Abstract
The purpose of this study was to investigate the effects of an intensive toilet training program on continence and self-initiation for elementary children with autism spectrum disorder (ASD). Researchers used a non-concurrent multiple baseline design (Watson and Workman in J Behav Ther Exp Psychiatry 12:257–259, 1981, 10.1016/0005-7916(81)90055-0) with regulated randomization (Koehler and Levin in Psychol Methods 3(2):206, 1998, 10.1037/1082-989X.3.2.206) to evaluate the effects of the intensive protocol with four students with ASD in the classroom where they received special education services. The protocol included increased access to fluids, contingent time intervals for sit schedules, programmed reinforcement, and dry checks. All four participants met mastery criteria and maintained independent toileting after the study’s completion. Three participants began self-initiating to use the restroom. The implications and recommendations for future research are discussed.
Keywords: Toilet training, Incontinence, Autism spectrum disorder, Classroom-based interventions
Children with autism spectrum disorder (ASD) are more likely to have higher rates of urinary incontinence than children without disabilities (Niemczyk et al. 2018; von Gontard 2013). Children who are incontinent beyond their 8th birthday are less likely to become continent which emphasizes a need for early intervention (Singh et al. 2006). According to the Centers for Disease Control and Prevention (2020), children with ASD may experience barriers to toilet training, thus long-term incontinence, due to communication, language, motivation, and rigidity of routines. Parents of children with ASD may be discouraged to begin toilet training if their child does not demonstrate skills considered readiness indicators such as remaining dry, completing steps associated with toileting and communicating about toileting (Schum et al. 2002; Wheeler 2007). Additionally, attention that may otherwise be spent on toileting, may be allocated to more pressing concerns such as communication and challenging behavior (Hayes and Watson 2013). A lack of emphasis on toilet training in the early years may pose challenges for individuals with ASD and their families later on.
Parents of children with ASD experience stress due to long-term support needs specific to toileting (Estes et al. 2009; Gray 1994). Stressors may include limited access to services, fewer opportunities to participate in the community, and increased costs. Individuals with disabilities experience greater opportunities to participate in inclusive environments with independent toileting skills (Cicero and Pfadt 2002). According to the American Academy of Pediatrics (1999), early care providers (e.g., daycares) should play a role in toilet training young children. However, access to these services may be limited for children experiencing incontinence after the typical age children are in diapers (i.e., 3 years). Some childcare policies prevent children over the age of three from moving on to classrooms with their same age peers or continuing in a program all together if children are not potty trained (Bever 2016). Once children enter elementary school, the Individuals with Disabilities Education Act (IDEA 2004) requires that public schools provide a free and appropriate public education to eligible students, but incontinence may restrict inclusive opportunities and extracurricular activities (Sansosti and Sansosti 2012). Additionally, time spent on toilet training and hygiene may take away time from other educational activities. Long-term urinary incontinence may impact parents' options for summer camps leaving them with fewer options for summer childcare. Finally, the required assistance needed to care for individuals who experience incontinence makes them more vulnerable to abuse (Sapi et al. 2009) and potentially diminishes their self-image (Collier et al. 2002). Given the barriers associated with incontinence, families and teachers of children with ASD may make toilet training a focal point during the early educational years.
Teachers and parents may incorporate goals related to toilet training as part of the Individualized Education Program. Toilet training interventions for individuals with developmental disabilities are often more intensive than home-based programs designed for children around 2 years without disabilities. Home-based programs for children around 2 years typically involve the parent taking the child to the restroom to sit at regular time points and asking the child if they need to use the restroom (Kaerts et al. 2014). However, interventions for toilet training become more intensive as the level of cognitive disability increases (Matson and Issarraras 2019). Azrin and Foxx (1971) developed a Rapid Toilet Training Method that shaped the way teachers, practitioners, and caregivers implement toilet training for children with developmental disabilities. This rapid program is intensive in that it comprises 16 components including emphasis on a specific environment, increased fluids, increased practices with dressing, approaching the toilet and other associated steps, regular monitoring for early detection of accidents, and complex consequences for voids on the toilet and accidents. More recent research in this area has incorporated components of the Rapid Toilet Training Method, including positive reinforcement for on toilet voids, increased fluid intake, dense trip schedules, and instruction for self-initiation with an emphasis on these services provided in nonclinical settings (Cicero and Pfadt 2002; Kroeger and Sorensen-Burnworth 2009; Kroeger and Sorensen 2010; LeBlanc et al. 2005; Stadtler et al. 1999).
Non-clinical settings, such as schools, present challenges to toilet training due to rigid schedules, increased student to teacher ratios, access to restrooms suitable for training, and increased emphasis on academic instruction. Kroeger and Sorensen-Burnworth reviewed the toilet training literature conducted with individuals with ASD prior to 2008. The findings dated back as far as 1971 and of the 28 data-based papers found, only three studies took place completely in a school (Cicero and Pfadt 2002; Sadler and Merkert 1977; Richmond 1983). With increased focus on functional skills due to IDEA (2004), additional research is necessary to evaluate the implementation of intensive toilet training (ITT) packages in traditional school settings.
Cocchiola et al. (2012) evaluated the effects of a school-based toilet training program with children ranging in age from 3 to 5 years diagnosed with ASD or a developmental delay. Each participant had all-day individualized support from an adult training to become a behavior analyst. The students remained in their diapers during baseline and the teachers checked the diaper every 30–60 min providing verbal praise contingent on dry diapers and on-toilet voids. During intervention, students’ diapers were removed, and they were offered fluids throughout the day. Researchers provided a task analysis and a verbal reminder of the contingency during each trip to the restroom. Children went to the restroom every 30 min initially, and this interval increased by 15 min after three consecutive days without accidents until the maximum interval, 120 min was met. All five participants remained dry for at least 2 h and urinated on the toilet after the completion of this study. Further research is necessary to replicate these findings and include programs to teach self-initiation to use the restroom.
