Abstract
Background
It is the aim of this study to conceptualize a scheme for patellar-height analysis suitable for knees without and with implanted endoprosthesis. Furthermore, patellar-height and change of patellar-height by total-knee-arthroplasty (TKA) should be studied and correlated with clinical outcomes. We hypothesize that not only True-Patella-Infera (TPI) but also Pseudo-Patella-Infera (PPI) might be correlated with elevated anterior-knee-pain and reduced range-of-motion.
Methods
Several patellar-height indices were measured by three independent raters in two passes. Indices were analyzed and intra- and interobserver agreements were determined. For radiographic and clinical evaluation of 92 knee arthroplasties, the Insall-Salvati Index (ISI) and the Caton-Deschamps Index (CDI) were used to determine patellar-height and especially the amounts of TPI and PPI. Patellar-height was correlated with clinical outcome parameters: pain, ROM, Oxford Knee Score, Knee Society Score, Kujala Score, SF-36, Tegner and Lysholm.
Results
All used patellar-height indices demonstrated good intra- and interobserver agreement. Low preoperative ROM was correlated with low postoperative ROM after primary TKA. Postoperatively, 2.2% of the patients had a TPI and 9.8% had a PPI. Patella infera was not correlated with reduced subjective or objective clinical outcome parameters.
Conclusions
Preoperative ROM is a good predictor of postoperative ROM after primary TKA. Patellar-height analysis can be sufficiently performed using the ISI and the CDI, respectively the derived CDI (dCDI) in cases with implanted endoprosthesis. As an alternative to the CDI/dCDI, the BPI/mBPI can be used. There seems to be a certain threshold of acceptable patellar-height reduction, in which clinical outcome is not deteriorated.
Keywords: TKA, Patella infera, Patella baja, Anterior knee pain, Insall-salvati, Caton-deschamps
1. Introduction
Multiple radiological patella-height indices (PHI) exist. Especially in knees with implanted endoprostheses valid measuring and comparing of patella-height is still a problem.1, 2, 3 Furthermore, it is under debate, if patella infera after total knee arthroplasty impairs clinical outcome.4
True patella infera (TPI) is defined as a direct shortening of the patellar tendon, probably due to scarring. Pseudo patella infera (PPI) is defined as indirect or relative alteration of patellar height, mostly due to joint line elevation. Both components (TPI and PPI) should be part of a complete patellar height assessment, which demands a combination of PHI analyzing both TPI and PPI.
It is the aim of this study to conceptualize a scheme for patellar-height analysis suitable for knees without and with implanted endoprosthesis. Furthermore, patellar height and change of patellar height by total knee arthroplasty (TKA) should be studied and correlated with clinical outcomes. We hypothesize that not only TPI but also PPI might be correlated with elevated anterior knee pain and reduced range of motion after TKA.
2. Patients and methods
From our database, we retrospectively identified the patients who received a primary bicondylar standard TKA without patella resurfacing in 2015. Randomly, eligible 150 patients were chosen. Exclusion criteria were: missing consent, patient not willing to come to final follow-up, patella resurfacing, missing or insufficient quality of radiographs, or severe lower back pain with neurological symptoms affecting the leg. We could see 71 patients for a final follow-up at least 24 months after surgery. 21 patients had received a TKA on the other side in our department before. We were able to analyze 92 knee joints (n = 92, female = 51, male = 41, right = 47, left = 45, age = 73 (52–88). The last follow-up was on average 60 months (24–138 months) postoperatively. The datasets at preoperative admission, three months, and twelve months postoperative were analyzed retrospectively. This research has been approved by the IRB of the corresponding author's firs institution and patient consents have been received for the conduction of this study.
2.1. Preoperative planning
For preoperative planning anteroposterior, lateral, skyline patellar view, and long-leg standing anteroposterior radiographs were done. Digital planning software (mediCAD, Hectec GmbH, Landshut, Germany) was used to choose the appropriate implant components and measure the correction of mechanical axis.
