Abstract
This study estimates the amount antiretroviral therapy (ART) clients paid out of pocket for preventive and treatment services and the percentage of ART clients incurring catastrophic payments during the period when ART services were transitioning from donor funding to domestic social health insurance (SHI) in Vietnam. Using a cross-sectional facility-based survey in 9 provinces, a sample of 582 clients across 18 ART facilities representatives of all facilities where SHI-financed ART was being implemented were interviewed in 2019. Results indicated 13.4% (95% CI: 5.7%, 28.2%) of clients incurred a payment for outpatient ART care. The average out of pocket expenditures for outpatient visits and HIV related outpatient visits was USD $71.2 and $8 per year, respectively. The average out of pocket expenditure for inpatient admission and HIV related inpatient admission was $7.1 and $1.6, respectively. Only 0.1% clients currently experienced HIV-related catastrophic payment at the 25% of total expenditures threshold. The study confirms the transition from donor-financed ART to SHI-financed ART is not causing financial hardship for ART clients. However, more commitment from the Government of Vietnam to strengthen HIV-related services under SHI may be needed in the future, and there is still need to ensure universal SHI coverage among people with HIV/AIDs in Vietnam.
Keywords: HIV/AIDS, antiretroviral therapy, out of pocket expenditures, catastrophic payments, Vietnam, donor transition
Introduction
Antiretroviral therapy (ART) reduces morbidity and mortality and increases the quality of life among people living with HIV (PLHIV). Therefore, access to ART has been a critical issue for HIV/AIDS control and prevention around the world.1,2 In the past, international sources such as the President’s Emergency Plan For AIDS Relief (PEPFAR) and the Global Fund to Fight AIDS, Tuberculosis and Malaria (GF) have financed the majority of the HIV/AIDS response in Vietnam. The global financial crisis together with the evolution of Vietnam to a lower-middle income country has resulted in international financial support for the HIV/AIDS response in Vietnam declining significantly over the last 5 year.3 Vietnam has committed to extending financial protection for PLHIV, including coverage of ART through Social Health Insurance (SHI). The coverage of SHI among the general population in Vietnam currently is 89.9%.4 With an annual premium of about $30, the benefit package covers both inpatient/outpatient services with a wide range of services covered from screening, diagnostics, and treatment to rehabilitation services.5 The Government Circular 15 of 20156 regulates that PLHIV coverage includes ARV treatment, other chemotherapies, medical supplies, HIV testing, and medical services for babies born to HIV-positive mothers, among other services.
According to current statistical reports from the Vietnam Authority of HIV/AIDS Control, the coverage of SHI among PLHIV was 90% in 2019. In response to the Prime Minister’s Decision No. 2188 (2016)7 and Resolution 20 of the Party’s Central Committee on Healthcare (2017),8 with the commitment to have 95% of the Vietnamese population covered by the national health insurance by 2025 and ending AIDS as a public health threat by 2030, the first centrally procured and SHI-covered ART drugs reached health facilities on 8 March 2019. With the intention to retain outpatient ART free-of-charge, at least until the transition to SHI-financed ART is completed (ie, by the end of 2020), during the period when this study took place, some clients were still receiving donor-financed ART while others were on SHI-financed ART and GF funds still sponsored CD4 and Viral Load tests.
Surveys conducted within the last 10 years indicate that, in keeping with the policies at the time that ART should be provided free of charge to clients, clients’ out of pocket expenditures (OOPE) for ART have been close to zero for outpatient care.9-11 However, after switching to SHI-covered ART, only selected groups can receive free services (ie, poor people, members of minority populations, and some other special groups) and others will have to incur a 20% copayment for any services received. To monitor the implementation of the transition of financing and identify any potential problems after the transition has been completed, this study aims to estimate the amount of ART clients’ OOPE on HIV/AIDS treatment services, including ART, treatment of opportunistic infections, and inpatient care at selected public (government-operated) facilities and to calculate the percentage of clients incurring catastrophic payments for ART services.
