Abstract
Objective
This was a post hoc analysis of the Edaravone Phase III Study MCI186-19 (‘Study 19’) to examine the utility of clinical staging systems as end points in clinical trials in amyotrophic lateral sclerosis (ALS).
Methods
Amyotrophic Lateral Sclerosis Functional Rating Scale—Revised item scores from Study 19 were retrospectively mapped to King’s stage and Milano-Torino staging (MiToS) stage. We assessed the percentage of patients who experienced progression in King’s and MiToS stages during Study 19. We also assessed disease progression in subgroups of patients according to baseline King’s stage.
Results
During double-blind treatment, the percentage of patients who experienced a progression in King’s stage was lower for edaravone (42.0%, 95% CI 30.4% to 53.6%) than placebo (55.9%, 95% CI 44.1% to 67.6%). The most pronounced effect was noted among patients who were in stage 1 and was maintained throughout open-label treatment. An analysis of a ≥2-stage progression in MiToS stage showed no difference between treatment arms during double-blind treatment, but during the open-label period, more rapid progression was noted among patients in the placebo–edaravone arm than among those in the edaravone–edaravone arm (log-rank test, p<0.001).
Conclusions
The King’s and MiToS staging systems provided utility in assessing clinical progression in Edaravone Study 19. These findings may support the use of staging systems as end points in ALS clinical trials and to understand the timing of benefit as measured by these scales.
Introduction
Clinical staging systems have proven valuable in a variety of neurological diseases, including Parkinson’s disease, multiple sclerosis and Alzheimer’s disease.1–4 In amyotrophic lateral sclerosis (ALS), most clinical studies have relied on change from baseline in the total Amyotrophic Lateral Sclerosis Functional Rating Scale—Revised (ALSFRS-R) score as the primary end point. Although functional rating scales such as the ALSFRS-R are useful measures in clinical trials for assessing change in a patient’s clinical status, they may not place sufficient emphasis on important milestones in disease progression. ALS clinical staging systems potentially could provide useful adjunctive information.
The King’s ALS clinical staging system assesses anatomical spread of ALS, based on the number of affected regions (bulbar, upper limb and lower limb) and includes advanced stages defined by nutritional or respiratory failure.5 6 The Milano-Torino staging (MiToS) system assesses the number of functional domains in which there is a loss of independent function.7 The domains in the MiToS system include movement (walking/self-care), swallowing, communicating, and breathing.7 The King’s and MiToS systems have demonstrated utility in a variety of settings. For example, retrospective analyses indicate that riluzole prolongs King’s stages 1 and 4, and MiToS stage 1.8 9
Two therapies—riluzole and edaravone—have been approved for treating ALS in several countries.10 11 Edaravone (Radicava; Mitsubishi Tanabe Pharma America, New Jersey, USA) has been shown in a clinical trial to slow the rate of functional loss, as measured by the ALSFRS-R.12 Based on the results of the pivotal phase III study for edaravone (Edaravone Phase III Study MCI186-19 (Study 19)), the drug has been approved for use in patients with ALS in Japan, South Korea, USA, Canada and Switzerland. However, countries and regions have differing opinions and requirements for drug approval (eg, edaravone is not yet approved in the European Union), which has sparked debate and differing viewpoints on edaravone. The King’s and MiToS staging systems were not available at the time Edaravone Study 19 was being planned and thus were not included as measures.
In order to help assess the value of clinical staging systems as end points in randomised controlled trials in ALS, we conducted a post hoc analysis of Study 19 with respect to progression in clinical staging, using both the King and MiToS systems.
Methods
Study 19 study design
Study 19 was a randomised, double-blind, parallel-group, placebo-controlled study conducted in Japan; details of the study and prespecified analyses of data from the 24-week double-blind treatment period and the 24-week open-label active-treatment extension have been previously reported (clinicaltrials.org: NCT01492686).12 13 The study design for Study 19 incorporated an enrichment strategy based on key learnings from a previous phase III study (MCI186-16, Study 16) to increase the ability of the trial to detect a significant effect of treatment with the ALSFRS-R within a 6-month time frame.
Eligible participants were aged 20–75 years, with ALS grade 1 or 2 on the Japan ALS Severity Classification, scores of ≥2 on all 12 items of the ALSFRS-R, forced vital capacity of ≥80%, definite or probable ALS according to the El Escorial and revised Airlie House criteria, and duration of disease from the first symptom (any ALS symptom) for <2 years. Patients were ineligible if they had scores of ≤3 on ALSFRS-R items for dyspnoea, orthopnoea or respiratory insufficiency; other exclusion criteria included a history of spinal surgery after onset of ALS or creatinine clearance of 50 mL/min or less. Initiation of riluzole after the start of the observation period was prohibited; however, patients receiving riluzole at study entry could continue to do so during the trial at an unchanged dose. Criteria for study discontinuation included patient request, ineligibility for the study, adverse event, requirement for tracheotomy, requirement for respiratory support all day long and worsening of ALS.
