Abstract
Social capital refers to the social norms and networks that build trust and enable individuals to pursue shared objectives; it can vary considerably between communities and across time. Considerable evidence suggests that the presence of social capital at the local or state level is associated with improved individual health and lower community-level mortality, chronic illness, and diseases of despair such as substance abuse. Social capital may influence health outcomes because community-engaged institutions are more common in communities with strong social bonds and cross-sector partnerships are more easily leveraged. This study examines the impact of social capital on the effectiveness of health care organizations, specifically hospitals, in establishing population health partnerships which are critical for addressing health disparities and reducing preventable deaths. In a national sample of hospitals, we find that in communities with high social capital, hospitals are more likely to hold partnerships with public health and social service agencies. Social capital within communities may create the conditions in which hospitals are able to easily identify possible partnerships and engage in collaborative efforts to improve population health.
Keywords: Hospital partnerships, Social capital, Population health
Highlights
-
•
In areas with high social capital, hospitals are more likely to partner with public health and social service agencies.
-
•
Larger hospitals see more partnership involvement; rural hospitals are more likely to partner with public health agencies.
-
•
Social capital may facilitate identification of partnerships and engagement in collaborative efforts to improve health.
1. Introduction
The United States stands out among peer countries in the West for preventable deaths often linked to chronic diseases and widespread disparities based on race/ethnicity and class status (Nolte & McKee, 2011). The Centers for Disease Control (CDC) estimates that 90% of the 3.5 trillion dollars spent on health care services in the U.S. is for chronic illnesses, many of which are preventable (CDC, 2020). Health disparities in particular cost Americans more than $100 billion each year (Artiga, Orgera, & Pham, 2020). To improve health outcomes, experts recommend an expanded health care approach which includes interventions to address upstream social determinants of health (Begun & Potthoff, 2017; Williams, Costa, Odunlami, & Mohammed, 2008).
Because the majority of health care dollars are concentrated in hospitals in the U.S., hospitals have been identified as key partners to help reduce preventable death (Mays, Mamaril, & Timsina, 2016). Recommendations for improving health outcomes, accordingly, involve strengthening connections between health care organizations and the public health system. Research shows that social capital—the networks and shared values that reflect community level trust needed to pursue shared objectives—is key to understanding and shaping change efforts (Putnam, 1995, 2002). Although engaging hospitals to participate in broader public health networks is critical, there is still considerable variation in the number of hospitals who are partnering with public health and community organizations and in the types of relationships developed to improve health outcomes and reduce health disparities (Hogg & Varda, 2016; Singh, Cramer, & Young, 2018). This paper examines hospitals’ decisions to partner with public health and other community organizations using the theoretical framework of social capital.
2. Methods
2.1. Data sources
Data for this study were sourced from multiple secondary data sets. For hospital data, we used data from the 2017 American Hospital Association Annual Survey indicating the presence of hospital partnerships with public health agencies, social service agencies, nonprofit organizations, governmental organizations, and other health care organizations. The American Hospital Association collects self-reported data by surveying over 6200 hospitals annually and produces the most comprehensive dataset on the characteristics and behaviors of U.S. hospitals and systems. This is the only available data set providing information on these types of partnerships across the U.S. hospital population. We also incorporated key hospital characteristics from this data set, including ownership status of hospitals, system membership status, bed size, and community outreach efforts.
Our social capital variables came from the Northeast Regional Center for Rural Development's “Social Capital Variables for 2014” dataset. This index allows for the comparison of relative levels of social capital across different communities in the United States through consideration of four data sources: voter turnout, census response rate, nonprofit organizations per capita, and associations per capita (e.g., religious, civic, social, business, political, professional, labor, sports associations) (Brewster, Lee, Curry, & Bradley, 2019). We aggregated county level variables provided by this dataset to the state level for use in our analysis. Other data sources provided community characteristics. The 2017 Area Health Resource File data provided the unemployment rate, as well as the designation of rural location (with counties considered as non-rural if they were coded as 1 or 2 on the continuum, or as rural if they were 3 or higher).
2.2. Measures
The dependent variables for this study are whether hospitals have partnerships across five categories: public health agency partnerships, social service agency partnerships, nonprofit organization partnerships, partnerships with other governmental organizations (besides those included in a previous category), and partnerships with other health care organizations. This question was asked as: “Describe the extent of your hospital's current partnerships with the following types of organizations for community or population health improvement initiatives.” The American Hospital Association Annual Survey collects information on ten types of partnerships (as well as allowing for hospitals to explain “other”). We selected the five categories most relevant to our research question, which was informed by previous research by Mays et al. (2016) and Mays and Scutchfield (2010) suggesting these are the most common types of partnerships (Mays et al., 2016; Mays & Scutchfield, 2010). For each type of partnership, hospitals could respond that they had no partnership, a collaboration, or a formal alliance. For the purposes of our analysis, we have created a dichotomous variable for each category of partnership, collapsing collaboration and alliance, to measure whether there was participation or no participation in a partnership. Our reason for this is that not all organizations may be equally suited toward formal alliances, which AHA defines as “formalized partnerships (or binding agreements).”