Methods
Study setting
This cost consequence analysis was conducted among a sample of clients representing all facilities where SHI-financed ART was being implemented (facilities still financed only via donor support at the time of the study were not part of the sample frame). The study subjects were ART clients 18 years of age or older, attending an ART clinic on the time of the survey for themselves (not, for example, picking up drugs for another person) and receiving ART through SHI financing.
Sample and survey design
Sample size was estimated on the basis on this formula:
With n being the estimated sample size needed, zα being the critical values for α = 0.05, σ is the standard deviation, d is the margin of error, and deff is the design effect due to clustering of respondents within facilities. The sample size was estimated based on having a margin of error of 200 000 Vietnamese Dong (VND) (about $8.70) for total OOPE incurred by ART clients; assuming a design effect of 1.3 and a standard deviation of 2 200 000 VND (based on a previous study assessing OOPE among clients with ART).7 The estimated sample was 604 interviews of ART clients.
This study employed a 3-stage stratified cluster design to ensure regional representation. The sample frame included the 43 provinces that have facilities where SHI-provided ARVs are provided. Provinces were selected with the probability of selection proportional to the sum of eligible ART clients, with at least 1 province selected from each of 6 regions (Central Highlands, Mekong River Delta, North Central and Central Coastal Areas, Northern Midlands and Mountain Areas, Red River Delta, and South East). The resulting sample contains 9 provinces (Hanoi, Ho Chi Minh City, Haiphong, Daklak, Tay Ninh, Lao Cai, Ca Mau, Dien Bien, Quang Tri). Facilities were then sampled with the probability of selection proportional to the number of ART clients from the selected provinces. In total, 18 unique ART facilities were selected. Within facilities, the first 20 clients to agree to the interview and meet the inclusion criteria of being 18 years of age or older and on ART were included in the sample. The final sample consisted of 582 clients (response rate of 96.3%).
All surveys were conducted by trained staff from the Hanoi University of Public Health. Interviewee answers were recorded electronically on tablets during the interview. Teams of field staff visited each facility, together with a supervisor to identify and solve any problems, answer questions, and coordinate the data collection effort. In addition, in-depth interviews were conducted with outpatient clinic (OPC) managers at all participating OPCs before data collection to collect information about the situation of ARV under SHI at the OPC as well as review barriers/enabling factors encountered when switching to the SHI payment model at OPCs.
Survey tools
This study employed and revised questionnaires from a previous study assessing OOPE among ART clients in Vietnam.11 However, the questionnaires omit some section on income, attitudes, and knowledge about health insurance that were included in the previous study. Further, questionnaires were updated to provide further clarity in wording and to capture costs for transportation and food. Revisions were piloted at 2 facilities. The main information collected in this study included socio-demographic factors, use of and expenditures on HIV prevention products, outpatient health care use during the last 30 days, inpatient health care use during the last year, and expenditures.
Measurement and definition
Expenditures assessed in this study was for the individual because the survey took place at ART clinics; thus, we did not have access to all members of household and did not have a valid means of ascertaining household expenditure. The study, therefore, modified some of the definitions and metrics used to assess poverty and catastrophic expenditures to suit the data available. An exchange rate of 23 000 Dong per US dollar is used.12 All results are presented in US dollars.
Expenditures: the study assessed the annual expenditures of the individual respondents. For some categories of responses, respondents were not able to differentiate between individual and household expenditures, and we calculate the “share” of expenditures attributed to the respondent by dividing the “household expenditure” by the total number of people in the household. Expenditures for outpatient care were asked over the period of the previous month and multiplied by 12 to obtain estimates of annual expenditures on outpatient care. Respondents were asked to report expenditures for inpatient care over the last year. To collect information about food expenditure, we asked ART clients whether they had to buy any food or drinks while waiting for ART services. To collect information about transportation, we asked ART clients whether they had to pay any fee for (1) public transportation such as a taxi, bus, or grab bike (a ridesharing company) to access OPCs to receive ART services or (2) any parking fee if they went to clinic using their own vehicles (thus, payments for petrol for their own vehicles was not included because it was difficult to estimate).
