Abstract
Introduction
Geriatric patients with foreign body aspiration (FBA) lack a detailed medical history. Meanwhile, FBA can mimic other diseases and present with wheezing. Here, we report on the difficulty of making a diagnosis of FBA in an elderly man with wheezing.
Case presentation
An 84-year-old man presented with wet cough. He had progressive lung cancer, for which only supportive care was provided. His physical examination revealed wheezing. We presumptively diagnosed acute exacerbation of chronic obstructive pulmonary disease (AE-COPD) and administered inhaled procaterol and parenteral methylprednisolone, which did not mitigate his symptoms. Computed tomography revealed a round nodule, 1 cm in diameter, in his right intermediate bronchus. Central airway obstruction (CAO) caused by the tumor was initially suspected. However, bronchoscopy revealed a pea (Pisum sativum) lodged in his right bronchus, which was removed using forceps.
Discussion
The typical clinical presentations of FBA are sudden-onset cough and dyspnea. However, some geriatric patients do not have cough or lack the cognitive capacity to inform of an episode of FBA. FBA can mimic other entities including AE-COPD and CAO, as seen in our case. Clinicians should not terminate the diagnostic process until all available information explaining the patient's signs and symptoms is collected.
Conclusion
Despite the lack of apparent aspiration, FBA is an important differential diagnosis of new wheezing in the elderly. Physicians need to carefully evaluate “trivial” information or collect additional information when encountering airway symptoms in elderly patients to avoid missing an FBA diagnosis.
Keywords: Airway obstruction, Foreign bodies, Lung cancer, Peas, Pisum sativum, Wheezing
Highlights
-
•
Geriatric patients with foreign body aspiration (FBA) lack a detailed medical history.
-
•
FBA can mimic other diseases and present with wheezing.
-
•
Clinicians should not terminate the diagnostic process early to avoid missing FBA.
-
•
Availability and anchoring biases could be involved during the process to diagnose FBA.
-
•
We should seek more information from accompanying persons to diagnose FBA early.
List of abbreviations
- AE-COPD
acute exacerbation of chronic obstructive pulmonary disease
- CAO
central airway obstruction
- COPD
chronic obstructive pulmonary disease
- FBA
foreign body aspiration
1. Introduction
Foreign body aspiration (FBA) can mimic other diseases and present with wheezing. Here, we report a case of a patient originally diagnosed with acute exacerbation of chronic obstructive pulmonary disease (AE-COPD), then suspected to have central airway obstruction (CAO) caused by a tumor, and finally diagnosed with FBA, highlighting the importance of including FBA in the differential diagnosis when elderly patients present with wheezing. This case was reported according to the SCARE statement [1].
2. Case presentation
An 84-year-old man presented with wet cough. He reported that his cough had started 8 hours prior to this visit and gradually exacerbated, prompting his visit to the emergency department. He had no other respiratory symptoms such as sore throat, nasal discharge, or chest pain. His medical history included lung cancer and chronic obstructive pulmonary disease (COPD). He denied history of FBA or aspiration pneumonia. His lung cancer had infiltrated the left vagal nerve without metastases, for which he only received supportive care. He also required 2.5 L/min oxygen as home oxygen therapy for COPD. He had been using vilanterol, fluticasone, glycopyrronium, and l-carbocisteine regularly for COPD, and had no known allergies to drugs or foods. His vital signs on arrival were as follows: body temperature, 36.2 °C; heart rate, 93 beats/min; blood pressure, 171/65 mmHg; respiratory rate, 30/min, and oxygen saturation on 3 L/min nasal cannula oxygen, 96%. Wheezing was noted on physical examination. The white blood cell count was 9,100 cells/mcL (neutrophils, 72.9%; and lymphocytes, 20.2%). A chest radiograph revealed the preexisting left lung tumor; no new findings were noted.