The key independent variable consists of a social capital index calculated at the state level. This index, sourced from the Northeast Regional Center for Rural Development, was created by bringing four factors together: an aggregate measure of religious, civic, business, political, professional, and recreational establishments by population; voter turnout; census response rate; and the number of non-profit organizations (excluding those with an international approach). To calculate the index, the four factors are standardized to have a mean of 0 and a standard deviation of 1. Additionally, we control for a range of hospital and community characteristics, as indicated in the descriptive statistics table (see Table 1). Hospital characteristics include variables such as size, ownership status, and whether a hospital participates in community outreach (e.g., interacting with the community to identify those in need of services, alerting persons and their families to the availability of services, etc.), among others.
Table 1.
Descriptive statistics of hospital partnership Participation, 2017 (n = 6882).
|
Full sample (all hospitals) |
Analytic sample (general medical centers, excluding federal hospitals) |
|||||
|---|---|---|---|---|---|---|
| N | % | Missing data | N | % | ||
| U·S. Hospitals | 6882 | 2885 | ||||
| Partnerships | ||||||
| General medical hospitals | 4665 | 67.79% | 0 | 2885 | 100% | |
| Hospital partners with public health | 2878 | 80.64% | 3313 | 2455 | 85.10% | |
| Hospital partners with social services | 2648 | 74.65% | 3335 | 2278 | 78.96% | |
| Hospital partners with nonprofits | 2672 | 75.42% | 3339 | 2309 | 80.03% | |
| Hospital partners with state or local government | 2405 | 68.11% | 3351 | 2089 | 72.41% | |
| Hospital partners with other health care organizations | 2772 | 77.43% | 3302 | 2335 | 80.94% | |
| Hospital ownership; nonprofit | 3133 | 45.52% | 0 | 2021 | 70.05% | |
| Hospital member; multihospital system | 4092 | 59.46% | 0 | 1935 | 67.07% | |
| Hospital size | ||||||
| Beds fewer than 50 | 2242 | 32.58% | 0 | 926 | 32.10% | |
| Beds 50-199 | 2452 | 35.63% | 0 | 999 | 34.63% | |
| Beds 200-399 | 999 | 14.52% | 0 | 573 | 19.86% | |
| Beds greater than 400 | 1189 | 17.28% | 0 | 387 | 13.41% | |
| Hospital does community outreach | 3053 | 71.33% | 2602 | 2390 | 82.84% | |
|
Hospital in rural location |
2477 |
36.03% |
7 |
1122 |
38.89% |
|
|
Mean |
Std Dev |
Missing data |
Mean |
Std Dev |
||
| State social capital index | −0.1 | 0.71 | 0 | −0.01 | 0.72 | |
| County percent unemployed | 4.51% | 1.45 | 3 | 4.40% | 1.28 | |
Data sources: American Hospital Association Annual Survey 2017, Northeast Regional Center for Rural Development Social Capital Resources, Area Health Resource File.
2.3. Sample
The American Hospital Association 2017 Annual Survey dataset provides us with a sample of 4665 general medical hospitals. However, about one-third to one-fourth of the hospitals did not respond to the full range of questions regarding each category of partnerships. We therefore removed the hospitals that did not provide responses for all six categories (1738 hospitals), due to missing data. After also excluding 42 federal hospitals, our final analytic sample was 2885 hospitals from across the United States. A t-test analysis of the hospitals with missing data did show some significant differences from the analytic sample. The hospitals removed for missing data tended to be significantly smaller (average bed size of 126 compared to 191), with significantly lower social capital scores (-.14 compared to -.01), and significantly higher county unemployment (4.66% compared to 4.4%). They were also significantly less likely to be nonprofit (49% nonprofit compared to 70%); less likely to be a system member (61% compared to 67%); and significantly more likely to be rural (46% compared to 39%).
2.4. Analysis
In addition to descriptive statistics, we employ logistic regression to assess a relationship between the level of social capital within a county and hospital partnerships by type. Each category of partnership is assessed in a separate model, resulting in five models. Each model includes consideration of the primary relationship between the social capital index and the partnership type while also controlling for hospital and community characteristics.
3. Theory
3.1. Hospital partnerships and population health
In the last two decades, recognition has grown within health care organizations that interventions focused on community or population health are necessary to make health care services more efficient and reduce unnecessary spending. The metrics of efficiency and spending have come under more scrutiny with the development of value-based payment mechanisms to replace traditional fee-for-service arrangements. These efforts have also been bolstered by new community benefit requirements included in the Affordable Care Act (ACA). The ACA requires nonprofit hospitals, nearly two-thirds of hospitals in the US, to regularly assess and report on pressing community health needs (Franz, Cronin, & Singh, 2019; Pennel, McLeroy, Burdine, Matarrita-Cascante, & Wang, 2016). More specifically, nonprofit hospitals must complete a Community Health Needs Assessment (CHNA) every three years and propose specific interventions to improve community health in a corresponding implementation strategy in exchange for tax exemption (James, 2016).
