et al.67 | Observation (criteria for classification are not specified) | Continuous users | Consistent use of the computer throughout the encounter for reviewing and entering data; often engages patients with the computer. |
| Minimal users | Minimal use of the computer during the patient visit (mostly for printing prescriptions). | ||
| End users | Leaves most of the computer usage for the end of the patient visit; types in notes before prescribing. | ||
| Rhodes et al.66 | Screen gaze | Bureaucratic | Body orientation is toward computer, and the focus of attention is mostly on the screen; uses changes in gaze to indicate the relative importance of topics to the patient. |
| Participative/patient-centered | Body orientation is mostly toward the patient; maintains eye contact most of the time; shifts in attention are indicated by changing lower body orientation. |
Emergent Themes
Patient Styles
Although clinician styles of interacting with HIT and patients have been reported on in previous reviews,16,68 a new theme that emerged from our literature review is that of patient styles of interacting with HIT and their clinicians. A number of studies suggest that patients also exhibit various behavioral styles in relation to the computer during consultations.
Pearce et al.60,65 classifies patient styles of interacting with HIT and the clinician as either dyadic or triadic. Dyadic patients focus mainly on the clinician, whereas triadic patients tend to deal with the computer as part of the consultation. Dyadic and triadic patients differ in lower body orientation (toward the clinician or computer, respectively) and behaviors. Pearce et al. reported that dyadic patients in their study tended to ignore the computer and wait passively for the clinician to complete working on the computer. They often used “screen ignoring” behaviors, such as deliberately turning away from the computer to draw the clinician’s attention back to them. In contrast, triadic patients tended to look more at the computer screen and actively involve the computer in the consultation by pointing at it, leaning over, or moving their seat so that they could see the computer screen.60
The combination of clinician and patient styles and behaviors in relation to HIT use could result in a conjugate gaze, when the patient and clinician’s gaze match, or in a disconjugate gaze, when they look at different objects. For triadic patients, a period of disconjugate gaze, in which the patient continued to watch the screen while the clinician had turned his or her attention to the patient, often followed periods of mutual screen-watching.60 In EHR settings, a conjugate gaze at the computer screen happened during an average of 10.3% of the visit time (excluding physical examination).50 This number was higher (13.84%) for clinicians who actively shared computer-based information with patients than for those who passively allowed patients to watch the computer screen (9.16%) and those who preferred not to use the EHR with the patient at all (0.7%). Clinician gaze at the screen was significantly associated with the patient’s gaze at the screen.51 Further analysis showed that clinician-initiated gaze at the screen, the patient, or other objects were significantly followed by the patients, resulting in a conjugate gaze. In contrast, patient-initiated gaze patterns were not always followed by clinicians. The authors identified significant patterns of the patient’s gaze at the clinician followed by the clinician’s gaze at the monitor and of the patient’s gaze at the screen followed by the clinician’s gaze at the patient, which they suggest “may indicate a failed opportunity to use the EHR as a shared artifact.”54
The Role of the Computer in Shaping the Clinical Encounter
Although it has previously been argued that the presence of a computer in the consultation room changes the dyadic patient-clinician interaction into a triadic interaction,69 it is now clearer than ever that the computer can play an important role in shaping the patient-clinician encounter. The computer exhibits agency that can affect this interaction in either passive or active ways.62,70,71
Passive influence occurs when the clinician searches the patient’s medical record for information (eg, test results) or notices missing information in the patient’s medical record (eg, demographics, smoking status) and tries to fill in these data by querying the patient.70 This often results in both individuals looking at the computer screen.65,70Active influence is mostly in the form of prompts, such as reminders and alerts, that pop-up on the computer screen (eg, reminders to order screening tests for the patient, drug interaction alerts) or flags (eg, for abnormal test results, medication renewals, or management of existing conditions). Such prompts can distract from the patient as the clinician turns these prompts and flags off, or they can change the direction of the conversation when the clinician responds to the prompts/flags.65,70–72
