Abstract
Objectives:
To evaluate the impact of coronavirus-19 (COVID-19) pandemic and its consequences on general surgery residents.
Methods:
Cross-sectional, survey based study including surgical residents in Kingdom of Saudi Arabia and Kingdom of Bahrain.
Results:
Surgical trainees who participated in our survey (n=234) were young (mean age 28), single (53.8%), and males (65.8%). Approximately half (50.4%) have been deployed to cover the staff shortage in intensive care units (ICUs) or emergency departments (EDs). Half of our trainees (117) scored positive in the screening tool of generalized anxiety disorder (GAD). There was a significant association between experiencing anxiety and male gender (p=0.055), level of training (p=0.002), deployment to cover ICUs (p=0.050), testing positive for COVID-19 (p=0.054) and having an infected family member (p=0.004).
Conclusion:
Coronavirus-19 pandemic has a serious effect on all healthcare workers and surgical residents have experienced a considerable amount of stress. Accordingly, this psychological burden should be appropriately addressed in organizations planning strategies. We suggest formulating guidelines to help surgical trainees to continue their learning process with least psychological burden.
Keywords: COVID-19, residency, psychology, anxiety, mental health, healthcare workers
Coronaviruses (CoV) are non-segmented, single-strand ribonucleic acid genome viruses with a positive sense, belonging to the family of Coronaviridae.1 Although they are primarily known to cause enzootic infections, within the past few decades they have evolved to infecting humans as well.2 Coronavirus illnesses range in severity from the common cold to more serious diseases such as severe acute respiratory syndrome (SARS-CoV) and the Middle East respiratory syndrome (MERS-CoV).3 In December 2019, Coronavirus-19 (COVID-19) first emerged in Wuhan, China in a cluster of severe respiratory illnesses of unknown origin. Its phenomenally rapid global spread sparked a severe viral issue and in March 2020, was determined to be a global pandemic by the World Health Organization (WHO).4
The inherent opportunities for CoV exposure place surgical residents at high risk for acquiring the infection; the stress of which may affect their health, both physically and mentally. The aim of our study is to evaluate the impact of COVID-19 pandemic and its consequences on general surgery residents.
Methods
This cross-sectional study was based on a questionnaire conducted in the Central, Southern, Eastern, and Western provinces of KSA and the Kingdom of Bahrain. It included all surgical residents enrolled in the Saudi General Surgery Board under the Saudi Commission for Health Specialties (SCHS) and the Imam Abdulrahman bin Faisal University (IAU), Saudi Arabia residency program. Literature review was conducted by authors using medical literature database platforms (Medline, Scopus, Google Scholar and Web of Science). Our sample size was calculated according to the total number of residents in specified areas. Proportionate stratified random samples were obtained using the formula: (sample size/population size) x stratum size (Table 1).
Table 1.
Sample size required in our study.

The inclusion criteria general surgery residency program trainees, Enrollment in either SCFHS or IAU residency programs, working in a healthcare facility that received and managed COVID-19 patients. The exclusion criteria Incomplete questionnaire response.
After validation, the questionnaire was distributed via an online link to all general surgical residents enrolled in the SCHS and IAU surgery programs. It included questions addressing their demography, past medical history, use of medications, screening for generalized anxiety disorders and any moral dilemmas they have experienced during the COVID-19 pandemic.
Our study does not carry any physical, psychological, social, legal, or economic risks. The consent was obtained from all participants. Our study is compliant with the principles of Helsinki Declaration. The study protocol was approved by the ethical review board (IRB) of IAU, Dammam, KSA.
Statistical analysis
An excel spreadsheet was established for the entry of data. Data analysis was carried out using the Statistical Package for Social Science for Mac version 22.0 (IBM Corp, Armonk, NY, USA). Categorical variables were summarized as frequencies and percentages, and to determine the significant association of the variables, Mann-Whitney U and Fisher exact tests were used with a significant level considered at p<0.05.
Results
We achieved a response rate of 85.4% (234/274) over a 10-day period. Demographical characteristics of the participants included age, marital status, gender, pregnancy, any changes in the nature of work during pregnancy, current level of training, current training center, training region and any covering of intensive care units (ICU) or emergency departments (ED) during this pandemic. All are presented in Table 1.
Education, training, learning outcomes and clinical competencies
Questions assessing the performance of general surgery residents regarding their education, training, educational achievements, and clinical competency outcomes demonstrate they have been negatively affected by the pandemic and are aware of increased stress and anxiety. Ten questions were answered on a 5-point median Likert scale from 0-5 (0=not applicable, 5=outstanding), interquartile range (Q1-Q3) and variance of each question, as demonstrated in Table 2.
Table 2.
Demographic data of participants.