Briefly, after a 12-week observation period, eligible patients (those with a decrease of 1–4 points in the ALSFRS-R score during this period) were randomly assigned 1:1 to receive 6 cycles of edaravone therapy or placebo over 24 weeks. At the end of the double-blind treatment, all patients could receive open-label treatment with edaravone for another 24 weeks (cycles 7–12). Edaravone was administered in a 60 mg dose, once a day, via intravenous infusion over 60 min. Infusion was given for 14 days for the first treatment cycle and for 10 days in the 14-day treatment period for all subsequent cycles. Each treatment cycle was followed by a 14-day drug-free period.
The primary efficacy end point of the study was the change in ALSFRS-R score from baseline to the end of week 24.
Study 19 patients
In total, 137 patients were randomised to receive either edaravone (n=69) or placebo (n=68) in Study 19. Baseline characteristics of patients were well balanced between the 2 treatment groups, except for male sex and ALS severity (table 1).12 13 A total of 127 patients completed double-blind treatment; 2 patients receiving edaravone and 8 patients receiving placebo discontinued treatment, principally due to disease progression. A total of 123 patients were enrolled in the open-label extension: 65 patients from the edaravone group (edaravone–edaravone) and 58 patients from the placebo group (placebo–edaravone); 53 and 40 of these patients, respectively, completed open-label treatment. At week 48 (ie, the end of the open-label extension), the discontinuation rate was 23% for patients initially assigned to receive edaravone and 41% for patients initially assigned to receive placebo.
Table 1.
Baseline demographics and clinical disease characteristics (FAS analysis)12 13
| Edaravone (n=69) | Placebo (n=68) | |
| Sex, n (%) | ||
| Men | 38 (55) | 41 (60) |
| Women | 31 (45) | 27 (40) |
| Mean age (years) (SD) | 60.5 (10) | 60.1 (10) |
| Mean duration of disease (years) (SD) | 1.13 (0.5) | 1.06 (0.5) |
| Initial symptom, n (%) | ||
| Bulbar symptom | 16 (23) | 14 (21) |
| Limb symptom | 53 (77) | 54 (79) |
| ALS diagnostic criteria, n (%)* | ||
| Definite | 28 (41) | 27 (40) |
| Probable | 41 (59) | 41 (60) |
| ALS severity, n (%)† | ||
| Grade 1 | 22 (32) | 16 (24) |
| Grade 2 | 47 (68) | 52 (76) |
| Mean ALSFRS-R score (SD) | ||
| Before observation period | 43.6 (2.2) | 43.5 (2.2) |
| Baseline (end of 12 weeks of observation) | 41.9 (2.4) | 41.8 (2.2) |
| Concomitant riluzole, n (%) | 63 (91) | 62 (91) |
| At the start of cycle 7 | Edaravone– edaravone |
Placebo– edaravone |
| ALS severity, n (%)† | ||
| Grade 1 | 8 (12.3) | 5 (8.6) |
| Grade 2 | 27 (41.5) | 22 (37.9) |
| Grade 3 | 21 (32.3) | 24 (41.4) |
| Grade 4 | 9 (13.8) | 7 (12.1) |
| Mean ALSFRS-R score (SD) | 37.8 (4.9) | 34.8 (5.8) |
*According to revised El Escorial criteria.
†According to Japan ALS severity classification (grades 1–5, with grade 5 being most severe).
ALS, amyotrophic lateral sclerosis; ALSFRS-R, Amyotrophic Lateral Sclerosis Functional Rating Scale—Revised; FAS, full analysis set.
Post hoc staging analyses
ALSFRS-R item responses in Study 19 were retrospectively mapped to King’s stage and MiToS stage as previously described.6 7 Mapping of ALSFRS-R item responses to clinical staging systems makes it more likely that a patient will experience an event before being lost to follow-up, because an event constitutes patterns of change in the ALSFRS-R, and such changes tend to occur relatively frequently. As mentioned in the Introduction section, the King’s ALS clinical staging system assesses anatomical spread of ALS, based on the number of affected regions (bulbar, upper limb and lower limb).5 6 King’s stage 1 consists of functional involvement of 1 central nervous system (CNS) region, while stages 2 and 3 correspond to functional involvement of 2 and 3 CNS regions, respectively. Stage 4A represents nutritional failure and stage 4B represents significant respiratory failure. Stage 5 is death. For King’s analysis, ALSFRS-R item responses were mapped to King’s staging system based on responses to items 1 (speech), 2 (salivation), 3 (swallowing), 4 (handwriting), 5A/B (self-feeding), 8 (walking), 10 (dyspnoea) and 12 (respiratory insufficiency) as previously described. The MiToS system assesses the number of functional domains in which there is a loss of independent function.7 MiToS stage 0 consists of no functional domains lost, while stages 1–4 consist of loss of 1 to 4 functional domains, respectively. Stage 5 is death. MiToS mapping was done by mapping ALSFRS-R item responses to the MiToS system based on responses to items 1 (speech), 3 (swallowing), 4 (handwriting), 6 (dressing/hygiene), 8 (walking), 10 (dyspnoea) and 12 (respiratory insufficiency).7 Study 19 was not designed to detect statistical differences in staging analyses nor were patients allocated according to stage.