Furthermore, the computer affects the way information is collected and documented during the patient-clinician encounter. As Pearce et al.70 noted, consultations shaped by the EHR “generated much more coded data, but at the expense of narrative information, and sometimes even of patient agenda.” Specifically, studies on using computerized templates during consultations suggest that templates promote a “bureaucratic” or “checklist” approach to consultations. Thus, the main task and the reason for the patient-clinician encounter become the completion of data fields in the template,59,66,73 with little room for discussion of self-management practices and complex interactions between various conditions and patient characteristics.59,73
Moreover, because templates profoundly change the way patient information is documented, they can potentially affect the clinician’s reasoning and decision making processes. Specifically, having separate templates for each chronic condition implies that complex multiple morbidities can be separated and clearly distinguished from each other. Templates focus on measurable items, thus reducing patients’ complex narratives and the complex interactions of their conditions and identities into checkboxes and quantifiable values. Finally, templates leave no room for ambiguity, eg, in diagnosis, which may result in patients being incorrectly identified as having a certain condition.59
HIT’s agency is often a manifestation of external policies.44,59,62,70,72 For example, Pearce et al.70 noted that flags related to pay-for-performance chronic disease management often drive consultations. Prompts may also reflect policies, such as drug prescription regulations, or government initiatives, such as health promotion.72 Swinglehurst et al.62 provide a different example, in which an alert that the patient is registered with the United Kingdom's government-initiated Quality and Outcomes Framework (QOF) for hypertension remained open throughout the consultation, indicating there are two QOF items that require attention. Nurses in another study also noted the QOF data entry requirements as a factor that affects patient-clinician consultations.44 Finally, computer templates reflect what institutions considered to be best practices and, as Swinglehurst et al.59 argue, “can change the very nature of what it means to ‘care.’”
Silent Time and Pauses in the Conversation
Silent time, or pauses in the conversations between patients and clinicians, is another emergent theme. Silences occurred regularly in patient-clinician encounters in computerized settings.52,56,66,74–77 Long pauses in patient-clinician interactions were often associated with computer use: in one study, 47.1% of silent time was associated with computer use.76 Other studies noted differences in the patterns of silent time in patient-clinician conversations held in paper-based settings versus computerized settings. Computer use was associated with a greater number of pauses in conversations and longer silences.75,77
Silences have both positive and negative impacts on communication. Although short pauses (<5 s) did not cause the topic of conversation to change,77 longer pauses often required participants to restate the topic they wished to discuss or resulted in the topic of conversation changing.52,66,74,77 On the positive side, pauses in the conversation may allow patients to bring up new topics that might have been missed otherwise,52,66,74 and they may be related to patients asking more questions.75 For the clinician, silent time may provide a necessary “time-out” to think.74,76 In some cases, mock computer use, when the clinician “would tap on the keyboard … or move the mouse around in silence with no computer output noted,” was used as a cue that such a “time-out” was needed.76 However, other researchers have reported that silences could deflect the conversation from the current topic of conversation77 and that silent time was significantly associated with lower patient-centered communication scores, less patient involvement, and greater clinician control of the conversation.56 Most pauses were initiated and terminated by the clinician, and therapeutic silence, initiated by the clinician and terminated by the patient, was rare (9.4% of all silences).76
How Clinicians Adapt to Using Computers During Consultations
Research suggests that clinicians adapt to using computers in consultations over time.38,78 Noordman et al.61 found that the portion of the consultation that the clinician spent using the computer decreased over time, which may be due to more effective integration of the EMR into the consultation or because the clinician began to use the computer more before and after the patient visit, rather than during. Most notably, clinicians adapted their practice and significantly reduced the portion of time spent on the computer during patient encounters that involved psychological components.60,67 Finally, many studies described strategies and techniques employed by clinicians to maintain rapport with patients and minimize the negative impact of HIT on communication in computerized settings (Table 4).
