Abstract
Many studies about Electrical muscle stimulation (EMS) have been performed to determine the effectiveness of EMS. However, most studies enrolled only elderly patients. Moreover, only a few studies have verified the effect of a whole body (WB)-EMS suit on young healthy women. Thus, the main purpose of this study was to verify the physiological effects of exercise training with a WB-EMS suit in young women. During the study periods, 24 young women were randomly assigned into two groups: 1) the WB-EMS training group, and 2) the control. All participants in the two groups performed the same low-intensity resistance exercise three times a week for 6 weeks at a training center. Group 1 used an electric current for WB-EMS suit which was switched on during the exercise period. Outcome measures were body composition, body circumference of hips and abdomen, isokinetic muscle function of knees, balance functions, Magnetic resonance imaging (MRI)s, cardiopulmonary functions, and lipid profiles. All outcomes were measured before and after the exercise protocol over 6 weeks. A total of 23 young women (group 1, n=11; group 2, n=12) completed a 6-week exercise regimen. After exercise, we compared the differences before and after the exercise program in each group. There were significant differences (p≤0.05) in body circumference, cardiopulmonary function in group 1 and 2. In particular, group 1 that activated WB-EMS showed significant differences in the isokinetic muscle function on knee flexors and balance functions. The results of this study show that exercise with a WB-EMS suit can be considered as an effective exercise addition for young women.
Keywords: Exercise, Muscle Strength, Electric Stimulation, Musculoskeletal System
INTRODUCTION
Electric Muscle Stimulation (EMS) has been used in therapy to induce muscle contractions artificially through electrical signals. This stimulation is transmitted to the surface of the skin to make muscle contracts, which has effects similar to the real motion of the muscle.1 Further EMS was often used to prevent the atrophy of muscles that occurs when skeletal muscle is denervated since the 1960s.
With advances in EMS technology, EMS has become increasingly popular for treating patients with central nervous system impairment secondary to brain injuries.2 In 1977, Kot, a Russian scientist, reported that current training was effective in promoting muscle strength in normal adults. EMS training has also been used to prevent muscle atrophy and improve muscle strength.3 Since then, researchers have been studying effective muscle stimulation methods and training for therapeutic purposes.4
In recent years, Whole Body-Electric Muscle Stimulation (WB-EMS) suits as a new therapeutic technology have been developed. It is an attractive and effective training method. It is also a time-saving alternative form of training.5 WB-EMS training is designed to maximize the effect of exercise by adjusting electric stimulation according to the amount and extent of the insulator material, such as fat. It is also known to improve the balance of muscles and blood flow, strengthen the heart, relieve pain, increase muscle activity, power, and exercise performance, as well as improve the body composition.6,7
As to the components, WB-EMS devices usually consist of a suit, a controller, and an application that operates the suit and controller. The suit is made up of stretchable material. It consists of a pad that carried the EMS signal inside the suit. EMS signals are activated by the application and delivered to the skin and muscles by the controller and panels inside the suit. Further the EMS mimics the way the nervous system initiates and simulates muscle activity. Thus, manufacturers of WB-EMS devices insist that EMS training with WB-EMS suit can be accompanied by stronger muscle contractions to provide efficient exercise with less time.7
Many studies have determined the effect of EMS and revealed that EMS is effective in improving muscle endurance, muscle mass, muscle strength, and waist circumference.8,9,10,11 However, there is still some debates as to the effect of EMS. Porcari et al.4 investigated the effects of EMS on 27 college-aged students after training for 8 weeks and concluded that the effectiveness of EMS for healthy individuals was not supported. Deley and Babault11 reported that EMS training has limitations because the EMS devices only stimulates muscles closed to electrodes.
Therefore, it is necessary to examine effects of EMS training closely. Most studies were performed on elderly patients. Only a few studies with randomized controlled trials have been performed on young people.12 Therefore, the purpose of this study was to investigate effects of WB-EMS on muscle mass, strength, decrease of fat, obesity index, balance function, and exercise capacity including cardiopulmonary function in women aged 20 to 30 year.
MATERIALS AND METHODS
1. Design
Participants were randomized with a single blinded-outcome assessor blinded-method to compare effects between WB-EMS training and general training in our center from July 1st, 2019 to September 30th, 2019.
2. Participants
This study was approved by Chonnam National University Institutional Review Board (CNU IRB number: 1040198-190320-HR-016-02).
We screened 65 participants who voluntarily applied to our Healthcare-wear R&BD Center at Chonnam National University for two months. Inclusion criteria were: 1) women aged 20 to 40 years, 2) BMI of 23 or above. Exclusion criteria were: 1) those who had contraindications to whole-body EMS training (medical implants, liver disease, pregnant women, and neurological disorders), 2) those who refused electrical stimulation, 3) those who were under treatment for diseases during the study period, and 4) those who had previous surgical history.
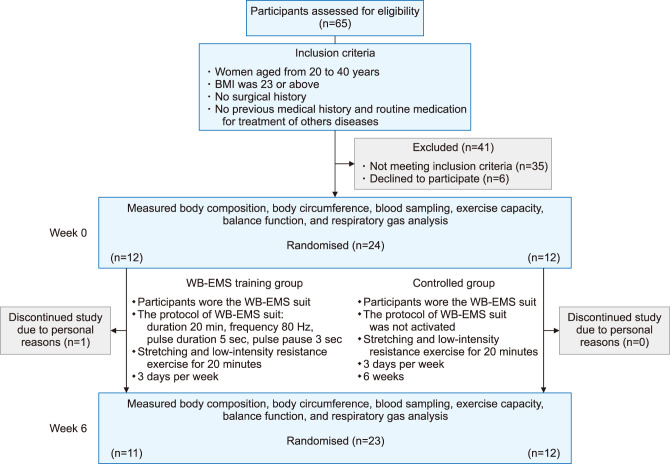
Among them, 35 participants failed to meet the inclusion criteria. After excluding them, we explained our study to eligible participants. Six subjects declined to participate. Finally, 24 participants were included in this study (Fig. 1).