In a component analysis, Perez et al. (2020) found that ITT packages may not be necessary for some students with ASD. Additionally, Greer et al. (2016) found wearing underwear to be the most important component for toilet training packages for young children and for some, this component alone was sufficient in improving continent voids with young children. The findings suggest students with ASD should experience wearing underwear during baseline conditions prior to intensive interventions to ensure complex interventions are necessary.
Further research is necessary to replicate these findings to older children with presumably more failed attempts at toilet training and in the classroom setting. Additionally, protocols should incorporate opportunities to remove diapers prior to implementation of intensive protocols and with components to teach self-initiation. The purpose of this study was to evaluate the effects of an ITT package on the urinary incontinence of early elementary students with ASD in a special education classroom. Researchers sought to answer the following research questions:
What are the effects of an ITT package on urinary incontinence of early elementary students with ASD in the context of a special education classroom?
What are the effects of an ITT package on self-initiation for using the restroom of early elementary students with ASD in the context of a special education classroom?
Method
Participants
Four Black students receiving special education services in a public, university-affiliated demonstration classroom participated in the study. Eight students received services in this classroom due to deficits in communication and functional skills. Prior to baseline, all participants could (a) follow simple directions, (b) sit on the toilet for 1–2 min without challenging behavior, (c) independently remove pants‚ undergarments‚ and diapers in order to void in the toilet, (d) complete self-care skills including feeding themselves, and (e) had a history of remaining dry for periods of time throughout the school day. The classroom teacher gathered this information through surveys sent home to families. Participant parent and/or guardians completed the survey and returned it to school. Students were not included in the research project if their parents had medical concerns pertaining to incontinence. The second author and lead teacher in the classroom where all students received special education services, recruited the students to participate in the research study after classroom data revealed they primarily voided in diapers. Researchers received parental permission for all students to participate in the study and prior to the onset of toilet training they were asked several questions about their history with toilet training. All parents reported attempting toilet training with their child upwards of 11 times with zero success.
Nate
The first participant, a first-grade male student, was 6.5 years of age and was eligible for special education services due to characteristics of ASD. Nates Verbal Behavior—Milestones and Placement Program (VB-MAPP; Sundberg 2008) scores were 11.5 out of 170 on Milestones, 68 out of 96 on Barriers, 22 on Transitions, and zero on the Early Echoic Skills Assessment (EESA; Esch 2008). Academic goals for Nate included receptive identification of letters, numbers, shapes‚ and common objects, as well as counting using 1:1 correspondence. Prior to the onset of the study, Nate communicated with one to two-word phrases on an iPad equipped with speech-generating software. He was taught to request ‘toilet’ with Most-to-Least prompting (Baer et al. 1967) using the speech-generating device for the initiation portion of the study. To access “toilet” on the device, Nate had to press the home living button and then the toilet button was visible.
Ivy
Ivy, a female kindergarten student, was 6.2 years of age at the start of the study. She had an educational eligibility of ASD. Ivy’s VB-MAPP scores were 60.5 out of 170 on the Milestones assessment, 41 out of 96 on the Barriers assessment, 29 on the Transitions assessment, and 72 on the EESA. Academic goals for Ivy included expressive identification of letters, numbers, letter sounds, common objects, shapes answering personal questions, rote counting‚ and counting using 1:1 correspondence. Prior to the study, Ivy communicated using two-to-three-word phrases and was taught to initiate bathroom trips by saying “potty” and/or exchanging a picture of a toilet with model prompts.
Dan
Dan, a first-grade male student, was 6.8 years of age at the time of the study with an educational eligibility of ASD. Dan scored 11.5 out of 170 on the VB-MAPP Milestones, 79 out of 96 on the Barriers, 16 on Transitions, and zero on the EESA. Academic goals for Dan included matching shapes, letters, numbers, and common objects. Prior to the onset of the study, Dan communicated with Picture Exchange Communication Systems (PECS; Bondy and Frost 1994) by combining sentence starters with pictures of items. He communicated with various staff across all school and community settings. Dan was taught to initiate bathroom trips by exchanging the sentence strip with two pictures to state ‘I want potty’ following the procedures of PECS.
James
James, a second-grade male student, was 7 years of age at the time of the study. James received special education services due to his significant developmental delays. James also engaged in behaviors consistent with ASD. On the VB-MAPP assessment, James scored a 4.5 out of 170 on Milestones, 85 out of 96 on Barriers, 16 on Transitions and 0 on the EESA. Academically, James's goals included matching shapes, numbers, letters in his name, and common objects. Prior to the onset of the study, James mostly communicated by taking the listener’s hand and directing it towards what he needed or handing the listener an item to request assistance. James had experience with PECS training but needed additional support with discriminating pictures. To assist with discriminating the picture of the toilet from other pictures, the team used a 2.5 × 4 in potty picture with bolded letters and a blue background.
Setting and Materials
The study took place primarily in the participants’ classroom and assigned hallway restroom. The classroom was located in an urban Title I public school in the southeast United States. Faculty and graduate students affiliated with the local university operated the classroom. The lead teacher, a certified teacher, completed her master’s program during the time of the project. The support staff in the classroom consisted of graduate students pursuing master’s degrees in applied behavior analysis and adapted curriculum special education. Each day there were at least five staff in the classroom. The lead teacher and one support person with a bachelor’s degree in special education conducted the study. All classroom staff and members of the research team were trained on how to communicate with students through their augmentative and alternative systems of communication.