2.2. Operative technique
All operations were performed by experienced surgeons and strictly according to internal standard operation procedures. Perioperatively, an intravenous medication with 2 g Cephazolin was applied as a single shot. All operations were controlled by computer navigation using the Orthopilot TKA software. After median skin incision an anteromedial parapatellar arthrotomy was performed. The Hoffa fat pad was partially resected. A patellar denervation with resection of osteophytes and without resurfacing the patella was done as part of the standard procedure. The rotation of the femoral component was oriented in relation to the transepicondylar axis. Prior to the cemented implantation of tibial and femoral components, the pneumatic tourniquet was applied, and bone surface was prepared by Jet Lavage. In addition to the software protocol, a manual control of range of motion and patella tracking were performed. A closed suction drainage was applied. In preparation of wound closure local anesthetics and tranexamic acid were injected. After wound closure a sterile dressing was applied.
2.3. Postoperative protocol
All patients were mobilized with allowed full weight-bearing at the first day after surgery. The suction drainage was removed at the second day after surgery. Patients received physiotherapy daily. Discharge was 7.1 days after surgery. A three-week rehab was organized. All patients had a postoperative follow-up appointment about three, six, twelve, and 24 months after surgery for clinical and radiographic control.
2.4. Patellar-height indices
We chose the following radiological indices for patellar-height measurements on the lateral radiographs:
-
•
Insall-Salvati Index (ISI)5
-
•
Modified Insall-Salvati Index (mISI)6
-
•
Caton-Deschamps Index7 (CDI) preoperatively and a derived Caton-Deschamps-Index8 (dCDI) postoperatively (Fig. 1)
-
•
Blackburne-Peel Index (BPI)9
Fig. 1.
Essential indices for Patellar-height analysis determining True patella height and Pseudo patella height alterations.
ISI Insall-Salvati Index, CDI Caton-Deschamps Index, dCDI derived Caton-Deschamps Index (Modification of the CDI for arthroplasty).
Values for classification into groups of patella infera, norma, or alta are shown in Table 1.
Table 1.
Patellar-height indices.
| Index | Patella infera | Patella norma | Patella alta |
|---|---|---|---|
| Insall-Salvati | <0.8 | 0.8–1.2 | >1.2 |
| Modified Insall-Salvati | <1.2 | 1.2–2.0 | >2.0 |
| Caton-Deschamps | <0.6 | 0.6–1.2 | >1.2 |
| Blackburne-Peel | <0.6 | 0-6 – 1.0 | >1.0 |
All radiographic PHI were measured on lateral radiographs of the knee independently by three raters (one inexperienced but trained rater, one experienced orthopaedic surgeon, and one experienced musculoskeletal radiologist). To determine not only the interrater reliability, but also the intrarater reliability, all measures were repeated after 6 weeks in randomized order.
2.5. Clinical outcome analysis
At the last follow-up, the following clinical outcome parameters were assessed:
-
•
Numeric pain scale (NRS)
-
•
Short Form Health Survey (SF-36)
-
•
Oxford Knee Score (OKS)
-
•
Knee Society Score (KSS)
-
•
Tegner Lysholm Knee Scoring Scale
-
•
Kujala Anterior Knee Pain Scale (AKPS)
Also, a standard clinical examination was performed by two independent observers, who were not involved in the treatment of the patients. The clinical examination consisted of:
-
•
Inspection and palpation of the knee
-
•
Range of motion (ROM) using a universal goniometer
-
•
Strength testing for extension and flexion
-
•
Frontal and sagittal stability
-
•
Walking distance and gait pattern
-
•
History for uncommon or adverse events and complications
2.6. Statistical analysis
For statistical analysis, IBM SPSS Statistics Version 26 was used. The Mann-Whitney-U test was utilized to compare the independent samples on variables that were ranked, or which distribution was asymmetrical. Only for comparison of the SF-36 test, a two-sample t-test was used in assumption of continuous and symmetrically distributed variables within groups. The t-test for dependent samples was used to check the measured values preoperatively and postoperatively. A normal distribution was checked and confirmed. A p-value of <0.05 was considered statistically significant.