One limitation of the study was its post hoc nature, since this analysis was based directly on the primary end point data from the study and simply converts ALSFRS-R score data into the 2 staging systems. Because findings were positive for the ALSFRS-R, these post hoc analyses would be biased towards a positive finding. Study 19, however, was not designed to assess effects on clinical staging and was not powered for this end point.
The percentages of patients in each treatment group who experienced a progression in King’s and MiToS stages were examined from baseline to the end of cycles 6 and 12. Data are reported as point estimates and 95% CI. Kaplan-Meier time-to-event analysis was used to examine time to first progression in King’s and MiToS stages and time to 2-stage progression in MiToS, at which point patients lost to follow-up were censored. Log-rank test was used to determine the statistical significance of differences in the Kaplan-Meier curves between study arms.
A subgroup analysis was conducted by analysing the trends in changes from baseline in ALSFRS-R score in patients grouped according to King’s stage at baseline. A linear mixed-effects model was used to examine the relationship between the trend of ALSFRS-R total scores over time and King’s stage at baseline. A random intercept was assumed, and ALSFRS–R scores at baseline were included as covariates for adjustment. Fixed effects included treatment, King’s stage at baseline, time since enrolment, and their interaction terms. Trend lines were plotted and differences in treatment effect were assessed by a mixed-effects model for repeated measures analysis.
Results
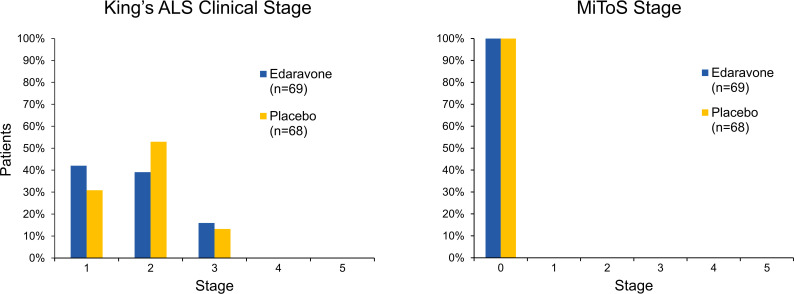
King’s and MiToS stages at baseline
Approximately 80% of patients were King’s stage 1 or 2 at study entry, and all patients were at MiToS stage 0, as expected based on the Study 19 inclusion criteria (figure 1). King’s stage at enrolment did not differ notably between the treatment groups.
Figure 1.
King’s and MiToS stages at study entry. Percentages of patients in each treatment arm corresponding to each clinical stage are shown (edaravone, blue columns; placebo, yellow columns). ALS, amyotrophic lateral sclerosis; MiToS, Milano-Torino staging.
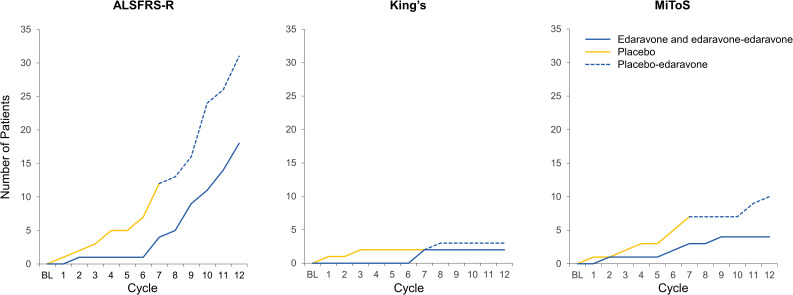
Loss to follow-up
One of the advantages of using clinical staging systems or mapping ALSFRS-R item responses to clinical staging systems is that patients may be more likely to experience a progression in clinical stage prior to being lost to follow-up, which reduces bias due to informative censoring. In this post hoc analysis, most patients experienced an event in King’s or MiToS analyses before dropping out of the study (figure 2).
Figure 2.
Number of patients lost to follow-up. The number of patients lost to follow-up is shown for each assessment. The blue lines represent patients receiving edaravone and edaravone–edaravone; the yellow lines represent patients receiving placebo, and the blue dashed lines represent patients receiving placebo–edaravone. ALSFRS-R, Amyotrophic Lateral Sclerosis Functional Rating Scale—Revised; MiToS, Milano-Torino staging.