Response Definitions and Data Collection
Researchers collected event recording data on the primary dependent variable, percent of urine in-toilet voids. The data sheets are available by contacting the first author. The researcher recorded on-toilet voids when they occurred during restroom trips and off-toilet voids when voids occurred without the student on the toilet. The team defined urine in-toilet voids as any void that produced at least one second of a continuous stream of urine in the toilet. Only one on-toilet void could be recorded per trip to the restroom. Off-toilet voids occurred when a student voided anywhere besides the toilet (e.g., next to the toilet, hallway, classroom). They calculated percent of voids by dividing the number of urine voids that took place on the toilet by the total voids (voids off toilet and voids on toilet) across each day. The research team also monitored initiated voids defined as any time the participant requested a trip to the restroom by exchanging a picture of a toilet, vocalizing “potty,” or any other associated word, or touching the picture on a speech-generating device. Researchers calculated these data by dividing the number of initiated voids by the total voids (voids off toilet and voids on toilet).
Procedures
Researchers implemented an ITT package (Harbin et al. 2016). Participants wore underwear under clothing during baseline and intervention conditions across the entire school day (8:00 AM to 2:00 PM) and had access to an established augmentative and alternative communication system (e.g., picture card or SGD) across baseline, intervention, and maintenance conditions and environments to allow for initiations to use the restroom. Each school day was considered one session. During baseline, the researcher brought the child to the restroom every 90 min and instructed them to remove their clothing and sit on the toilet for 5 min. Intervention consisted of several components including: contingent time intervals for sit schedule, programmed reinforcement for on-toilet voids, dry checks after accidents, increased access to fluids, and initiation training.
Pre-baseline
Pre-baseline represented the classroom procedures prior to the onset of the study. These data were collected daily to communicate with families and provide a routine around using the restroom. During this time, all participants wore diapers (sent by their caregivers) under their clothing throughout the school day. Researchers took students to the restroom every 60–90 min. Researchers gave students the opportunity to sit on the toilet if they initiated but did not require them to sit. If the participant had soiled their diaper, the researcher used graduated guidance (MacDuff et al. 1993) to prompt the participant to complete the steps to remove soiled clothing and replace with clean clothing. If the participant voided on the toilet the researcher simply said, “Good job going potty” and returned to the classroom activities.
Preference Assessment
Researchers conducted preference assessments for all participants prior to the start of intervention. A multiple stimulus without replacement (MSWO) preference assessment was conducted for food and leisure items. Researchers chose five items to include for each category based on the participants general classroom preferences. General classroom preferences were determined at the beginning of the school year through parent/caregiver interview, records review, and classroom observations. For each category the MSWO was conducted two to three times for each participant to ensure a consistent hierarchy. The top-ranking food and leisure items were used as reinforcers during intervention.
Baseline
The purpose of this condition was to establish the frequency of voids without an ITT package and introduce underwear prior to intervention. At the start of each participant’s day researchers helped participants change out of their diaper and into underwear. The researchers took participants to the restroom every 90 min from 8:00 AM to 2:00 PM. If participants arrived late to school, they changed to underwear upon arrival. Every 90-min interval, researchers escorted each participant to the closest school bathroom. After determining if the participant was wet or dry, the child sat for 5-min on the toilet. During the 5-min, researchers provided the participant with moderate attention. If a participant voided on the toilet during baseline, the researcher stated “Good job going potty” with neutral affect. If the participant voided off the toilet during baseline, the researchers escorted the child to the restroom and changed their soiled clothes with neutral affect and minimal vocalizations.
Intervention
Contingent Time Intervals for Sit Schedule
At the start of intervention researchers brought the participant to the restroom every 15 min. Similar to baseline, researchers encouraged participants to sit on the toilet for 5 min during each scheduled sit. If the participant voided in the toilet, the interval between sits increased by 5 min. Each successful void resulted in an increase in the interval by 5 min (i.e., 15 min, 20 min, 25 min) until the interval reached 120 min. If the participant voided off the toilet twice without a successful void, the interval was decreased by 5 min (e.g., 25–20 min). If there were two consecutive off-toilet voids followed by an on-toilet void, the interval length remained the same.
Programmed Reinforcement
If the participant voided on the toilet, the researchers provided behavior specific praise (e.g., “Good job going pee in the potty”) and the top reinforcer identified in the preference assessment immediately following the void on the toilet. The participant could play with tangible items for 2 min and consume one preferred food item. The reinforcer for on-toilet voids was only available for successful voids during the course of the training.
Response to Accidents
If a participant voided off the toilet, researchers responded by saying “we pee on the potty” in a quiet neutral affect and they were immediately brought to the restroom. Researchers instructed the student to remove their soiled clothing and implemented graduated guidance as needed. If the void began off the toilet but ended on the toilet, a successful void was counted, and the student accessed the programmed reinforcer.
Dry Checks
If the participant did not urinate on the toilet during a scheduled trip to the restroom the researchers implemented dry checks for the subsequent interval. The researcher set an interval timer that alerted them every 5 min. At this time the researcher approached the student and stated, “I am going to check to see if you are wet or dry” and prompted them to check their underwear with their own hand with physical prompting. If the participant was dry, the researcher stated, “Good job staying dry” and if they were wet the researcher immediately brought them to the restroom and completed the steps for off-toilet voids. If the participant voided on the toilet, dry checks did not take place during the following interval.
