Abstract
Objective
For patients with atherosclerotic renal artery stenosis (ARAS), the role of percutaneous transluminal renal angioplasty (PTRA) remains inconclusive. This study aimed to comparatively evaluate the benefits of best medical therapy (BMT) plus PTRA and BMT alone in treating ARAS.
Methods
We performed a systematic review and meta-analysis, and searched for all randomized, controlled trials that reported patients with ARAS. The effectiveness and safety in the BMT plus PTRA and BMT alone groups were estimated, taking into account hypertension, stroke, renal events, cardiac events, and mortality.
Results
Nine randomized, controlled trials involving 2309 patients were included. In the BMT plus PTRA group, the incidence of refractory hypertension was significantly lower compared with that in the BMT alone group (odds ratio 0.09; 95% confidence interval 0.01, 0.70). However, there were no significant differences in the rates of stroke, renal events, cardiac events, cardiac mortality, and all-cause mortality between the two groups.
Conclusions
PTRA plus BMT improves blood pressure in patients with ARAS, but there is insufficient evidence for this therapy in improving stroke, renal events, cardiac events, and cardiac and all-cause mortality.
Keywords: Atherosclerotic renal artery stenosis, renal event, cardiac mortality, percutaneous transluminal renal angioplasty, best medical therapy, stroke, all-cause mortality
Introduction
Renal artery stenosis is caused by atherosclerotic disease in 90% of cases and by fibromuscular dysplasia in 10%.1 Among patients aged older than 66 years, the incidence of atherosclerotic renal artery stenosis (ARAS) has reached 6.8%.2 ARAS is defined as at least 50% to 70% stenosis.3 Hemodynamically significant ARAS is a leading cause of refractory hypertension, progressive deterioration of renal function, ischemic renal events, cardiac diseases, such as aortic syndrome, recurrent hyperemia heart failure, and acute coronary syndrome, and even death.4–7 In patients with refractory hypertension, ARAS is the most common secondary cause of refractory hypertension (2%–5%) which could lead to severe stroke. However, there is frequently no indication of any cause of ARAS.2,8 Approximately more than half of these patients show aggravation of stenosis within 5 years of diagnosis, of whom 15% to 20% develop end-stage renal failure or require replacement therapy.9 Among patients undergoing cardiac catheterization owing to suspected coronary artery disease, the prevalence of ARAS varies from 25% to 30%.10–14
The treatment of ARAS includes medical therapy and surgery. Currently, open surgery has been increasingly replaced with endovascular surgery because of severe trauma.15,16 Generally, percutaneous transluminal renal angioplasty (PTRA) is regarded as endovascular surgery, and is commonly accompanied by stenting. Nevertheless, the indications of PTRA remain debatable. Previous observational studies have shown that PTRA might be beneficial17–19 or detrimental20,21 to patients with ARAS. Therefore, this systematic review aimed to comparatively assess the effectiveness and safety between best medical therapy (BMT) plus PTRA and BMT alone.
Methods
Search strategy
The review protocol was developed by the steering committee and approved by the ethics review committee of Tianjin Medical University General Hospital. This meta-analysis was registered with PROSPERO (CRD42020150880). The PRISMA statement22 was followed in our literature research. Following Population, Intervention, Comparison, Outcomes, and Study design, different researchers (Y-HC and H-RP) searched PubMed, EMBASE, Web of Science, Wanfang database, and the Cochrane Library using various combinations of key words, such as “stents”, “endovascular”, “angioplasty”, “drug”, “medicine”, “medical”, “renal”, “kidney”, “stenosis” and “randomized”. Detailed search strategies are shown in Supplemental Tables 1 to 5. We were able to access five databases, including Core Collection, KCI-Korean Journal Database, Medline, Russian Science Citation Index, and SciELO Citation Index through searching the Web of Science. Additionally, a reference search was carried out to identify additional publications by screening reference lists. Only studies written in English were considered in this meta-analysis.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) diagnosis of ARAS; (2) the experimental group was BMT plus PTRA (with stents necessary) and the control group was BMT alone; (3) randomized, controlled trials (RCTs); and (4) published studies. The exclusion criteria included the following: (1) no information was available; (2) there was a significant difference in variables at baseline; (3) repeated publication data; and (4) non-RCTs. Studies that met none of the inclusion criteria or any of the exclusion criteria were excluded.
To ensure the accuracy and completeness of the data, two researchers (Y-HC and H-RP) screened all studies independently. Additionally, a third researcher (G-ZL) intervened in case of dispute arising between inclusion and exclusion criteria.
Data extraction
Data were extracted from the patients at baseline, as well as bias risk indicators, endpoint events, and conclusions. For those studies that lacked some requisite information, the author was contacted by e-mail. We also focused on baseline differences, hemodynamic assessment during follow-up, determination of endpoint events, laboratory or imaging assessment, withdrawal, and funding sources.
Statistical analysis
Review Manager 5.3 software (Cochrane Collaboration, London, United Kingdom) was used for analysis. The quality of selected studies was evaluated using the risk of bias as recommended by the Cochrane instructions. Odds ratios (ORs) and 95% confidence intervals (CIs) were adopted to evaluate the outcomes. The evaluation methods for heterogeneity used in this study included the forest plot (showing Q and I2 statistics) and the funnel chart. The fixed model was applied if I2 was <50%. Conversely, if I2 was >50%, the level of heterogeneity was treated as significant. In this circumstance, the random model was used for meta-analysis. The full text was reviewed to identify the source of the heterogeneity and subgroup analysis was conducted. Subgroup analysis was also implemented in RCTs at different follow-up time and baselines.