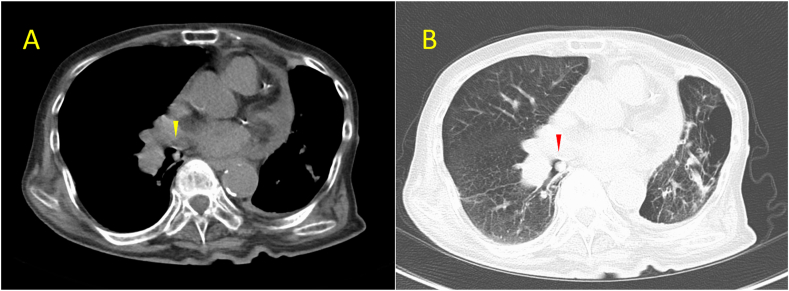
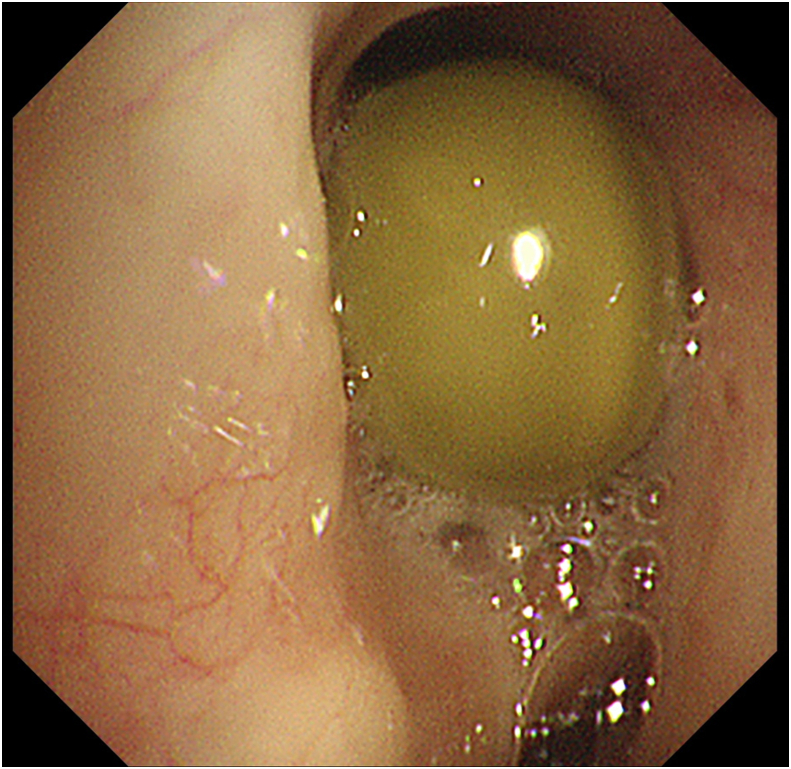
We presumptively diagnosed AE-COPD possibly due to a viral infection and administered inhaled procaterol and parenteral methylprednisolone (40 mg) first. However, because the response to these drugs was limited, we considered the possibility of bronchial diseases such as CAO given his history of untreated lung cancer and the lack of new findings on the chest radiograph. Non-contrast computed tomography of the lung showed a round nodule, 1 cm in diameter, in the right intermediate bronchus, which partially obstructed the bronchial lumen (Fig. 1). Considering that the nodule had not been present 2 months prior to this visit, and only supportive care was being provided to the patient for his lung cancer, we suspected progression of the tumor. A pulmonary physician with 15 years' experience performed a bronchoscopy. Bronchoscopy revealed a pea (Pisum sativum) lodged in the patient's right bronchus (Fig. 2), which established the diagnosis of pea aspiration. The pea was subsequently removed using forceps, and the wheezing resolved. There were no complications during the bronchoscopy. Repeat history taking from the patient's family suggested that the cough started while the patient ate peas, which also supported the diagnosis. He was discharged with no sequelae on hospitalization day 5. On discharge, we advised the patient and his family to seek medical advice if he experienced an acute exacerbation of his respiratory symptoms while eating because it might indicate aspiration of food. They understood this advice and the patient did not experience recurrent food aspiration during 5 months of follow-up.
Fig. 1.