Initiation Training
All participants had access to their established augmentative and alternative communication system throughout the day. Researchers placed a picture of a toilet on the front of PECS books or the home screen of each individual’s speech-generating device. For participants who communicated primarily with spoken words, the researcher ensured they had access to a laminated picture of the toilet throughout the day to allow for prompting an exchange and multiple modalities of communication. During intervention, researchers prompted the participant to exchange or activate their SGD prior to each trip to the restroom using most-to-least prompting (McDonnell and Ferguson 1989). All participants had the opportunity to initiate a trip to the restroom anytime throughout the day if they vocalized, exchanged a picture or activated their device. If they initiated a trip, the researcher immediately brought the participant to the restroom and allowed them to sit on the toilet for 5 min. If they voided on the toilet after initiation, they accessed programmed reinforcers and the time in between intervals was increased by 5 min. If during the interval the participant initiated and did not void on the toilet, the researcher brought them back to the classroom and responded to every subsequent initiation during the interval with “we’ll go to the potty in a little bit.”
Increased Access to Fluids
After changing into underwear and arriving at the classroom, researchers provided the participant with access to one cup of a moderately preferred drink (i.e., water, juice). Researchers moved the cup within 1 m of the participant throughout the day to ensure participants had access to fluids throughout the day. Researchers prompted participants to drink fluids every 10 min during off-toilet intervals until the interval reached 60 min at which point the researcher prompted approximately 2–3 times during the interval. Participants were never forced to drink fluids. Fluid intake never exceeded 24 oz (710 mL). Researchers tracked the participants fluid intake by filling up a pitcher with labeled measurements at the beginning of each school day and filling up the participant’s personal cup from that pitcher. At the end of the day the remaining fluid in the participant's personal cup was poured back into the pitcher and the number of ounces that remained in the pitcher was then subtracted from the amount from the start of the day. This information was recorded on the data sheet.
Generalization and Maintenance
Researchers programmed for generalization by exploiting natural consequences, reinforcing occurrences of generalization, training diversely with sufficient stimulus exemplars, and incorporating common salient social and physical stimuli (Stokes and Osnes 1989). When participants remained dry, they escaped discomfort due to soiled clothes thus accessed the natural consequence. When participants voided in other settings and with other classroom staff, they also accessed programmed positive reinforcers (e.g., food and preferred leisure items). Participants were taken to the various restrooms within the school and during community-based instruction (e.g., community center pool, fast food restrooms, retail locations) by various classroom staff. By incorporating different settings and classroom staff, researchers programmed for the transfer of stimulus control to the naturally occurring stimuli in the environment. Despite the variability in staff and restroom location, researchers kept the toilet picture and teacher directive consistent throughout all environments to incorporate common salient stimuli.
Researchers programmed for maintenance by gradually increasing the time between restroom visits, systematically thinning the schedule of reinforcement for on-toilet voids, and training parents and other staff at the completion of toilet training. Once each participant reached mastery criteria, 1 full day at 120 min intervals with zero accidents, researchers continued the intervention package for 6 days. During those 6 days, the researcher refrained from conducting dry checks and did not offer additional fluids to the participant. After 6 days, researchers thinned the schedule of reinforcement for on-toilet voids. Every 2 days that the participant did not have an accident, the magnitude of reinforcement was reduced. For example, for Nate, his reinforcement included 4 chips and 2 min on the iPad during treatment. Post-maintenance, time on the iPad was thinned by 30 s every 2 days, contingent upon zero accidents, until it was no longer used as a reinforcer. Chips were reduced by one every 2 days after this, when the number of chips reached one, half of the chip was given and then ¼ until it was no longer used as a reinforcer. Social praise provided by the researcher, such as “great job going pee on the toilet” remained constant throughout maintenance. Once each participant reached criterion for mastery, the primary researcher invited the parents or guardians to the classroom to provide training to program for generalization and maintenance in the home setting. During the parent training, the researcher reviewed information specific to how the participant initiated and any idiosyncrasies pertaining to their toilet training plan. The researcher also provided guidance on how often to take the children to the restroom, how to respond to accidents, and how to respond to in-toilet voids at home. Parents also had the opportunity to ask questions and were encouraged to discontinue diapers during the time the participant was awake at home.
Reliability
Interobserver agreement (IOA) was collected across 27% of all baseline, intervention, and maintenance sessions for all participants. A trained support person from the classroom that was available at the time of the bathroom trip collected this data. The support person varied depending on the time of day. The second author calculated IOA with trial-by-trial (Cooper et al. 2020), by dividing the number of trials with agreements by the number of trials with agreements plus disagreements and multiplied by 100. IOA for all sessions was 100% agreement across all participants. A support person also collected procedural fidelity data using a checklist specific to the baseline, intervention, and maintenance sessions. Procedural fidelity across 27% of all conditions for all participants was 100%.
Experimental Design
Researchers evaluated the effects of the ITT package on incontinence with a non-concurrent multiple probe design (Gast et al. 2018) with regulated randomization (Koehler and Levin 1998). Kratochwill and Levin (2010) describe regulated randomization with two primary components: (1) random assignment of the order participants begin intervention (2) and randomization of the specific start time within each tier. After identifying four participants based on the inclusion and exclusion criteria, the team randomized the order participants would begin intervention prior to baseline. Once baseline responding was stable and after 5 days of baseline data collection, the researchers randomly decided on the start point by flipping a coin. For instance, if baseline data were stable after 5 days of responding the researcher flipped a coin on the 5th day to determine if the participant would begin intervention on day 6 or 7. The team used the ‘flip a coin’ function on google.com, deciding prior to the flip that heads meant to start intervention and tails meant 1 more day of baseline. Therefore, there were two random start points for each participant (k = 2). By randomizing the start point after stable baseline responding, the team did not compromise visual analysis, an important component of single-case design. After the first participant began intervention, they remained in the intervention condition until they voided 100% of voids on the toilet for 1 day with scheduled trips to the restroom every 90 min. In order to maintain a staggered start point across participants the second participant did not begin intervention until the first participant had begun responding to treatment (reaching the criteria of 90 min off toilet intervals and 100% of voids in the toilet). Therefore, the second participant did not begin intervention until day 21 and the third participant did not begin intervention until the 32nd day. Researchers collected probe data throughout intervention to evaluate the internal validity of the independent variable.