FIG. 1. Design and flow showing the selection of participants for this study.
We used a randomization allocation software program developed by M. Saghaei, MD (Department of Anesthesia, Isfahan University of Medical Sciences, Isfahan, Iran) to implement the random allocation sequence. Participants were randomly allocated into a WB-EMS training group (12 participants, group 1) and a control group (12 participants, group 2). The randomization process was performed by a person who was not involved in any other study procedure.
3. Interventions
Each participant performed exercise sessions three times a week of 20 minutes in duration for 6 weeks for a total of 18 times at our training center. Evaluation of participants was performed by one doctor and one physical therapist before training and after six weeks of training. The investigator who performed pre- and post-treatment outcome measurements remained blind to group allocation. Exercise sessions were performed by the other trainer who was not engaged in the evaluation. Participants in this study did not know which group they were assigned to.
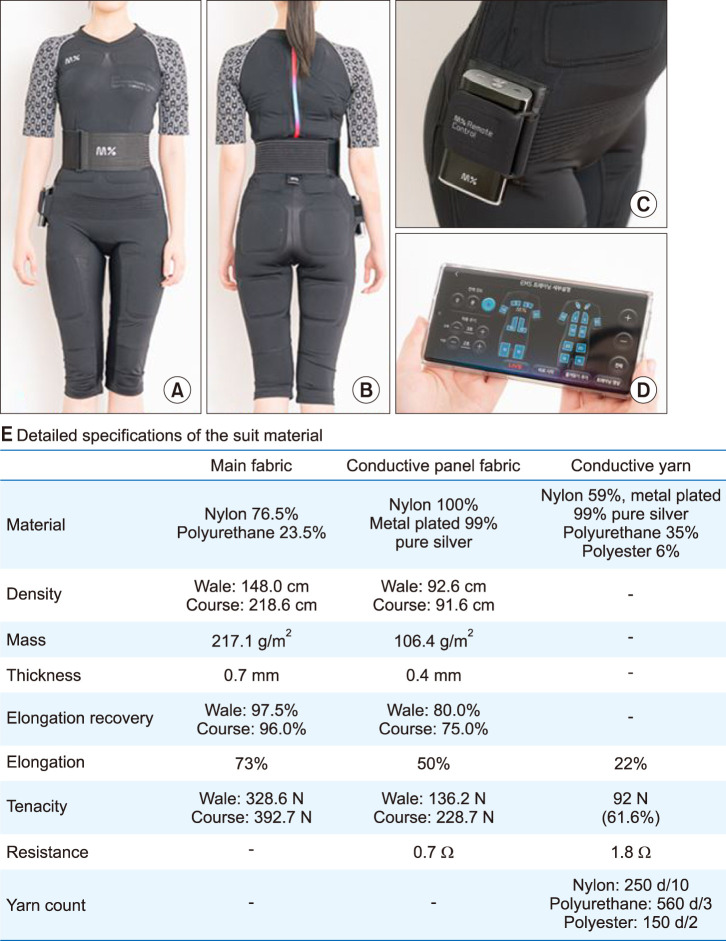
During each training session, all participants wore the WB-EMS Suit (Bodyfriend, Seoul, Korea) (Fig. 2) and performed the low-intensity resistance exercise protocol guided by the trainer.11,13 The suit was selected because it was necessary to verify the effect as a new development. The suit was operated by the controller and the application. The WB-EMS Suit is equipped with 20 conductive panels located on the shoulder (2 panels), arms (4 panels), chest (2 panels), back (4 panels), abdomen (2 panels), buttocks (2 panels), and legs (4 panels) to stimulate the muscle belly of brachialis, triceps of arm, pectoralis major, latissimus dorsi, rectus abdominis, gluteus maximus, rectus femoris, biceps of thigh, semitendinosus, and so on. Specifications of the suit material are shown in Fig. 2. The protocol of WB-EMS device was set by the controller and application; duration of 20 min, frequency of 80 Hz, pulse duration of 5 sec, and pulse pause of 3 sec. The intensity was adjusted and set before each exercise only for group 1.
FIG. 2. Whole-body electric muscle stimulation suit (WB-EMS Suit). (A) The front of the WB-EMS Suit, (B) The back of the WB-EMS Suit, (C) The controller connecting the suit and the application, (D) The application to operate the suit and controller, (E) Specifications of suit materials.
Dynamic stretching was performed before and after main exercises and the overall exercise lasted for 20 minutes in both groups. Main exercises were designed with squats, lunges, crunches, and planks.11,14 Squats and lunges are typical lower body exercises that can strengthen the quadriceps, gluteus maximus, and hamstrings. Crunches are an abdominal exercise that can strengthen the upper rectus abdominis. Planks are the most basic exercises for core muscle that strengthen core muscles around the spine. Squats, lunges, and crunches were performed 20 times each and the plank exercise was performed for 1 minute with qual intensity in both groups.