Changes in health care reimbursement and policy have also coincided with the development of a new paradigm in medicine; population health, a close cousin to public health, aims to improve “the health outcomes of a group of individuals, including the distribution of such outcomes within the group” (Kindig & Stoddart, 2003, p. 381). The growing focus on population health has not only led to new interventions to address the health of communities, above and beyond that of individual patients, but has also contributed to the growth of new population health departments within hospitals, new personnel, and new collaborative partnerships with government, nonprofit, and other community organizations.
The growth in these collaborative efforts in the past two decades reflects the increased recognition that poor health and inequality are the result of a multitude of factors – including many social and cultural factors which fall outside the traditional expertise of the health sector (Trujillo & Plough, 2016). The impact of social determinants on health status and outcomes has been widely established. However, it is also recognized that a hospital's ability and capacity to act alone to address these concerns may be limited, underscoring the need for novel partnerships between hospitals and a wide range of public health, social service, and community-based organizations which may have greater impact on population health (Henize, Beck, Klein, Adams, & Kahn, 2015; Mattessich & Rausch, 2014; Mays & Scutchfield, 2010).
Important to note is that the community benefit expectations for nonprofit hospitals to complete CHNAs include a requirement to consult outside stakeholders and at least one public health agency, which may encourage the development or strengthening of cross-sector partnerships (Somerville, Seeff, Hale, & O'Brien, 2015). Indeed, there is growing evidence that hospitals are developing new partnerships after the ACA expanded community benefit requirements and that collaborating with health departments in particular leads to hospitals investing more dollars into community health activities (Carlton & Singh, 2018). Additional evidence suggests that collaborating with a local health department may improve the overall quality of the CHNA which suggests that partnerships may help hospitals adequately assess local health needs and address them through collaborative strategies (Pennel, McLeroy, Burdine, & Matarrita-Cascante, 2015). Further, existing research suggests that hospital programs that involve partnerships (rather than programs undertaken by the hospital alone) may be more effective and include outreach to the community, community involvement, staff and funding, and provide benefit to underserved populations at higher rates than sole undertakings (Burke et al., 2014). Moving beyond community benefit which is specific to nonprofit hospitals, evidence suggests that U.S. communities that perform well on both health care costs and utilization may be at least partially explained by effective cross-sector partnerships between hospitals and other organizations (Brewster, Brault, Tan, Curry, & Bradley, 2018).
A number of factors have been proposed as encouraging hospitals to participate in external partnerships. As mentioned previously, new ACA requirements for nonprofit hospitals require consultation of public health departments and may encourage new collaborations (Somerville et al., 2015). Other studies suggest that institutional and community characteristics may also shape hospital partnerships and that hospitals with strong partnerships tend to be larger, not-for-profit, members of a health system, teaching-affiliated, and located in urban areas (Park, Hamadi, Apatu, & Spaulding, 2019). Still other scholars note the importance of policy and administrative actions to support public health partnerships and the broader social environment which may strengthen norms around collaboration (Brewster, Brault, et al., 2018; Mays & Scutchfield, 2010).
3.2. The proposed role of social capital
One potential social factor that has been relatively understudied in relationship to hospital participation in population health networks is social capital. Social capital refers to the social norms and networks that build trust and enable individuals to pursue shared objectives; social capital has been shown to vary considerably between communities and across time (Coleman, 1988; Putnam, 1995, 2002). Considerable evidence suggests that the presence of social capital at the local or state level is associated with improved individual health and lower community-level mortality, chronic illness, and diseases of despair such as substance abuse (Kawachi, Kennedy, Lochner, & Prothrow-Stith, 1997; Yang, Jensen, & Haran, 2011; Zoorob & Salemi, 2017). Social capital may influence health outcomes because community-engaged institutions are more common in communities and countries with strong social bonds, and these community-engaged institutions may include population health partnerships (Hoi, Wu, & Zhang, 2018). Social capital measures focus on a combination of individual and community level indicators—behaviors, perspectives, and number of various types of organizations—in order to understand the relationships that build social trust necessary for these collaborations. In the assessment of the value of networks, the organizational-level relationships of hospitals can reflect engagement of a wide range of stakeholders that contributes to trust-building. Few studies, however, have specifically assessed the impact of social capital on the effectiveness of health care organizations in participating in population health interventions (Ko, Derose, Needleman, & Ponce, 2014; Lee, Chen, & Weiner, 2004).