Results
Study selection and characteristics
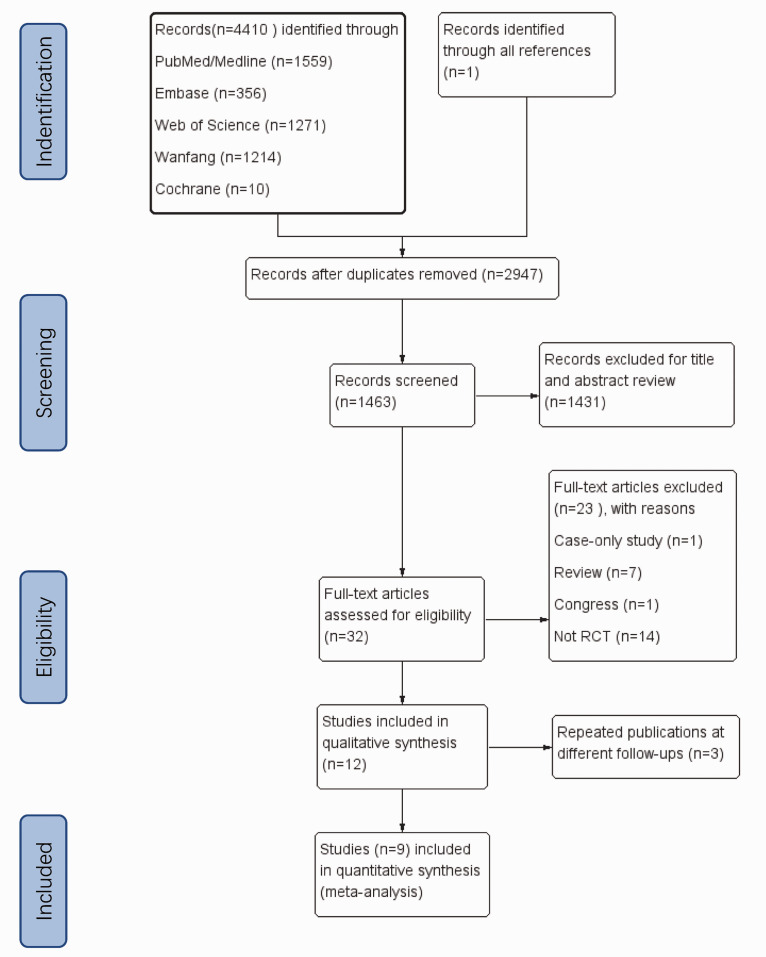
A total of 4410 studies were selected from various online databases, including 1559 articles in PubMed/Medline, 356 articles in Embase, 1271 articles in the Web of Science databases, 1214 articles in the Wanfang database, and 10 articles in the Cochrane Library. One record was identified in a search of references. A total of 9 RCTs (EMMA,23 SNRASCG,24 DRASTIC,25 STAR,26 RASCAD,27 CORAL,28 RADAR,29 NITER,30 and ASTRAL31) involving 2309 patients were chosen. Figure 1 shows a flowchart illustrating the search strategy for RCTs on PTRA and BMT in patients with ARAS.
Figure 1.
Detailed flowchart showing the search strategy for randomized, controlled trials on percutaneous transluminal renal angioplasty and best medical therapy in patients with atherosclerotic renal artery stenosis.
The baseline participants’ characteristics are shown in Table 1. There was a difference in sample size among the studies. Except for the total sample of the CORAL28 and ASTRAL31 studies, which exceeded 800, most of the other studies (EMMA,23 SNRASCG,24 RASCAD,27 and RADAR29) included less than 100 people. With regard to the mean degree of stenosis of the kidney, the RADAR study29 exceeded 80% and DRASTIC exceeded 70%, while the others showed a similar degree of stenosis >50%. The remaining features were not significantly different among the studies. The patients’ inclusion criteria in each selected study are shown in Table 2.
Table 1.
Participants’ baseline characteristics of nine included randomized, controlled trials.
|
Studies |
EMMA |
SNRASCG |
DRASTIC |
STAR |
RASCAD |
CORAL |
RADAR |
NITER |
ASTRAL |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Year of study |
1998 |
1998 |
2000 |
2009 |
2012 |
2016 |
2017 |
2018 |
2020 |
||||||||||
| Country | France | UK | The Netherlands | The Netherlands, France | Italy | USA | Germany | Italy | UK, Australia, New Zealand | ||||||||||
| Group | BMT | BMT+PTRA | BMT | BMT+PTRA | BMT | BMT+PTRA | BMT | BMT+PTRA | BMT | BMT+PTRA | BMT | BMT+PTRA | BMT | BMT+PTRA | BMT | BMT+PTRA | BMT | BMT+PTRA | |
| Patients (n) | 26 | 23 | 30 | 25 | 50 | 56 | 76 | 64 | 41 | 43 | 472 | 459 | 45 | 41 | 28 | 24 | 403 | 403 | |
| Mean age (%) | 59.2 | 59.5 | 61 | 61 | 61 | 59 | 67 | 66 | 69 | 69 | 69 | 69 | 68.3 | 71.1 | 74 | 69 | 71 | 70 | |
| Men (%) | 69 | 78 | 60 | 56 | 56 | 66 | 59 | 67 | 66 | 54 | 49 | 51 | 64.8 | 67.2 | 61 | 58 | 63 | 63 | |
| DM (%) | 15 | 26 | NM | NM | 6 | 5 | 31 | 30 | 32 | 44 | 34 | 32 | 39 | 31.1 | 57 | 67 | 29 | 31 | |
| Smoking history (%) | 62 | 65 | 50 | 36 | 70 | 82 | 68 | 72 | 60 | 47 | 32.2 | 28 | 48.8 | 55.6 | 64 | 63 | 55 | 51 | |
| Mean SBP (mmHg) | 165 | 165 | 175 | 182 | 180 | 179 | 163 | 160 | 131 | 133 | 150 | 150 | NM | NM | 149 | 148 | 152 | 149 | |
| No. of drugs | NM | NM | 2.4 | 2.4 | 2 | 2 | 2.9 | 2.8 | 2–3 | 2–3 | 2.1 | 2.1 | 2.8 | 2.4 | 3.3 | 3.3 | 2.8 | 2.79 | |
| Bilateral (%) | 0 | 0 | 53 | 48 | 22 | 23 | 46 | 50 | 5 | 9 | 18.1 | 22 | NM | NM | 46 | 50 | 61 | 58 | |
| Degree of stenosis | >50% | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 99 |
| >70% | NM | NM | NM | NM | 70 | 79 | 68 | 66 | NM | NM | NM | NM | 97.4 | 97.9 | 100 | 100 | 58 | 60 | |
| PTRA only, (%) | 91.3 | 80 | 96.4 | NM | NM | 0 | NM | 0 | 7 | ||||||||||
| Mean FU (months) | 6 | 6 | 12 | 24 | 12 | 43 | 12 | 43 | 60 | ||||||||||
BMT, best medical therapy; PTRA, percutaneous transluminal renal angioplasty; DM, diabetes mellitus; SBP, systolic blood pressure; NM, not mentioned; FU, follow-up.