In group 1, the electric current for WB-EMS suit was switched on during exercise. In group 2, the electric current was switched off. Whole-body EMS training electrical variables are shown in Fig. 1. In both groups, exercise was designed to stop when participants felt dizziness, chest discomfort, muscle soreness, or other medically related symptoms.
4. Outcome measures
We excluded participants who performed less than 15 of the 18 sessions. All outcome measures were checked before starting the exercise protocol and after finishing the exercise protocol.
1) Physical examination / body composition analysis
To evaluate the physique and body mass index, an InBody370 (InBody, Seoul, Korea) was used. During the test, participants took off their shoes and put on a light dress in an upright position. They were measured for about 45 seconds. Body weight, skeletal muscle mass, body fat mass, and BMI were all measured
2) Body circumference
All body circumferences were measured using a tape measure with relaxed posture. Waist circumference at the thinnest part of the waist (WCIT), waist circumference at umbilicus level (WCIU), and hip circumference at the widest part of the hip (HC) were measured with their legs gathered, their arms placed on both shoulders, and breathing out.
3) Lipid profile of laboratory finding
Blood sampling was conducted with participants keeping NPO(nothing per oral) for at least 8 hours. Levels of total cholesterol, triglyceride, HDL-cholesterol, and LDL cholesterol were also checked.
4) Magnetic resonance imaging (MRI) scan
Transverse MR images were acquired using a 1.5 Tesla Magnetom Vision system (Siemens, Erlangen, Germany), and the participants were instructed to void their bladder and bowels before imaging. To avoid tension on the anterior abdominal wall during imaging, participants were positioned in supine position with their knees and hips resting on a foam wedge. The imaging volume was then oriented to be perpendicular to the anterior abdominal wall and consisted of 10 slices at a thickness of 6 mm with an inter-slice distance of 0.5 mm.
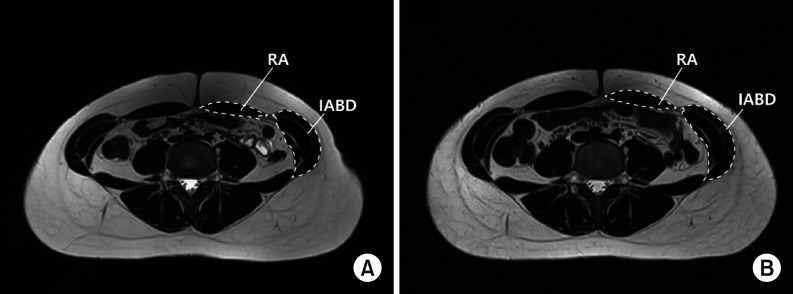
A couple of separate observers who were unaware of this study evaluated the volume of muscle around anterior abdominal wall. During offline image processing, the image slice placed at or closest to the center of the umbilicus was chosen for analysis. If the scanning region was positioned off-center, two slices superior and inferior to the target position were chosen for analysis. Bilateral cross-sectional area (CSA) measurements were conducted for the rectus abdominis, and anterolateral abdominal muscles (external oblique, internal oblique, transversus abdominis) (Fig. 3). Two examiners conducted all measurements. The 2nd staging surveys were performed independently 3 days apart.
FIG. 3. Representative images of RA (Rectus abdominis) and IABD (Anterolateral abdominal) for body morphometric analysis. (A) MRI scan before WB-EMS training, (B) MRI scan after WB-EMS training.
The intraobserver reliability of the measurements was high (intraclass correlation coefficients; range, 0.92, 0.99 for each muscle; 2 repeated measurements of one image from each subject). The interobserver reliability of the measurements was also high (interclass correlation coefficients; 0.96 between two examiners for each muscle).
5) Isokinetic muscle function assessment
In this study, we compared peak torques of the quadriceps and hamstring muscles using a HUMAC NORM 502140 (Computer Sports Medicine, Inc., Stoughton, USA). During the measurement, participants were accustomed to the evaluation through two preliminary exercises. The number of repetitions was controlled regularly at five times at 60 deg/sec and 180 deg/sec, respectively.
6) Balance function evaluation
Balance function was evaluated using I Balance S (Cybermedic Co., Iksan, Korea). Measurements were taken while participant was standing firmly on both feet on the balance pad. Images on the computer monitor were placed just in front of the platform. Participants were asked to keep balance on soft pad with eyes open (OO) and eyes closed (OC). Balance function was assessed by checking the distance of sway.
7) Cardiopulmonary function test
To evaluate exercise effect and energy expenditure of participants, we used a K4b2 portable metabolic analyzer (COSMED, Rome, Italy) and a cardiopulmonary function analyzer. We also measured total exercise time, test mode, VO2max, HRmax, BPmax, and METs (Metabolic equivalent or a unit of sitting oxygen uptake).
For the gas analysis, participants rode a bicycle ergometer (CASE & E-bike, Ge healthcare, USA) and conducted a gradual test following the ACSM guideline.15
5. Sample size and statistical analysis
In this study, sample size was referred to other similar studies.4,11 Assuming a dropout rate of 10%, we recruited 24 participants per group. The sample size for the present study was calculated based on Cohen's formula. The number of groups was set as two, the number of measurements was two, the effect size was 0.9, the significance level was 0.05, and the statistical power was 0.5. The total sample size required for a analysis of variance, calculated using G*power, was 22 (eleven/group). All data were analyzed using SPSS version 23.0 (SPSS Inc., Chicago, IL, USA). Mean Value (M) and standard deviation (SD) were calculated to present descriptive statistics of body composition, blood index, and physical fitness variables in group 1 and group 2. For items with the interaction, Mann-Whitney test and Wilcoxon signed rank test was performed. The significance level (p-value) of all statistical analysis was set at p<0.05.