Table 4:
Strategies and Techniques to Maintain Patient-Centeredness in Computerized Clinical Settings
| Strategy/technique | References |
|---|---|
| Maintaining body orientation toward the patient (especially lower body); touching the patient while working on the computer. | Chen et al.,40 Swinglehurst et al.,59 Rhodes et al.,66 Doyle et al.78 |
| Talking while working on the computer to maintain engagement with the patient and break long silences. | Dowell et al.,52 Newman et al.77 |
| Explaining computer use (eg, the purpose for using it); verbalizing actions on the computer (eg, describing what they are looking for); reading out loud while typing. | Shield et al.,38 McCord et al.,41 Al Alawi et al.,45 Anderson,46 Dowell et al.,52 Shachak et al.,55 Alsos et al.,57,58 Swinglehurst et al.59 |
| Sharing the screen with the patient; involving the patient in building their chart. | Shield et al.,38 Chen et al.,40 McCord et al.,41 Adams et al.,44 Al Alawi et al.,45 Anderson,46 Asan and Montague,51 Kumarapeli and de Lusignan,53 Shachak et al.,55 Swinglehurst et al.,59 Pearce et al.70 |
| Separating computer use from communication with the patient, especially when building rapport or discussing treatment options; verbalizing or using gestures to indicate switches in attention between the patient and the computer. | McCord et al.,41 Adams et al.,44 Anderson,46 Fiks et al.,49 Shachak et al.55 |
| Using gaps in the interaction with the patient for computer work (eg, when the patient is dressing after a physical examination). | Asan and Montague,51 Dowell et al.,52 Shachak et al.55 |
| Using the mouse with the non-dominant hand, to minimize disengaging body language. | Pearce et al.63 |
| Starting the visit by asking about the patient’s concerns and building rapport. | Anderson,46 Swinglehurst et al.59 |
| Reviewing the patient’s medical record before calling the patient in. | Kumarapeli and de Lusignan,53 Swinglehurst et al.59 |
| Documenting the patient encounter in the patient’s medical record after the visit. | Adams et al.,44 Al Alawi et al.,45 Anderson,46 Fiks et al.,49 Dowell et al.52 |
DISCUSSION
The study of patient-clinician-computer interaction has matured and is now well established. This article provides a detailed review of the current research in the field. A recent systematic review on the topic68 reported on several themes, including the impact of EHRs on information exchange between patients and clinicians; maintaining positive relationships with, activating, and partnering with patients; and the EHR as an amplifier of existing communication behaviors. Most of these themes had been also identified in our previous review,16 and the current study reiterates and expands on them. Due to low recall and stringent inclusion criteria, the literature review by Kazmi only included 13 articles published between 1994 and 2013 and missed some key studies on this topic.68 In contrast, our search strategy and more permissive inclusion criteria enabled us to include 51 articles, published from 2007 to 2014, in our thematic analysis. As a result, we were able to identify several new themes within the research on patient-clinician-computer interaction, which have not been reported in previous review articles, including patient styles of interacting with HIT and clinicians, silent time and pauses during patient-clinician communication, and how clinicians adapt to using a computer during clinical encounters.
A fast-growing trend in the United States is the use of scribes to enter patient data into EHRs.80 Clinicians who use scribes describe it as “liberating” and note that it allows them to devote attention to the patient and to clinical tasks.80 However, our findings suggest that, in contrast to this view as well as common criticism of HIT,13,14 the impact of HIT on the clinical encounter is complex and not all negative. Although HIT obviously does have some negative impacts on the clinical encounter, such as requiring clinicians to divide their attention between the patient and computer, difficulty maintaining eye contact, and other aspects of patient-centeredness, it also has some positive impacts. These positive impacts include increased information sharing between patients and clinicians and increased opportunities to engage with and empower patients by sharing computer-based information and resources with them. Long pauses in patient-clinician conversations caused by using HIT may provide opportunities for patients to ask questions, provide more information to the clinician, or raise additional concerns.
Whether these potential positive impacts are realized or not depends, to a large extent, on clinicians’ styles of interacting with HIT and patients as well as how they adapt to using HIT in the consultation. Rather than delegating tasks, we believe that clinicians should embrace the use of HIT with the patient, learn the verbal and nonverbal cues that indicate patient styles of communicating and adapt their practice accordingly, eg, by sharing the computer screen with the patient.81,82 By adopting some of the strategies and techniques described above, clinicians can leverage HIT to support their interactions with patients. To help with this, educators could build on this review to develop interventions to educate clinicians about the challenges and trade-offs of as well as best practices for integrating computer use into clinical encounters. There are currently some promising initiatives in this direction,20,22,83–85 but more work is needed.
Our findings demonstrate the active role that computers play in patient-clinician consultations. As described above, computers exhibit agency that can affect the patient-clinician interaction as well as the course of the consultation. Our findings support earlier research86 that showed that changes to the way patient information is gathered and documented may affect the completeness of the patient’s medical record – especially as regards the patient’s narrative – and, thereby, the clinician’s reasoning and decision making. Because the HIT agency often reflects high-level policies, both clinicians and policy makers need to be aware of the impacts that HIT policies have on the micro-level (ie, the clinical encounter) and take these impacts into consideration when developing HIT-related policies.