In King’s staging analysis through cycle 12, 50 patients in the edaravone–edaravone group experienced an event through cycle 12, with 2 patients censored; in the placebo–edaravone group, 54 patients experienced an event, with 3 patients censored. In the MiToS analysis of time to any progression, through cycle 12, in the edaravone–edaravone group, 46 patients experienced an event, with 4 patients censored; in the placebo–edaravone group, 50 patients experienced an event, with 10 patients censored. In the MiToS analysis of time to progression by ≥2 stages, through cycle 12, in the edaravone–edaravone group, 7 patients experienced an event, with 16 patients censored; in the placebo–edaravone group, 16 patients experienced an event, with 20 patients censored.
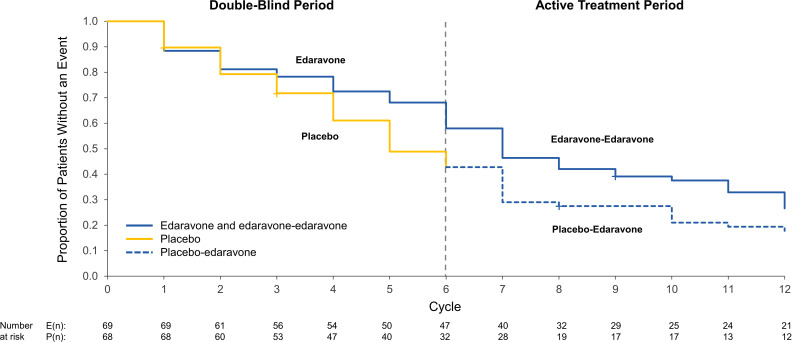
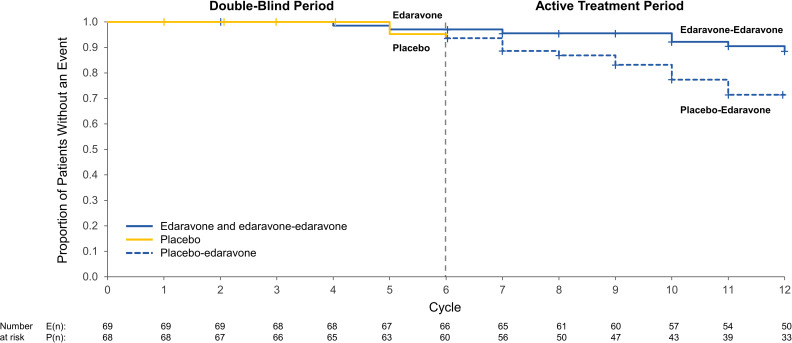
Time to progression in King’s clinical stage
Patients in the placebo arm experienced shorter times to progression in King’s clinical stage as compared with patients in the edaravone arm (figure 3); the difference did not reach statistical significance (log-rank test, p=0.103). Among patients who received edaravone during double-blind treatment, fewer experienced a progression in King’s stage by the end of cycle 6 versus those receiving placebo: edaravone, 42.0% (95% CI 30.4% to 53.6%) vs placebo, 55.9% (95% CI 44.1% to 67.6%).
Figure 3.
Kaplan-Meier analysis of time to any decline in King’s ALS clinical stage. Kaplan-Meier curves are shown for time to any decline in King’s ALS clinical stage for patients in the double-blind period (blue line, edaravone; yellow line, placebo) and in the active-treatment period (blue line, edaravone–edaravone; dashed blue line, placebo–edaravone). Plus symbols represent patients who were censored from the analysis due to loss to follow-up (a plus symbol may represent more than one patient). The number of patients at risk is listed under the graph at each time point for each arm. ALS, amyotrophic lateral sclerosis.
Patients receiving placebo crossed over to open-label edaravone treatment at cycle 7, and by the end of cycle 12, a progression in King’s stage was experienced by 72.5% (95% CI 62.3% to 82.6%) of patients receiving edaravone–edaravone vs 79.4% (95% CI 69.1% to 88.2%) of those receiving placebo–edaravone.
King’s stage at which edaravone affects disease progression
The effects of edaravone on King’s clinical stage were also assessed by conducting a Kaplan-Meier analysis of patients remaining in each King’s clinical stage (figure 4). Edaravone treatment appeared to show the most pronounced effect in slowing the transition from stage 1 to stage 2, that is, the spread of functional involvement of ALS from 1 CNS region to 2 CNS regions (figure 4A). There may have also been an effect in slowing the transition from stage 2 to stage 3, but this was less well pronounced than the effect on the stage 1 to stage 2 transition (figure 4B). There were no discernible effects on later transitions in King’s clinical stage by edaravone treatment (figure 4C, D).
Figure 4.
