Abstract
Background and Purpose
Identifying changes in the prevalence, disability, and management patterns of migraine is important for reducing the burden of this disease. However, data on the changes in these variables are scarce.
Methods
We compared data obtained in the 2009 Korean Headache Survey and the 2018 Korean Sleep-Headache Survey.
Results
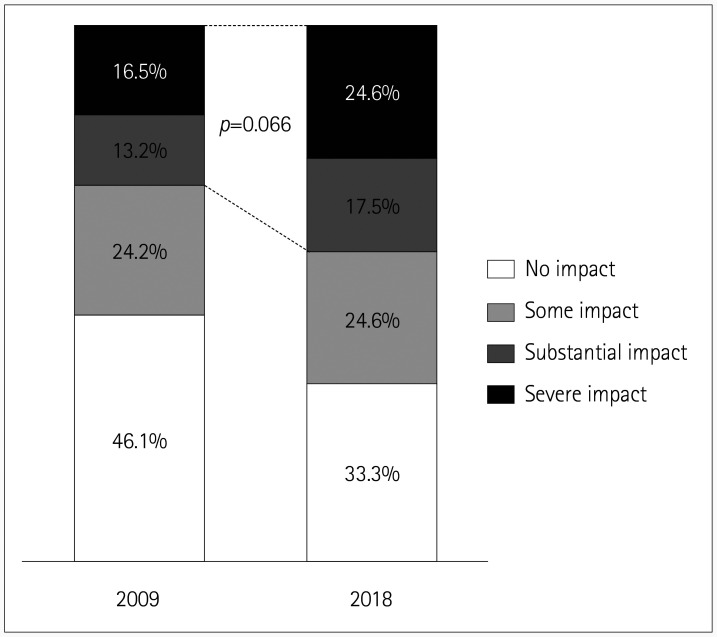
The 1-year migraine prevalence did not differ significantly between 2018 and 2009 [5.2% (114/2,200) vs. 6.0% (91/1,507), p=0.492]. The number of days with missed activity due to headache during the previous 3 months was larger in the 2018 survey than in the 2009 survey [1.1±2.9 vs. 0.3±1.0 days (mean±standard deviation), p=0.013]. The number of days with reduced productivity during the previous 3 months did not differ significantly between the two surveys (0.8±2.8 vs. 1.4±1.4 days, p=0.679). The proportion of subjects with a substantial-to-severe headache impact (Headache Impact Test-6 score ≥56) was marginally larger in the 2018 survey than in the 2009 survey [42.1% (48/114) vs. 29.7% (27/91), p=0.066]. The rate of lifetime medical consultations did not differ between the 2018 and 2009 surveys [34.2% (39/114) vs. 30.8% (28/91), p=0.615].
Conclusions
Migraine prevalence was stable over the 9-year period between the surveys, but disability due to missed activity was greater in 2018 than in 2009 in Korea.
Keywords: migraine, prevalence, disability evaluation, epidemiology, headache
INTRODUCTION
Migraine is a highly prevalent neurological disorder that imposes a large burden on the general public. Individuals with migraine may experience various types of disability, such as absenteeism or decreased productivity at work, school, and in the household.1 Although migraine was found to be the second cause of disability among 328 disorders in the Global Burden of Diseases studies performed in 1990, 2006, and 2016, its prevalence and disability have changed considerably over time.2,3 Its prevalence and the associated disability are the two most important factors that determine the burden of migraine, and so estimating changes in these parameters could be useful for developing strategies to reduce the burden of migraine.
Some studies have provided serial data on the prevalence of migraine in the same population,4,5,6,7,8 but the findings have varied. The migraine prevalence has generally been found to be stable, but some studies have found significant changes over time. The use of comparable methodologies is required to reliably compare prevalence between surveys. To date, only a few studies have replicated surveys of the prevalence of migraine using comparable methodologies. Furthermore, even fewer studies have examined serial changes in disability or the impact of headaches caused by migraine, along with its prevalence.6,7
Advances in the diagnosis and treatment of migraine have provided opportunities to reduce its burden. Previous studies have revealed that migraine has historically been underdiagnosed and undertreated.4 Recent studies on migraine management found increases in medical consultations and changes in treatment patterns.4,9 Nevertheless, most of these studies were conducted in North American and European countries, and data from other regions are scarce.
The enormous burden of migraine makes reducing migraine-related disability an urgent public health concern. Identifying the cumulative effects and pattern of changes in migraine-related disability will lead to a better understanding of this debilitating disorder. A better understanding of migraine-related disability will enable medical professionals to provide migraine patients with coping mechanisms to reduce their migraine-related disability.10
The Korean Headache Survey in 2009 and the Korean Sleep-Headache Survey in 2018 provided an opportunity to investigate changes in the prevalence, disability, and management patterns of migraine over a 9-year timespan. Both surveys used the same strategies for assessing migraine prevalence, the disability and impact of headache, medical consultations, and treatment patterns, and adopted a two-stage clustered random sampling method, although they differed in their target sample numbers. We compared the data from these surveys based on the hypothesis that these factors did not differ between 2009 and 2018 in Korea. The aim of the present study was to determine the changes in the prevalence, disability, medical consultations, and treatment patterns of migraine between 2009 and 2018.