3. Results
3.1. Conception of standardized patellar-height analysis
Inter- and intrarater reliability was good for all used indices. ISI an mISI can be used equally. They showed a good correlation (preop: ICC 0.553, p < 0.001; postop: ICC 0.368, p < 0.001). CDI/dCDI and BPI can be used equally. They showed a good correlation (preop: ICC 0.873, p < 0.001; postop: ICC 0.949, p < 0.001). In the interests of simplification, we only used ISI and CDI/dCDI for the assessments at the last follow-up.
3.2. Proof of concept and clinical follow-up correlation
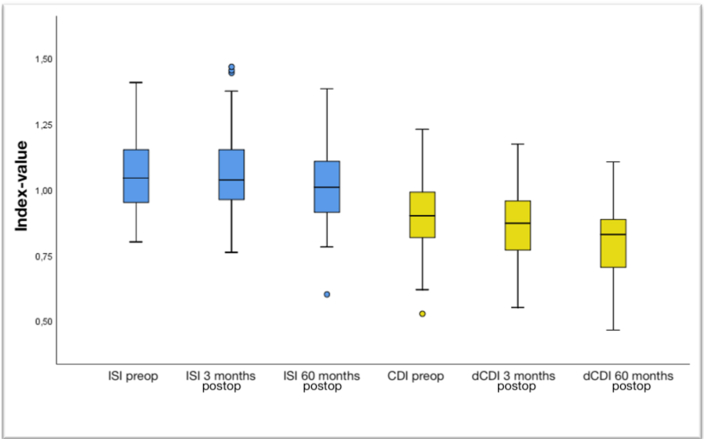
At the last follow-up, the ISI was 3.8% (p < 0.001) lower than preoperatively, while the CDI/dCDI decreased by 10% (p < 0.001) (Fig. 2). The ROM significantly improved in all patients (p = 0.001). Reduced preoperative ROM was associated with reduced postoperative ROM (p = 0.002) (Fig. 3).
Fig. 2.
ISI and CDI/dCDI measurements at different times of follow-up.
CDI Caton-Deschamps Index, dCDI derived Caton-Deschamps Index, ISI Insall-Salvati Index.
Fig. 3.
Correlation of preoperative ROM with postoperative ROM after TKA.
ROM range of motion, TKA Total Knee Arthroplasty.
Patients were grouped into a control group without decrease of patella height after TKA and a group with pseudo patella infera (n = 9) after TKA. Two patients hat a true patella infera. Regarding the numerical rating scale (NRS) for pain, all patients did not have any pain at rest and under stress. With a median of 0, neither group showed a statistically significant difference in the Mann-Whitney-U test for pain.
The OKS assesses the condition of the patient's knee joint with its 12 questions. The control group with a median of 16 (AM: 18.0 ± 5.8) and the group with PPI with a median of 15 (AM: 16.4 ± 5.1) showed no significant difference in the OKS score. U = 284,500, Z = −1.083, p = 0.279, r = −0.114.
For the KSS, consisting of two subcategories, the Knee Score (kKSS) and the Function Score (fKSS), a maximum of 100 points can be achieved in both categories. There was no significant difference in the scores in the kKSS with a median of 82 (AM: 79.6 ± 12.5) in the control group and a median of 88 (AM: 85.7 ± 8.2) in the PPI group. U = 254.000, p = 0.162, r = −0.147. In the fKSS, there was also no significant difference with a median of 80 (AM: 81 ± 19.9) in the control group and a median of 100 (AM: 86.7 ± 22.9) in the PPI group. U = 280.000, p = 0.237, r = −0.125.
The modified Lysholm Score with a maximum of 100 points with the best possible patient outcome and the associated activity scale from 0 to 10 points showed no significant differences between the groups. In the control group, the Lysholm score showed a median of 91 (AM: 88.7 ± 11.7) and the activity score according to Tegner showed a median of 3 (AM: 3.3 ± 1.2). In the PPI group, the Lysholm score showed a median of 91 (AM: 90.7 ± 7.3) and the activity score according to Tegner showed a median of 4 (AM: 3.4 ± 1.0). Lysholm Score: U = 359.500, p = 0.946, r = −0.007. Activity score according to Tegner: U = 282.500, p = 0.286, r = −0.112.