Social capital within communities may create the conditions in which hospitals are able to easily identify possible partnerships and engage in collaborative efforts to improve population health. One key study found that hospitals located in areas with low social capital had higher rates of readmissions (Brewster et al., 2019) which are associated with a number of poor outcomes, including increased health care expenditures and patient mortality (Alban, Nisim, Ho, Nishi, & Shabot, 2006; Jencks, Williams, & Coleman, 2009). A subsequent study found that hospitals’ informal partnerships also predicted readmission rates, suggesting that partnerships may mediate the relationship between social capital and poor health outcomes in US communities (Brewster, Kunkel, Straker, & Curry, 2018).
The aim of this study is to build on existing research to examine the extent to which community-level social capital is associated with hospital partnerships beyond existing institutional and community factors that have been identified. Using secondary data on hospital partnerships, we explore whether social capital predicts hospitals’ engagement in different types of external partnerships. We hypothesize that social capital will be positively related to hospital participation in partnerships and that this relationship will be strongest in partnerships that enable hospitals to engage in non-traditional health care activities, such as with public health or social service organizations. These findings are critical as public health policies could target communities and states where hospitals are in most need of support to carry out population health activities.
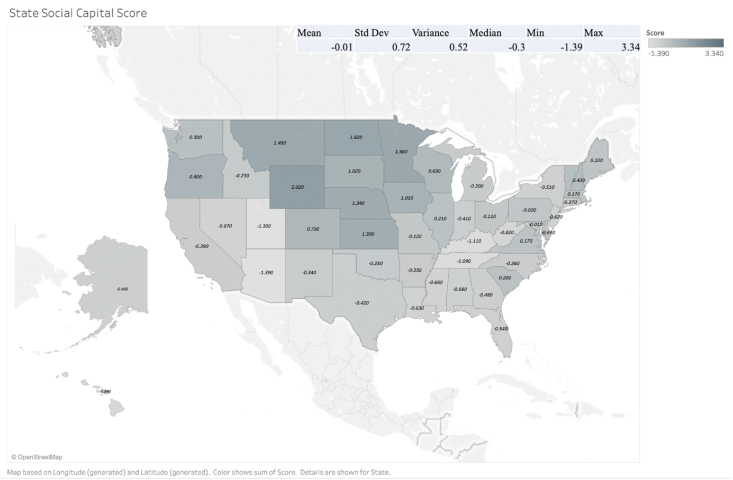
4. Results
Descriptive results show that about 70% of counties in the U.S. have general medical hospitals. Of the 2885 general hospitals in our sample, we found that 85% partner with public health departments; 80% partner with nonprofits in the community; 81% partner with other health care organizations; 79% partner with social service agencies; and 72% partner with local government. The average state social capital score is -.01, with a median of -.3 and a range of −1.39–3.34. Among states with the highest social capital are North Dakota (1.62), Wyoming (2.02), and the District of Columbia (3.34); the three lowest are Arizona (−1.39), Utah (−1.30), and Kentucky (−1.11). (See Table 1; Fig. 1.).
Fig. 1.
State social capital score.
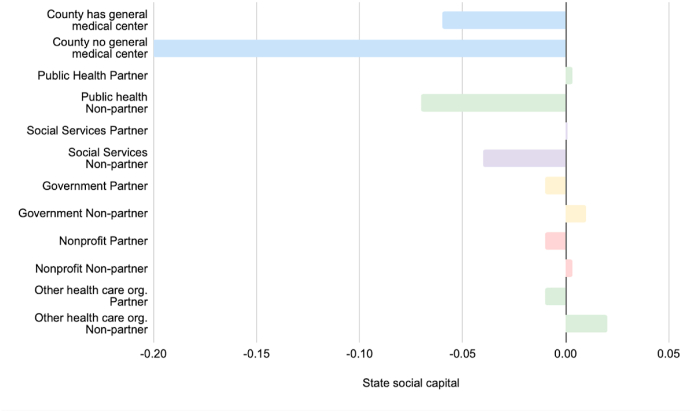
On average, we see that counties with general medical centers are positively and significantly correlated with social capital scores. Additionally, counties where hospitals partner with public health agencies also have higher social capital on average (See Fig. 2.).
Fig. 2.
Mean state social capital by indicator.
Logistic regression results indicate that state social capital is significantly and positively associated with hospitals partnering with public health and social services agencies, when controlling for ownership, system membership, size, community engagement, and county characteristics. (The relationships with other types of partnerships were also positive but did not show statistical significance.) Rural location and unemployment rate also showed significant relationships, positive and negative respectively, with public health partnerships. Additionally, hospital community engagement is significant and positively associated with each of the five types of partnerships. Other hospital characteristics that were found to have significant relationships to hospital partnerships included nonprofit status and larger size. Both were positively associated with all five types of partnerships (See Table 2.).
Table 2.