Poor and Near-poor: The government of Vietnam in 2019 used an income cut off to determine poverty of 700 000 VND/person/month in rural areas and 900 000 VND/person/month in urban areas and for “near poverty” used 1 000 000 VND/person/month in rural areas and 1 300 000 VND/person/month in urban areas.
Catastrophic payments: Catastrophic payments are often defined as occurring when the ratio between total health expenditure and total expenditures is more than 40%.13 However, other studies also suggest to use the 10% or 25% as the cut off point.14 This study employs all 3 definitions. Catastrophic payments are assessed using individual expenditures because total household expenses for health and in total were not, as explained above, available.
Data analysis
Data analyses were done using STATA/IC 16.0.15 All the analysis took into account the survey design and survey weight. Taylor-linearized standard errors are used to estimate all the confidence intervals presented in this report. Some respondent reported not knowing the amount of expenditure for certain categories. Multiple imputation with chained equations was employed to impute missing data for expenditures. Predicted mean matching was applied to avoid imputing negative expenditures.16 We also assessed catastrophic health expenditure under a scenario for year 2020 when funding from donors will no longer be available to pay for CD4 and Viral load laboratory tests.
Ethical review
This study received special exemption status with limited review from the Abt Associates, Inc. Institutional Review Board in July 2019 and approval from the Hanoi University of Public Health (HUPH) Ethical Review Board for Biomedical Research in June 2019.
Results
Characteristics of the study population
Most respondents’ highest level of education attained was secondary school (28.9%) or high school (23.6%). About 5.2% of respondents had not finished primary school (Table 1). Less than 15% of the respondent had finished university/higher education. The majority of respondents (73.7%) have regular SHI cards (ie, household cards), with 12.2% of respondents holding a SHI card that would exempt them from making copayments. The majority of respondents were working, with 51.2% reporting that they had a full-time job and 31% reporting that they had a part time job. However, most of those with full-time jobs appear to be working in the informal sector because only 9.7% of respondents had a worker social health insurance card.
Table 1.
Characteristics of the study population.
| Variable | n | % | 95%CI |
|---|---|---|---|
| Female (%) | 582 | 34.6 | (25.2, 45.3) |
| Highest level of education | |||
| No qualification | 582 | 5.2 | (2.2, 11.6) |
| Primary school | 582 | 25.7 | (19.9, 32.5) |
| Secondary school | 582 | 28.9 | (21.6, 37.5) |
| High school | 582 | 23.6 | (18.9, 29.1) |
| Vocational/training school | 582 | 3.7 | (2.4, 5.5) |
| College | 582 | 3.3 | (2.0, 5.3) |
| University | 582 | 8.6 | (4.9, 14.7) |
| Post-graduate | 582 | 1.0 | (0.3, 3.4) |
| Employment status | |||
| Full time employment | 582 | 51.2 | (41.7, 60.6) |
| Part time employment | 582 | 31.0 | (19.9, 44.8) |
| On Leave/Sick leave | 582 | 0.5 | (0.1, 4.3) |
| Seeking work | 582 | 3.0 | (1.5, 5.9) |
| Homemaker | 582 | 6.2 | (3.6, 10.4) |
| Student | 582 | 1.6 | (0.2, 12.2) |
| Not working, not looking for work | 582 | 0.7 | (0.1, 5) |
| Other | 582 | 5.5 | (4.7, 6.4) |
| Don’t know/not stated | 582 | 0.4 | (0.1, 2.9) |
| Health insurance status | |||
| SHI (Regular) | 582 | 73.7 | (50.6, 88.4) |
| SHI (Poor) | 582 | 7.3 | (1.4, 30.3) |
| SHI (Near poor) | 582 | 1.9 | (0.8, 4.4) |
| SHI (Police, military) | 582 | 1.0 | (0.3, 3.7) |
| SHI (Ethnic minority) | 582 | 3.9 | (0.5, 23.7) |
| SHI (Student) | 582 | NA | NA |
| SHI (Worker) | 582 | 9.7 | (3.3, 25.3) |
| SHI (Other) | 582 | 0.6 | (0.2, 1.8) |
| Private | 582 | 0.5 | (0.1, 3.7) |
| Other | 582 | 1.4 | (0.5, 4.3) |
| Marital status | |||
| Single | 582 | 27.9 | (18.0, 40.5) |
| Married | 582 | 49.7 | (39.1, 60.4) |
| Widowed | 582 | 6.4 | (3.4, 11.9) |
| Divorced | 582 | 11.1 | (7.5, 16.1) |
| Separated | 582 | 4.9 | (2.8, 8.2) |
Payment for health care/ART services
The ARV drugs are covered by SHI. If clients are not classified as poor or a member of other eligible group for government-paid copayments and their total amount of cost for services was over 200.000VND ($8.70 USD), they will incur copayments for examination fee, blood test, x-rays, etc. For outpatient services, 22.7% (95% CI: 11.2%, 40.7%) of the ARV clients participating in this study reported incurring an out of pocket payment during the last month (Table 2). For outpatient care related to ARV/HIV services, 13.4% (with 95% CI: 5.7%, 28.2%) made a payment. When using ARV services, 25.2% of the clients had to pay for food and/or transportation (95% CI: 19.4%, 32.1%).