The SF-36 with its eight dimensions, showed no statistically significant difference between the control group and the patients with PPI (p > 0.05).
The Kujala score for anterior knee pain with its 13 questions and a maximum of 100 points showed no significant difference between groups. U = 322.500, p = 0.572, r = −0.060. The control group had a median of 72 (AM: 71.2 ± 11.7) and the PPI group a median of 73 (AM: 74.3 ± 14.0).
In the patella-norma-group (control), 76 patients were satisfied with their knee joint and five were not. 77 patients reported that their knee has improved by the surgery.
In the PPI group, eight patients told to be satisfied and one was not. All patients reported improvement of their knee problems by the operation.
In the control group, 49 patients stated that they could easily walk more than 2000 m. 23 could go up to 2000 m or less (n = 72). Nine patients did not specify a walking distance.
In the PPI group, seven patients reported a walking distance of over 2000 m. One patient stated a walking distance of 400 m (n = 8). One patient did not specify a walking distance.
Regarding the ROM, we found no significant differences in the PPI group compared with the patella-norma group (p = 0.781). The Zohlen sign was positive in one patient of both groups. We didn't find any positive apprehension sign.
4. Discussion
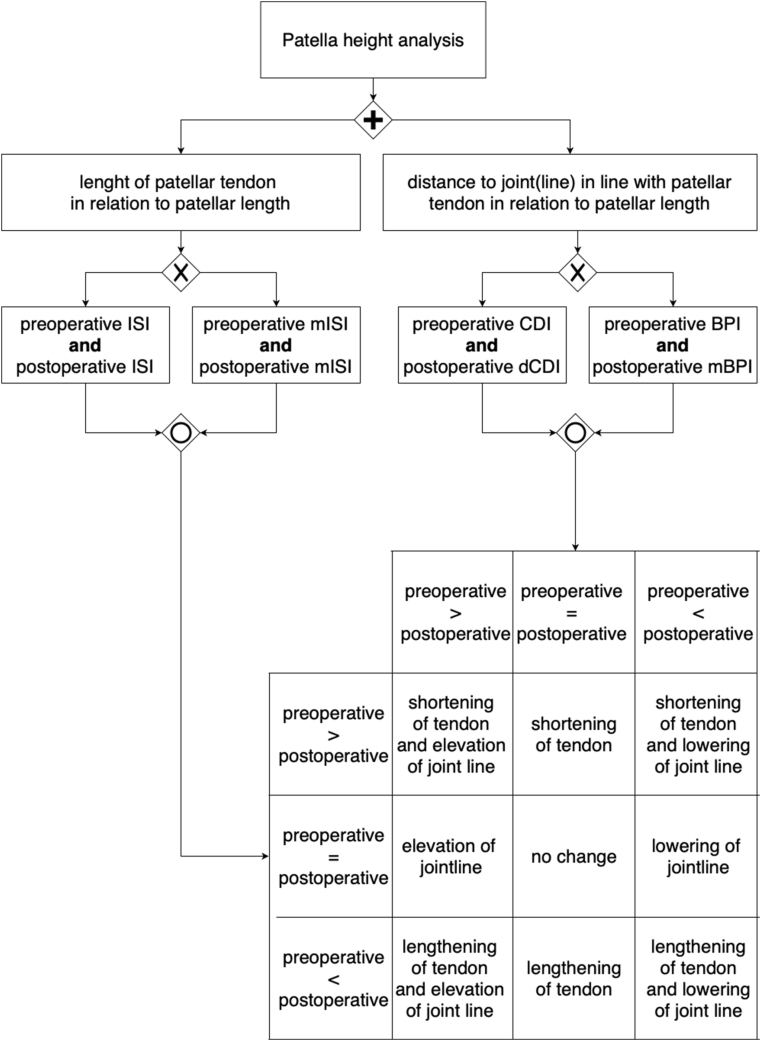
One important finding of this study is that preoperative ROM is a good predictor of postoperative ROM after primary TKA (Fig. 3). We demonstrated that patella-height analysis can be sufficiently performed using the ISI and the CDI, respectively the dCDI in cases with implanted endoprosthesis. As an alternative to the CDI/dCDI, the BPI/mBPI can be used. Using this concept of patellar-height analysis, Fig. 4 helps with interpretation of measurement results.