Logistic regression of partnership types by state and hospital Characteristics, 2017 (n = 2885).
| Partnerships | Public health |
Social services |
Nonprofit organizations |
|||
|---|---|---|---|---|---|---|
| N = 2885 |
95% Conf. | N = 2885 |
95% Conf. | N = 2885 |
95% Conf. | |
| OR (SE.) | OR (SE.) | OR (SE.) | ||||
| State social capital score | 1.18 (0.10)* | [0.05–1.00] | 1.28 (0.10)** | [0.00–1.10] | 1.15 (0.09) | [0.07–0.99] |
| Ownership: Nonprofit | 2.05 (0.24)*** | [0.00–1.63] | 2.01 (0.21)*** | [0.00–1.64] | 2.68 (0.28)*** | [0.00–2.18] |
| System member | 1.40 (0.17)** | [0.01–1.11] | 1.55 (0.16)*** | [0.00–1.26] | 1.64 (0.18)*** | [0.00–1.33] |
| Bed size 50-199 | 1.36 (0.18)* | [0.02–1.05] | 1.32 (0.16)* | [0.02–1.05] | 1.43 (0.17)** | [0.00–1.13] |
| Bed size 200-399 | 1.62 (0.29)** | [0.01–1.14] | 1.63 (0.26)** | [0.00–1.19] | 1.8 (0.30)*** | [0.00–1.3] |
| Bed size larger than 400 | 4.70 (1.29)*** | [0.00–2.74] | 4.91 (1.23)*** | [0.00–3.01] | 5.55 (1.51)*** | [0.00–3.26] |
| Hospital community outreach | 2.12 (0.27)*** | [0.00–1.66] | 2.31 (0.26)*** | [0.00–1.85] | 1.99 (0.23)*** | [0.00–1.58] |
| Rural classified county | 1.36 (0.18)* | [0.02–1.05] | 0.90 (0.1) | [0.36–0.71] | 0.82 (0.10) | [0.10–0.65] |
| County percent unemployed |
0.91 (0.04)* |
[0.03–0.84] |
0.98 (0.04) |
[0.59–0.91] |
0.98 (0.04) |
[0.58–0.90] |
| State and local government | Other health care organizations | |||||
| N = 2885 | 95% Conf. | N = 2885 | 95% Conf. | |||
| OR (SE.) |
OR (SE.) |
|||||
| State social capital score | 1.10 (0.07) | [0.16–0.96] | 1.08 (0.08) | [0.30–0.93] | ||
| Ownership: Nonprofit | 1.34 (0.13)** | [0.00–1.11] | 1.87 (0.2)*** | [0.00–1.52] | ||
| System member | 1.30 (0.12)** | [0.01–1.08] | 0.99 (0.11) | [0.90–0.79] | ||
| Bed size 50-199 | 1.27 (0.14)* | [0.03–1.03] | 1.4 (0.17)** | [0.00–1.11] | ||
| Bed size 200-399 | 1.37 (0.19)* | [0.02–1.04] | 2.24 (0.38)*** | [0.00–1.60] | ||
| Bed size larger than 400 | 3.44 (0.67)*** | [0.00–2.35] | 3.88 (0.91)*** | [0.00–2.44] | ||
| Hospital community outreach | 1.95 (0.21)*** | [0.00–1.57] | 1.88 (0.22)*** | [0.00–1.50] | ||
| Rural classified county | 0.90 (0.09) | [0.31–0.73] | 0.84 (0.1) | [0.15–0.67] | ||
| County percent unemployed | 1.00 (0.04) | [0.94–0.93] | 0.99 (0.04) | [0.80–0.92] | ||
* = p < .05; ** = p < .01; *** = p < .001.
5. Discussion
The aim of this study was to examine if the presence of state-level social capital creates conditions in which hospitals are more likely to leverage external partnerships to improve population health. We found that greater social capital at the state level was associated with hospitals partnering more often with both public health agencies and social services, independent of other institutional and community-level factors. By examining hospital-community partnerships and levels of social capital, we have further insight into how to facilitate hospital involvement in population health partnerships and where hospitals may need additional support to identify and leverage partners for population health improvement.
Although social capital was not a significant predictor of all types of hospital partnerships, the significant association with both public health and social service organizations is important. While the survey does not define these categories further, we can assume from the response choices that public health and social service organizations include agencies such as a county health department or an office on aging. This reflects the type of partnerships that develop from Community Health Needs Assessments, which are required of both public health agencies and nonprofit hospitals. These findings also suggest that hospitals are seeking out partnerships with agencies that may help them address community health issues that are outside of their traditional expertise, such as social determinants of health and mental health. Given the evidence that hospitals face considerable barriers to moving upstream in their community benefit work (Begun, Kahn, Cunningham, Malcolm, & Potthoff, 2018), social capital's role in fostering these types of partnerships is important. If these barriers are more easily overcome in communities with more social capital, this has significant implications for public health interventions to improve collaboration related to population health. This also comports with previous studies that suggest the need for state and national policies to support rural and low-volume hospitals in building partnership networks, particularly in underserved areas (Park et al., 2019). For example, if there are a limited number of community organizations or minimal civic engagement, initiatives such as intervention mapping (Fernandez, Ruiter, Markham, & Kok, 2019) may help hospitals identify and collaborate with external organizations in areas where social bonds are not as strong.