RESULTS
In this study, we compared each item with the differences before and after exercise program in each group.
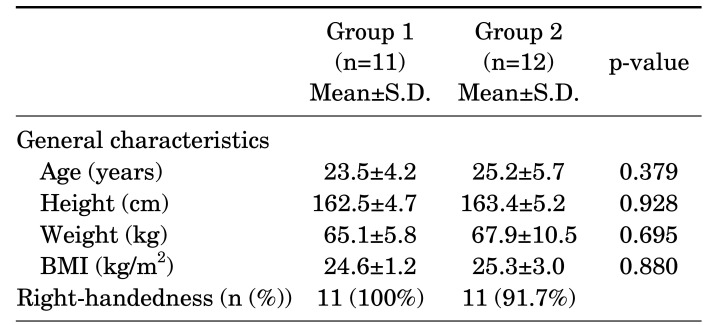
1. Participant demographics
During the period, no complications related to the WB-EMS Suit was observed in either group. A total of 24 participants were assigned to the study protocol. Only one participant refused to follow up the study protocol for personal reasons. Therefore, 23 participants completed the study (11 participants in group 1 and 12 participants in group 2). Baseline demographics and clinical characteristics of the subjects by mean standard deviation are presented in Table 1. The two groups were matched well in baseline characteristics. There was no statistically significant difference in analyzed parameters between the two groups.
TABLE 1. General characteristics.
Group 1 : WB-EMS (whole body - electric muscle stimulation) training group, Group 2 : control group.
2. Physical examination/ body composition analysis
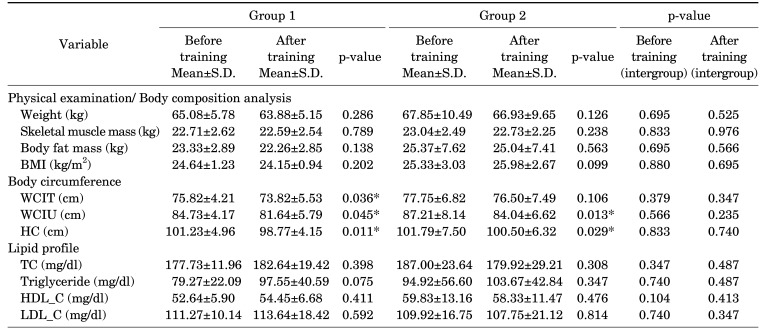
Results of physical examination and body composition analysis are shown in Table 2. In each group, there were no significant differences between before exercise (BE) and after exercise (AE) in body weight, skeletal muscle mass, body fat mass, or BMI. There were also no significant differences in any parameters either in intergroup analysis of BE or AE.
TABLE 2. Differences between group 1 and group 2 for changesin body composition, body circumference, and lipid profile.
WCIT: Waist circumferencein the thinnest part, WCIU: Waist circumference in umbilicus, HC: Hip circumference, T_C: Total cholesterol, HDL_C: HDL cholesterol, LDL_C: LDL cholesterol.
3. Body circumference
Results of body circumference are shown in Table 2. In group 1, WCIT (BE: 75.82±4.21, AE: 73.82±5.53; p<0.05), WCIU (BE: 84.73±4.17, AE: 81.64±5.79; p<0.05), and HC (BE: 101.23±4.96, AE: 98.77±4.15; p<0.05) were significantly lower after 6 weeks of training program compared to initial assessment. In group 2, WCIU (BE: 87.21±8.14, AE: 84.04±6.62; p<0.05) and HC (BE: 101.79±7.50, AE: 100.50±6.32; p<0.05) were significantly lower after 6weeks of training program compared to initial assessment. There were no significant differences in any body circumferences in intergroup analysis of BE or AE.
4. Lipid profile of laboratory finding
Results of lipid profile of laboratory finding are shown in Table 2. In both groups, there was no significant difference in total cholesterol, triglyceride, HDL cholesterol, or LDL cholesterol. There were no significant differences in lipid profiles in intergroup analysis of BE or AE.