This literature review has several implications for research. First, a lack of consistent terminology continues to be an issue – eg, several studies have reported similar clinician styles of interacting with HIT and the patient, but different researchers use different terms to describe these styles. Likewise, different terms are often used to describe similar spatial layouts of consultation rooms. Our previously suggested terminology16 for clinician styles of interacting with HIT and patients is cumbersome, so we propose going back to the terminology suggested by Ventres87 of informational, managerial, and interpersonal styles. For other terms, we recommend that researchers refer to the consensus statement by IMIA PCI WG.26 Second, we noticed that many studies have not described the physical layout of the clinical setting. We believe that this information would be beneficial to understanding and interpreting research findings, especially in observational studies of computer use during the clinical encounter. Finally, most of the research we identified emerged from primary care and outpatient settings, in which desktop computers are used. There is a dearth of research on acute care settings, in which the patient-clinician-computer interaction may be very different. Despite widespread use by the general public, and growing adoption in clinical settings, studies on the use of mobile technology during patient-clinician consultations are few. More research is needed to explore the impacts of mobile devices on the clinical encounter.
Limitations
Variations in the study designs and the quality of the studies we identified in our literature review may affect these studies’ reported results. Because we conducted a scoping review, we have not selected any particular study design to focus on and have not appraised the quality of the studies we identified. We only included research articles that address the use of HIT in face-to-face patient-clinician interactions. However, technology is increasingly being used for virtual communication, ranging in media richness and synchronicity88,89 from videoconferencing to text messaging to e-mail. Reviewing the literature on this topic was beyond the scope of this article.
CONCLUSION
In contrast to the common negative view, this literature review suggests that HIT affects the clinical encounter in multiple ways, both positive and negative. By applying identified strategies and best practices, HIT can support patient-clinician interaction rather than interfere with it.
CONTRIBUTORS
N.H.C. conducted the database search; screening of titles, abstracts, and full text of articles for inclusion in the study; conducted the charting according to the IMIA PCI WG framework; participated in preparing the manuscript; and reviewed and approved the submitted manuscript. S.R. participated in the thematic analysis; critically revised the manuscript; and reviewed and approved the submitted manuscript. A.S. participated in the screening of titles, abstracts, and full text of articles for inclusion in the study; conducted the thematic analysis; drafted the manuscript; and reviewed and approved the submitted manuscript.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
COMPETING INTERESTS
None.
Supplementary Material
ACKNOWLEDGEMENTS
We greatly appreciate the help of Heather Cunningham in formulating the search strategy and performing the database search. We are also grateful to Mehreen Zaman for pilot testing the use of the IMIA PCI WG faceted classification system for charting the identified articles. Noah Crampton started this study as part of the medical informatics research elective at McGill University.
SUPPLEMENTARY MATERIAL
Supplementary Data is available online at http://jamia.oxfordjournals.org/.