METHODS
Korean Headache Survey in 2009
The Korean Headache Survey in 2009 was a nationwide, cross-sectional survey of primary headaches, including migraine. We have previously described the sampling and survey processes.11,12 In brief, we used a two-stage cluster random sampling method proportional to the population distribution of all Korean territories except Jeju-do, based on data from the 2005 population and the housing census performed by the National Statistical Office.13 Korea is geographically divided into 15 administrative divisions, which were designated as primary sampling units. In the second stage, we further selected representative basic administrative units from each primary sampling unit. Overall, 60 representative basic administrative units were selected for inclusion in this study. For each representative basic administrative unit, we assigned a target sample size based on age, sex, and education level. The target sample size was 1,500 and the estimated sampling error was ≤2.5%.
The survey was conducted by door-to-door visits and face-to-face interviews with questionnaires among adults aged 19–69 years. The interviewers were not medical personnel and had previous experience of performing social surveys. All interviewers were employees of Gallup Korea (Seoul, Korea). The questionnaire was designed to assess demographic characteristics, headache profiles, headache diagnoses, use of medical services, medical consultations, disability from headache, and impact of headache. The Korean Headache Survey was performed in March 2009 in accordance with the ethical guidelines of the Council for International Organizations of Medical Sciences and the principles in the Declaration of Helsinki.14 Written informed consent was obtained from all participants before the survey.
Korean Sleep-Headache Survey in 2018
The Korean Sleep-Headache Survey in 2018 was also a nationwide, cross-sectional survey of primary headaches. The sampling and survey processes were the same as those in the 2009 survey, with only the target sample number differing. Two-stage clustered random sampling was performed based on the data from the 2017 population and housing census conducted by the National Statistical Office of Korea.13 The target sample size in the 2018 survey was 2,500 adults aged 19 years or older, and the estimated sampling error was ≤1.9%. We selected the data of 2,200 adults aged 19–69 years from the 2018 survey to match the age group in the 2009 survey. The representativeness of our sample was assessed by comparing demographic distributions between our samples and the total population of Korea in 2018 (Supplementary Table 1 in the online-only Data Supplement).
Like for the 2009 survey, the 2018 survey was conducted by Gallup Korea through door-to-door visits and face-to-face interviews using a questionnaire. The questionnaire items for evaluating the disability from headache, impact of headache, medical consultations, and treatment pattern were the same as those in 2009 survey. The 2018 survey was approved by the Institutional Review Board of Severance Hospital, Yonsei University (Approval No. 2018-1269-001). The present study was approved by the Institutional Review Board of Severance Hospital, Yonsei University (Approval No. 2019-1721-001). Written informed consents were obtained from all participants before the surveys.
Diagnosis, impact, disability, and management patterns of migraine
Migraine was diagnosed based on the diagnostic criteria for migraine without aura in the second edition of the International Classification of Headache Disorders (code 1.1), which was the valid scale at the time of the surveys.15 We did not assess the presence of aura because it this is very difficult to evaluate in an epidemiological study.16 Therefore, “migraine” herein includes migraine with and without aura as reported in the 2009 and 2018 surveys. The diagnostic validity of our questionnaire has been previously reported.11 If a participant responded positively to the question “Did you have headache during the previous year?” and their headache fulfilled the criteria of migraine, we classified them as a case of migraine.
The impact of headache was investigated using the Headache Impact Test-6 (HIT-6). We classified the impact of headache based on the HIT-6 score as follows: <50, little or no impact; 50–55, some impact; 56–59, substantial impact; and ≥60, severe impact.17,18
Disability from migraine was assessed using the following two questions: 1) “On how many days in the last 3 months did you miss work, school, or housework because of your headaches?” and 2) “On how many days in the last 3 months was your productivity for work, school, or housework reduced by half or more because of your headaches? (Do not include days you counted in the question about missing work, school, or housework).”
Lifetime medical consultations for headache were evaluated using the question “Did you ever visit a doctor for your headaches?” If the participant responded positively, they were classified as having lifetime medical consultations for headache. Treatment patterns for headache were assessed using the question “How are you treating your headaches? Please select all treatments you have used in the past year: 1) no treatment, 2) treatment with over-the-counter (OTC) medications, 3) visiting traditional Korean medical clinics, 4) alternative methods other than traditional medicine, and 5) visiting clinics or hospitals.”
Statistical analyses
The primary analysis performed in this study was comparing the variables between the 2009 survey and 2018 survey. The 1-year prevalence of migraine was compared between the 2009 survey and 2018 survey as the number of cases per 100 persons. Binary and ordinal variables are presented as numbers and percentages, while interval variables are represented as mean±standard-deviation or median and interquartile- range values, as appropriate. The normality of the ratio of variables was tested using the Kolmogorov-Smirnov test. Independent two-tailed t-tests or one-way analyses of variance were used for intergroup comparisons of variables that conformed to a normal distribution. Two-tailed Mann-Whitney U tests or Kruskal-Wallis tests were used for variables that did not conform to a normal distribution.
Since the prevalence of and disability from migraine varied significantly according to sex and age, we compared data between the 2009 survey and 2018 survey while adjusting for these variables.3,19 The categorical variables were compared between the 2009 survey and 2018 survey using logistic regression analyses while adjusting for age (in years, as a continuous variable) and sex. Linear regression analyses while adjusting for age and sex were used for comparing numerical variables between the surveys. The Statistical Package for Social Sciences (version 24.0, IBM, Armonk, NY, USA) was used for all statistical analyses. The criterion for statistical significance was set as p<0.05.