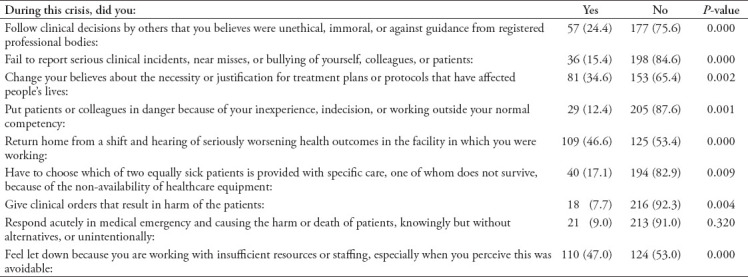
Screening for generalized anxiety disorders and exposure to moral dilemmas
Half of the participants (50%) suffered from anxiety warranting further investigation. A further 132 (56.4%) experienced excessive generalized anxiety over relatively minor issues such as being late for an appointment, facilitating minor home repairs and completing homework. One hundred twenty-two (92.4%) identified an exacerbation of their anxiety in terms of intensity, frequency and volume of distress. Ninety-seven (41.5%) had difficulty controlling their anxiety once in effect. Regarding moral challenges, 9 questions to assess the impact in situations which included life or death decision making, circumstances with a high probability of disappointment or failure, and those without a clear right or wrong pathway but where the chosen route may result in harm. The responses are listed below in Table 3.
Table 3.
Residents’ concern regarding the educational and learning process during COVID-19 pandemic with its association with covering ICU during this pandemic.

Fifty-five (23.5%) participants utilized some form of stress relief, with 48 of them stating it was effective. Sixteen (6.8%) were advised by their program directors to try relieving their stress through various means. Four (1.7%) used psychotherapy, 8 (3.4%) used medication, 5 (2.1%) used meditation, 32 (13.7%) used exercise and 4 (1.7%) used other forms of stress relief.
Regarding interaction with COVID-19 patients, 175 (74.8%) had come in contact with infected patients and the locations were as follows: 72 participants from the ward or ICU, 82 from ED, 10 during surgical procedures, 3 were exposed in the clinic, and 13 documented contact in each of the above-mentioned sources. One hundred and twenty-eight (54.7%) were subsequently tested for COVID-19, with 14 found to be positive. Among those, 7 required admission and 7 were assigned to home isolation. Forty-two (17.9%) reported positive COVID-19 tests within their families.
There were statistically significant associations between experiencing excessive degrees of anxiety and being male (p=0.055); the resident’s level of training (p=0.002); being deployed to work in the ICU (p=0.050), positive results of COVID-19 (p=0.054), and having a family member with a positive COVID-19 test (p=0.004).
Discussion
In general, the field of healthcare can be mentally, physically, and emotionally demanding. During times of crisis such as this pandemic, surgeons and those in training, find their workload markedly altered and inflated. It can be inordinately stressful to care for patients while simultaneously fearing for their own health and that of their families. For surgical residents, their training and educational process is an added concern.
In this study, surgical trainees who participated in our questionnaire were mostly young (mean age 28), single (53.8%) males (65.8%) as shown in Table 2. Approximately half of the responders (50.4%) have been deployed to cover staffing shortages in either intensive care units (ICUs) or emergency departments (EDs), with 175 (74.8%) coming in contact with COVID-19 positive patients, and 14 (8%) testing positive themselves.
There was a significant association between experiencing excessive anxiety and being a male, resident’s level of training, deployment to cover ICU, tested positive for COVID-19 and having a family member with a positive COVID-19 test (p-values of 0.055, 0.002, 0.050, 0.054 and 0.004 respectively). Likewise, Lai et al5 found that 50.4% of 1257 Chinese health care workers suffered from depressive symptoms, while 44.6% had anxiety symptoms. Nurses, female health care workers, and front liners are of higher incidence of experiencing anxiety were more severely affected by the pandemic as reported by Huang et al5,6 Contradicting our results in which male surgeons were found to experience excessive anxiety than female participants. On the other hand, Song et al7 have demonstrated the corresponding result in the form of that male emergency medical staff have suffered from depression and post-traumatic stress disorder (PTSD) more than female staff who were included in their study.
While 105 pediatricians enrolled in the study of Chen et al,8 there was no significant difference in the prevalence of anxiety when comparing physicians who had exposure to COVID-19 patients and physicians who did not.
Additionally, we found that alterations in the nature of work such as covering ICUs and caring for COVID-19 patients has negatively impacted the improvement of surgical skills (median Likert scale 1, p=0.047). On the other hand, this did not impact communication skills with colleagues and superiors (median Likert scale 3, p=0.008), or with nurses (median Likert scale 3, p=0.019). It also did not affect the ability to make clinical decisions (median Likert scale 3, p=0.017) (Table 3). Meanwhile, Wen Lu et al9 observed that medical staff who were working in the departments of respiratory, emergency and infectious disease medicine or covering ICU are more susceptible to develop psychological disorders.