REFERENCES
- 1. Institute of Medicine (US), Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington, D.C.: National Academy Press; 2001. [PubMed] [Google Scholar]
- 2. Bardes CL. Defining “Patient-Centered Medicine”. N Engl J Med. 2012;366(9):782–783. [DOI] [PubMed] [Google Scholar]
- 3. Balint E. The possibilities of patient-centered medicine. J R Coll Gen Pract. 1969;17(82):269–276. [PMC free article] [PubMed] [Google Scholar]
- 4. Engel G. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–136. [DOI] [PubMed] [Google Scholar]
- 5. Epstein RM Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nasca TJ Philibert I Brigham T Flynn TC. The next GME accreditation system–rationale and benefits. N Engl J Med. 2012;366(11):1051–1056. [DOI] [PubMed] [Google Scholar]
- 7. Mead N Bower P. Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ Couns. 2002;48(1):51–61. [DOI] [PubMed] [Google Scholar]
- 8. Street RL Jr Makoul G Arora NK Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295–301. [DOI] [PubMed] [Google Scholar]
- 9. Beck RS Daughtridge R Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002;15(1):25–38. [PubMed] [Google Scholar]
- 10. Fawole OA Dy SM Wilson RF et al. A systematic review of communication quality improvement interventions for patients with advanced and serious illness. J Gen Intern Med. 2013;28(4):570–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 12. Fremont AM Cleary PD Hargraves JL Rowe RM Jacobson NB Ayanian JZ. Patient-centered processes of care and long-term outcomes of myocardial infarction. J Gen Intern Med. 2001;16(12):800–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Toll E. A piece of my mind. The cost of technology. JAMA. 2012;307(23):2497–2498. [DOI] [PubMed] [Google Scholar]
- 14. Feldman E. A piece of my mind. The day the computer tried to eat my alligator. JAMA. 2010;304(24):2679. [DOI] [PubMed] [Google Scholar]
- 15. Friedberg MW Chen PG Van Busum KR et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy: Rand Corporation; 2013. http://www.rand.org/pubs/research_reports/RR439.html. Accessed July 22, 2015. [PMC free article] [PubMed] [Google Scholar]
- 16. Shachak A Reis S. The impact of electronic medical records on patient-doctor communication during consultation: a narrative literature review. J Eval Clin Pract. 2009;15(4):641–649. [DOI] [PubMed] [Google Scholar]
- 17. Charles D King J Patel V Furukawa MF. Adoption of electronic health record systems among US non-federal acute care hospitals: 2008-2012: Office of the National Coordinator for Health Information Technology; 2013. https://www.healthit.gov/sites/default/files/oncdatabrief9final.pdf. Accessed July 22, 2015. [Google Scholar]
- 18. National physician survey. http://www.nationalphysiciansurvey.ca/ Accessed July 22, 2015.
- 19. Schoen C Osborn R Squires D et al. A survey of primary care doctors in ten countries shows progress in use of health information technology, less in other areas. Health Aff. 2012;31(12):2805–2816. [DOI] [PubMed] [Google Scholar]
- 20. Wald HS George P Reis SP Taylor JS. Electronic health record training in undergraduate medical education: bridging theory to practice with curricula for empowering patient- and relationship-centered care in the computerized setting. Acad Med. 2014;89(3):380–386. [DOI] [PubMed] [Google Scholar]
- 21. Assis-Hassid S Heart T Reychav I Pliskin J Reis S. Enhancing patient-doctor-computer communication in primary care: towards measurement construction. Isr J Health Policy Res. 2015;4(1):4–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Silverman H Ho YX Kaib S et al. A novel approach to supporting relationship-centered care through electronic health record ergonomic training in preclerkship medical education. Acad Med. 2014;89(9):1230–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Arksey H O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 24. Buckland M Gey F. The relationship between recall and precision. J Am Soc Inform Sci. 1994;45(1):12. [Google Scholar]
- 25. Hersh WR. Information Retrieval: a Health and Biomedical Perspective. 3rd ed New York, NY: Springer; 2009: 96–99. [Google Scholar]
- 26. de Lusignan S Pearce C Kumarapeli P et al. Reporting observational studies of the use of information technology in the clinical consultation. A position statement from the IMIA Primary Health Care Informatics Working Group (IMIA PCI WG). Yearb Medical Inform. 2011;6(1):39–47. [PubMed] [Google Scholar]
- 27. Roter D Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns. 2002;46(4):243–251. [DOI] [PubMed] [Google Scholar]