Table 2.
Brief inclusion criteria in each selected study.
| Selected study | Inclusion criteria |
|---|---|
| EMMA | • Diastolic office blood pressure >95 mmHg on anti-hypertensive medication• Ccr ≥50 mL/minute• A reduction in arterial diameter of >60%• A functional kidney on the opposite side with a normal main artery |
| SNRASCG | • A minimum diastolic blood pressure of 95 mmHg on two or more anti-hypertensive medications• Stenosis of ≥50% in the arteries |
| DRASTIC | • Difficult-to-treat hypertension• Diastolic blood pressure remained at ≥95 mmHg• Unilateral or bilateral renal artery stenosis of at least 50% |
| STAR | • Ccr <80 mL/minute• A reduction in the renal artery of ≥50% |
| ASTRAL | Substantial anatomical atherosclerotic stenosis in at least one renal artery |
| RASCAD | • Ischemic heart disease• Renal artery stenosis >50% and ≤80% |
| CORAL | • Hypertension on two or more anti-hypertensive medications• Renal dysfunction (≥stage 3 chronic kidney disease) • Renal artery stenosis >60% |
| RADAR | • Renal artery stenosis >70%• Estimated glomerular filtration rate >10 mL/minute• Hypertension |
| NITER | • Glomerular filtration rate ≥30 mL/minute • Hypertension• Renal artery stenosis >70% |
Ccr, creatinine clearance.
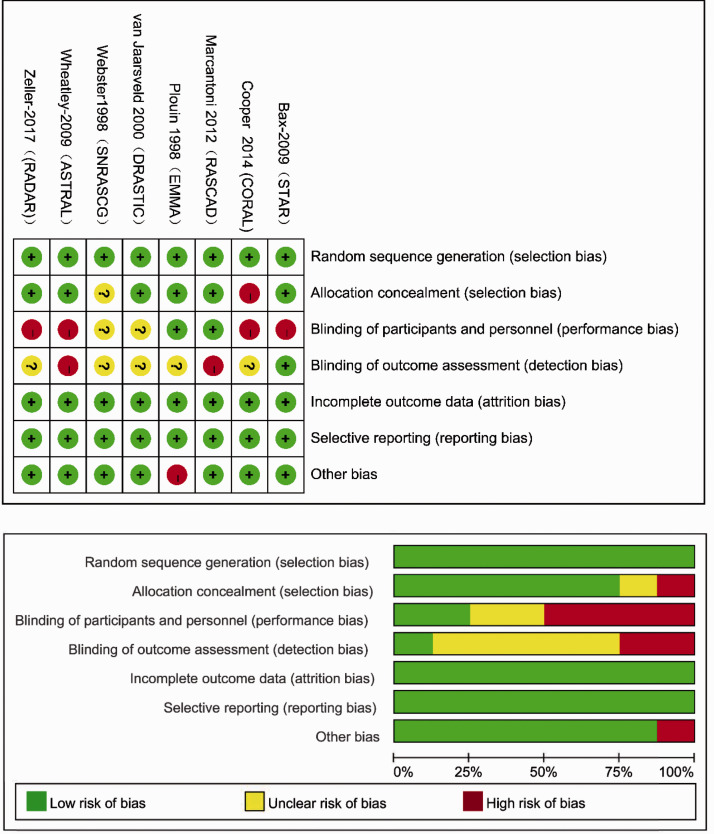
Risk of bias
The risk bias of the nine RCTs was determined by the risk of bias as recommended in the Cochrane instructions (Figure 2). Most of the items were identified as low in risk, except for some studies that were assessed as posing a high risk in performance bias and detection bias.
Figure 2.
Risk of bias graph of the nine included randomized, controlled trials.
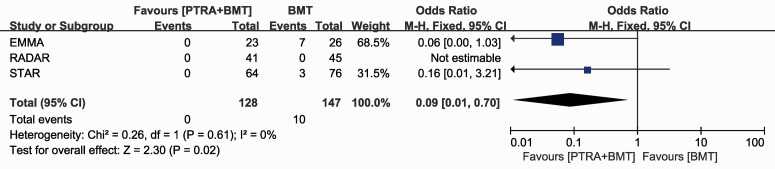
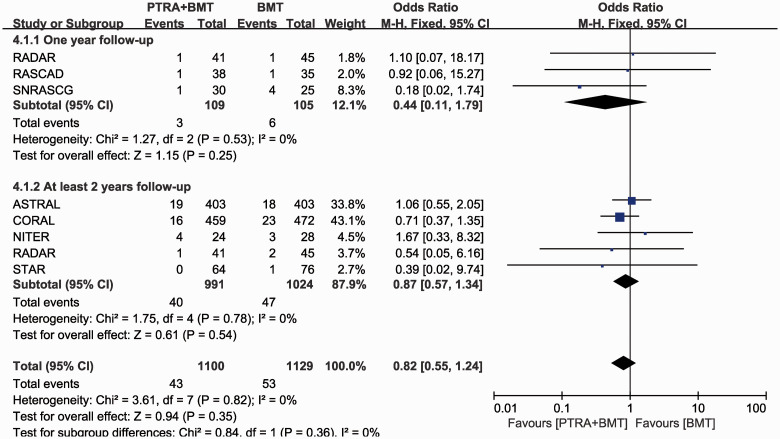
Meta-analysis results
We found that BMT plus PTRA significantly reduced the incidence of refractory hypertension compared with BMT alone within 2 years of follow-up (OR 0.09; 95% CI 0.01, 0.70; P=0.02) (Figure 3). There was no significant difference in stroke at 1 year (OR 0.44; 95% CI 0.11, 1.79) or with at least 2 years of follow-up (OR 0.87; 95% CI 0.57, 1.34) between BMT plus PTRA and BMT alone (Figure 4).