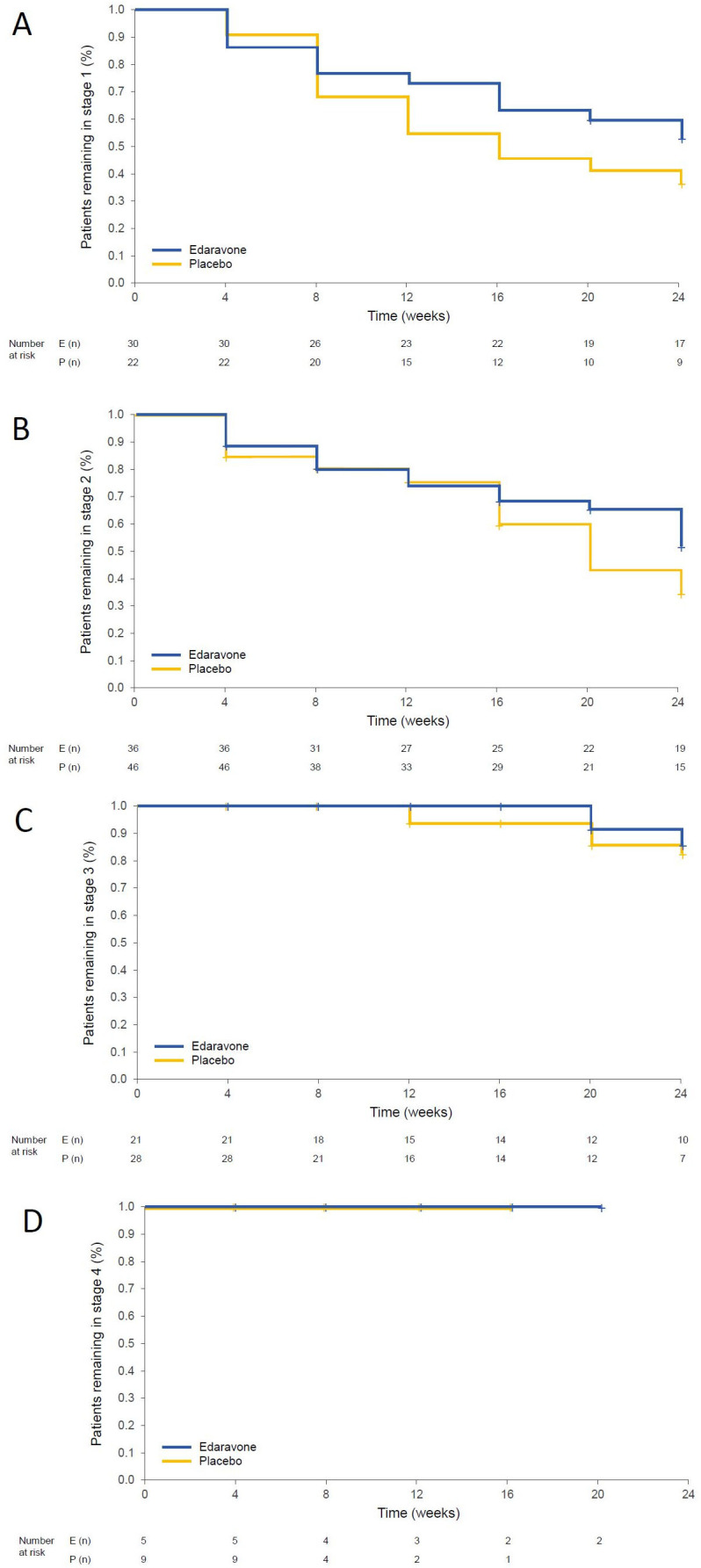
Kaplan-Meier analyses of patients remaining in each King’s stage. Kaplan-Meier curves show time to event analyses for proportions of patients remaining in King’s stage 1 (A), stage 2 (B), stage 3 (C) or stage 4 (D). All analyses are for time points during the 24-week double-blind treatment period. Plus symbols represent patients who were censored from the analysis (a plus symbol may represent more than one patient). The number of patients at risk is listed under the graph at each time point for each arm.
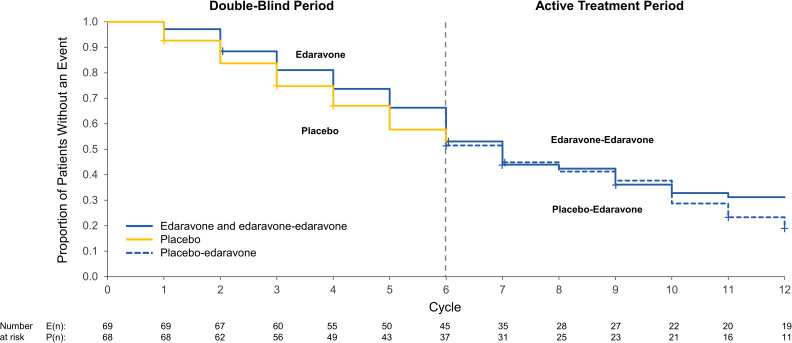
Time to progression in MiToS clinical stage
Patients in both the placebo and edaravone arms experienced similar times to progression in MiToS clinical stage through the double-blind period; however, there appeared to be a lower risk of progression during the open-label extension among patients receiving edaravone–edaravone than among those receiving placebo–edaravone (figure 5). At end of cycle 6, the percentage of patients experiencing a progression in MiToS stage were comparable: edaravone, 46.4% (95% CI 34.8% to 58.0%) vs placebo, 47.1% (95% CI 35.3% to 58.8%). During the open‐label phase, separation in Kaplan-Meier curves for any progression in MiToS stage was noted at the end of cycle 12, although this separation was not statistically significant (log-rank test, p=0.308): edaravone–edaravone, 66.7% (95% CI 55.1% to 76.8%) vs placebo–edaravone, 73.5% (95% CI 63.2% to 83.8%).