When we examined specific hospital characteristics in relationship to hospital partnerships, we found important differences in how different types of hospitals fared with engaging in population health partnerships. The analysis showed that nonprofit status and hospital size (defined by the number of beds) were both associated with a greater likelihood to partner in all five categories. Nonprofit hospitals have long been subject to a number of community benefit regulations in exchange for tax exemption, including new requirements under the ACA to consult public health agencies as part of their CHNA, which helps explain why they are more likely to engage a number of external partners in pursuit of local population health improvement. Although small hospitals may stand to benefit considerably from partnerships with other organizations, our findings are in line with previous studies which suggest that larger hospitals are more likely to engage in population health and community benefit activities (Park et al., 2019). Hospital size, in other words, is an indicator of general capacity and resources available to develop and maintain community partnerships.
Despite the robust relationship between hospital size and partnering behavior, we find that rural hospitals were significantly more likely to enact partnerships with public health agencies than hospitals located in urban areas. States with high social capital are disproportionately rural (Social Capital Project, 2018), which may help explain this partnering behavior. In addition, rural hospitals may need to engage in more health education-type activities because of an absence of other community organizations that serve this purpose, in contrast to more densely populated areas. Although rural hospitals tend to be smaller and less capitalized in regard to financial resources, it may be that stronger social bonds, both on the individual and institutional level, help rural hospitals develop partnerships with public health organizations specifically. Because public health organizations exist in rural communities as well as urban communities, this may be one area where rural hospitals are able to leverage external partnerships successfully to improve local population health.
5.1. Limitations
This study had several limitations that are important to note. First, we had to remove a number of hospitals who did not complete the questions related to partnerships on the AHA annual survey. The hospitals removed for missing data tended to be significantly smaller, located in states with significantly lower social capital scores, and in communities with higher unemployment, suggesting that the number of hospitals undertaking partnerships may be overestimated. Hospitals without partnerships may be less likely to complete the section on partnerships, but because no other comprehensive data source on hospital partnerships is currently available, we are limited to understanding the partnering behavior of hospitals who completed the full survey. Second, we found that hospitals who are highly engaged in community improvement efforts are more likely to partner, but it is not possible to ascertain the direction of this relationship with cross-sectional data. Because partnership data only recently became available through the AHA survey, future studies should analyze multiple years of data to assess this relationship further. Additionally, it is important to note that all survey information from AHA is self-reported, thus we must rely on hospitals to be candid and comprehensive in their responses. Our use of these survey responses also does not allow for analysis of the strength or quality of the reported partnerships. There is also the possibility that the way the question regarding partnerships is phrased, which assumes partnerships exist, creates expectations for hospitals to report partnerships.
Another recognized limitation of this study is that the measurement of social capital at the state level cannot account for variation in social capital at the community level. It is possible that hospital partnerships reflect social capital in the more immediate community, but robust measures of social capital are challenging to measure at the local level. The use of county-level data presented challenges in itself. One such challenge was that using county-level data would mean losing any measure of social capital for counties that do not have hospitals residing in them. Relatedly, we feel that it is important to emphasize that many hospitals are regional health care providers, with extensive service areas. Therefore, they may be influenced by resources beyond their own county, including surrounding counties that may not have hospitals themselves. On balance, we felt that the state-level data for social capital provided a fuller picture, and our findings suggest that social capital within the broader region is associated with hospital behavior, independent of local community level factors such as unemployment. Developing additional means and methods of assessing social capital, in a way that is more adaptable to institutions such as hospitals, would be a worthwhile goal of future research.
5.2. Conclusion
Hospital participation in local population health networks is critical to improving health care services and health equity in the United States. Our findings suggest that beyond institutional differences, the presence of social capital in the surrounding state is associated with hospitals fostering external partnerships critical to population health improvement. Important to note is that social capital seems to support partnerships with public health and social service organizations--two areas where hospitals have traditionally faced barriers in developing community health activities. The presence of social capital may be critically important in areas where organizational partners are scarce, such as rural or underserved communities. Public health initiatives aimed at improving cross-sector collaboration among different types of organizations should provide support to strengthen social networks in areas where social bonds are not as strong. Such interventions may help hospitals successfully identify and leverage partnerships to adopt and implement successful population health initiatives.