- 28. De Leon SF Silfen SL Wang JJ Kamara TS Wu WY Shih SC. Patient experiences at primary care practices using electronic health records. J Med Pract Manage. 2012;28(3):169–176. [PubMed] [Google Scholar]
- 29. Al-Jafar E. Exploring patient satisfaction before and after electronic health record (EHR) implementation: the Kuwait experience. Perspect Health Inf Manag. 2013; 10 (Spring):1c, Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3692323/. [PMC free article] [PubMed] [Google Scholar]
- 30. Barker F Court G. PC-based note taking in patient-centred diagnostic interviews: a thematic analysis of patient opinion elicited using a pilot survey instrument. Inform Prim Care. 2011;19(1):51–54. [DOI] [PubMed] [Google Scholar]
- 31. Baysari MT Adams K Lehnbom EC Westbrook JI Day RO. iPad use at the bedside: a tool for engaging patients in care processes during ward rounds? Intern Med J. 2014;44(10):986–990. [DOI] [PubMed] [Google Scholar]
- 32. Freeman MC Taylor AP Adelman JU. Electronic medical record system in a headache specialty practice: a patient satisfaction survey. Headache. 2009;49(2):212–215. [DOI] [PubMed] [Google Scholar]
- 33. Kushnir T Esterson A Bachner YG. Attitudes of Jewish and Bedouin responders toward family physicians' use of electronic medical records during the medical encounter. Patient Educ Couns. 2013;93(3):373–380. [DOI] [PubMed] [Google Scholar]
- 34. Lelievre S Schultz K. Does computer use in patient-physician encounters influence patient satisfaction? Can Fam Physician. 2010;56(1):e6–e12. [PMC free article] [PubMed] [Google Scholar]
- 35. Montague E Asan O. Considering social ergonomics: the effects of HIT on interpersonal relationships between patients and clinicians. Work. 2012;41 (Suppl 1):4479–4483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Piper AM Hollan JD. Supporting medical communication for older patients with a shared touch-screen computer. Int J Med Inform. 2013;82(11):e242–e250. [DOI] [PubMed] [Google Scholar]
- 37. Rosen P Spalding SJ Hannon MJ Boudreau RM Kwoh CK. Parent satisfaction with the electronic medical record in an academic pediatric rheumatology practice. J Med Internet Res. 2011;13(2):e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Shield RR Goldman RE Anthony DA Wang N Doyle RJ Borkan J. Gradual electronic health record implementation: new insights on physician and patient adaptation. Ann Fam Med. 2010;8(4):316–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Strayer SM Semler MW Kington ML Tanabe KO. Patient attitudes toward physician use of tablet computers in the exam room. Fam Med. 2010;42(9):643–647. [PubMed] [Google Scholar]
- 40. Chen Y Ngo V Harrison S Duong V. Unpacking exam-room computing: negotiating computer-use in patient-physician interactions. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. Vancouver, BC, Canada; Association for Computing Machinery, 2011: 3343-3352. [Google Scholar]
- 41. McCord G Pendleton BF Schrop SL Weiss L Stockton L Hamrich LM. Assessing the impact on patient-physician interaction when physicians use personal digital assistants: a Northeastern Ohio Network (NEON) study. J Am Board Fam Med. 2009;22(4):353–359. [DOI] [PubMed] [Google Scholar]
- 42. Stewart RF Kroth PJ Schuyler M Bailey R. Do electronic health records affect the patient-psychiatrist relationship? A before & after study of psychiatric outpatients. BMC Psychiatr. 2010;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ratanawongsa N Barton JL Schillinger D Yelin EH Hettema JE Lum PJ. Ethnically diverse patients' perceptions of clinician computer use in a safety-net clinic. J Health Care Poor Underserved. 2013;24(4):1542–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Adams A Adams R Thorogood M Buckingham C. Barriers to the use of e-health technology in nurse practitioner-patient consultations. Inform Prim Care. 2007;15(2):103–109. [DOI] [PubMed] [Google Scholar]
- 45. Al Alawi S Al Dhaheri A Al Baloushi D Al Dhaheri M Prinsloo EA. Physician user satisfaction with an electronic medical records system in primary healthcare centres in Al Ain: a qualitative study. BMJ Open. 2014;4(11):e005569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Anderson RE. The art of caring in the computer age: perceptions of home care occupational therapy practitioners. Home Commun Health Special Interest Section Quarterly. 2008;15(2):1–4. [PMC free article] [PubMed] [Google Scholar]
- 47. Johnson KB Serwint JR Fagan LA Thompson RE Wilson ME Roter D. Computer-based documentation: effects on parent-provider communication during pediatric health maintenance encounters. Pediatrics. 2008;122(3):590–598. [DOI] [PubMed] [Google Scholar]