Figure 5.
Kaplan-Meier analysis of time to any decline in MiToS stage. Kaplan-Meier curves are shown for time to any decline in MiToS stage for patients in the double-blind period (blue line, edaravone; yellow line, placebo) and in the active-treatment period (blue line, edaravone–edaravone; dashed blue line, placebo–edaravone). Plus symbols represent patients who were censored from the analysis due to loss to follow-up (a plus symbol may represent more than one patient). The number of patients at risk is listed under the graph at each time point for each arm. MiToS, Milano-Torino staging.
To further investigate this finding, an analysis of ≥2-stage progression in the MiToS stage revealed that most patients in either group did not experience this type of decline during the double-blind period (ie, through cycle 6) (figure 6). However, more rapid progression was found in the placebo–edaravone arm than in the edaravone–edaravone arm in the open-label period (log-rank test, p<0.001) (figure 6). The percentage of patients who experienced a ≥2-stage progression in the MiToS stage by the end of cycle 6 were similar: edaravone, 2.9% (95% CI 0.0% to 7.2%) vs placebo, 5.9% (95% CI 1.5% to 11.8%). By the end of cycle 12, however, there was separation in the Kaplan-Meier curves for a ≥2-stage progression in MiToS (log-rank test, p<0.001) (figure 6). Point estimates at the end of cycle 12 were as follows: edaravone–edaravone, 10.1% (95% CI 4.3% to 17.4%) vs placebo–edaravone, 23.5% (95% CI 13.2% to 33.8%).
Figure 6.
Kaplan-Meier analysis of time to a ≥2-stage decline in MiToS. Kaplan-Meier curves are shown for time to a ≥2-stage decline in MiToS for patients in the double-blind period (blue line, edaravone; yellow line, placebo) and in the active-treatment period (blue line, edaravone–edaravone; dashed blue line, placebo–edaravone). Plus symbols represent patients who were censored from the analysis due to loss to follow-up (a plus symbol may represent more than one patient). The number of patients at risk is listed under the graph at each time point for each arm. MiToS, Milano-Torino staging.
Concordance analysis indicated that there was overall poor concordance between King’s and MiToS systems in terms of identification of patients who underwent no progression versus any progression (table 2). This finding confirms that the 2 staging systems assess different aspects of disease progression and are therefore complementary and largely not duplicative in terms of the information they provide. This difference is consistent with previous findings.12
Table 2.
Concordance between King’s and MiToS declines (cycles 1–6)
| Decline in King’s Health State | Decline in MiToS Health state | ||
| No Decline | Any Decline | Total | |
| No decline | 44 (32.1%) | 26 (19.0%) | 70 (51.5%) |
| Any decline | 29 (21.2%) | 38 (27.7%) | 67 (48.9%) |
| Total | 73 (53.3%) | 64 (46.7%) | 137 (100%) |
MiToS, Milano-Torino staging.
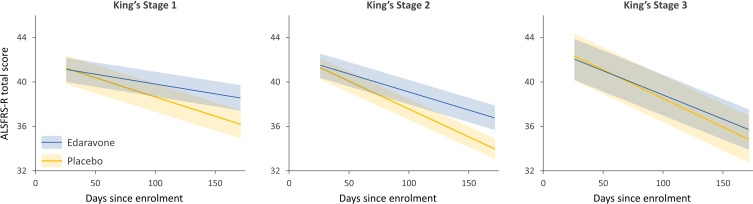
Analysis of disease progression in King’s stage subgroups at baseline
A subgroup analysis was conducted by analysing disease progression (ie, trends in changes in ALSFRS-R score from baseline to cycle 6) in patients grouped according to King’s stage at baseline (figure 7). This analysis revealed that patients in lower King’s stages progressed at slower rates than patients in higher King’s stages. Analysis of variance indicated statistically significant interactions between time since enrolment and King’s stage at baseline and also between time since enrolment and treatment (p<0.001 for both).
Figure 7.
Change in ALSFRS-R scores by King’s stage at baseline and treatment group. Trends in changes in ALSFRS-R score over time were plotted for patients in the following King’s stages at baseline: stage 1 (edaravone, n=29; placebo, n=21), stage 2 (edaravone, n=27; placebo, n=36) and stage 3 (edaravone, n=11; placebo, n=9). Least squares means treatment differences from baseline to cycle 6, as assessed by MMRM analysis, were as follows: stage 1, 2.33 units (p=0.043); stage 2, 3.5 units (p=0.0057), and stage 3, 0.81 units (p=0.69). ALSFRS-R, Amyotrophic Lateral Sclerosis Functional Rating Scale—Revised; MMRM, mixed-effects model for repeated measures.