5. Magnetic resonance imaging (MRI) scan
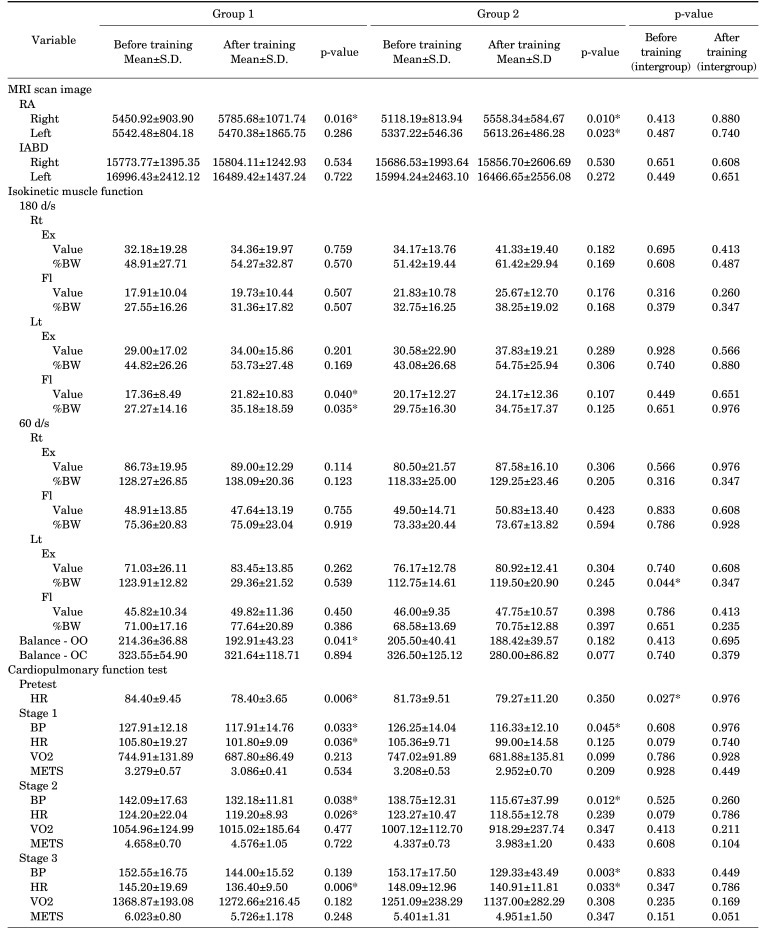
The results of magnetic resonance imaging (MRI) scan are shown in Table 3. The CSA after low-intensity resistance training was significantly increased for the RA muscle on the right in both groups (group 1 BE 5450.92±903.90, AE 5785.68±1071.74; p<0.05; group 2 BE 5118.19±813.94, AE 5558.34±584.67; p<0.05) and RA muscle on the left in group2 (BE: 5337.22±546.36, AE: 5613.26±486.28; p<0.05). However, there was no significant difference in intergroup analysis of BE and AE.
TABLE 3. Differences between group 1 and group 2 for changes in MRI, isokinetic muscle function, balance, and cardiopulmonary function.
RA: Rectus abdominis, IABD: Anterolateral abdominal, Rt: Right, Lt: Left, Ex: Extensors, Fl: Flexors, OO: sway distance on soft pad with eye open, OC: sway distance on soft pad with eye closed.
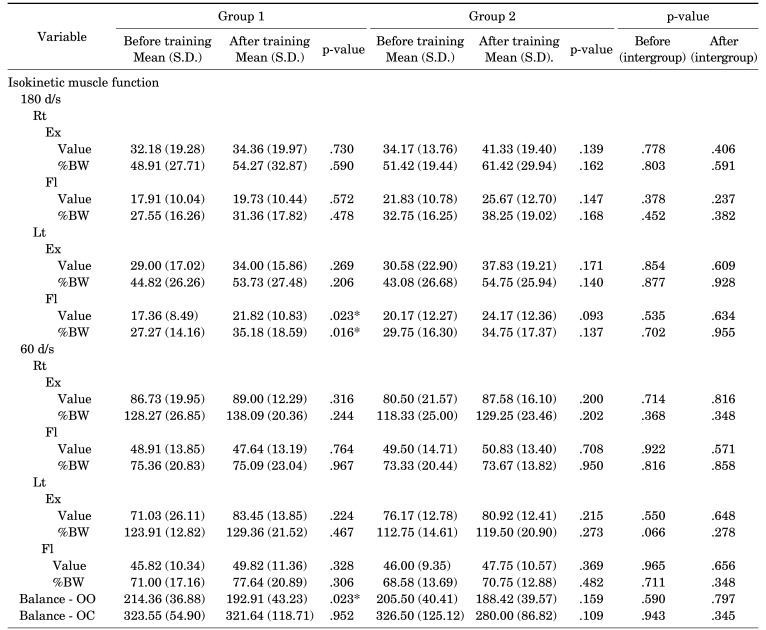
6. Isokinetic muscle function assessment
Results of isokinetic muscle function assessment are shown in Table 4. In group 1, only the strength of the left leg was significantly improved with knee flexed at 180 d/s (Value: BE, 17.36±8.49; AE, 21.82±10.83; p<0.05; % Body Weight :BE, 27.27±14.16; AE, 35.18±18.59; p<0.05) after exercise. In group 2, there was no significant difference in isokinetic muscle function in either leg. There was no significant difference in isokinetic muscle function in intergroup analysis of BE or AE.
TABLE 4. Differences between group 1 and group 2 for changesin isokinetic muscle function and balance function.
Rt: Right, Lt: Left, Ex: Extensors, Fl: Flexors, OO: sway distance on soft pad with eye open, OC: sway distance on soft pad with eye closed.
7. Balance function evaluation
Results of balance function evaluation are shown in Table 4. Only in group 1, OO score (sway distance on soft pad with eye open) was significantly lower after 6weeks of training compared to initial score (BE: 214.36±36.88, AE: 192.91±43.23; p<0.05). However, there was no significant difference in balance function in intergroup analysis of BE or AE.
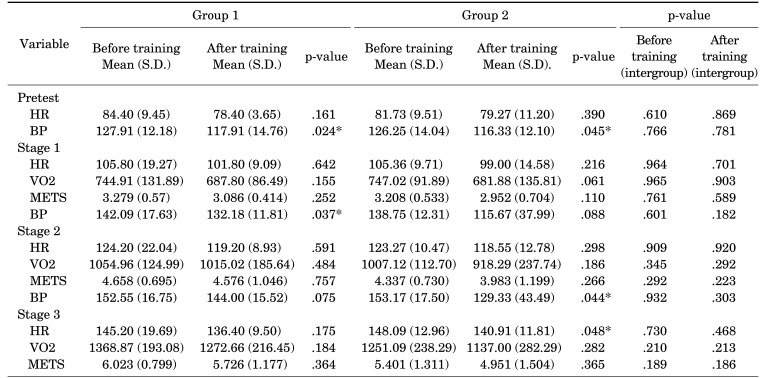
8. Cardiopulmonary function evaluation
Results of cardiopulmonary function are shown in Table 5. There was no significant difference in gas analysis. In both group, blood pressure and heart rate were significantly decreased after exercise. In group 1, blood pressure and heart rate were decreased at stage 1 and 2, and heart rate was decreased at stage 3 with significantly difference. In group 2, blood pressure was decreased at stage 1 and 2, and blood pressure and heartrate were decreased with significantly different at stage 3. Heart rate at pretest was decreased in group 1 and intergroup analysis of before training with significantly difference (BE: 84.40±9.45, AE: 78.40±3.65; p<0.05).