Figure 3.
Refractory hypertension within 2 years of follow-up
PTRA, percutaneous transluminal renal angioplasty; BMT, best medical therapy; M-H, Mantel–Haenszel; CI, confidence interval.
Figure 4.
Stroke in 1 year and with at least 2 years of follow-up
PTRA, percutaneous transluminal renal angioplasty; BMT, best medical therapy; M-H, Mantel -Haenszel; CI, confidence interval.
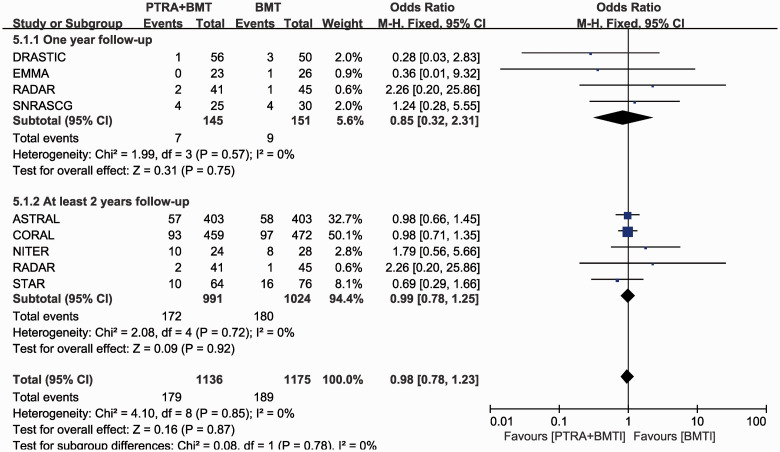
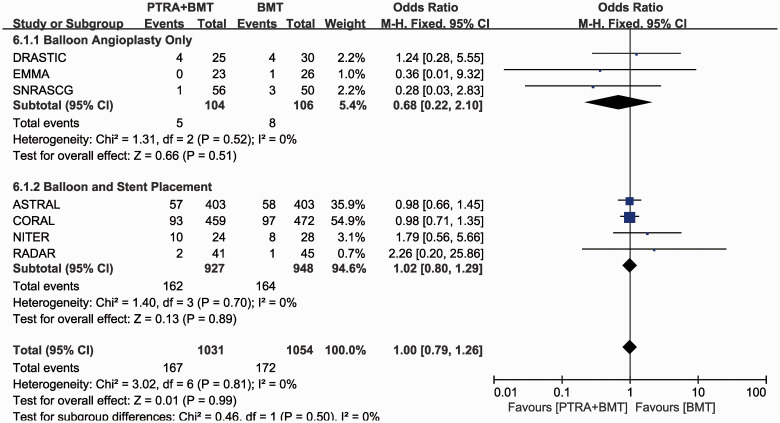
There was no significant difference in renal events at 1 year ( (OR 0.85; 95% CI 0.32, 2.31) or with at least 2 years of follow-up (OR 0.99; 95% CI 0.78, 1.25) between the two groups (Figure 5). There was also no significant difference in renal events in patients with balloon angioplasty only (OR 0.68; 95% CI 0.22, 2.10) or additional stent placement (OR 1.02; 95% CI 0.80, 1.29) (Figure 6).
Figure 5.
Renal events in 1 year and with at least 2 years of follow-up
PTRA, percutaneous transluminal renal angioplasty; BMT, best medical therapy; M-H, Mantel -Haenszel; CI, confidence interval.
Figure 6.
Renal events between balloon angioplasty only and additional stent placement
PTRA, percutaneous transluminal renal angioplasty; BMT, best medical therapy; M-H, Mantel -Haenszel; CI, confidence interval.