Discussion
In this retrospective analysis of data from the edaravone phase III trial, Study 19, both King’s ALS clinical staging system and the MiToS system appeared to detect differences in clinical progression between patients randomised to edaravone versus placebo. While the King’s system captured differences in early follow-up, the MiToS system appeared to capture later separation between treatment groups, especially in terms of a ≥2-stage progression. The complementary nature of the information provided by each staging system was further confirmed by a concordance analysis conducted on the data from these analyses. This may be expected, as these 2 staging systems have previously been shown to be complementary, with King’s staging showing greatest resolution in early to mid-disease and MiToS showing higher resolution for later stages of disease.14
Post hoc analyses in this study indicated that edaravone had the greatest effects in slowing the transition from King’s stage 1 to stage 2. Similar analyses of riluzole show a benefit in King’s stages 1 and 4 and in MiToS stage 1.8 9 The effects in prolonging time spent in King’s stage 1 may be particularly important to patients, as this is when disability is relatively low. This may also have implications for health economics because the earlier stages of ALS are associated with lower costs than later stages.7 15 16
This study highlights the potential value of ALS clinical staging systems as assessment tools in randomised controlled trials of new treatments for ALS. In that regard, the MiToS system is currently being used as the primary end point in an ongoing phase II trial in ALS17 and King’s system as a secondary end point in another phase II trial in ALS (www.mirocals.eu).
One limitation of the study was its post hoc nature, since this analysis was based directly on the primary end point data from the study and simply converts ALSFRS-R score data into the 2 staging systems. Because findings were positive for the ALSFRS-R, these post hoc analyses would be biased towards a positive finding. Study 19, however, was not designed to assess effects on clinical staging and was not powered for this end point. Another limitation is that the correlation between clinical stage by examination and ALSFRS-R–estimated stage is 0.92.6
The key findings of this post hoc analysis are consistent with the proposition that ALS staging systems may be useful end points in clinical trials. These staging systems may be a novel and interesting way to deal with the problem of informative censoring that can confound results of randomised controlled trials and have the potential to bias their findings to the null. They also may help to identify the settings in which particular treatments might be optimally used. The independent and complementary nature of the 2 systems, one tracking anatomical spread of disease (the King’s Clinical Staging System) and the other focusing on loss of function (the MiToS system), means they can provide different insights that may be particularly important in counselling patients on the potential benefits of therapy. Thus, clinical studies in ALS would be expected to benefit from including assessments of clinical staging as a primary or secondary end point in the study. This would likely require powering the study to include sufficient numbers of patients at each stage, dynamic allocation of patients to help ensure adequate balance among study arms, and capturing staging data at study exit to help avoid censoring and improve statistical power.
Acknowledgments
The authors thank Jeffrey Zhang, PhD, and Peter Lu, PhD, of Princeton Pharmatech for assistance with the data analysis and the preparation of figures. The authors also thank Alex Morla, PhD, of p-value communications for editorial assistance.
Footnotes
Twitter: @AmmarAlChalabi
Contributors: AA-C: contributed to writing, study design, clinical interpretation and data interpretation. AC: contributed to writing, study design, clinical interpretation and data interpretation. GO: contributed to writing, literature search, study design, and data analysis and interpretation. RB: contributed to writing, literature search, study design, data analysis and interpretation, and figures. CM: contributed to writing, literature search, study design, data analysis and interpretation, and figures. WA: contributed to writing, literature search, study design, and data analysis and interpretation. SA: contributed to study design and data analysis and interpretation.
Funding: This study was funded by Mitsubishi Tanabe Pharma America, Inc. (MTPA). Policy Analysis Inc, Princeton Pharmatech, and p-value communications received funding from MTPA for the work conducted on this study. No funding was received from MTPA by Ammar Al-Chalabi, PhD, FRCP, or Adriano Chiò, MD, FAAN, for their participation in this study. Ammar Al-Chalabi, PhD, FRCP, received funding in part by an EU Joint Programme - Neurodegenerative Disease Research (JPND) project. The project is supported through the following funding organisations under the aegis of JPND (www.jpnd.eu), UK, Medical Research Council (MR/L501529/1; MR/R024804/1) and Economic and Social Research Council (ES/L008238/1)) and through the Motor Neurone Disease Association. Participation by Ammar Al-Chalabi, PhD, FRCP, in this study represents independent research in part funded by the National Institute for Health Research Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The participation of Adriano Chiò, MD, FAAN, in this study was performed under the Department of Excellence grant of the Italian Ministry of Education, University and Research to the ‘Rita Levi Montalcini’ Department of Neuroscience, University of Torino, Italy.