- 48. Kaner E Heaven B Rapley T et al. Medical communication and technology: a video-based process study of the use of decision aids in primary care consultations. BMC Med Inform Decis Mak. 2007;7:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Fiks AG Alessandrini EA Forrest CB Khan S Localio AR Gerber A. Electronic medical record use in pediatric primary care. JAMIA. 2011;18(1):38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Asan O Montague E. More screen time, less face time - implications for EHR design. J Eval Clin Pract. 2014;20(6):896–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Asan O Montague E. Technology-mediated information sharing between patients and clinicians in primary care encounters. Behav Inform Technol. 2014;33(3):258–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Dowell A Stubbe M Scott-Dowell K Macdonald L Dew K. Talking with the alien: interaction with computers in the GP consultation. Aust J Prim Health. 2013;19(4):275–282. [DOI] [PubMed] [Google Scholar]
- 53. Kumarapeli P de Lusignan S. Using the computer in the clinical consultation; setting the stage, reviewing, recording, and taking actions: multi-channel video study . JAMIA. 2013;20(e1):e67–e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Montague E Asan O. Dynamic modeling of patient and physician eye gaze to understand the effects of electronic health records on doctor-patient communication and attention. Int J Med Inform. 2014;83(3):225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Shachak A Hadas-Dayagi M Ziv A Reis S. Primary care physicians’ use of an electronic medical record system: a cognitive task analysis. J Gen Intern Med. 2009;24(3):341–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Street RL Jr Liu L Farber NJ et al. Provider interaction with the electronic health record: the effects on patient-centered communication in medical encounters. Patient Educ Couns. 2014;96(3):315–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Alsos OA Dabelow B Faxvaag A. Doctors’ concerns of PDAs in the ward round situation. Lessons from a formative simulation study. Methods Inf Med. 2011;50(2):190–200. [DOI] [PubMed] [Google Scholar]
- 58. Alsos OA Das A Svanaes D. Mobile health IT: the effect of user interface and form factor on doctor-patient communication. Int J Med Inform. 2012;81(1):12–28. [DOI] [PubMed] [Google Scholar]
- 59. Swinglehurst D Greenhalgh T Roberts C. Computer templates in chronic disease management: ethnographic case study in general practice. BMJ Open. 2012;2(6):e001754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Pearce C Arnold M Phillips C Trumble S Dwan K. The patient and the computer in the primary care consultation. JAMIA. 2011;18(2):138–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Noordman J Verhaak P van Beljouw I van Dulmen S. Consulting room computers and their effect on general practitioner-patient communication. Fam Pract. 2010;27(6):644–651. [DOI] [PubMed] [Google Scholar]
- 62. Swinglehurst D Roberts C Greenhalgh T. Opening up the ‘black box' of the electronic patient record: a linguistic ethnographic study in general practice. Commun Med. 2011;8(1):3–15. [DOI] [PubMed] [Google Scholar]
- 63. Pearce C Walker H O'Shea C. A visual study of computers on doctors' desks. Inform Prim Care. 2008;16(2):111–117. [DOI] [PubMed] [Google Scholar]
- 64. Almquist JR Kelly C Bromberg J Bryant SC Christianson TH Montori VM. Consultation room design and the clinical encounter: the space and interaction randomized trial. HERD. 2009;3(1):41–78. [DOI] [PubMed] [Google Scholar]
- 65. Pearce C Dwan K Arnold M Phillips C Trumble S. Doctor, patient and computer–a framework for the new consultation. Int J Med Inform. 2009;78(1):32–38. [DOI] [PubMed] [Google Scholar]
- 66. Rhodes P Small N Rowley E Langdon M Ariss S Wright J. Electronic medical records in diabetes consultations: participants' gaze as an interactional resource. Qual Health Res. 2008;18(9):1247–1263. [DOI] [PubMed] [Google Scholar]
- 67. Chan WS Stevenson M McGlade K. Do general practitioners change how they use the computer during consultations with a significant psychological component? Int J Med Inform. 2008;77(8):534–538. [DOI] [PubMed] [Google Scholar]
- 68. Kazmi Z. Effects of exam room EHR use on doctor-patient communication: a systematic literature review. Inform Prim Care. 2013;21(1):30–39. [DOI] [PubMed] [Google Scholar]