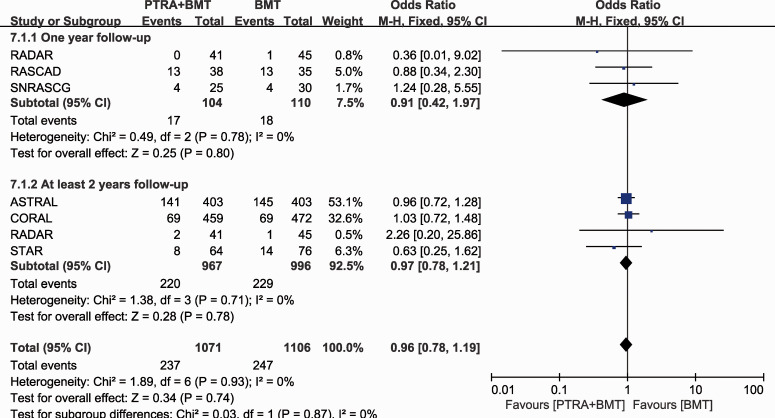
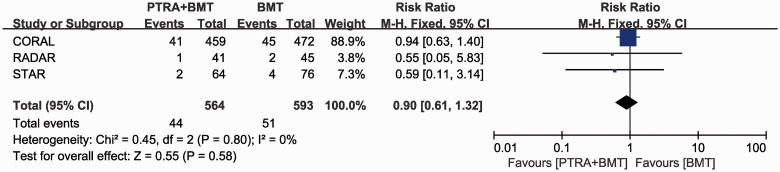
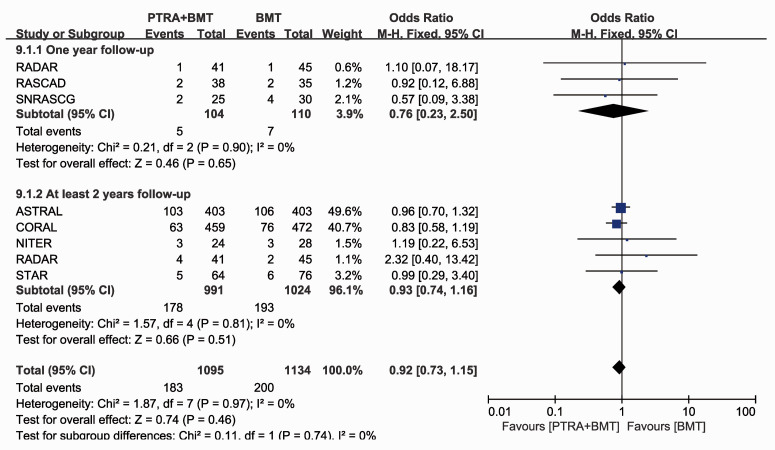
There was no significant difference in cardiac events within 1 year (OR 0.91; 95% CI 0.42, 1.97) or with at least 2 years of follow-up between the two groups (OR 0.97; 95% CI 0.78, 1.21) (Figure 7). There was also no significant difference in the incidence of cardiac mortality beyond 2 years of follow-up between the two groups (OR 0.90; 95% CI 0.61, 1.32) (Figure 8). There was no significant difference in all-cause mortality at 1 year (OR 0.76; 95% CI 0.23, 2.50) or with at least 2 years of follow-up between the two groups (OR 0.93; 95% CI 0.74, 1.16) (Figure 9).
Figure 7.
Cardiac events in 1 year and with at least 2 years of follow-up
PTRA, percutaneous transluminal renal angioplasty; BMT, best medical therapy; M-H, Mantel -Haenszel; CI, confidence interval.
Figure 8.
Cardiac mortality after 2 years of follow-up
PTRA, percutaneous transluminal renal angioplasty; BMT, best medical therapy; M-H, Mantel -Haenszel; CI, confidence interval.
Figure 9.
All-cause mortality in 1 year and with at least 2 years of follow-up
PTRA, percutaneous transluminal renal angioplasty; BMT, best medical therapy; M-H, Mantel -Haenszel; CI, confidence interval.
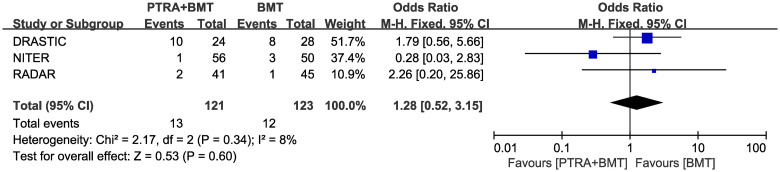
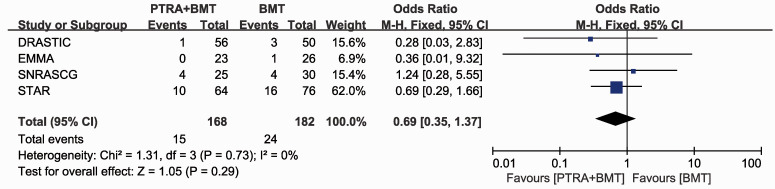
For a degree of ARAS >70%, BMT plus PTRA did not significantly reduce the incidence of renal events at 1 or 2 years of follow-up (OR 1.28; 95% CI 0.52, 3.15) compared with BMT alone (Figure 10). We also found no significant difference in renal events in patients with grade 2 hypertension between the two groups within 2 years of follow-up (OR 0.69; 95% CI 0.35, 1.37) (Figure 11).
Figure 10.
Degree of stenosis >70% in 1 year of follow-up
PTRA, percutaneous transluminal renal angioplasty; BMT, best medical therapy; M-H, Mantel -Haenszel; CI, confidence interval.
Figure 11.
Grade 2 hypertension within 2 years of follow-up
PTRA, percutaneous transluminal renal angioplasty; BMT, best medical therapy; M-H, Mantel -Haenszel; CI, confidence interval.
Discussion
In this study, we found that BMT plus PTRA significantly reduced the incidence of refractory hypertension within 2 years of follow-up compared with BMT alone. The ability of BMT plus PTRA to reduce resistant hypertension was proven by three previous RCTs.24,31,32 Our results also support recommendations of the American College of Cardiology and American Heart Association guidelines33 and the Society for Cardiovascular Angiography and Interventions appropriate use criteria34 that PTRA is beneficial in patients with resistant hypertension. Many researchers have suggested that patients showing renal blush grade,36 an abnormal renal frame count,35,36 unstable angina or congestive heart failure,37,38 or flash pulmonary edema38 have a significantly improved prognosis of hypertension.
In our meta-analysis, there was no reduction in renal events for BMT plus PTRA during the follow-up in patients with balloon angioplasty only, additional stent placement, or grade 2 hypertension. For patients with a degree of stenosis of 70% in the kidney, we still could not find any obvious reduction in renal events. Additionally, renal events resulted from diabetes, nephritis, nephropathy, heart failure, and a solitary functioning kidney. In a previous meta-analysis,39 7 studies focused on the efficacy of PTRA on patients with a solitary functioning kidney, involving 253 cases. This previous meta-analysis showed that a renal artery stent was beneficial for patients with a solitary functioning kidney regarding improved or stabilized renal function. The benefit rate was 0.77. The authors of some recent retrospective studies40–42 reached the conclusion that PTRA might be conducive to refractory control of blood pressure and kidney function, but only for those with high-risk clinical manifestations, including rapid deterioration of kidney function, episodic pulmonary edema, and post-transplant renal artery stenosis. Nevertheless, our results showed little evidence of the benefits of PTRA in improving renal function.
