Abstract
Diphallia or duplication of penis is extremely rare condition with a reported incidence of 1 in 5-6 million live births. Approximately around 100 cases of diphallia have been described in literature, each case have a unique presentation from associated anomalies. Clinically these patients can be classified into complete (true diphallia) or partial duplication. In true diphallia, each penis has 2 corpora cavernosa and 1 corpus spongiosum. If the duplicate penis is smaller or rudimentary with complete structure, it is described as true partial diphallia. The term bifid phallus is used if there is only one corpus cavernosum in each penis. Due to low incidence and varied presentation, not much is known about the underlying pathophysiology, management options, and outcomes. Here, we report a case of partial diphallia with associated penoscrotal transposition of 2 hemi-scrotums.
Keywords: Diphallia, Penoscrotal transposition, Bifid phallus
Background
Diphallia or duplication of penis is extremely rare condition with an estimated incidence of 1 in 5-6 million live births [1,2]. Approximately about 100 cases have been described in the literature, each case have a unique presentation, from associated various anomalies. The reported anomalies include duplication of bladder, urethra, and/or colon, anorectal malformations and vertebral anomalies [1], [2], [3].
There is no universally accepted classification system, but the cases can be broadly classified into true diphallia or bifid phallus. In true diphallia each penis has 2 corpora cavernosa and 1 spongiosum. If there is partial duplication, that is if the penis has one corpora cavernosum in each penis, it is classified as bifid phallus [1,2,4].
Due to low incidence and varied presentation, not much is known about the underlying pathophysiology, management options and outcomes [2,[5], [6], [7]]. Here, we report a case of diphallia with associated penoscrotal transposition of 2 hemiscrotums.
Case report
A 6-month-old full-term infant presented to the urology clinic for management of diphallia (Fig. 1). No reported relevant past medical history. Physical examination demonstrated 2 completely developed penis with normal looking meatus, both penises covered at the mid-part of the shaft with one penile skin shaft, penoscrotal malposition, right side scrotal skin tag, sacral dimple, and undescended testes. Both of them have urine flow from the urethras. Amniotic karyotype was 46 XY.
Fig. 1.
Physical examination demonstrated 2 completely developed penis with normal looking meatus, both penises covered at the mid-part of the shaft with one penile skin shaft and penoscrotal malposition.
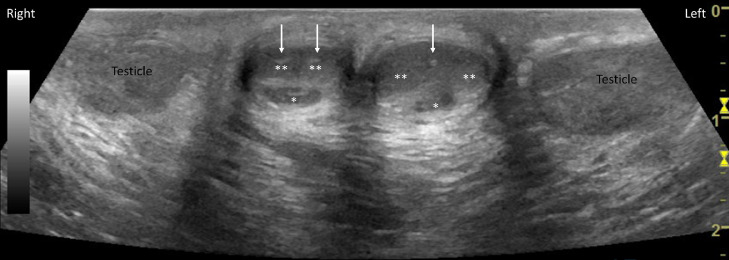
Ultrasound of the penis and scrotum (Fig. 2) demonstrated well-developed right penis, with normal corpora spongiosum and normal separate corpora cavernosa each supplied by separate cavernosal artery. Left penis demonstrated normal corpora spongiosum, and 2 separate corpora cavernosa supplied by 1 cavernosal artery. Undescended well-developed testes were also seen in the inguinal canal (Fig. 3). Doppler imaging demonstrated normal flow to both the testes.
Fig. 2.
Ultrasound of the penis and scrotum demonstrates well-developed right penis, with normal corpora spongiosum (*) and normal separate corpora cavernosa (**) each supplied by separate cavernosal artery (white arrow). Left penis demonstrated normal corpora spongiosum (*), and 2 separate corpora cavernosa (**) supplied by one cavernosal artery (white arrow).
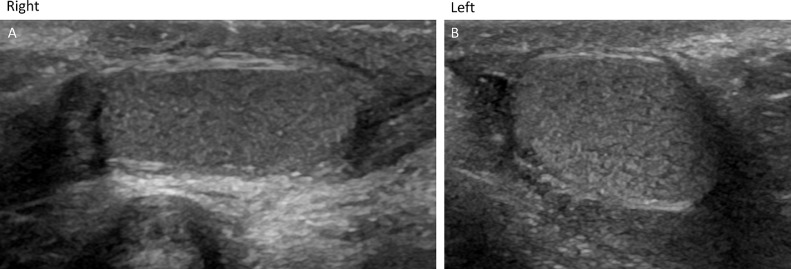
Fig. 3.
Undescended well-developed testes noted in the inguinal canal. Doppler imaging demonstrated normal flow to both the testes (not shown in the figure).
Vesicocystourethrogram (Fig. 4) demonstrates normal flow during voiding phase in the well-developed right penile urethra. The left penile urethra was relatively smaller in caliber (but patent) and proximally it terminated in the right prostatic urethra. The imaging findings were consistent with true partial diphallia.
Fig. 4.
Voiding phase of the vesicocystourethrogram demonstrates a well-developed urethra of the right penile shaft (white arrow). The left penile urethra is relatively smaller in caliber (but patent), which proximally terminates to the main prostatic urethra (yellow arrow).
The patient is scheduled for resection of left penis at the level of the base of left penile urethra.