Author statement
Cory E. Cronin: Conceptualization, Data curation, Project administration, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. Berkeley Franz: Conceptualization, Project administration, Writing – original draft, Writing – review & editing. Sarah Garlington: Conceptualization, Project administration, Writing – original draft, Writing – review & editing
Financial support
None.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Alban R.F., Nisim A.A., Ho J., Nishi G.K., Shabot M.M. Readmission to surgical intensive care increases severity-adjusted patient mortality. The Journal of Trauma, Injury, Infection, and Critical Care. 2006;60(5):1027–1031. doi: 10.1097/01.ta.0000218217.42861.b7. [DOI] [PubMed] [Google Scholar]
- Artiga S., Orgera K., Pham O. Disparities in health and health care: Five key questions and answers. 2020. https://www.kff.org/disparities-policy/issue-brief/disparities-in-health-and-health-care-five-key-questions-and-answers/ Retrieved from.
- Begun J.W., Kahn L.M., Cunningham B.A., Malcolm J.K., Potthoff S. A measure of the potential impact of hospital community health activities on population health and equity. Journal of Public Health Management and Practice. 2018;24(5):417–423. doi: 10.1097/PHH.0000000000000617. [DOI] [PubMed] [Google Scholar]
- Begun J.W., Potthoff S. Moving upstream in U.S. hospital care toward investments in population health. Journal of Healthcare Management/American College of Healthcare Executives. 2017;62(5):343–353. doi: 10.1097/JHM-D-16-00010. [DOI] [PubMed] [Google Scholar]
- Brewster A.L., Brault M.A., Tan A.X., Curry L.A., Bradley E.H. Patterns of collaboration among health care and social services providers in communities with lower health care utilization and costs. Health Services Research. 2018;53:2892–2909. doi: 10.1111/1475-6773.12775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewster A.L., Kunkel S., Straker J., Curry L.A. Cross-sectoral partnerships by Area Agencies on Aging: Associations with health care use and spending. Health Affairs. 2018;37(1):15–21. doi: 10.1377/hlthaff.2017.1346. [DOI] [PubMed] [Google Scholar]
- Brewster A.L., Lee S., Curry L.A., Bradley E.H. Association between community social capital and hospital readmission rates. Population Health Management. 2019;22(1):40–47. doi: 10.1089/pop.2018.0030. [DOI] [PubMed] [Google Scholar]
- Burke J.G., Truong S., Albert S., Steenrod J., Gibert C., Folb B. What can Be learned from the types of community benefi t programs that hospitals already have in place? Journal of Health Care for the Poor and Underserved. 2014;25 doi: 10.1353/hpu.2014.0058. [DOI] [PubMed] [Google Scholar]
- Carlton E.L., Singh S.R. Joint community health needs assessments as a path for coordinating community-wide health improvement efforts between hospitals and local health departments. American Journal of Public Health. 2018;108(5):676–682. doi: 10.2105/AJPH.2018.304339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC Health and economic costs of chronic diseases. 2020. https://www.cdc.gov/chronicdisease/about/costs/index.htm Retrieved September 7, 2020, from.
- Coleman J.S. Social capital in the creation of human capital. American Journal of Sociology. 1988;94:S95–S120. 1988. [Google Scholar]
- Fernandez M.E., Ruiter R.A.C., Markham C.M., Kok G. Intervention mapping: Theory-and evidence-based health promotion program planning: Perspective and examples. Frontiers in Public Health. 2019;7(AUG):209. doi: 10.3389/fpubh.2019.00209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franz B., Cronin C.E., Singh S. Are nonprofit hospitals addressing the most critical community health needs that they identify in their community health needs assessments? Journal of Public Health Management and Practice. 2019;1 doi: 10.1097/phh.0000000000001034. [DOI] [PubMed] [Google Scholar]
- Henize A.W., Beck A.F., Klein M.D., Adams M., Kahn R.S. A road map to address the social determinants of health through community collaboration. Pediatrics. 2015;136(4):e993–e1001. doi: 10.1542/peds.2015-0549. [DOI] [PubMed] [Google Scholar]
- Hogg R.A., Varda D. Insights into collaborative networks of nonprofit, private, and public organizations that address complex health issues. Health Affairs. 2016;35(11):2014–2019. doi: 10.1377/hlthaff.2016.0725. [DOI] [PubMed] [Google Scholar]
- Hoi C.K., Wu Q., Zhang H. Community social capital and corporate social responsibility. Journal of Business Ethics. 2018;152(3):647–665. doi: 10.1007/s10551-016-3335-z. [DOI] [Google Scholar]
- James J. Health policy brief: Nonprofit hospitals' community benefit requirements. Health Affairs. 2016;1–5 doi: 10.1377/hpb2016.3. [DOI] [Google Scholar]