TABLE 5. Differences between group 1 and group 2 for changes in cardiopulmonary function test.
DISCUSSION
In this study, body circumferences for the participants' waists and hips decreased in both exercise groups, although there was no significant difference between the two groups after exercise. Although each group showed significant differences in different items, mean scores of WCIT, WCIU, and HC were reduced after exercise in both groups. Many studies have determined the effect of reducing WC by exercise and suggested that exercise might be potentially beneficial in reducing central obesity.16,17,18 Likewise, in this study, body circumferences seem to be improved after exercise in both groups.
In this study, participants' body compositions including skeletal muscle mass, fat mass, and BMI and lipid profile makers were not significantly different in intergroup analysis of BE or AE. There is some debate about changes of body composition and blood profile after exercise.4,18,19,20,21,22,23,24
Various observations have suggested that specific exercise programs can affect muscle mass and fat mass.4,22,23 However, other observations negated the possibility of improvement in body composition or detected a spot improvement according to the type of exercise.4,24 In the literature related to lipid profile, Hammond et al.17 and Yildirim et al.20 showed no significant differences in lipid profile after 6 weeks or 8 weeks of exercise compared to baseline. On the other hand, Kostrzewa-Nowak et al.21 reported a significant difference in lipid profile for an over-weight exercise group after 12 weeks exercise compared to baseline.
Studies investigating effects of exercise on body composition and lipid profiles have shown different results depending on nutrition, type of exercise, duration of exercise, and intensity of exercise.19,20,21,25 In the present study, participants' dietary habits without diet program and short duration of exercise for 6 weeks might have led to the no effect of exercise on body composition and lipid profiles.
Measurement using the MRI method is helpful to evaluate muscle mass provided by the cross-sectional area.26,27 In this study, MRI measurement was used to evaluate the effects of EMS training. And the CSA of RA muscle on the right was increased in group 1, while CSA of RA on both side was increased in group 2. The increase in CSA of the muscle by the exercise has also been emphasized by other studies.26,27,28 In this study, the difference in muscle increase of RA and IABD within both groups might be due to the position and size of the electric panel attached to the WB-EMS Suit. However, the methods used to measure the correct volume of muscle may not be accurate, although the interobserver and intraobserver ICC were every high. Therefore, these may have acted as variables in this study. Further study is required.
As to the muscle function, especially in group 1, significant differences were found when the left leg was flexed at 180 d/s while muscle function was improved but not significantly different in group 2. In this study, EMS was applied to both extensor and flexor muscles. This might have affected both extensor and flexor. Significant differences were present only in the left lower limb. When the loading of 180 d/s and 60 d/s are compared at the same period, loading with 180 d/s is greater. So the effect of muscle strengthening may have affected the result with 180 d/s more than that with 60 d/s. Although there is no significant difference in intergroup analysis, this result suggests that EMS might have affected the muscle function of the non-dominant side.
Some articles have reported that exercise of the dominant limb can affect the strength of both dominant limb and non-dominant limb due to resistance of the contralateral stabilization bar.29 In the study, resistance of the contralateral stabilization bar was also applied when EMS was activated. In general, a dominant limb is more activated during exercise. In this study, only in group 1, the EMS suit was activated. Thus, dominant and non-dominant limbs were activated simultaneously. This might have affected the balance scale. Not only the limb, but also core muscles were activated bilaterally. Core muscles are mainly composed of abdominal muscles and back muscles including latissimus dorsi muscle and rectus abdominis muscle where panels are placed in this study. Many studies have reported that core muscle training can improve muscle strength and balance of torso.30,31,32 Although we did not evaluate the core muscle, EMS stimulation might have affected core muscles. Although the value of balance function was not significantly different between the two groups, sway distance on soft pad with eye open showed a significant difference after exercise only in group 1. This result might be due to the effect of muscle stimulation of EMS as an effective stimulation in strengthening core muscles.
In this study, systolic blood pressure and heart rate improved significantly in both groups after exercise with different s tage and d ifferent items. This result was comparable to another study that explored exercise efficiency.33 However, in our study, all participants were healthy young women and the exercise protocol did not consider cardiac function that could influence exercise capacity and the protocol was applied during short periods such as 6weeks. We did not consider life style, nutrient plans, or others that might affect cardiopulmonary function.34,35 And in the EMS group, we could not exclude the possibility of the effect on cardiac function with EMS stimulation. Thus, further studies considering cardiac function are needed.
This study had some limitations. The major limitation of this study was the same intensity of exercise, which was conducted without considering participants' motor skills. The intensity of exercise should be designed considering individual's age, health, and athletic condition in the future. However, the intensity of both groups was matched to meet all conditions except for EMS stimulation. In addition, we trained participants for a short period of six weeks without a diet program. Hence, further studies considering diet, long-term follow-up, and exercise intensity are needed.