We used the weighted values of participants based on clustered sampling processes in the analyses. Weighted values were determined by dividing the actual number of participants by the number of target samples allocated at each survey unit. As with most survey studies, there were missing data due to nonresponses for several variables. The reported data are based on the available data; imputation techniques were not employed in order to minimize any effects of nonresponses.20
RESULTS
Sample and survey
The 2009 and 2018 surveys were completed by 1,507 and 2,200 individuals aged 19–69 years, respectively. The sex and age distributions of our samples in 2009 and 2018 did not differ significantly from those in the total Korean populations in 2009 and 2018 (Supplementary Table 1 in the onlineonly Data Supplement). All participants aged 19–69 years in the 2009 and 2018 surveys reported headache characteristics and accompanying symptoms, and so we could diagnose all migraine cases that met the diagnostic criteria.
Migraine prevalence
In the 2009 survey, 91 respondents [6.0%, 95% confidence interval (CI)=4.8–7.2%] were classified as having migraine, while 114 respondents (5.2%, 95% CI=4.1–5.9%) were classified as having migraine. in the 2018 survey. The migraine prevalence did not differ significantly between the two surveys (p=0.492).
Clinical characteristics of migraine
The monthly headache frequency and the score for the headache intensity on a visual analogue scale did not differ significantly between the surveys. Unilateral pain, pulsating quality, and vomiting were more prevalent in 2018 than in 2009, while aggravation by movement was more prevalent in 2009 (Table 1).
Table 1. Clinical characteristics of individuals with migraine in the 2009 Korean Headache Survey and the 2018 Korean Sleep-Headache Survey.
| 2009 (n=91) | 2018 (n=114) | p† | |
|---|---|---|---|
| Age, years | 41.8±11.2 | 43.1±12.8 | 0.465 |
| Monthly headache frequency | 1.0 [0.4–4.0] | 0.8 [0.3–3.0] | 0.583 |
| Headache severity, VAS score | 6.0 [5.0–7.0] | 6.0 [5.0–7.0] | 0.747 |
| Headache intensity | |||
| Mild | 20 (22.0) | 19 (16.7) | 0.336* |
| Moderate | 58 (63.7) | 73 (64.0) | |
| Severe | 13 (14.3) | 22 (19.3) | |
| Unilateral location | 50 (54.9) | 78 (60.9) | 0.529 |
| Pulsating quality | 51 (56.0) | 89 (78.1) | 0.365 |
| Aggravation during routine physical activity | 62 (68.1) | 56 (49.1) | 0.005 |
| Nausea | 82 (90.1) | 102 (89.5) | 0.784 |
| Vomiting | 28 (30.8) | 52 (45.6) | 0.028 |
| Photophobia | 41 (45.1) | 44 (38.6) | 0.330 |
| Phonophobia | 54 (59.3) | 63 (55.3) | 0.737 |
| Osmophobia | 47 (51.6) | 45 (39.5) | 0.104 |
Data are mean±standard-deviation, median [interquartile range], or n (%) values.
*Comparison of the proportion with moderate-to-severe headache intensity, †Categorical variables were compared using linear regression analyses while adjusting for sex and age (in years, as a continuous variable), and numerical variables were compared using logistic regression analyses while adjusting for age and sex.
VAS: visual analogue scale.
Impact of headache among individuals with migraine
The proportion of subjects with a substantial-to-severe headache impact (HIT-6 score ≥56) was marginally larger in the 2018 survey than in the 2009 survey [42.1% (48/114) vs. 29.7% (27/91), p=0.066] (Fig. 1).
Fig. 1. Impact of headache as assessed using the HIT-6 among individuals with migraine in the 2009 Korean Headache Survey and the 2018 Korean Sleep-Headache Survey. HIT-6 scores: little to no impact, <50; some impact, 50–55; substantial impact, 56–59; severe impact, ≥60. HIT-6: Headache Impact Test-6.
Disability from headache among individuals with migraine
In the 2009 survey, 11.0% (10/91) of individuals with migraine reported that they had missed activity at work, school, or in the household during the previous 3 months because of headaches. Missed activity occurred on 0.3±1.0 days, while reduced productivity occurred on 1.4±1.4 days.
In the 2018 survey there were 1.1±2.9 days of missed activity among the individuals with migraine, while there were 0.8±2.8 days with reduced activity. The number of days with missed activity was significantly larger in the 2018 survey than in the 2009 survey (p=0.013). The number of days with reduced productivity did not differ significantly between the two surveys (p=0.679) (Table 2).
Table 2. Headache-related disability of individuals with migraine in the 2009 Korean Headache Survey and the 2018 Korean Sleep-Headache Survey.
| 2009 (n=91) | 2018 (n=114) | p‡ | |
|---|---|---|---|
| Missed activity (days/3 months) | |||
| 0 | 80 (87.9) | 77 (67.5) | 0.001† |
| 1–2 | 5 (5.5) | 27 (23.7) | |
| 3–5 | 5 (5.5) | 5 (4.4) | |
| ≥6 | 0 (0.0) | 5 (4.4) | |
| No response | 1 (1.1) | 0 (0.0) | |
| Duration | 0.3±1.0 | 1.1±2.9 | 0.013* |
| Reduced productivity (days/3 months) | |||
| 0 | 67 (73.6) | 92 (80.7) | 0.228† |
| 1–2 | 11 (12.1) | 12 (10.5) | |
| 3–5 | 10 (11.0) | 8 (7.0) | |
| ≥6 | 0 (0.0) | 2 (1.8) | |
| No response | 3 (3.3) | 0 (0.0) | |
| Duration | 1.4±1.4 | 0.8±2.8 | 0.679* |
Data are n (%) or mean±standard-deviation values.