- Jencks S.F., Williams M.V., Coleman E.A. Rehospitalizations among patients in the medicare fee-for-service program. New England Journal of Medicine. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Kawachi I., Kennedy B.P., Lochner K., Prothrow-Stith D. Social capital, income inequality, and mortality. American Journal of Public Health. 1997;87(9):1491–1498. doi: 10.2105/AJPH.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindig D., Stoddart G. What is population health? American Journal of Public Health. 2003;93 doi: 10.2105/ajph.93.3.380. http://www.cihr-irsc.gc.ca/ Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko M., Derose K.P., Needleman J., Ponce N.A. Whose social capital matters? The case of U.S. Urban public hospital closures and conversions to private ownership. Social Science & Medicine. 2014;114:188–196. doi: 10.1016/j.socscimed.2014.03.024. [DOI] [PubMed] [Google Scholar]
- Lee S.D., Chen W.L., Weiner B.J. Communities and hospitals: Social capital, community accountability, and service provision in U.S. Community hospitals. Health Services Research. 2004;39(5):1487–1509. doi: 10.1111/j.1475-6773.2004.00300.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattessich P.W., Rausch E.J. Cross-sector collaboration to improve community health: A view of the current landscape. Health Affairs. 2014;33(11):1968–1974. doi: 10.1377/hlthaff.2014.0645. [DOI] [PubMed] [Google Scholar]
- Mays G.P., Mamaril C.B., Timsina L.R. Preventable death rates fell where communities expanded population health activities through multisector networks. Health Affairs. 2016;35(11):2005–2013. doi: 10.1377/hlthaff.2016.0848. [DOI] [PubMed] [Google Scholar]
- Mays G.P., Scutchfield F.D. Improving public health system performance through multiorganizational partnerships. Preventing Chronic Disease. 2010;7(6):A116. http://www.ncbi.nlm.nih.gov/pubmed/20950523 Retrieved from. [PMC free article] [PubMed] [Google Scholar]
- Nolte E., McKee M. Variations in amenable mortality-Trends in 16 high-income nations. Health Policy. 2011;103(1):47–52. doi: 10.1016/j.healthpol.2011.08.002. [DOI] [PubMed] [Google Scholar]
- Park S., Hamadi H., Apatu E., Spaulding A.C. Hospital partnerships in population health initiatives. Population Health Management. 2019:1–8. doi: 10.1089/pop.2019.0074. 00(00) [DOI] [PubMed] [Google Scholar]
- Pennel C.L., McLeroy K.R., Burdine J.N., Matarrita-Cascante D. Nonprofit hospitals-approach to community health needs assessment. American Journal of Public Health. 2015;105(3):e103–e113. doi: 10.2105/AJPH.2014.302286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennel C.L., McLeroy K.R., Burdine J.N., Matarrita-Cascante D., Wang J. Community health needs assessment: Potential for population health improvement. Population Health Management. 2016;19(3):178–186. doi: 10.1089/pop.2015.0075. [DOI] [PubMed] [Google Scholar]
- Putnam R.D. Tuning in, tuning out: The strange disappearance of social capital in America. PS: Political Science and Politics. 1995;28(4):664. doi: 10.2307/420517. [DOI] [Google Scholar]
- Putnam R.D. Oxford University Press; 2002. Democracies in flux: The evolution of social capital in contemporary society. [Google Scholar]
- Singh S.R., Cramer G.R., Young G.J. The magnitude of a community's health needs and nonprofit hospitals' progress in meeting those needs: Are we faced with a paradox? Public Health Reports. 2018;133(1):75–84. doi: 10.1177/0033354917739581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Social Capital Project The geography of social capital in America. 2018. https://www.jec.senate.gov/public/index.cfm/republicans/2018/4/the-geography-of-social-capital-in-america Washington DC. Retrieved from.
- Somerville M.H., Seeff L., Hale D., O'Brien D.J. Hospitals, collaboration, and community health improvement. Journal of Law Medicine & Ethics. 2015;43(s1):56–59. doi: 10.1111/jlme.12217. [DOI] [PubMed] [Google Scholar]
- Trujillo M.D., Plough A. Building a culture of health: A new framework and measures for health and health care in America. Social Science & Medicine. 2016;165:206–213. doi: 10.1016/j.socscimed.2016.06.043. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Costa M.V., Odunlami A.O., Mohammed S.A. Moving upstream: How interventions that address the social determinants of health can improve health and reduce disparities. Journal of Public Health Management and Practice: JPHMP. 2008;14 Suppl doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang T.C., Jensen L., Haran M. Social capital and human mortality: Explaining the rural paradox with county-level mortality data. Rural Sociology. 2011;76(3):347–374. doi: 10.1111/j.1549-0831.2011.00055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoorob M.J., Salemi J.L. Bowling alone, dying together: The role of social capital in mitigating the drug overdose epidemic in the United States. Drug and Alcohol Dependence. 2017;173:1–9. doi: 10.1016/j.drugalcdep.2016.12.011. 2017. [DOI] [PubMed] [Google Scholar]