In this study, the body circumferences were decreased and muscle mass, and cardiopulmonary function were increased with a low-intensity resistance training for 6 weeks. While, body circumferences decreased and muscle strength, muscle mass, cardiopulmonary function, and balance function improved with WB-EMS training. Though we cannot conclude which one is better in this study, it could be considered as a way to improve body composition and physical strength of young women. As a result, the WB-EMS Suit can be considered as an effective exercise and a time-efficient tool for end users of young women. However, further study is needed to clarify the effect of WB-EMS training for different ages, genders, and health conditions.
ACKNOWLEDGEMENTS
This study was supported by a grant from Bodyfriend, Seoul, Korea and supported by a grant from NRF-2016M3A9E9941832.
The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The experiments comply with the current laws of the country in which they were performed.
Footnotes
CONFLICT OF INTEREST STATEMENT: None declared.
References
- 1.Maffiuletti NA, Minetto MA, Farina D, Bottinelli R. Electrical stimulation for neuromuscular testing and training: state-of-the art and unresolved issues. Eur J Appl Physiol. 2011;111:2391–2397. doi: 10.1007/s00421-011-2133-7. [DOI] [PubMed] [Google Scholar]
- 2.Jee YS. The efficacy and safety of whole-body electromyostimulation in applying to human body: based from graded exercise test. J Exerc Rehabil. 2018;14:49–57. doi: 10.12965/jer.1836022.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ward AR, Shkuratova N. Russian electrical stimulation: the early experiments. Phys Ther. 2002;82:1019–1030. [PubMed] [Google Scholar]
- 4.Porcari JP, McLean KP, Foster C, Kernozek T, Crenshaw B, Swenson C. Effects of electrical muscle stimulation on body composition, muscle strength, and physical appearance. J Strength Cond Res. 2002;16:165–172. [PubMed] [Google Scholar]
- 5.Adams V. Electromyostimulation to fight atrophy and to build muscle: facts and numbers. J Cachexia Sarcopenia Muscle. 2018;9:631–634. doi: 10.1002/jcsm.12332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kemmler W, von Stengel S. Whole-body electromyostimulation as a means to impact muscle mass and abdominal body fat in lean, sedentary, older female adults: subanalysis of the TEST-III trial. Clin Interv Aging. 2013;8:1353–1364. doi: 10.2147/CIA.S52337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kemmler W, Teschler M, Weißenfels A, Bebenek M, Fröhlich M, Kohl M, et al. Effects of whole-body electromyostimulation versus high-intensity resistance exercise on body composition and strength: a randomized controlled study. Evid Based Complement Alternat Med. 2016;2016:9236809. doi: 10.1155/2016/9236809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karatzanos E, Gerovasili V, Zervakis D, Tripodaki ES, Apostolou K, Vasileiadis I, et al. Electrical muscle stimulation: an effective form of exercise and early mobilization to preserve muscle strength in critically ill patients. Crit Care Res Pract. 2012;2012:432752. doi: 10.1155/2012/432752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wall BT, Dirks ML, Verdijk LB, Snijders T, Hansen D, Vranckx P, et al. Neuromuscular electrical stimulation increases muscle protein synthesis in elderly type 2 diabetic men. Am J Physiol Endocrinol Metab. 2012;303:E614–E623. doi: 10.1152/ajpendo.00138.2012. [DOI] [PubMed] [Google Scholar]
- 10.Kemmler W, Schliffka R, Mayhew JL, von Stengel S. Effects of whole-body electromyostimulation on resting metabolic rate, body composition, and maximum strength in postmenopausal women: the Training and ElectroStimulation Trial. J Strength Cond Res. 2010;24:1880–1887. doi: 10.1519/JSC.0b013e3181ddaeee. [DOI] [PubMed] [Google Scholar]
- 11.Deley G, Babault N. Could low-frequency electromyostimulation training be an effective alternative to endurance training? An overview in one adult. J Sports Sci Med. 2014;13:444–450. [PMC free article] [PubMed] [Google Scholar]
- 12.Pano-Rodriguez A, Beltran-Garrido JV, Hernández-González V, Reverter-Masia J. Effects of whole-body ELECTROMYOSTIMULATION on health and performance: a systematic review. BMC Complement Altern Med. 2019;19:87. doi: 10.1186/s12906-019-2485-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bemben DA, Fetters NL, Bemben MG, Nabavi N, Koh ET. Musculoskeletal responses to high- and low-intensity resistance training in early postmenopausal women. Med Sci Sports Exerc. 2000;32:1949–1957. doi: 10.1097/00005768-200011000-00020. [DOI] [PubMed] [Google Scholar]
- 14.Song JE. The comparison of the effects of whole-body EMS training with different frequency for 8 weeks [PhD dissertation] Yongin: Kyung Hee University; 2018. [Google Scholar]
- 15.Swain DP, Brawner CA, Nagelkirk P, Swank AM, Bayles MP, Chambliss HO American College of Sports Medicine. ACSM's resource manual for guidelines for exercise testing and prescription. 7th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 16.Ostman C, Smart NA, Morcos D, Duller A, Ridley W, Jewiss D. The effect of exercise training on clinical outcomes in patients with the metabolic syndrome: a systematic review and meta-analysis. Cardiovasc Diabetol. 2017;16:110. doi: 10.1186/s12933-017-0590-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hammond BP, Stotz PJ, Brennan AM, Lamarche B, Day AG, Ross R. Individual variability in waist circumference and body weight in response to exercise. Med Sci Sports Exerc. 2019;51:315–322. doi: 10.1249/MSS.0000000000001784. [DOI] [PubMed] [Google Scholar]