*Compared using linear regression analyses while adjusting for sex and age (in years, as a continuous variable), †Comparison of the proportion of having missed activity or fewer productivity days using logistic regression analyses while adjusting for age and sex, ‡Three individuals with migraine did not report the number of days with missed activity, and one individual with migraine did not report the number of days with reduced activity in the 2009 survey. All individuals with migraine reported the number of days with missed activity and reduced activity in the 2018 survey.
Medical consultations and treatment patterns
Lifetime medical consultations for headache were reported by 30.8% (28/91) and 34.2% (39/114) of individuals with migraine in the 2009 and 2018 surveys, respectively (p=0.615).
The treatment patterns of the migraine participants are summarized in Table 3. The proportions of patients with no treatment, treatment with OTC medications, treatment at traditional Korean medical clinics, treatment by alternative medicine other than traditional Korean medicine, and treatment by visiting clinics or hospitals did not differ significantly between the 2009 survey and 2018 survey.
Table 3. Headache treatment patterns among individuals with migraine in the 2009 Korean Headache Survey and the 2018 Korean Sleep-Headache Survey.
| 2009 (n=91) | 2018 (n=114) | p | |
|---|---|---|---|
| No treatment | 29 (33.0) | 30 (26.3) | 0.298 |
| OTC medications | 47 (50.0) | 62 (54.4) | 0.533 |
| Traditional Korean medical clinic | 3 (3.3) | 4 (3.5) | 1.000 |
| Alternative medicine | 0 (0.0) | 4 (3.5) | 0.131 |
| Clinics or hospitals | 17 (19.8) | 20 (17.5) | 0.682 |
Data are n (%) values.
OTC: over-the-counter.
DISCUSSION
This study compared survey data from 2009 and 2018 with the aim of identifying changes in migraine prevalence, disability, impact, and treatment in Korea. We found that 1) the migraine prevalence did not differ significantly between the 2009 survey and 2018 survey, 2) disability due to missed activity was more common in 2018 than in 2009, whereas there was no significant difference in disability due to decreased productivity, and 3) there was no significant change in medical consultations or treatment patterns over the 9-year study period.
Several studies have examined the serial 1-year prevalence of migraine, and most studies involving adult populations have found this to be stable. Four nationwide surveys of the USA population aged 12 years or older showed that the migraine prevalence was stable over a 23-year period: 12% in 1989, 13% in 2001, 12% in 2005, and 14% in 2012.5,21,22,23 A Danish study of people aged 25–36 years similarly found a stable migraine prevalence over a 12-year period: 11% in 1989 and 15% in 2001.8 However, divergent results have been obtained among adolescents. A Norwegian study of adolescents demonstrated stable migraine prevalence over a 4-year period (7.2% in 1997 and 8.5% in 2001),24 whereas one in Taiwan found that the migraine prevalence increased significant over a 2-year period, from 5.2% to 7.4%. The present study included an adult population aged 19–69 years and showed a stable 1-year migraine prevalence over a 9-year period, indicating that the data obtained in the two analyzed surveys are reliable.
Some studies have evaluated longitudinal changes in headache-related disability in individuals with migraine, and found small changes over time. The American Migraine Prevalence and Prevention (AMPP) study in 2004 and the Chronic Migraine Epidemiology and Outcomes (CaMEO) study in 2012 were nationwide studies conducted in the USA that adopted the same headache classification strategies and headache-disability assessment instrument [Migraine Disability Assessment (MIDAS)]. The proportion of subjects with moderate-to-severe disability (MIDAS score >10) increased slightly over 8 years among those with episodic migraine (AMPP: 23.0% of males and 31.8% of females; CaMEO: 26.7% of males and 37.9% of females) and those with chronic migraine (AMPP: 66.9% of males and 78.9% of females; CaMEO: 71.0% of males and 82.6% of females).25 However, these studies did not analyze differences in headache-related disability. Also, these studies were based in the USA, and longitudinal changes in headache-related disability from migraine have never been reported for other regions. The present study is the first to perform statistical analyses of differences in disability and identify longitudinal changes in headache-related disability in individuals with migraine in Asia, which accounts for more than half of the world's population.
We found that disability due to missed activity was more common in the 2018 survey than in the 2009 survey, whereas the prevalence of disability due to decreased productivity did not differ significantly between the two surveys. Considering that missed activity represents a greater loss than decreased productivity, the overall disability from migraine might have been greater in 2018 than in 2009. The underlying reasons for the changes observed in headache-related disability in individuals with migraine remain unknown. The present study found that the prevalence and clinical features of migraines did not differ significantly over the 9-year study period. These findings suggest that increased migraine-related disability can be attributed to changes in sociodemographic factors rather than changes in the prevalence or clinical features of migraine.
The per-capita gross domestic product in Korea increased by 171% from 2009 to 2018 (18,299 USD in 2009 and 31,370 USD in 2018).26 Such economic growth can lead to social change, which may increase the awareness of disability from headache. The Global Burden of Disease (GBD) study performed in 2015 found that the burden of migraine (quantified as disability-adjusted life years) increased with the sociodemographic index.3 Another study found that disability from migraine is greater in high-income countries than in low-income countries.27
Another possible explanation is changes in the population composition. The mean age of the Korean population was 37.4 years in 2009, which increased to 41.7 years in 2018,28 and this could affect disability from migraine. The GBD study in 2015 found that the global number of years of life lived with disability from migraine was largest among those aged 40–45 years.3 The two survey samples assessed in the present study showed different age distributions, which reflected the change in the composition of the population over the 9-year study period (Supplementary Table 1 in the online-only Data Supplement). The increase in the mean age resulted in more participants with migraine being in their 40s, which might have increased the prevalence of disability. The mean age of individuals with migraine in the 2018 survey was numerically higher than that in the 2009 survey, although the difference was not statistically significant (Table 1). The small number of individuals with migraine is a possible reason for the lack of a statistical difference, and so further studies with larger samples may clarify the association between age and migraine-related disability. The present study was designed to compare the prevalence of and disability from migraine between the 2009 survey and 2018 survey conducted in Korea, and so we did not adjust for age when comparing the migraine prevalence between the two surveys.