Results
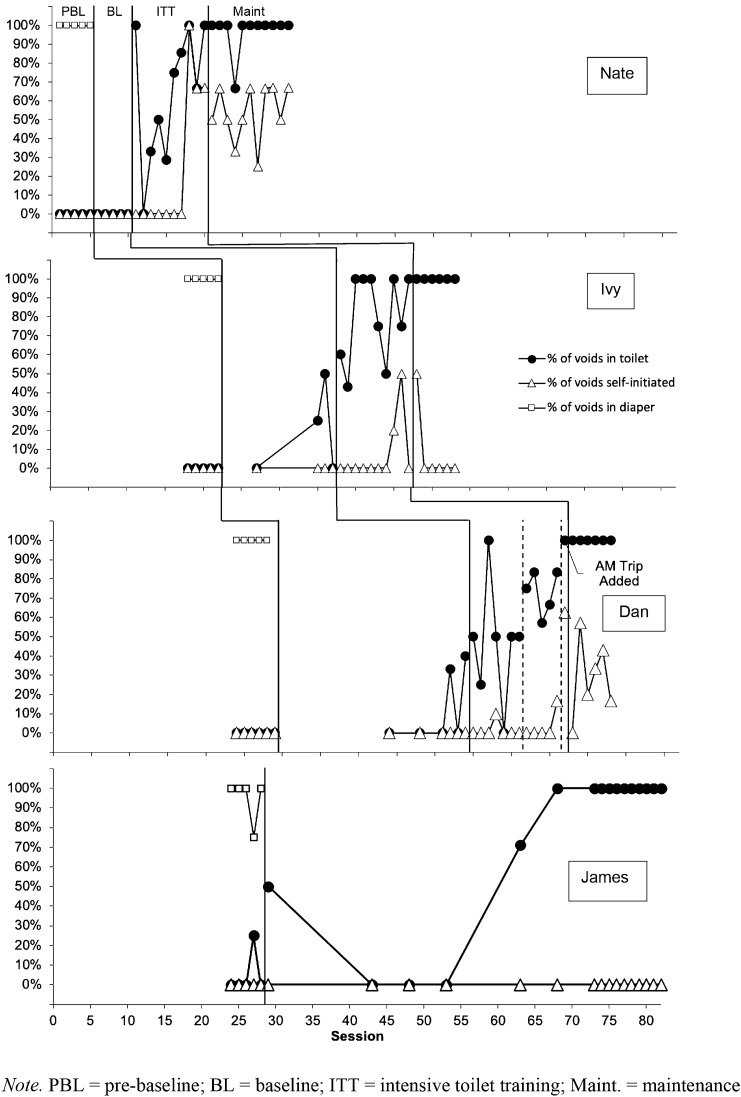
Figure 1 displays the percentage of voids in the participant’s diaper during pre-baseline and on toilet voids and self-initiated voids for all four participants during baseline and intervention. Each session represents one school day.
Fig. 1.
Percentage of voids in diaper, in-toilet voids, and self-initiated voids
On-Toilet Voids
Nate
During the pre-baseline condition, Nate urinated 100% of voids across all sessions in his diaper. All of Nate’s voids occurred outside of the toilet during baseline when Nate transitioned to underwear. At the onset of intervention, an immediate change in level occurred for Nate, but data remained variable with one data point dropping to baseline levels. By the eighth session of intervention (75–80 min interval restroom trips), Nate’s voids occurred in the toilet 100% of the time. Nate reached the criteria of 1 full-day at 120-min interval restroom trips with zero accidents on the 15th day of intervention. Nate remained dry across all six sessions of maintenance.
Ivy
During the pre-baseline condition, Ivy urinated 100% of voids across all sessions in her diaper. Ivy voided in the toilet for two out of four sessions during baseline, but the percentage of in-toilet voids did not exceed 50%. Following the introduction of intervention there was a change in level compared to the baseline condition with six of eight sessions remaining above baseline levels. Ivy voided in the toilet 100% of sessions with 1 full day at 120 min intervals with zero accidents by the tenth session of intervention. Ivy remained continent across all six sessions of maintenance.
Dan
During the pre-baseline condition, Dan urinated 100% of voids across all sessions in his diaper. Dan voided in the toilet for two out of seven sessions, but his percentage of on-toilet voids did not exceed 40% in baseline. A slight change in level occurred during intervention and five of the initial seven data points did not overlap with baseline data. Following the removal of excess fluids at day 39, there was an immediate change in level with some variability and Dan voided off the toilet at least 20% of every session. Accidents commonly occurred in the morning, so researchers incorporated an additional trip to the restroom following breakfast. Following this slight change in procedures, Dan remained dry across the entire school day with trips to the restroom every 120 min. Dan remained dry across all six sessions of maintenance.