Regarding residents’ psychological health and their ability to cope during this demanding time, we investigated for generalized anxiety disorder (GAD) using a short screening tool comprised of 4 questions; formulated by the Anxiety and depression association of America. Having 2 or more ‘yes’ responses to these questions implies that the respondent warrants further psychiatric evaluation, but does not necessarily diagnose GAD. We observed that half of our trainees (n=117) scored positive using this screening tool.
One hundred and thirty two (56.4%) residents described themselves as experiencing excessive anxiety, with 92.4% of them identifying a worsening in episodic frequency and intensity levels. Also, 23.5% of the participants use some form of stress relief; with exercise the most frequently used by 13.7%, and psychotherapy as the least utilized option used by 1.7% of the residents. Only 2.1% of the residents reported the use of anxiolytic medication.
In terms of practice and the delivery of patient care, we concluded that clinical encounters during this pandemic have significantly contributed to the anxiety and distress general surgery trainees have suffered (Table 4). Ninety-two percent of 275 urology residents enrolled in the French association of urologists report having experienced stress during this pandemic; with 60% further documenting that this crisis has negatively impacted their quality of life and 83.3% stating their urological training has been negatively affected. Additionally, researchers have found that being stressed is significantly associated with working in a high epidemic region, caring for COVID-19 positive patients, and having a personal medical history of respiratory illness.10
Table 4.
Result of moral injuries and its significant association with experiences excessive anxiety among residents during this pandemic.
Both medical and non-medical personnel caring for COVID-19 patients in tertiary institutions in Singapore have been investigated for psychological morbidities, with a total of 470 participants. Approximately 14% screened positive for anxiety, 8.9% for depression, 6.6% for stress, and 7.7% experienced post-traumatic stress disorder.11
Turkish emergency physicians have also shown to be affected by the pandemic with 62% of 290 physicians reporting depressive symptoms and 35.5% reporting symptoms of anxiety.12
Surgical residents of a tertiary care hospital recorded a considerable decrease in burnout prevalence inconsistent with the forced reduction of working hours due to pandemic crisis mode. Among 122 residents, 61% were concerned about the health of their families and 38.4% feared dying as a result of direct exposure to the virus.13
Finally, in a similar study conducted by Al Sulais et al,14 in KSA, including 529 physicians from various specialties across the Kingdom; worry (67.5%), isolation (56.9%) and fear (49.7%) were the most identified emotions. Female physicians were more likely to experience fear.
In line with the literature, the psychological burden of this global pandemic have been well described throughout the world and it has been of interest to researchers to explore its effect on healthcare workers regardless of their levels and specialties. To cope and overcome the drastic change brought by the pandemic, institutions have implemented restructuring organizational strategies in order to maintain provision of care for emergency and oncology patients as well as handling the influx of COVID-19 patients. A given example is the Italian experience in restructuring their colorectal services, Saverio et al,15 described their modification to practice, starting from suspending all elective non-cancer procedures, employ telemedicine to follow outpatients, adhere to conservative approach whenever amenable, mandatory screening of all patients requiring emergency interventions, postponing chemo and immune modulation therapies if possible. While concerning hospital staff; they reduced number of staff attending patients, handled all patient as COVID-19 positive by taking proper precautions and use of personal protective equipments (PPE), assigned negative pressure rooms, and specific routes for transferring COVID-19 patients, intubated and recovered patients inside theaters.15 However, in order to achieve minimum aerosolization and spread of infection; surgeons were practicing number of measures; use of sealed trocars, perform small incisions, deflate pneumoperitoneum via negative pressure suction connected to water seal, avoid laparoscopy lavage, minimize use of electrocautery during open procedures, perform one stage definitive procedures, minimize anesthesia time, and utilize local anesthesia when suitable. They also defined a classification system to prioritize colorectal cancer patients to prevent substantial delay in their treatment plans.15
Benitez et al,16 have published a number of recommendations concerning proper use of PPE when handling suspected or confirmed cases, limit the use of laparoscopy and gas leak during procedures. While most of these measures were formulated to help alleviate the stress of health working forces and providing safer work environment, many surgeons have reported that the use of PPE during procedures hindered their surgical performance.17 On the other hand, educational institutions have an extra responsibility in maintaining their training programs at excellency. As seen in McGill university health center, surgical residents were given special attention by providing them access to webinars and simulation facilities, regulating their re-allocation according to their level of training to acquire appropriate competencies, ensuring their active participation in available practice such as telemedicine and guaranteeing their return to regular surgical workflow as soon as restrictions are lifted.18
Study Limitations
In our study, we were confined by certain limitations which were mainly demonstrated in sampling and reaching sufficient complete response form participants and their willingness to disclose details about their psychological and mental health. Further studies are needed to be carried out in KSA to identify surgical residents’ concerns during COVID-19 pandemic. Moreover, healthcare workers in general, and surgical residents in particular, should be educated and provided with all the necessary infection control protective measures as well as effective adequate psychosocial support.