Temporal increases in medical consultations for migraine have been found in previous studies. For example, the rate of medical consultations for migraine in the USA was 16% in 1984, 47% in 1999,4,29 and 80% in 2016.9 Although not significantly different, the rate of medical consultations for migraine was higher in our 2018 survey than in the 2009 survey. Medical consultations can be affected by efforts of relevant organizations for disease recognition, socioeconomic status, and the medical system. The Korean Headache Society (KHS) was founded in 1999. The KHS conducted a campaign to increase the awareness of distress, disability, and treatment of migraine in 2015 using public lectures, broadcasting, social network services, web pages, and other types of media.30 At the time of the 2018 survey (i.e., only 3 years after the start of the KHS campaign), there was no major change in the rate of medical consultations. However, we expect further increases in medical consultations for migraine, which may lead to increases in the rates of diagnosing and treating migraine, which may ultimately reduce the burden of migraine.31
The Korean government implemented a National Health Insurance system for all citizens in 1989. However, the accessibility of hospitals is partly affected by economic status due to the need to make visit copayments, and so the economic status of individuals could influence whether they seek medical consultations.32 Recent improvements in the economic status in Korea could increase the number of medical consultations.
The 1-year migraine prevalence rates in Korea in the 2009 and 2018 surveys were 6.0% and 5.2%, respectively, which are lower than those reported for European (10–25%) and North American (9–16%) countries.33 The 1-year prevalence of migraine in Asian countries has been reported to range between 4.7% and 9.1%.34 Therefore, the prevalence of migraine in Korea found in the present study was similar to those reported for other Asian countries. Possible reasons for the migraine prevalence being lower in Asian countries are the low rate of obesity, dietary factors, and ethnicity differences. Obesity has been associated with a higher migraine prevalence,35 and the prevalence of obesity is lower in Asian countries than in Western countries.36 Moreover, a low-fat diet was found to reduce the severity of migraine, and the dietary fat consumption is lower in Asian than Western countries.37,38 Finally, a lower migraine prevalence among Asian communities compared with other global ethnic groups has been consistently reported in the USA.39
Most of the headache characteristics and accompanying symptoms in individuals with migraine were similar in the two surveys. However, a unilateral location, pulsating quality, and vomiting were more prevalent in the 2018 survey, whereas aggravation during routine physical activity was more prevalent in the 2009 survey. We assessed these features using the same questions and adopted a two-stage clustered random sampling method when analyzing both surveys. There had been no major change in language use in Korea between 2009 and 2018, and so it is difficult to identify exactly why these features changed significantly over the 9-year study period.
Migraine aura reportedly affects approximately 30% of individuals with migraine,40 and it differs in terms of triggering factors, female-to-male ratio, and comorbidity profiles.40,41,42,43 Although migraine aura is a distinct subtype of migraine, inadequate epidemiological data on migraine with aura were available owing to difficulties in evaluating this condition in population-based studies.9 At the time of the initial survey in 2009, there was no valid instrument for assessing aura symptoms, and the survey did not include questions regarding aura symptoms. We therefore could not compare aura symptoms between the two surveys. In the future we plan to conduct epidemiological studies on prevalence, comorbidities, and migraine-related disability using a valid instrument for assessing migraine with aura.
Migraine-related disability is affected by various comorbidities.44 Psychiatric comorbidities such as anxiety and depression are common in migraine patients and are associated with severe migraine-related disability.45 Fibromyalgia (FM) is a chronic pain condition that is common among migraine patients. The MIDAS score (reflecting the degree of migraine-related disability) was found to be higher in migraine patients with FM that in those without FM.46 However, the 2009 survey analyzed in the present study focused on the prevalence of and disability from headache, and did not include questions allowing the identification of comorbidities such as anxiety, depression, and FM. This meant that we could not compare the factors associated with migraine-related disability between the two surveys. Identifying the factors affecting migraine-related disability is important for reducing the burden of migraine, and these factors may vary with the socioeconomic status.47 Further studies identifying the factors associated with migraine-related disability are needed in Korea.
The present study had several limitations. First, although this study used data from two nationwide surveys with large samples that were consistent with the population distribution in Korea, the smallness of the samples in some of the subgroups could have negatively affected the analyses. Second, we did not analyze the use of migraine-specific medications and preventive treatment. Triptans and ergot derivatives are migraine-specific medications that are effective at treating migraine attacks. Preventive treatment can reduce the occurrence of migraine attacks. Migraine-specific medications and preventive treatment can be more effective at reducing the burden of migraine than analgesic treatment alone. Third, the cooperation rate in the 2009 survey was 37.2%, and we did not evaluate the cooperation rate in the 2018 survey.12 Nevertheless, we used a similar two-stage clustered random sampling method in both surveys. We assume that the cooperation rate in the 2018 survey would have been similar to that in the 2009 survey. The age and sex distributions in the 2009 and 2018 surveys were similar to those in the total population of Korea, and it was estimated that the sampling errors were low for both surveys. Furthermore, the 1-year prevalence of migraine in the present study was similar to the prevalence rates found in previous studies performed in Asian countries.34 Therefore, we can assume that the 2009 and 2018 surveys employed valid sampling techniques. Fourth, we used two questions to assess migraine-related disability regarding missed activity and decreased productivity at work, school, or in the household. The MIDAS is a widely used instrument for the measurement of disability from migraine that comprises five items: 1) missed days at work or school, 2) decreased productivity days at work or school, 3) missed days for housework, 4) decreased productivity days for housework, and 5) missed days for family, social, or leisure activities during the previous 3 months.48,49 Thus, our two questions related to disability assessment encompassed four items of the MIDAS. Although we did not assess migraine-related disability in family, social, or leisure activities, the present study could compare disability levels during work, school, and housework between 2009 and 2018.