James
During the pre-baseline condition, James voided in his diaper for 100% of all but one session. During the fourth data collection day of pre-baseline, James voided 25% of the time in the toilet. When James transitioned to underwear from diapers, he immediately voided in the toilet 50% of trips to the restroom. The following three sessions he did not void in the toilet, but there was an abrupt change in level following the fourth session of baseline. By the sixth session of baseline, James voided in the toilet for 100% of voids and continued this pattern across the remainder of sessions.
Initiation
Nate
During pre-baseline and baseline, Nate did not initiate trips to the restroom. On session 18, the 8th day of intervention, Nate initiated 100% of trips to the restroom with his SGD. Nate initiated across all remaining sessions of intervention and maintenance for 33–67% of trips to the restroom.
Ivy
During pre-baseline and baseline, Ivy never initiated trips to the restroom. Ivy first initiated a trip to the restroom on day 28, the 8th day of intervention, by vocalizing. She never initiated more than 50% of trips to the restroom and this behavior did not maintain beyond the first session of maintenance.
Dan
Dan did not initiate trips to the restroom during pre-baseline or baseline conditions. Dan infrequently initiated trips to the restroom after session 35, the 4th session of intervention by exchanging a PECS sentence strip with the words and pictures, “I want to potty.” The last session of intervention, Dan initiated 63% of trips. The variability in initiation stabilized slightly across the last five sessions of maintenance ranging from 57 to 17%.
James
James did not participate in initiation training during the course of the study, since he became continent with the removal of the diaper.
Discussion
The purpose of this study was to evaluate the effects of an ITT program in the context of a school setting on continent voids and self-initiation for restroom trips for children with ASD. Three of the four participants met the mastery criteria and remained dry across the school day when taken to the restroom every 120 min. The fourth participant reached mastery criterion during baseline when his diaper was removed. Three of the four participants demonstrated some improvement with self-initiation for trips to the restroom.
These findings provide additional evidence to support the effectiveness of ITT packages implemented in classroom settings (Cocchiola et al. 2012). The ITT incorporated components of the Foxx and Azrin (1973) protocol but notably did not include punishment-based procedures (e.g., overcorrection) suggesting these components may not be necessary when toilet training children with ASD and developmental disabilities. This is relevant considering the requirement of behavior analysts and classroom teachers to avoid punitive measures if possible (Behavior Analysis Certification Board 2014; Council for Exceptional Children 2015). This study extended the findings of previous research by incorporating strategies to teach self-initiation (Cocchiola et al. 2012; Kroeger and Sorensen-Burnworth 2009) and exposure to underwear prior to intensive interventions (Greer et al. 2016; Perez et al. 2020).
Clinical Implications
These findings provide preliminary support for consistently pairing trips to the restroom with prompted communication for initiation. Participants did not initiate all trips to the restroom, but the percentage of self-initiated restroom trips may have been appropriate for this age of students since students in early elementary years are often taken to the restroom regularly throughout the day as a preventative measure. Additionally, these findings suggest that ITT programs are effective in the classroom setting as long as enough staff are available to support the student. School systems may consider providing short term classroom support (e.g., 1–2 weeks) for the initial days of toilet training before a reasonable sit interval is attained (e.g., 60 min between trips to the restroom). Finally, teachers may be more likely to approach toilet training with students still in diapers, but they should consider removing diapers before toilet training or as part of the intervention (Greer et al. 2016). As noted by the final participant, James, diaper removal was sufficient for increasing continence and on-toilet voids.
Future Research
Researchers should consider incorporating similar phases, pre-baseline with diapers, baseline without, and intensive intervention but stagger the onset of baseline to evaluate the effects of diaper removal. Some informal follow up with families took place following the completion of the maintenance phase, but formal follow up and extended maintenance was made impossible due to the COVID-19 pandemic. Future research should evaluate the effects of the program on home toileting to determine the level of training necessary to transfer stimulus control to the home setting.
Limitations
Although the results of this study indicate that the ITT package was effective for increasing on-toilet voids and initiations, some limitations may have impacted the internal validity of the study. First, the ITT package did not directly teach participants to have a bowel movement on the toilet. When participants did have a bowel movement the team provided the same reinforcers for on-toilet urine voids and treated the occurrence as an accident for off-toilet bowel movements. The participants did not regularly have bowel movements at school. Next, researchers evaluated the effects of the intervention with a non-concurrent multiple baseline design. Researchers attempted to strengthen this design and dispel concerns regarding threats to internal validity such as history and maturation by incorporating regulated randomization (Koehler and Levin 1998) and chronologically displayed data. Due to logistics including number of staff and sanitation issues, researchers did not begin baseline on the same day for all participants but provided pre-baseline data to indicate the number of on toilet voids and accidents for all participants. Finally, the incorporation of regulated randomization prevented the researchers from extending the baseline phase specifically for Ivy and Dan to determine if the long-term use of underwear would have led to mastery criterion for both participants. When researchers determined the start point for intervention, all baseline data were stable. The researchers chose to continue with the intervention condition despite some variability in baseline due to the a priori determination of randomized intervention start times (Koehler and Levin 1998) and the necessity to prevent off-toilet voids due to cleanliness and the dignity of the students.
Results of this study suggest that ITT packages are effective at increasing on-toilet voids and continence for early elementary students with ASD in the classroom setting. All participants became continent during the course of the study and one student became continent during baseline after his diaper was removed. Additionally, the three students that participated in the intensive toilet training package demonstrated initial progress with self-initiation. Additional research is needed to continue to investigate the various components of ITT packages.
Acknowledgments
The authors would like to acknowledge the classroom staff that supported this endeavor including Megan Lee and Dr. Kevin Ayres. We would also like to express our appreciation to the students who participated in this research project. We wish each student the best as they pursue a more independent life.