In our study, we did not find any significant difference in cardiac events, cardiac mortality, or all-cause mortality between PTRA plus BMT and BMT alone. Authors in a previous study found that almost half of the patients who had congestive heart failure had ARAS.8 Therefore, determining the hemodynamic significance simply by the degree of anatomical stenosis is limited.20,43,44 When ARAS is compounded by heart failure, determining which factor contributes more significantly to the occurrence of renal events is extremely difficult. Some other studies27,45 were unable to detect a clinically significant benefit from PTRA on left ventricular mass in patients with ARAS of 50% to 80%. When stenosis was ≥80% in a recently published RCT,29 there was improvement in clinical outcomes in cardiac events in 3 years after PTRA. Iwashima et al.45 found that fibromuscular dysplasia, severe ARAS (≥90%), and a higher left ventricular mass index were independent predictors of better cardiac outcomes.
Several previous meta-analyses evaluated the role of PTRA in ARAS as follows. In a meta-analysis by Natalie et al., 210 patients were recruited from three randomized studies (EMMA,23 SNRASCG,24 and DRASTIC25). They showed a more significant reduction in systolic/diastolic blood pressure (P=0.02/P=0.03) and a trend in improvement of creatinine levels in the PTRA arm (P=0.06). Shetty et al.46 identified five RCTs (EMMA,23 SNRASCG,24 DRASTIC,25 STAR,26 and ASTRAL31) and discovered an upward trend in systolic blood pressure (P=0.07), diastolic blood pressure (P=0.12), or serum creatinine levels (P=0.07) in patients who underwent PTRA compared with those who had BMT only.
There are some limitations of our review. First, in the studies that we summarized, different criteria were used to select patients for angiography. Therefore, we included a heterogeneous population. Potential confounding factors between randomly assigned treatment groups might have reduced the chance of identifying advantages of PTRA over BMT. Second, some RCTs (EMMA,23 SNRASCG,24 DRASTIC,25 STAR,26 RASCAD,27 CORAL,28 and ASTRAL31) included many patients with stenosis <70% who might not have obtained a benefit from PTRA. Third, the NITER study was terminated prematurely because of an insufficient inclusion. Finally, the criteria to preserve renal function in our included RCTs varied from each other. Therefore, we could not perform a meta-analysis on the effect of PTRA on renal function.
In conclusion, our study shows that PTRA plus BMT reduces the incidence of refractory hypertension, but does not improve the rates of stroke, renal events, cardiac events, cardiac mortality, and all-cause mortality compared with BMT alone. Because of the low strength of the meta-analysis for these findings, we believe that if candidates for PTRA are carefully selected, PTRA will have more effect.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_0300060520983585 for Use of percutaneous transluminal renal angioplasty in atherosclerotic renal artery stenosis: a systematic review and meta-analysis by Yonghui Chen, Hongrui Pan, Guangze Luo, Peng Li and Xiangchen Dai in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_0300060520983585 for Use of percutaneous transluminal renal angioplasty in atherosclerotic renal artery stenosis: a systematic review and meta-analysis by Yonghui Chen, Hongrui Pan, Guangze Luo, Peng Li and Xiangchen Dai in Journal of International Medical Research
Acknowledgement
We thank Dr. Song from the Department of Urology for proofreading the manuscript in a professional manner.
Footnotes
Author contributions: Research idea and study design: Y-HC, H-RP, and X-CD; data acquisition: Y-HC and H-RP; data analysis/interpretation: H-RP; statistical analysis: Y-HC and H-RP; manuscript writing: Y-HC, H-RP, G-ZL, and X-CD.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iDs: Guangze Luo https://orcid.org/0000-0002-2984-9281
Xiangchen Dai https://orcid.org/0000-0001-9074-6452
Supplemental material: Supplemental material for this article is available online.
References
- 1.Weber BR, Dieter RS. Renal artery stenosis: epidemiology and treatment. Int J Nephrol Renovasc Dis 2014; 7: 169–181. DOI: 10.2147/ijnrd.S40175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hansen KJ, Edwards MS, Craven TE, et al. Prevalence of renovascular disease in the elderly: a population-based study. J Vasc Surg 2002; 36: 443–451. DOI: 10.1067/mva.2002.127351. [DOI] [PubMed] [Google Scholar]
- 3.Raman G, Adam GP, Halladay CW, et al. Comparative Effectiveness of Management Strategies for Renal Artery Stenosis: An Updated Systematic Review. Ann Intern Med 2016; 165: 635–649. DOI: 10.7326/m16-1053. [DOI] [PubMed] [Google Scholar]
- 4.Kerut EK, Geraci SA, Falterman C, et al. Atherosclerotic renal artery stenosis and renovascular hypertension: clinical diagnosis and indications for revascularization. J Clin Hypertens (Greenwich) 2006; 8: 502–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baumgartner I, Lerman LO. Renovascular hypertension: screening and modern management. Eur Heart J 2011; 32: 1590–1598. DOI: 10.1093/eurheartj/ehq510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Edwards MS, Craven TE, Burke GL, et al. Renovascular disease and the risk of adverse coronary events in the elderly: a prospective, population-based study. Arch Intern Med 2005; 165: 207–213. DOI: 10.1001/archinte.165.2.207. [DOI] [PubMed] [Google Scholar]