Notwithstanding the above limitations, the present study had several strengths. First, we used data from two nationwide surveys and found that the migraine prevalence was stable over 9 years, while disability from migraine increased. Several studies have found longitudinal changes in disability from migraine, but those studies did not analyze the changes in disability.25 The present study is the first to show a significant increase in disability from migraine over time. Second, we assessed migraine symptoms in addition to its prevalence, impact, and migraine-related disability. We found that migraine- related disability was greater in the 2018 survey despite migraine symptoms being similar in the 2009 and 2018 surveys.5,21,25 Third, most studies investigating changes in migraine prevalence and disability have been conducted in North American and European countries, and there have been very few studies of changes in migraine prevalence and disability in other regions. The present study is the first to investigate changes in the prevalence of and disability from migraine in Korea; this is an important distinction, since the prevalence and symptoms of migraine in Asian countries differ somewhat from those in Western countries.34
In conclusion, we have analyzed data from two nationwide population-based surveys on the prevalence, disability, and impact of migraine as well as migraine-related medical consultations and treatment patterns in 2009 and 2018. The two surveys used similar sampling processes and the same evaluation strategies, and these have demonstrated that the prevalence of migraine was stable, whereas the level of migraine-related disability due to missed activity was higher in 2018 than in 2009. The measured rate of medical consultations was also higher in the 2018 survey than the 2009 survey, but this difference was not statistically significant. Treatment patterns did not differ significantly between the two surveys.
The data and conclusions presented here can be used to improve the detection and treatment of migraine worldwide, especially to increase public awareness about its prevalence and treatment outcomes.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (2019R1F1A10 53841).
Footnotes
- Conceptualization: Kyung Min Kim, Soo-Jin Cho, Min Kyung Chu.
- Data Curation: Kwang Ik Yang, Daeyoung Kim, Chang-Ho Yun, Min Kyung Chu.
- Formal analysis: Kyung Min Kim, Soo-Jin Cho, Min Kyung Chu, Hye Jung Shin.
- Funding acquisition: Min Kyung Chu.
- Investigation: Kwang Ik Yang, Daeyoung Kim, Chang-Ho Yun, Min Kyung Chu.
- Writing—original draft: Kyung Min Kim, Soo-Jin Cho, Min Kyung Chu.
- Writing—review & editing: Kyung Min Kim, Min Kyung Chu.
Conflicts of Interest: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: SJC was involved as a site investigator of a multicenter trial sponsored by Otsuka Korea, Eli Lilly and Company, and Novartis and worked as an advisory member for Teva, and received research support from Hallym University Research Fund 2016 and a grant from Korean Neurological Association (KNA-16-MI-09). MKC was a site investigator for a multicenter trial sponsored by Otsuka Korea, Novartis International AG, and Eli Lilly and Company. He worked as an advisory member for Teva, and received lecture honoraria from Allergan Korea, Handok-Teva, and Yuyu Pharmaceutical Company in the past 24 months. He received grants from Yonsei University College of Medicine (2018-32-0037) and National Research Foundation of Korea (2019R1F1A1053841). The other authors have no potential conflicts of interest to disclose.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.3988/jcn.2021.17.1.77.