Fig. 4.
Algorithm and interpretation of patellar-height measuring using ISI or mISI and CDI/dCDI or BPI/mBPI.
BPI Blackburne-Peel Index, CDI Caton-Deschamps Index, dCDI derived Caton-Deschamps Index, ISI Insall-Salvati Index, mBPI modified Blackburne-Peel Index, mISI modified Insall-Salvati Index.
We showed good intra- and interobserver reliability for each of these PHI. Using a combination of PHI like mentioned here and illustrated in Fig. 1, not only the whole amount of patella infera, but also the amounts of TPI and PPI can be determined. This is essential to fully understand the pathology and for consideration of treatment options.
Other authors demonstrated the best reliability for the mISI, but they recommended to use the ISI because it had the second-best reliability but better validity than the mISI.10 In line with our results, another study demonstrated sufficient patellar-height analysis before and after TKA by ISI, BPI, and CDI showing an overall high interobserver agreement.11 Like the CDI, the BPI could be used for patella height comparison before and after TKA, as these indices show similar and not significant different relative amounts (%) of patella height alteration.
In our patients, the proportions of TPI (2.2%) and PPI (9.8%) were very low compared to the literature.12, 13, 14, 15 Reasons for low rates of patella infera might be meticulous preoperative planning and adjunct intraoperative control by navigation. We could not find any tendencies of inferior clinical outcomes in those patients, who showed a patellar height index reduction after primary TKA. There seems to be a certain threshold of acceptable patellar height reduction, in which clinical outcome is not deteriorated.
In the literature, TPI showed significantly worse clinical outcomes, whereas PPI was described as a relatively common finding without significant impact on clinical outcomes.4,16 Our study is limited due to the number of patients and its retrospective character. Based on our results, we cannot tell the amount of PPI, which might provoke any symptoms like anterior knee pain or reduced ROM. We demonstrated that a patella height reduction of up to 10% (preoperatively versus two years postoperatively) did not compromise clinical outcome.
5. Conclusions
We demonstrated preoperative ROM is a good predictor of postoperative ROM after primary TKA. Patellar-height analysis can be sufficiently performed using the ISI and the CDI, respectively the derived CDI (dCDI) in cases with implanted endoprosthesis. As an alternative to the CDI/dCDI, the BPI/mBPI can be used. There seems to be a certain threshold of acceptable patellar-height reduction, in which clinical outcome is not deteriorated. This is at least 10%.
Declaration of competing interest
The authors declare that they have no competing interests.
Abbreviations
- AKPS
Kujala Anterior Knee Pain Scale
- BPI
Blackburne-Peel Index
- CDI
Caton-Deschamps-Index
- dCDI
derived Caton-Deschamps Index
- ICC
Intraclass Correlation
- ISI
Insall-Salvati Index
- KSS
Knee Society Score
- mBPI
modified Blackburne-Peel Index
- mISI
modified Insall-Salvati Index
- NRS
Numeric Rating Scale for pain
- OKS
Oxford Knee Score
- PHI
Patellar-height indices
- PPI
Pseudo patella infera
- ROM
range of motion
- SF-36
Short Form Health Survey
- TKA
Total knee arthroplasty
- TPI
True patella infera
Ethical approval and consent to participate
This research has been approved by the Institutional Review Board of the University of Tübingen under the project number 764/2018BO2. Informed consent to use data and diagnostic images was obtained.
Consent for publication
Yes.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Funding
No funding was received for this study.
Authors’ contributions
CK initiated and planned the study, collected the data, analyzed the data, and wrote the manuscript. JR collected and analyzed the data. LCG, FS, AS, FS supported data collection. FE supported data collection, analyzed the data, and wrote the manuscript. All authors approved the final manuscript.