- 7.Zalunardo N, Tuttle KR. Atherosclerotic renal artery stenosis: current status and future directions. Curr Opin Nephrol Hypertens 2004; 13: 613–621. DOI: 10.1097/00041552-200411000-00006. [DOI] [PubMed] [Google Scholar]
- 8.De Mast Q, Beutler JJ. The prevalence of atherosclerotic renal artery stenosis in risk groups: a systematic literature review. J Hypertens 2009; 27: 1333–1340. DOI: 10.1097/HJH.0b013e328329bbf4. [DOI] [PubMed] [Google Scholar]
- 9.Kądziela J, Prejbisz A, Michałowska I, et al. Relationship between hemodynamic parameters of renal artery stenosis and the changes of kidney function after renal artery stenting in patients with hypertension and preserved renal function. Blood Press 2015; 24: 30–34. DOI: 10.3109/08037051.2014.958304. [DOI] [PubMed] [Google Scholar]
- 10.Tumelero RT, Duda NT, Tognon AP, et al. Prevalence of renal artery stenosis in 1,656 patients who have undergone cardiac catheterization. Arq Bras Cardiol 2006; 87: 248–253. DOI: 10.1590/s0066-782x2006001600004. [DOI] [PubMed] [Google Scholar]
- 11.Weber-Mzell D, Kotanko P, Schumacher M, et al. Coronary anatomy predicts presence or absence of renal artery stenosis. A prospective study in patients undergoing cardiac catheterization for suspected coronary artery disease. Eur Heart J 2002; 23: 1684–1691. DOI: 10.1053/euhj.2002.3314. [DOI] [PubMed] [Google Scholar]
- 12.Rihal CS, Textor SC, Breen JF, et al. Incidental renal artery stenosis among a prospective cohort of hypertensive patients undergoing coronary angiography. Mayo Clin Proc 2002; 77: 309–316. DOI: 10.4065/77.4.309. [DOI] [PubMed] [Google Scholar]
- 13.Jean WJ, Al-Bitar I, Zwicke DL, et al. High incidence of renal artery stenosis in patients with coronary artery disease. Cathet Cardiovasc Diagn 1994; 32: 8–10. DOI: 10.1002/ccd.1810320103. [DOI] [PubMed] [Google Scholar]
- 14.Harding MB, Smith LR, Himmelstein SI, et al. Renal artery stenosis: prevalence and associated risk factors in patients undergoing routine cardiac catheterization. J Am Soc Nephrol 1992; 2: 1608–1616. [DOI] [PubMed] [Google Scholar]
- 15.Semple PF, Dominiczak AF. Detection and treatment of renovascular disease: 40 years on. J Hypertens 1994; 12: 729–734. [PubMed] [Google Scholar]
- 16.Missouris CG, Buckenham T, Cappuccio FP, et al. Renal artery stenosis: a common and important problem in patients with peripheral vascular disease. Am J Med 1994; 96: 10–14. DOI: 10.1016/0002-9343(94)90109-0. [DOI] [PubMed] [Google Scholar]
- 17.Fujihara M, Yokoi Y, Abe T, et al. Clinical outcome of renal artery stenting for hypertension and chronic kidney disease up to 12 months in the J-RAS Study - prospective, single-arm, multicenter clinical study. Circ J 2015; 79: 351–359. DOI: 10.1253/circj.CJ-14-0908. [DOI] [PubMed] [Google Scholar]
- 18.Muray S, Martin M, Amoedo ML, et al. Rapid decline in renal function reflects reversibility and predicts the outcome after angioplasty in renal artery stenosis. Am J Kidney Dis 2002; 39: 60–66. DOI: 10.1053/ajkd.2002.29881. [DOI] [PubMed] [Google Scholar]
- 19.Beutler JJ, Van Ampting JM, Van De Ven PJ, et al. Long-term effects of arterial stenting on kidney function for patients with ostial atherosclerotic renal artery stenosis and renal insufficiency. J Am Soc Nephrol 2001; 12: 1475–1481. [DOI] [PubMed] [Google Scholar]
- 20.Prince M, Tafur JD, White CJ. When and How Should We Revascularize Patients With Atherosclerotic Renal Artery Stenosis? JACC Cardiovasc Interv 2019; 12: 505–517. DOI: 10.1016/j.jcin.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 21.Isles CG, Robertson S, Hill D. Management of renovascular disease: a review of renal artery stenting in ten studies. QJM 1999; 92: 159–167. DOI: 10.1093/qjmed/92.3.159. [DOI] [PubMed] [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. J Clin Epidemiol 2009; 62: 1006–1012. DOI: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 23.Plouin PF, Chatellier G, Darne B, et al. Blood pressure outcome of angioplasty in atherosclerotic renal artery stenosis: a randomized trial. Essai Multicentrique Medicaments vs Angioplastie (EMMA) Study Group. Hypertension 1998; 31: 823–829. DOI: 10.1161/01.hyp.31.3.823. [DOI] [PubMed] [Google Scholar]
- 24.Webster J, Marshall F, Abdalla M, et al. Randomised comparison of percutaneous angioplasty vs continued medical therapy for hypertensive patients with atheromatous renal artery stenosis. Scottish and Newcastle Renal Artery Stenosis Collaborative Group. J Hum Hypertens 1998; 12: 329–335. DOI: 10.1038/sj.jhh.1000599. [DOI] [PubMed] [Google Scholar]
- 25.Van Jaarsveld BC, Krijnen P, Pieterman H, et al. The effect of balloon angioplasty on hypertension in atherosclerotic renal-artery stenosis. Dutch Renal Artery Stenosis Intervention Cooperative Study Group. N Engl J Med 2000; 342: 1007–1014. DOI: 10.1056/nejm200004063421403. [DOI] [PubMed] [Google Scholar]
- 26.Bax L, Woittiez AJ, Kouwenberg HJ, et al. Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med 2009; 150: 840–848, w150-841. [DOI] [PubMed] [Google Scholar]
- 27.Marcantoni C, Zanoli L, Rastelli S, et al. Effect of renal artery stenting on left ventricular mass: a randomized clinical trial. Am J Kidney Dis 2012; 60: 39–46. DOI: 10.1053/j.ajkd.2012.01.022. [DOI] [PubMed] [Google Scholar]