Sociodemographic distributions of survey participants, the total Korean population, and cases identified as migraine in the 2009 Korean Headache Survey and the 2018 Korean Sleep-Headache Survey
References
- 1.Leonardi M, Raggi A. A narrative review on the burden of migraine: when the burden is the impact on people's life. J Headache Pain. 2019;20:41. doi: 10.1186/s10194-019-0993-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211–1259. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:954–976. doi: 10.1016/S1474-4422(18)30322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lipton RB, Stewart WF, Simon D. Medical consultation for migraine: results from the American Migraine Study. Headache. 1998;38:87–96. doi: 10.1046/j.1526-4610.1998.3802087.x. [DOI] [PubMed] [Google Scholar]
- 5.Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache. 2001;41:646–657. doi: 10.1046/j.1526-4610.2001.041007646.x. [DOI] [PubMed] [Google Scholar]
- 6.Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF AMPP Advisory Group. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343–349. doi: 10.1212/01.wnl.0000252808.97649.21. [DOI] [PubMed] [Google Scholar]
- 7.Buse DC, Fanning KM, Reed ML, Murray S, Dumas PK, Adams AM, et al. Life with migraine: effects on relationships, career, and finances from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study. Headache. 2019;59:1286–1299. doi: 10.1111/head.13613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lyngberg AC, Rasmussen BK, Jørgensen T, Jensen R. Has the prevalence of migraine and tension-type headache changed over a 12-year period? A Danish population survey. Eur J Epidemiol. 2005;20:243–249. doi: 10.1007/s10654-004-6519-2. [DOI] [PubMed] [Google Scholar]
- 9.Lipton RB, Munjal S, Alam A, Buse DC, Fanning KM, Reed ML, et al. Migraine in America Symptoms and Treatment (MAST) study: baseline study methods, treatment patterns, and gender differences. Headache. 2018;58:1408–1426. doi: 10.1111/head.13407. [DOI] [PubMed] [Google Scholar]
- 10.Lipton RB, Bigal ME. Ten lessons on the epidemiology of migraine. Headache. 2007;47 Suppl 1:S2–S9. doi: 10.1111/j.1526-4610.2007.00671.x. [DOI] [PubMed] [Google Scholar]
- 11.Kim BK, Chu MK, Lee TG, Kim JM, Chung CS, Lee KS. Prevalence and impact of migraine and tension-type headache in Korea. J Clin Neurol. 2012;8:204–211. doi: 10.3988/jcn.2012.8.3.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim BK, Chung YK, Kim JM, Lee KS, Chu MK. Prevalence, clinical characteristics and disability of migraine and probable migraine: a nationwide population-based survey in Korea. Cephalalgia. 2013;33:1106–1116. doi: 10.1177/0333102413484990. [DOI] [PubMed] [Google Scholar]
- 13.Korean Statistical Information Service. Statistical database, population, households and housing units [Internet] Daejeon: Korean Statistical Information Service; 2005. [cited 2019 Sep 23]. Available from: http://kosis.kr/eng/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ETITLE&parmTabId=M_01_01&statId=1962001&themaId=#SelectStatsBoxDiv. [Google Scholar]
- 14.Council for International Organizations of Medical Sciences. International ethical guidelines for biomedical research involving human subjects. Bull Med Ethics. 2002:17–23. [PubMed] [Google Scholar]
- 15.Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24 Suppl 1:9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 16.Stang PE, Osterhaus JT. Impact of migraine in the United States: data from the national health interview survey. Headache. 1993;33:29–35. doi: 10.1111/j.1526-4610.1993.hed3301029.x. [DOI] [PubMed] [Google Scholar]
- 17.Yang M, Rendas-Baum R, Varon SF, Kosinski M. Validation of the Headache Impact Test (HIT-6™) across episodic and chronic migraine. Cephalalgia. 2011;31:357–367. doi: 10.1177/0333102410379890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chu MK, Im HJ, Ju YS, Yu KH, Ma HI, Kim YJ, et al. Validity and reliability assessment of Korean Headache Impact Test-6 (HIT-6) J Korean Neurol Assoc. 2009;27:1–6. [Google Scholar]
- 19.Buse DC, Loder EW, Gorman JA, Stewart WF, Reed ML, Fanning KM, et al. Sex differences in the prevalence, symptoms, and associated features of migraine, probable migraine and other severe headache: results of the American Migraine Prevalence and Prevention (AMPP) study. Headache. 2013;53:1278–1299. doi: 10.1111/head.12150. [DOI] [PubMed] [Google Scholar]
- 20.Little RJ, Rubin DB. Statistical analysis with missing data. 3rd ed. Hoboken, NJ: John Wiley & Sons; 2019. [Google Scholar]
- 21.Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine headache in the United States. Relation to age, income, race, and other sociodemographic factors. JAMA. 1992;267:64–69. [PubMed] [Google Scholar]
- 22.Chu MK, Buse DC, Bigal ME, Serrano D, Lipton RB. Factors associated with triptan use in episodic migraine: results from the American Migraine Prevalence and Prevention Study. Headache. 2012;52:213–223. doi: 10.1111/j.1526-4610.2011.02032.x. [DOI] [PubMed] [Google Scholar]
- 23.Adams AM, Serrano D, Buse DC, Reed ML, Marske V, Fanning KM, et al. The impact of chronic migraine: the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia. 2015;35:563–578. doi: 10.1177/0333102414552532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jacobsena BA, Dyb G, Hagen K, Stovner LJ, Holmen TL, Zwart JA. The Nord-Trøndelag Health Study shows increased prevalence of primary recurrent headaches among adolescents over a four-year period. Scand J Pain. 2018;2:148–152. doi: 10.1016/j.sjpain.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Lipton RB, Manack Adams A, Buse DC, Fanning KM, Reed ML. A comparison of the Chronic Migraine Epidemiology and Outcomes (CaMEO) study and American Migraine Prevalence and Prevention (AMPP) study: demographics and headache-related disability. Headache. 2016;56:1280–1289. doi: 10.1111/head.12878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Korean Statistical Information Service. [National accounts] [Internet] Daejeon: Statistics Korea; 2019. [cited 2019 Oct 19]. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=301&tblId=DT_102Y002&vw_cd=MT_ZTITLE&list_id=301_A_A05_B01&seqNo=&lang_mode=ko&language=kor&obj_var_id=&itm_id=&conn_path=MT_ZTITLE. [Google Scholar]