- 69. Margalit RS Roter D Dunevant MA Larson S Reis S. Electronic medical record use and physician-patient communication: an observational study of Israeli primary care encounters. Patient Educ Couns. 2006;61(1):134–141. [DOI] [PubMed] [Google Scholar]
- 70. Pearce C Kumarpeli P de Lusignan S. Getting seamless care right from the beginning - integrating computers into the human interaction. Stud Health Technol Inform. 2010;155:196–202. [PubMed] [Google Scholar]
- 71. Pearce C Trumble S Arnold M Dwan K Phillips C. Computers in the new consultation: within the first minute. Fam Pract. 2008;25(3):202–208. [DOI] [PubMed] [Google Scholar]
- 72. Pearce C Arnold M Phillips CB Trumble S Dwan K. The many faces of the computer: an analysis of clinical software in the primary care consultation. Int J Med Inform. 2012;81(7):475–484. [DOI] [PubMed] [Google Scholar]
- 73. Blakeman T Chew-Graham C Reeves D Rogers A Bower P. The Quality and Outcomes Framework and self-management dialogue in primary care consultations: a qualitative study. Br J Gen Pract. 2011;61(591):e666–e673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Booth A Lecouteur A Chur-Hansen A. The impact of the desktop computer on rheumatologist-patient consultations. Clin Rheumatol. 2013;32(3):391–393. [DOI] [PubMed] [Google Scholar]
- 75. McGrath JM Arar NH Pugh JA. The influence of electronic medical record usage on nonverbal communication in the medical interview. Health Informatics J. 2007;13(2):105–118. [DOI] [PubMed] [Google Scholar]
- 76. Gibbings-Isaac D Iqbal M Tahir MA Kumarapeli P de Lusignan S. The pattern of silent time in the clinical consultation: an observational multichannel video study. Fam Pract. 2012;29(5):616–621. [DOI] [PubMed] [Google Scholar]
- 77. Newman W Button G Cairns P. Pauses in doctor–patient conversation during computer use: The design significance of their durations and accompanying topic changes. Int J Hum Comput Stud. 2010;68(6):398–409. [Google Scholar]
- 78. Doyle RJ Wang N Anthony D Borkan J Shield RR Goldman RE. Computers in the examination room and the electronic health record: physicians' perceived impact on clinical encounters before and after full installation and implementation. Fam Pract. 2012;29(5):601–608. [DOI] [PubMed] [Google Scholar]
- 79. Pearce CM Kumarapeli P de Lusignan S. “Effects of exam room EHR use on doctor-patient communication: a systematic literature review” - triadic and other key terms may have identified additional literature. Inform Prim Care. 2013;21(1):40–42. [DOI] [PubMed] [Google Scholar]
- 80. Hafner K. A busy doctor’s right hand, ever ready to type. The New York Times. January 12, 2014. http://www.nytimes.com/2014/01/14/health/a-busy-doctors-right-hand-ever-ready-to-type.html. Accessed July 22, 2015. [Google Scholar]
- 81. White A Danis M. Enhancing patient-centered communication and collaboration by using the electronic health record in the examination room. JAMA. 2013;309(22):2327–2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Shachak A Reis S Pearce C. Patient-physician interactions and electronic health records. JAMA. 2013;310(17):1857–1858. [DOI] [PubMed] [Google Scholar]
- 83. Duke P Frankel RM Reis S. How to integrate the electronic health record and patient-centered communication into the medical visit: a skills-based approach. Teach Learn Med. 2013;25(4):358–365. [DOI] [PubMed] [Google Scholar]
- 84. Reis S Sagi D Eisenberg O et al. The impact of residents' training in Electronic Medical Record (EMR) use on their competence: report of a pragmatic trial. Patient Educ Couns. 2013;93(3):515–521. [DOI] [PubMed] [Google Scholar]
- 85. Shachack A Domb S Borycki E et al. A pilot study of computer-based simulation training for enhancing Family Medicine residents’ competence in computerized settings. Medinfo 2015; August 21; Sao Paulo, Brazil. [PubMed] [Google Scholar]
- 86. Patel VL Kushniruk AW Yang S Yale JF. Impact of a computer-based patient record system on data collection, knowledge organization, and reasoning. JAMIA. 2000;7(6):569–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Ventres W Kooienga S Marlin R Vuckovic N Stewart V. Clinician style and examination room computers: a video ethnography. Fam Med. 2005;37(4):276–281. [PubMed] [Google Scholar]
- 88. Dennis AR Fuller RM Valacich JS. Media, tasks, and communication processes: a theory of media synchronicity. MIS Quarterly. 2008;32(3):575–600. [Google Scholar]
- 89. Daft RL Lengel RH. Organizational information requirements, media richness and structural design. Manag Sci. 1986;32(5):554–571. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.