- 28.Murphy TP, Cooper CJ, Pencina K, et al. Relationship between albuminuria and renal artery stent outcomes: Results of the cardiovascular outcomes with renal artery lesions (CORAL) randomized clinical trial. Cardiovasc Intervent Radiol 2016; 39: S184. Conference Abstract. DOI: 10.1007/s00270-016-1405-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zeller T, Krankenberg H, Erglis A, et al. A randomized, multi-center, prospective study comparing best medical treatment versus best medical treatment plus renal artery stenting in patients with hemodynamically relevant atherosclerotic renal artery stenosis (RADAR) - one-year results of a pre-maturely terminated study. Trials 2017; 18: 380. DOI: 10.1186/s13063-017-2126-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Siddiqui EU, Murphy TP, Naeem SS, et al. Interaction between Albuminuria and Treatment Group Outcomes for Patients with Renal Artery Stenosis: The NITER Study. J Vasc Interv Radiol 2018; 29: 966–970. DOI: 10.1016/j.jvir.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 31.Zachrisson K, Krupic F, Svensson M, et al. Results of renal artery revascularization in the post-ASTRAL era with 4 years mean follow-up. Blood Press 2020; 29: 285–290. DOI: 10.1080/08037051.2020.1756740. [DOI] [PubMed] [Google Scholar]
- 32.Cooper CJ, Murphy TP, Cutlip DE, et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med 2014; 370: 13–22. DOI: 10.1056/NEJMoa1310753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol 2006; 47: 1239–1312. DOI: 10.1016/j.jacc.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 34.Klein AJ, Jaff MR, Gray BH, et al. SCAI appropriate use criteria for peripheral arterial interventions: An update. Catheter Cardiovasc Interv 2017; 90: E90–E110. DOI: 10.1002/ccd.27141. [DOI] [PubMed] [Google Scholar]
- 35.Leesar MA, Varma J, Shapira A, et al. Prediction of hypertension improvement after stenting of renal artery stenosis: comparative accuracy of translesional pressure gradients, intravascular ultrasound, and angiography. J Am Coll Cardiol 2009; 53: 2363–2371. DOI: 10.1016/j.jacc.2009.03.031. [DOI] [PubMed] [Google Scholar]
- 36.Naghi J, Palakodeti S, Ang L, et al. Renal frame count: a measure of renal flow that predicts success of renal artery stenting in hypertensive patients. Catheter Cardiovasc Interv 2015; 86: 304–309. DOI: 10.1002/ccd.25946. [DOI] [PubMed] [Google Scholar]
- 37.Khosla S, White CJ, Collins TJ, et al. Effects of renal artery stent implantation in patients with renovascular hypertension presenting with unstable angina or congestive heart failure. Am J Cardiol 1997; 80: 363–366. DOI: 10.1016/s0002-9149(97)00368-8. [DOI] [PubMed] [Google Scholar]
- 38.Gray BH, Olin JW, Childs MB, et al. Clinical benefit of renal artery angioplasty with stenting for the control of recurrent and refractory congestive heart failure. Vasc Med 2002; 7: 275–279. DOI: 10.1191/1358863x02vm456oa. [DOI] [PubMed] [Google Scholar]
- 39.Ma Z, Liu L, Zhang B, et al. Renal artery stent in solitary functioning kidneys: 77% of benefit: A systematic review with meta-analysis. Medicine (Baltimore) 2016; 95: e4780. DOI: 10.1097/md.0000000000004780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim S, Kim MJ, Jeon J, et al. Effects of percutaneous angioplasty on kidney function and blood pressure in patients with atherosclerotic renal artery stenosis. Kidney Res Clin Pract 2019; 38: 336–346. DOI: 10.23876/j.krcp.18.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ritchie J, Green D, Chrysochou C, et al. High-risk clinical presentations in atherosclerotic renovascular disease: prognosis and response to renal artery revascularization. Am J Kidney Dis 2014; 63: 186–197. DOI: 10.1053/j.ajkd.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 42.Mohan IV, Bourke V. The management of renal artery stenosis: an alternative interpretation of ASTRAL and CORAL. Eur J Vasc Endovasc Surg 2015; 49: 465–473. DOI: 10.1016/j.ejvs.2014.12.026. [DOI] [PubMed] [Google Scholar]
- 43.Manolis AS, Manolis AA, Melita H. Current Status of Renal Artery Angioplasty and Stenting for Resistant Hypertension: A Case Series and Review of the Literature. Curr Hypertens Rev 2017; 13: 93–103. DOI: 10.2174/1573402113666170804153026. [DOI] [PubMed] [Google Scholar]
- 44.Mitchell JA, Subramanian R, White CJ, et al. Predicting blood pressure improvement in hypertensive patients after renal artery stent placement: renal fractional flow reserve. Catheter Cardiovasc Interv 2007; 69: 685–689. DOI: 10.1002/ccd.21095. [DOI] [PubMed] [Google Scholar]
- 45.Iwashima Y, Fukuda T, Horio T, et al. Impact of Percutaneous Revascularization on Left Ventricular Mass and Its Relationship to Outcome in Hypertensive Patients With Renal Artery Stenosis. Am J Hypertens 2020; 33: 570–580. DOI: 10.1093/ajh/hpaa036%J American Journal of Hypertension. [DOI] [PubMed] [Google Scholar]
- 46.Shetty R, Biondi-Zoccai GG, Abbate A, et al. Percutaneous renal artery intervention versus medical therapy in patients with renal artery stenosis: a meta-analysis. EuroIntervention 2011; 7: 844–851. DOI: 10.4244/eijv7i7a132. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_0300060520983585 for Use of percutaneous transluminal renal angioplasty in atherosclerotic renal artery stenosis: a systematic review and meta-analysis by Yonghui Chen, Hongrui Pan, Guangze Luo, Peng Li and Xiangchen Dai in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_0300060520983585 for Use of percutaneous transluminal renal angioplasty in atherosclerotic renal artery stenosis: a systematic review and meta-analysis by Yonghui Chen, Hongrui Pan, Guangze Luo, Peng Li and Xiangchen Dai in Journal of International Medical Research