- 27.World Health Organization. The global burden of disease: 2004 update. Geneva: World Health Organization; 2008. [Google Scholar]
- 28.Korean Statistical Information Service. [Prospective population estimates] [Internet] Daejeon: Statistics Korea; 2019. [cited 2019 Oct 19]. Available from: https://kosis.kr/statHtml/%20statHtml.do?orgId=101&tblId=DT_1BPA002&vw_cd=MT_%20Z%20T%20I%20T%20L%20E%20&%20l%20i%20s%20t%20_%20i%20d%20=%20A%204%201%20_%201%200%20&%20s%20e%20q%20N%20o%20=%20&%20l%20a%20n%20g%20_%20mode=ko&language=kor&obj_var_id=&itm_id=&conn_path=MT_%20ZTITLE. [Google Scholar]
- 29.Lipton RB, Scher AI, Kolodner K, Liberman J, Steiner TJ, Stewart WF. Migraine in the United States: epidemiology and patterns of health care use. Neurology. 2002;58:885–894. doi: 10.1212/wnl.58.6.885. [DOI] [PubMed] [Google Scholar]
- 30.migrainecluster.com [Internet] Seoul: Korea Headache Society; 2015. [cited 2019 Dec 10]. Available from: http://www.migrainecluster.com. [Google Scholar]
- 31.Lipton RB, Amatniek JC, Ferrari MD, Gross M. Migraine. Identifying and removing barriers to care. Neurology. 1994;44:S63–S68. [PubMed] [Google Scholar]
- 32.Lipton RB, Serrano D, Holland S, Fanning KM, Reed ML, Buse DC. Barriers to the diagnosis and treatment of migraine: effects of sex, income, and headache features. Headache. 2013;53:81–92. doi: 10.1111/j.1526-4610.2012.02265.x. [DOI] [PubMed] [Google Scholar]
- 33.Stovner LJ, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27:193–210. doi: 10.1111/j.1468-2982.2007.01288.x. [DOI] [PubMed] [Google Scholar]
- 34.Peng KP, Wang SJ. Epidemiology of headache disorders in the Asiapacific region. Headache. 2014;54:610–618. doi: 10.1111/head.12328. [DOI] [PubMed] [Google Scholar]
- 35.Bigal ME, Liberman JN, Lipton RB. Obesity and migraine: a population study. Neurology. 2006;66:545–550. doi: 10.1212/01.wnl.0000197218.05284.82. [DOI] [PubMed] [Google Scholar]
- 36.Walpole SC, Prieto-Merino D, Edwards P, Cleland J, Stevens G, Roberts I. The weight of nations: an estimation of adult human biomass. BMC Public Health. 2012;12:439. doi: 10.1186/1471-2458-12-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elmadfa I, Kornsteiner M. Dietary fat intake--a global perspective. Ann Nutr Metab. 2009;54:8–14. doi: 10.1159/000220822. [DOI] [PubMed] [Google Scholar]
- 38.Ferrara LA, Pacioni D, Di Fronzo V, Russo BF, Speranza E, Carlino V, et al. Low-lipid diet reduces frequency and severity of acute migraine attacks. Nutr Metab Cardiovasc Dis. 2015;25:370–375. doi: 10.1016/j.numecd.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 39.Stewart WF, Lipton RB, Liberman J. Variation in migraine prevalence by race. Neurology. 1996;47:52–59. doi: 10.1212/wnl.47.1.52. [DOI] [PubMed] [Google Scholar]
- 40.Russell MB, Rasmussen BK, Thorvaldsen P, Olesen J. Prevalence and sex-ratio of the subtypes of migraine. Int J Epidemiol. 1995;24:612–618. doi: 10.1093/ije/24.3.612. [DOI] [PubMed] [Google Scholar]
- 41.Le H, Tfelt-Hansen P, Russell MB, Skytthe A, Kyvik KO, Olesen J. Comorbidity of migraine with somatic disease in a large populationbased study. Cephalalgia. 2011;31:43–64. doi: 10.1177/0333102410373159. [DOI] [PubMed] [Google Scholar]
- 42.Vgontzas A, Burch R. Episodic migraine with and without aura: key differences and implications for pathophysiology, management, and assessing risks. Curr Pain Headache Rep. 2018;22:78. doi: 10.1007/s11916-018-0735-z. [DOI] [PubMed] [Google Scholar]
- 43.Hauge AW, Kirchmann M, Olesen J. Trigger factors in migraine with aura. Cephalalgia. 2010;30:346–353. doi: 10.1111/j.1468-2982.2009.01930.x. [DOI] [PubMed] [Google Scholar]
- 44.Yalinay Dikmen P, Yavuz BG, Aydinlar EI. The relationships between migraine, depression, anxiety, stress, and sleep disturbances. Acta Neurol Belg. 2015;115:117–122. doi: 10.1007/s13760-014-0312-0. [DOI] [PubMed] [Google Scholar]
- 45.Buse DC, Manack A, Serrano D, Turkel C, Lipton RB. Sociodemographic and comorbidity profiles of chronic migraine and episodic migraine sufferers. J Neurol Neurosurg Psychiatry. 2010;81:428–432. doi: 10.1136/jnnp.2009.192492. [DOI] [PubMed] [Google Scholar]
- 46.Seng EK, Buse DC, Klepper JE, J Mayson S, Grinberg AS, Grosberg BM, et al. Psychological factors associated with chronic migraine and severe migraine-related disability: an observational study in a tertiary headache center. Headache. 2017;57:593–604. doi: 10.1111/head.13021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Whealy M, Nanda S, Vincent A, Mandrekar J, Cutrer FM. Fibromyalgia in migraine: a retrospective cohort study. J Headache Pain. 2018;19:61. doi: 10.1186/s10194-018-0892-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stewart WF, Lipton RB, Simon D. Work-related disability: results from the American migraine study. Cephalalgia. 1996;16:231–238. doi: 10.1046/j.1468-2982.1996.1604231.x. [DOI] [PubMed] [Google Scholar]
- 49.Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 2001;56(6 Suppl 1):S20–S28. doi: 10.1212/wnl.56.suppl_1.s20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Sociodemographic distributions of survey participants, the total Korean population, and cases identified as migraine in the 2009 Korean Headache Survey and the 2018 Korean Sleep-Headache Survey