A round nodule in the patient's right intermediate bronchus on non-contrast computed tomography (arrow) on the lung window setting (A) and mediastinal window setting (B).
Fig. 2.
A pea (Pisum sativum) lodged in the patient's right bronchus was removed using forceps.
3. Discussion
Foreign body aspiration (FBA) frequently occurs in children aged < 3 years [2]. However, FBA can also occur in adults, including geriatric patients, particularly those with neurological impairment and drug or alcohol intoxication. Geriatric patients with FBA often aspirate teeth, pins, and whistles [3].
The typical clinical presentations of FBA are sudden-onset cough and dyspnea. However, some geriatric patients do not have cough or lack the cognitive capacity to inform of an episode of FBA. Lin et al. reported that only 29% of geriatric patients can declare an event of aspiration [4]. Furthermore, the asymptomatic period from the timing of aspiration can be longer than the following symptomatic period [5]. These factors complicate diagnosing geriatric patients with FBA. Furthermore, chest radiographs do not detect approximately 80% of foreign bodies [6]. Therefore, to directly detect and remove foreign bodies, bronchoscopy should be considered.
FBA can mimic entities such as asthma, anaphylaxis, angioedema, CAO, AE-COPD, congestive heart failure, drug reaction, and vocal cord dysfunction [7]. CAO caused by malignancy is mostly observed in patients with lung cancer [8]. Metastases, mostly from thyroid, breast, or colon cancer, melanoma, or renal carcinoma, can also obstruct the central airways [8]. As both FBA and CAO can be associated with obstructive pneumonia, atelectasis, lung abscess, or pleural effusion, early diagnosis and restoration of the obstructed airway are important.
The symptoms of FBA in geriatric patients can be atypical, and detailed history taking is not always possible. Thus, we should seek other clues for the diagnosis of FBA. For example, there may be some differences in the respiratory sounds between the bilateral lungs. Bronchial foreign bodies can present as unilateral wheezing [9]. A prone or a head-down position can relieve symptoms of FBA [10]. The respiratory sounds also diminish or change in these positions. Although chest radiographs cannot always detect foreign bodies, hyperinflation of the affected lung can be an indirect sign of FBA. Clinicians should seek subtle physical signs and abnormalities on imaging for a prompt and accurate FBA diagnosis.
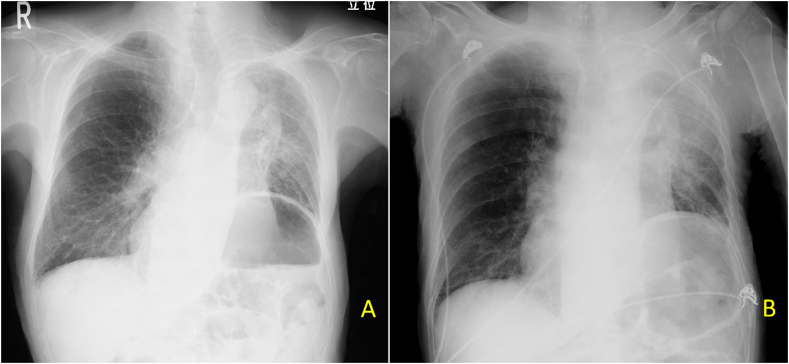
In our patient, we failed to promptly diagnose FBA for the following reasons. First, we should have obtained the medical history earlier from the patient's accompanying family. Only on repeat history taking, the patient's family informed us that the cough suddenly started while the patient was eating peas. Thus, we should seek more information from any accompanying persons when encountering respiratory symptoms that cannot be easily explained based on the medical history and underlying conditions. Second, we did not screen for laterality of, or changes in, auscultation findings in different body positions. Third, we initially detected no changes in the patient's chest radiograph. However, upon retrospectively reviewing the radiograph (Fig. 3A), we noted hyperinflation of the affected lung in the newer one (Fig. 3B), which could indirectly suggest the existence of a check-valve mechanism in the lung. Finally, there might have been availability and anchoring biases involved. Availability bias refers to the tendency to overestimate the likelihood of events when they are easily recalled [11]. Anchoring bias is defined as the tendency to be attached to particular initial traits of a presentation very early in the diagnostic process, making it difficult to correct errors afterward [11]. Our initial diagnosis of AE-COPD was influenced by availability bias because respiratory symptoms in patients with COPD are often related to AE-COPD. The later diagnosis of CAO was susceptible to anchoring bias because this patient had not experienced AE-COPD previously but had an untreated lung cancer, which could potentially manifest as metastasis to the bronchus, thereby developing CAO. Our case emphatically suggests that clinicians should not terminate the diagnostic process until all available information explaining the patient's signs and symptoms is collected.