- 18.Aamann L, Dam G, Borre M, Drljevic-Nielsen A, Overgaard K, Andersen H, et al. Resistance training increases muscle strength and muscle size in patients with liver cirrhosis. Clin Gastroenterol Hepatol. 2020;18:1179–1187.e6. doi: 10.1016/j.cgh.2019.07.058. [DOI] [PubMed] [Google Scholar]
- 19.Ferrauti A, Weber K, Strüder HK. Effects of tennis training on lipid metabolism and lipoproteins in recreational players. Br J Sports Med. 1997;31:322–327. doi: 10.1136/bjsm.31.4.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yildirim I, Aydin Altinbas M, Demirezen NB, Dener S, Sezgin V. The effect of different exercise types on sedentary young women's lipid profile. J Back Musculoskelet Rehabil. 2020;33:469–475. doi: 10.3233/BMR-181323. [DOI] [PubMed] [Google Scholar]
- 21.Kostrzewa-Nowak D, Nowak R, Jastrzębski Z, Zarębska A, Bichowska M, Drobnik-Kozakiewicz I, et al. Effect of 12-week-long aerobic training programme on body composition, aerobic capacity, complete blood count and blood lipid profile among young women. Biochem Med (Zagreb) 2015;25:103–113. doi: 10.11613/BM.2015.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muollo V, Rossi AP, Milanese C, Masciocchi E, Taylor M, Zamboni M, et al. The effects of exercise and diet program in overweight people - Nordic walking versus walking. Clin Interv Aging. 2019;14:1555–1565. doi: 10.2147/CIA.S217570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beavers KM, Ambrosius WT, Rejeski WJ, Burdette JH, Walkup MP, Sheedy JL, et al. Effect of exercise type during intentional weight loss on body composition in older adults with obesity. Obesity (Silver Spring) 2017;25:1823–1829. doi: 10.1002/oby.21977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scotto di Palumbo A, Guerra E, Orlandi C, Bazzucchi I, Sacchetti M. Effect of combined resistance and endurance exercise training on regional fat loss. J Sports Med Phys Fitness. 2017;57:794–801. doi: 10.23736/S0022-4707.16.06358-1. [DOI] [PubMed] [Google Scholar]
- 25.Brownell KD, Bachorik PS, Ayerle RS. Changes in plasma lipid and lipoprotein levels in men and women after a program of moderate exercise. Circulation. 1982;65:477–484. doi: 10.1161/01.cir.65.3.477. [DOI] [PubMed] [Google Scholar]
- 26.Rutkowska-Kucharska A, Szpala A. The use of electromyography and magnetic resonance imaging to evaluate a core strengthening exercise programme. J Back Musculoskelet Rehabil. 2018;31:355–362. doi: 10.3233/BMR-169780. [DOI] [PubMed] [Google Scholar]
- 27.DeFreitas JM, Beck TW, Stock MS, Dillon MA, Sherk VD, Stout JR, et al. A comparison of techniques for estimating training-induced changes in muscle cross-sectional area. J Strength Cond Res. 2010;24:2383–2389. doi: 10.1519/JSC.0b013e3181ec86f3. [DOI] [PubMed] [Google Scholar]
- 28.Hides J, Wilson S, Stanton W, McMahon S, Keto H, McMahon K, et al. An MRI investigation into the function of the transversus abdominis muscle during “drawing-in” of the abdominal wall. Spine (Phila Pa 1976) 2006;31:E175–E178. doi: 10.1097/01.brs.0000202740.86338.df. [DOI] [PubMed] [Google Scholar]
- 29.Moritani T, deVries HA. Neural factors versus hypertrophy in the time course of muscle strength gain. Am J Phys Med. 1979;58:115–130. [PubMed] [Google Scholar]
- 30.Agmon M, Belza B, Nguyen HQ, Logsdon RG, Kelly VE. A systematic review of interventions conducted in clinical or community settings to improve dual-task postural control in older adults. Clin Interv Aging. 2014;9:477–492. doi: 10.2147/CIA.S54978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amiridis IG, Hatzitaki V, Arabatzi F. Age-induced modifications of static postural control in humans. Neurosci Lett. 2003;350:137–140. doi: 10.1016/s0304-3940(03)00878-4. [DOI] [PubMed] [Google Scholar]
- 32.Aladro-Gonzalvo AR, Machado-Díaz M, Moncada-Jiménez J, Hernández-Elizondo J, Araya-Vargas G. The effect of Pilates exercises on body composition: a systematic review. J Bodyw Mov Ther. 2012;16:109–114. doi: 10.1016/j.jbmt.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 33.Jurik R, Stastny P. Role of nutrition and exercise programs in reducing blood pressure: a systematic review. J Clin Med. 2019;8:1393. doi: 10.3390/jcm8091393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saneei P, Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L. Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: a systematic review and meta-analysis on randomized controlled trials. Nutr Metab Cardiovasc Dis. 2014;24:1253–1261. doi: 10.1016/j.numecd.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 35.Schwingshackl L, Chaimani A, Schwedhelm C, Toledo E, Pünsch M, Hoffmann G, et al. Comparative effects of different dietary approaches on blood pressure in hypertensive and pre-hypertensive patients: a systematic review and network meta-analysis. Crit Rev Food Sci Nutr. 2019;59:2674–2687. doi: 10.1080/10408398.2018.1463967. [DOI] [PubMed] [Google Scholar]