Author Contributions
Rachel R. Cagliani designed and oversaw the study and drafted, reviewed, and revised the manuscript. Sara Kathryn Snyder supervised the research, trained data collectors, implemented the protocol, collected data, contributed to the initial draft, reviewed, and revised the manuscript. Emily N. White provided input with the design of the study, supported data collection, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
No funding was provided for this study.
Compliance with Ethical Standards
Conflict of interest
We have no known conflict of interest to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- American Academy of Pediatrics Toilet training guidelines: Day care providers—The role of the daycare provider in toilet training. Pediatrics. 1999;103(Supplement 3):1367–1368. [PubMed] [Google Scholar]
- Azrin NH, Foxx RM. A rapid method of toilet training the institutionally retarded. 1. Journal of Applied Behavior Analysis. 1971;4(2):89–99. doi: 10.1901/jaba.1971.4-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer DM, Peterson RF, Sherman JA. The development of imitation by reinforcing behavioral similarity to a model. Journal of Experimental Analysis of Behavior. 1967;10:405–416. doi: 10.1901/jeab.1967.10-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bever, L. (2016). The potty-training expulsion that got a N.J. school sued by the state. Washington Post. https://www.washingtonpost.com/news/education/wp/2016/10/31/the-potty-training-expulsion-that-got-a-n-j-school-sued-by-the-state/.
- Behavior Analyst Certification Board. (2014). Professional and ethical compliance code for behavior analysts. Littleton, CO: Behavior Analyst Certification Board. https://www.bacb.com/wp-content/uploads/2020/05/BACB-Compliance-Code-english_190318.pdf.
- Bondy A, Frost L. The picture exchange communication system. Focus on Autism and Other Developmental Disabilities. 1994;9(3):1–19. doi: 10.1177/108835769400900301. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Case Study II: A Closer Look. https://www.cdc.gov/ncbddd/actearly/autism/case-modules/anticipatory-guidance/06-closer-look.html.
- Cicero FR, Pfadt A. Investigation of a reinforcement-based toilet training procedure for children with autism. Research in Developmental Disabilities. 2002;23(5):319–331. doi: 10.1016/S0891-4222(02)00136-1. [DOI] [PubMed] [Google Scholar]
- Cocchiola MA, Martino GM, Dwyer LJ, Demezzo K. Toilet training children with autism and developmental delays: An effective program for school settings. Behavior Analysis in Practice. 2012;5(2):60–64. doi: 10.1007/BF03391824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collier J, Butler RJ, Redsell SA, Evans JH. An investigation of the impact of nocturnal enuresis on children’s self-concept. Scandinavian Journal of Urology and Nephrology. 2002;3:204–208. doi: 10.1080/003655902320131884. [DOI] [PubMed] [Google Scholar]
- Cooper JO, Heron TE, Heward WL. Applied behavior analysis. Boston: Pearson; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council for Exceptional Children. (2015). What every special educator must know: Professional ethics and standards. Arlington, VA: CEC. https://exceptionalchildren.org/sites/default/files/2020-07/Code%20of%20Ethics.pdf.
- Esch BE. Early echoic skills assessment. In: Sundberg ML, editor. Verbal behavior milestones assessment and placement program: The VB-MAPP. Concord: AVB Press; 2008. p. 24. [Google Scholar]
- Estes A, Munson J, Dawson G, Koehler E, Zhou XH, Abbott R. Parenting stress and psychological functioning among mothers of preschool children with autism and developmental delay. Autism. 2009;13(4):375–387. doi: 10.1177/1362361309105658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foxx RM, Azrin NH. Dry pants: A rapid method of toilet training children. Behaviour Research and Therapy. 1973;11(4):435–442. doi: 10.1016/0005-7967(73)90102-2. [DOI] [PubMed] [Google Scholar]
- Gast DL, Lloyd BP, Ledford JR. Multiple baseline and multiple probe designs. In: Ledford JR, Gast DL, editors. Single case research methodology: Applications in special education and behavioral sciences. 3. London: Routledge; 2018. p. 270. [Google Scholar]
- Gray D. Coping with autism: Stresses and strategies. Sociology of Health and Illness. 1994;16(3):275–300. doi: 10.1111/1467-9566.ep11348729. [DOI] [Google Scholar]
- Greer BD, Neidert PL, Dozier CL. A component analysis of toilet-training procedures recommended for young children. Journal of Applied Behavior Analysis. 2016;49(1):69–84. doi: 10.1002/jaba.275. [DOI] [PubMed] [Google Scholar]
- Harbin, E.R., Ledford, J.R., & Chazin, K.T. (2016). Intensive toilet training. In Evidence-based instructional practices for young children with autism and other disabilities. Retrieved from http://ebip.vkcsites.org/intensive-toilet-training.