Acknowledgements
Not applicable.
References
- 1.Narkbunnam R., Chareancholvanich K. Effect of patient position on measurement of patellar height ratio. Arch Orthop Trauma Surg. 2015;135(8):1151–1156. doi: 10.1007/s00402-015-2268-9. [DOI] [PubMed] [Google Scholar]
- 2.Verhulst F.V., van Sambeeck Jdp, Olthuis G.S., van der Ree J., Koëter S. Patellar height measurements: Insall-Salvati ratio is most reliable method. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):869–875. doi: 10.1007/s00167-019-05531-1. [DOI] [PubMed] [Google Scholar]
- 3.Yiannakopoulos C.K., Mataragas E., Antonogiannakis E. The effect of quadriceps contraction during weight-bearing on four patellar height indices. J Bone Joint Surg Br. 2008;90(7):870–873. doi: 10.1302/0301-620X.90B7.20111. [DOI] [PubMed] [Google Scholar]
- 4.Aguirre-Pastor A., Ortolá D.J., Lizaur-Utrilla A., Rosa M.A., Lopez-Prats F.A. Is pseudo-patella baja really a serious complication of total knee arthroplasty? J Arthroplasty. 2020;32(2):557–562. doi: 10.1016/j.arth.2019.09.031. [DOI] [PubMed] [Google Scholar]
- 5.Insall J., Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 6.Grelsamer R.P., Meadows S. The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop Relat Res. 1992;282(9):170–176. [PubMed] [Google Scholar]
- 7.Caton J., Deschamps G., Chambat P., Lerat J.L., Dejour H. [Patella infera. Apropos of 128 cases] Rev Chir Orthop Reparatrice Appar Mot. 1982;68(5):317–325. [PubMed] [Google Scholar]
- 8.Xu B., Xu W.-X., Lu D., Sheng H.-F., Xu X.-W., Ding W.-G. Application of different patella height indices in patients undergoing total knee arthroplasty. J Orthop Surg Res. 2017;12(1):191. doi: 10.1186/s13018-017-0694-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blackburne J.S., Peel T.E. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59(2):241–242. doi: 10.1302/0301-620X.59B2.873986. [DOI] [PubMed] [Google Scholar]
- 10.van Duijvenbode D., Stavenuiter M., Burger B., van Dijke C., Spermon J., Hoozemans M. The reliability of four widely used patellar height ratios. Int Orthop. 2016;40(3):493–497. doi: 10.1007/s00264-015-2908-2. [DOI] [PubMed] [Google Scholar]
- 11.Cabral F., Sousa-Pinto B., Pinto R., Torres J. Patellar height after total knee arthroplasty: comparison of 3 methods. J Arthroplasty. 2017;32(2):552–557. doi: 10.1016/j.arth.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Chonko D.J., Lombardi A.V.J., Berend K.R. Patella baja and total knee arthroplasty (TKA): etiology, diagnosis, and management. Surg Technol Int. 2004;12:231–238. [PubMed] [Google Scholar]
- 13.Davies G.S., van Duren B., Shorthose M. Changes in patella tendon length over 5 years after different types of knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):3029–3035. doi: 10.1007/s00167-016-4170-6. [DOI] [PubMed] [Google Scholar]
- 14.Gracitelli G.C., Pierami R., Tonelli T.A. Assessment of patellar height measurement methods from digital radiography. Rev Bras Ortop. 2015;47(2):210–213. doi: 10.1016/S2255-4971(15)30088-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lum Z.C., Saiz A.M., Pereira G.C., Meehan J.P. Patella baja in total knee arthroplasty. J Am Acad Orthop Surg. 2020;28(8):316–323. doi: 10.5435/JAAOS-D-19-00422. [DOI] [PubMed] [Google Scholar]
- 16.Bugelli G., Ascione F., Cazzella N. Pseudo-patella baja: a minor yet frequent complication of total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1831–1837. doi: 10.1007/s00167-017-4828-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.