Discussion
The first case of diphallia was reported in 1609 [4,8]. Following which approximately 100 cases have been reported in the literature with varied presentations. These cases are associated with other urogenital and anorectal malformations, such as hypospadias, epispadias, exstrophy bladder, duplication of bladder, renal agenesis, caudal duplication syndrome, imperforate anus, duplication, and triplication of the colon [1], [2], [3], [4].
Underlying mechanism is unclear, but postulated to be: (1) “separation” of the pubic tubercles during embryogenesis, in which each phallus has one corporal body and urethra, or (2) “cleavage” of the pubic tubercle in which each phallus has 2 corporal cavernous bodies and urethras [4].
Gyftopoulos et al [4] proposed classification where cases can be divided into 2 broad categories: True diphallia and bifid phallus. Both can be subclassified into partial or complete duplication. True complete diphallia will have 2 well-developed penis (with 2 corpora cavernosa and 1 corpora spongiosum). True partial diphallia will have smaller or rudimentary duplicate penis (with complete structures that is 2 corpora cavernosa and 1 corpora spongiosum). If the duplicate penis does not have all the structures, for example one corpora cavernosum they are classified as bifid phallus. Depending on the degree of separation, bifid phallus is further subclassified into complete and partial. Complete bifid phallus has separation at the base whereas, partial bifid phallus has separation at the glans [4].
Due to wide variability in presentation the management strategies differ [[5], [6], [7],9]. Surgical correction is individualized with the aim of achieving proper urinary continence and erection with adequate cosmesis [10,11].
Karagözlü et al [12] recommend complete penectomy and urethral-urethrostomy while preserving the posterior urethra may be a better choice for individualized treatment of diphallia, without the risk of damaging the sphincter and the prostate gland.
Acknowledgement
Authors would like to acknowledge sonographer Ms. Amber Karlen, RT (R), RDMS, for help with ultrasound image acquisition.
Footnotes
Declaration of competing interest: Authors have no relevant disclosures.
Patient consent: Institutional Review Board at West Virginia University authorized the publication of case report, under IRB protocol number: 2008090783.
Contributor Information
Dhairya A. Lakhani, Email: dhairya.lakhani@hsc.wvu.edu.
Mary Cannon, Email: mcannon@hsc.wvu.edu.
Sanjeev Katyal, Email: skatyal@hsc.wvu.edu.
Eyassu Hailemichael, Email: ehailemichael_hsc2@wvumedicine.org.
References
- 1.Kundal VK, Gajdhar M, Shukla AK. A rare case of isolated complete diphallia and review of the literature. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2012-008117. bcr2012008117. Published 2013 Feb 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jesus LE, Dekermacher S, Lopes E. Glans duplication: In-depth review and proposal of a new classification. J Pediatr Urol. 2017;13(2):172–176. doi: 10.1016/j.jpurol.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 3.Tirtayasa PM, Prasetyo RB, Rodjani A. Diphallia with associated anomalies: a case report and literature review. Case Rep Urol. 2013;2013 doi: 10.1155/2013/192960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhat HS, Sukumar S, Nair TB. Successful surgical correction of true diphallia, scrotal duplication, and associated hypospadias. J Pediatr Surg. 2006;41:13–14. doi: 10.1016/j.jpedsurg.2006.06.024. [DOI] [PubMed] [Google Scholar]
- 5.Gyftopoulos K, Wolffenbuttel KP, Nijman RJ. Clinical and embryologic aspects of penile duplication and associated anomalies. Urology. 2002;60(4):675–679. doi: 10.1016/s0090-4295(02)01874-5. [DOI] [PubMed] [Google Scholar]
- 6.De Oliveira MC, Ramires R, Soares J. Surgical treatment of penile duplication. J Pediatr Urol. 2010;6:257. doi: 10.1016/j.jpurol.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 7.Karaca I, Turk E, Ucan AB. Surgical management of complete penile duplication accompanied by multiple anomalies. Can Urol Assoc J. 2014;8:741–743. doi: 10.5489/cuaj.2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mirshemirani AR, Sadeghyian N, Mohajerzadeh L. Diphallus: report on six cases and review of the literature. Iran J Pediatr. 2010;20(3):353–357. [PMC free article] [PubMed] [Google Scholar]
- 9.Elsawy M, Pippi Salle JL, Abdulsalam M. Penile duplication: is it necessary to excise one of the penises? J Pediatr Urol. 2012;8:434–436. doi: 10.1016/j.jpurol.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 10.Corrêa Leite MT, Fachin CG, de Albuquerque Maranhão RF. Penile duplication without removal of corporal tissue: step by step of an excellent cosmetic result. J Pediatr Urol. 2014;10:567–570. doi: 10.1016/j.jpurol.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 11.Muramatsu M, Shishido S, Nihei H. Urinary reconstruction in vertebral, anorectal, cardiac, trachea-esophageal, renal abnormalities and limb defects association with chronic renal failure and penile duplication. Int J Urol. 2015;22:125–127. doi: 10.1111/iju.12598. [DOI] [PubMed] [Google Scholar]
- 12.Karagözlü A, Uçar M, Çelik F. Complete penile duplication with structurally normal penises: a case report. Balkan Med J. 2018;35(4):340–343. doi: 10.4274/balkanmedj.2017.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]