- Hayes SA, Watson SL. The impacts of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disability. 2013;43:629–642. doi: 10.1007/s10803-012-1604-y. [DOI] [PubMed] [Google Scholar]
- Individuals with Disabilities Education Act, 20 U.S.C. § 1400 (2004)
- Kaerts N, Vermandel A, Van Hal G, Wyndaele JJ. Toilet training in healthy children: Results of a questionnaire study involving parents who make use of day-care at least once a week. Neurourology and Urodynamics. 2014;33(3):316–323. doi: 10.1002/nau.22392. [DOI] [PubMed] [Google Scholar]
- Koehler MJ, Levin JR. Regulated randomization: A potentially sharper analytical tool for the multiple-baseline design. Psychological Methods. 1998;3(2):206. doi: 10.1037/1082-989X.3.2.206. [DOI] [Google Scholar]
- Kratochwill TR, Levin JR. Enhancing the scientific credibility of single-case intervention research: Randomization to the rescue. Psychological Methods. 2010;3(2):124–144. doi: 10.1037/14376-003. [DOI] [PubMed] [Google Scholar]
- Kroeger K, Sorensen R. A parent training model for toilet training children with autism. Journal of Intellectual Disability Research. 2010;54(6):556–567. doi: 10.1111/j.1365-2788.2010.01286.x. [DOI] [PubMed] [Google Scholar]
- Kroeger KA, Sorensen-Burnworth R. Toilet training individuals with autism and other developmental disabilities: A critical review. Research in Autism Spectrum Disorders. 2009;3(3):607–618. doi: 10.1016/j.rasd.2009.01.005. [DOI] [Google Scholar]
- LeBlanc LA, Carr JE, Crossett SE, Bennett CM, Detweiler DD. Intensive outpatient behavioral treatment of primary urinary incontinence of children with autism. Focus on Autism and Other Developmental Disabilities. 2005;20(2):98–105. doi: 10.1177/10883576050200020601. [DOI] [Google Scholar]
- Ledford J, Lane JD, Barton EE. Methods for teaching in early education. London: Routledge; 2019. [Google Scholar]
- MacDuff GS, Krantz PJ, McClannahan LE. Teaching children with autism to use photographic activity schedules: Maintenance and generalization of complex response chains. Journal of Applied Behavior Analysis. 1993;26:89–97. doi: 10.1901/jaba.1993.26-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matson JL, Issarraras A. Handbook of intellectual disabilities. Cham: Springer; 2019. Incontinence; pp. 1093–1103. [Google Scholar]
- McDonnell J, Ferguson B. A comparison of time delay and decreasing prompt hierarchy strategies in teaching banking skills to students with moderate handicaps. Journal of Applied Behavior Analysis. 1989;22:85–91. doi: 10.1901/jaba.1989.22-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niemczyk J, Wagner C, Von Gontard A. Incontinence in autism spectrum disorder: A systematic review. European Child & Adolescent Psychiatry. 2018;27(12):1523–1537. doi: 10.1007/s00787-017-1062-3. [DOI] [PubMed] [Google Scholar]
- Perez BC, Bacotti JK, Peters KP, Vollmer TR. An extension of commonly used toilet-training procedures to children with autism spectrum disorder. Journal of Applied Behavior Analysis. 2020 doi: 10.1002/jaba.727. [DOI] [PubMed] [Google Scholar]
- Richmond G. Shaping bladder and bowel continence in developmentally retarded preschool children. Journal of Autism and Developmental Disorders. 1983;13(2):197–204. doi: 10.1007/BF01531819. [DOI] [PubMed] [Google Scholar]
- Sadler OW, Merkert F. Evaluating the Foxx and Azrin toilet training procedure for retarded children in a day training center. Behavior Therapy. 1977;8:499–500. doi: 10.1016/S0005-7894(77)80093-2. [DOI] [Google Scholar]
- Sansosti JM, Sansosti FJ. Inclusion for students with high-functioning autism spectrum disorders: Definitions and decision making. Psychology in the Schools. 2012;49:917–931. doi: 10.1002/pits.21652. [DOI] [Google Scholar]
- Sapi MC, Vasconcelos JS, Silva FG, Damiao R, da Silva EA. Assessment of domestic violence against children and adolescents with enuresis. Journal of Pediatrics. 2009;85:433–437. doi: 10.2223/JPED.1935. [DOI] [PubMed] [Google Scholar]
- Schum TR, Kolb TM, McAuliffe TL, Simms MD, Underhill RL, Lewis M. Sequential acquisition of toilet-training skills: A descriptive study of gender and age differences in normal children. Pediatrics. 2002;109(3):e48–e48. doi: 10.1542/peds.109.3.e48. [DOI] [PubMed] [Google Scholar]
- Singh BK, Masey H, Morton R. Levels of continence in children with cerebral palsy. Pediatric Nursing. 2006;18(4):23. doi: 10.7748/paed.18.4.23.s17. [DOI] [PubMed] [Google Scholar]
- Smith LE, Maenner MJ, Seltzer MM. Developmental trajectories in adolescents and adults with autism: The case of daily living skills. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(6):622–631. doi: 10.1016/j.jaac.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadtler AC, Gorski PA, Brazelton TB. Toilet training methods, clinical interventions, and recommendations. Pediatrics. 1999;103(Supplement 3):1359–1361. [PubMed] [Google Scholar]
- Stokes TF, Osnes PG. An operant pursuit of generalization. Behavior Therapy. 1989;20(3):337–355. doi: 10.1016/S0005-7894(89)80054-1. [DOI] [PubMed] [Google Scholar]
- Sundberg ML. Verbal behavior milestones assessment and placement program-guide. Concord: AVB Press; 2008. [Google Scholar]
- Von Gontard A. Urinary incontinence in children with special needs. Nature Reviews Urology. 2013;10(11):667. doi: 10.1038/nrurol.2013.213. [DOI] [PubMed] [Google Scholar]
- Watson PJ, Workman EA. The nonconcurrent multiple baseline across-individuals design: An extension of the traditional multiple baseline design. Journal of Behavior Therapy and Experimental Psychiatry. 1981;12:257–259. doi: 10.1016/0005-7916(81)90055-0. [DOI] [PubMed] [Google Scholar]
- Wheeler M. Toilet training for individuals with autism or other developmental issues: A comprehensive guide for parents & teachers. Arlington: Future Horizons; 2007. [Google Scholar]