In conclusion, the COVID-19 pandemic has profoundly affected healthcare workers at all levels, including those enrolled in residency programs. Clinical exposure to the virus with its associated consequences has led to a considerable amount of stress felt by surgical residents. Accordingly, in planning their COVID-19 pandemic strategies, organizations should address the potential for additional psychological stresses felt by their trainees.
Nonetheless, the current situation provides an opportunity for the exploration of educational strategies invoking less anxiety and burnout. We suggest formulating specific guidelines that facilitate the learning process for surgical residents while presenting the least amount of psychological risk.
Footnotes
References
- 1.Fung TS, Liu DX. Human coronavirus: host-pathogen interaction. Annu Rev Microbiol. 2019;73:529–557. doi: 10.1146/annurev-micro-020518-115759. [DOI] [PubMed] [Google Scholar]
- 2.Schoeman D, Fielding BC. Coronavirus envelope protein: current knowledge. Virol J. 2019;16:69. doi: 10.1186/s12985-019-1182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan JF, Lau SK, To KK, Cheng VC, Woo PC, Yuen KY. Middle East respiratory syndrome coronavirus: another zoonotic betacoronavirus causing SARS-like disease. Clin Microbiol Rev. 2015;28:465–522. doi: 10.1128/CMR.00102-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. [Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19] Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38:192–195. doi: 10.3760/cma.j.cn121094-20200219-00063. In Chinese. [DOI] [PubMed] [Google Scholar]
- 7.Song X, Fu W, Liu X, Luo Z, Wang R, Zhou N, et al. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav Immun. 2020;88:60–65. doi: 10.1016/j.bbi.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Y, Zhou H, Zhou Y, Zhou F. Prevalence of self-reported depression and anxiety among pediatric medical staff members during the COVID-19 outbreak in Guiyang, China. Psychiatry Res. 2020;288:113005. doi: 10.1016/j.psychres.2020.113005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abdessater M, Rouprêt M, Misrai V, Pinar U, Matillon X, Gondran-Tellier B, et al. COVID-19 outbreak situation and its psychological impact among surgeons in training in France. World J Urol. 2020:1–2. doi: 10.1007/s00345-020-03207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan BYQ, Chew NWS, Lee GKH, Jing M, Goh Y, Yeo LLL, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173:317–320. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caliskan F, Dost B. The evaluation of knowledge, attitudes, depression and anxiety levels among emergency physicians during the COVID-19 pandemic. Signa Vitae. 2020;16:163–171. [Google Scholar]
- 13.Osama M, Zaheer F, Saeed H, Anees K, Jawed Q, Syed SH, et al. Impact of COVID-19 on surgical residency programs in Pakistan;a residents'perspective. Do programs need formal restructuring to adjust with the “new normal”? A cross-sectional survey study. Int J Surg. 2020;79:252–256. doi: 10.1016/j.ijsu.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al Sulais E, Mosli M, AlAmeel T. The psychological impact of COVID-19 pandemic on physicians in Saudi Arabia: a cross-sectional study. Saudi J Gastroenterol. 2020;26:249–255. doi: 10.4103/sjg.SJG_174_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Saverio S, Pata F, Gallo G, Carrano F, Scorza A, Sileri P, et al. Coronavirus pandemic and colorectal surgery: practical advice based on the Italian experience. Colorectal Dis. 2020;22:625–634. doi: 10.1111/codi.15056. [DOI] [PubMed] [Google Scholar]
- 16.BenÍtez CY, Pedival AN, Talal I, Cros B, Ribeiro MAF, Azfar M, et al. Adapting to an unprecedented scenario: surgery during the COVID-19 outbreak. Rev Col Bras Cir. 2020;47:e20202701. doi: 10.1590/0100-6991e-20202701. [DOI] [PubMed] [Google Scholar]
- 17.Yánez Benítez C, Güemes A, Aranda J, Ribeiro M, Ottolino P, Di Saverio S, et al. Impact of personal protective equipment on surgical performance during the COVID-19 pandemic. World J Surg. 2020;44:2842–2847. doi: 10.1007/s00268-020-05648-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.ElHawary H, Salimi A, Alam P, Gilardino MS. Educational alternatives for the maintenance of educational competencies in surgical training programs affected by the COVID-19 pandemic. J Med Educ Curric Dev. 2020;7:2382120520951806. doi: 10.1177/2382120520951806. [DOI] [PMC free article] [PubMed] [Google Scholar]