Fig. 3.
(A) The radiograph taken one month prior to the current episode, and (B) hyperlucency and hyperinflation of the right lung as of the current episode.
4. Conclusion
Geriatric patients with FBA can present with atypical or scant histories and physical findings. FBA is an important differential diagnosis of new wheezing in the elderly. Physicians need to carefully evaluate “trivial” information or collect additional information when encountering airway symptoms in elderly patients to avoid missing an FBA diagnosis.
Ethical approval
Not required for case reports. We obtained written informed consent from the patient's family.
Sources of funding
There are no sources of funding.
Author contribution
HM and AK looked after the patient, wrote and revised the draft, and approved the submission of the current article.
Research registration
Not applicable.
Guarantor
AK serves as the guarantor for this article.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Informed consent
Written informed consent was obtained from the patient's family for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.01.064.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Group S. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 2.Colavita L., Gelli C., Pecorari L., Peroni D.G. A history of recurrent wheezing can delay the diagnosis of foreign body aspiration in a paediatric emergency department. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-211946. bcr2015211946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sehgal I.S., Dhooria S., Ram B., Singh N., Aggarwal A.N., Gupta D. Foreign body inhalation in the adult population: experience of 25,998 bronchoscopies and systematic review of the literature. Respir. Care. 2015;60(10):1438–1448. doi: 10.4187/respcare.03976. [DOI] [PubMed] [Google Scholar]
- 4.Lin L., Wang Y., Zha X., Tang F., Lv L., Liu X. Cayenne aspiration: an unusual type of lower airway foreign-body aspiration. Clin. Interv. Aging. 2014;9:2019–2025. doi: 10.2147/CIA.S73985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang L., Pudasaini B., Wang X.F. Diagnose of occult bronchial foreign body: a rare case report of undetected Chinese medicine aspiration for 10 long years. Medicine. 2016;95(31) doi: 10.1097/MD.0000000000004076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cherrez-Ojeda I., Felix M., Vanegas E., Mata V.L., Jimenez F.M., Ugarte Fornell L.G. Rhonchus and valve-like sensation as initial manifestations of long-standing foreign body aspiration: a case report. Am. J. Case Rep. 2019;20:70–73. doi: 10.12659/AJCR.913405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kann K., Long B., Koyfman A. Clinical mimics: an emergency medicine-focused review of asthma mimics. J. Emerg. Med. 2017;53(2):195–201. doi: 10.1016/j.jemermed.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 8.Murgu S.D., Egressy K., Laxmanan B., Doblare G., Ortiz-Comino R., Hogarth D.K. Central airway obstruction: benign strictures, tracheobronchomalacia, and malignancy-related obstruction. Chest. 2016;150(2):426–441. doi: 10.1016/j.chest.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Brewer D.C., Regala M., Hess J. Calcium pill aspiration: a case report. J. Emerg. Med. 2017;52(5):e201–e202. doi: 10.1016/j.jemermed.2016.12.014. [DOI] [PubMed] [Google Scholar]
- 10.Luczak A. Effect of body position on relieve of foreign body from the airway. AIMS Publ. Health. 2019;6(2):154–159. doi: 10.3934/publichealth.2019.2.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stiegler M.P., Neelankavil J.P., Canales C., Dhillon A. Cognitive errors detected in anaesthesiology: a literature review and pilot study. Br. J. Anaesth. 2012;108(2):229–235. doi: 10.1093/bja/aer387. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.