Competing interests: AA-C serves as a consultant for Chronos Therapeutics, OrionPharma, GSK, Novartis, Lilly, Biogen Idec, AB Science, Cytokinetics Inc, MTPA, Mitsubishi Tanabe Pharma Europe and Treeway. AC serves as a consultant for Biogen and MTPA and receives research support from the Italian Ministry of Health and Italian Ministry of Education, University and Research. GO and RB served as consultants to MTPA, in their capacities as employees at Policy Analysis, which provides consulting and contract research services to biopharma companies. CM and WA are former employees of MTPA. SA is an employee of MTPA.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. Data are available on request to Mitsubishi Tanabe Pharma America, Inc, from researchers at academic institutions.
References
- 1. Goetz CG, Poewe W, Rascol O, et al. . Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations. Mov Disord 2004;19:1020–8. 10.1002/mds.20213 [DOI] [PubMed] [Google Scholar]
- 2. Movement Disorder Society Task Force on Rating Scales for Parkinson's Disease The unified Parkinson's disease rating scale (UPDRS): status and recommendations. Mov Disord 2003;18:738–50. 10.1002/mds.10473 [DOI] [PubMed] [Google Scholar]
- 3. Cummings J. The role of biomarkers in Alzheimer's disease drug development. Adv Exp Med Biol 2019;1118:29–61. 10.1007/978-3-030-05542-4_2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Inojosa H, Schriefer D, Ziemssen T. Clinical outcome measures in multiple sclerosis: a review. Autoimmun Rev 2020;19:102512. 10.1016/j.autrev.2020.102512 [DOI] [PubMed] [Google Scholar]
- 5. Roche JC, Rojas-Garcia R, Scott KM, et al. . A proposed staging system for amyotrophic lateral sclerosis. Brain 2012;135:847–52. 10.1093/brain/awr351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Balendra R, Jones A, Jivraj N, et al. . Estimating clinical stage of amyotrophic lateral sclerosis from the ALS functional rating scale. Amyotroph Lateral Scler Frontotemporal Degener 2014;15:279–84. 10.3109/21678421.2014.897357 [DOI] [PubMed] [Google Scholar]
- 7. Chiò A, Hammond ER, Mora G, et al. . Development and evaluation of a clinical staging system for amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 2015;86:38–44. 10.1136/jnnp-2013-306589 [DOI] [PubMed] [Google Scholar]
- 8. de Jongh AD, van Eijk RPA, van den Berg LH. Evidence for a multimodal effect of riluzole in patients with ALS? J Neurol Neurosurg Psychiatry 2019;90:1183–4. 10.1136/jnnp-2018-320211 [DOI] [PubMed] [Google Scholar]
- 9. Fang T, Al Khleifat A, Meurgey J-H, et al. . Stage at which riluzole treatment prolongs survival in patients with amyotrophic lateral sclerosis: a retrospective analysis of data from a dose-ranging study. Lancet Neurol 2018;17:416–22. 10.1016/S1474-4422(18)30054-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mitsubishi Tanabe Pharma Radicava® (edaravone injection) [package insert]. Jersey City, NJ: Mitsubishi Tanabe Pharma Corporation, 2018. [Google Scholar]
- 11. Sanofi-Aventis U.S. LLC Rilutek® (riluzole) [package insert]. Bridgewater, NJ: Sanofi-Aventis U.S. LLC, 2012. [Google Scholar]
- 12. Writing Group, Edaravone (MCI-186) ALS 19 Study Group . Safety and efficacy of edaravone in well defined patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled trial. Lancet Neurol 2017;16:505–12. 10.1016/S1474-4422(17)30115-1 [DOI] [PubMed] [Google Scholar]
- 13. Writing Group on Behalf of the Edaravone (MCI-186) ALS 19 Study Group Open-label 24-week extension study of edaravone (MCI-186) in amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener 2017;18:55–63. 10.1080/21678421.2017.1364269 [DOI] [PubMed] [Google Scholar]
- 14. Fang T, Al Khleifat A, Stahl DR, et al. . Comparison of the King's and MiToS staging systems for ALS. Amyotroph Lateral Scler Frontotemporal Degener 2017;18:227–32. 10.1080/21678421.2016.1265565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jones AR, Jivraj N, Balendra R, et al. . Health utility decreases with increasing clinical stage in amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener 2014;15:285–91. 10.3109/21678421.2013.872149 [DOI] [PubMed] [Google Scholar]
- 16. Oh J, An JW, Oh S-I, et al. . Socioeconomic costs of amyotrophic lateral sclerosis according to staging system. Amyotroph Lateral Scler Frontotemporal Degener 2015;16:202–8. 10.3109/21678421.2014.999791 [DOI] [PubMed] [Google Scholar]
- 17. Bella ED, Tramacere I, Antonini G, et al. . Protein misfolding, amyotrophic lateral sclerosis and guanabenz: protocol for a phase II RCT with futility design (promise trial). BMJ Open 2017;7:e015434. 10.1136/bmjopen-2016-015434 [DOI] [PMC free article] [PubMed] [Google Scholar]