Table 2.
Utilization and out of pocket payment for health care/ART services.
| Variable | n | % | 95%CI |
|---|---|---|---|
| Any payment for outpatient care, last month (%) | 582 | 22.7 | (11.2, 40.7) |
| Any payment for outpatient care related to HIV, last month (%) | 582 | 13.4 | (5.7, 28.2) |
| Paid for transport or food (related to HIV- outpatient care) (%) | 582 | 25.2 | (19.4, 32.1) |
| Percentage of patients with any inpatient admittance in last year | 582 | 16.5 | (13.0, 20.8) |
| Percentage of patients with any HIV-related inpatient admittance in last year | 582 | 3.0 | (0.9, 9.6 ) |
| Any payment for inpatient care, last year (%) | 582 | 13.9 | (11.3, 17.1) |
| Any payment for inpatient care related to HIV, last year (%) | 582 | 2.7 | (0.8, 9.1) |
For inpatient services, 13.9% of all respondents reported an out of pocket payment during the last year. The percentage of all surveyed subjects reporting an out of pocket payment for HIV/AIDS related inpatient care was 2.7% (with 95% CI: 0.8%, 9.1%).
Table 3 provides separate estimates of the amount of out of pocket payment among all respondents and among those who incurred any payment for services. Overall, an ART client had to pay $71.2 (with 95% CI: 30.2, 112.3) per year for outpatient visits of which $8.0 (with 95% CI: 2.5, 13.6) was related to HIV. On average, an ART client paid $7.1 (with 95% CI: 0, 17.1) and $1.6 (with 95% CI: 0, 5.4) per year for inpatient admission and inpatient admission related to HIV, respectively.
Table 3.
Estimated OOPE for health care/HIV services during the last 12 months.
| Variable | n | Average OOPE among all ART patients | n | Average OOPE among who paid |
|---|---|---|---|---|
| Prevention services | ||||
| Condom | 575 | 5.8 (3.2; 8.3) | 137 | 23.5 (16.4; 30.6) |
| Outpatient utilization | ||||
| Total paid for outpatient care (including outside health facility) | 577 | 71.2 (30.2; 112.3) | 85 | 312.1 (242.8; 381.4) |
| Total paid for outpatient care related to HIV | 582 | 8.0 (2.5; 13.6) | 39 | 60.1 (41.3; 78.9) |
| Paid for transport or food (related to HIV) | 578 | 14.5 (8.4; 20.6) | 138 | 58.4 (46.2; 70.7) |
| Inpatient utilization | ||||
| Total paid for inpatient care | 582 | 7.1 (0; 17.1) | 67 | 42.0 (0.0; 91.3) |
| Total paid for inpatient care related to HIV | 582 | 1.6 (0; 5.4) | 15 | 58.6 (0.0; 126.0) |
| Total paid for all health care | 582 | 78.9 (45.6; 117.2) | 118 | 309.5 (250.1: 375.9) |
| Total paid for all care related to HIV | 582 | 10.5 (3.9; 15.9) | 45 | 73.7 (27.5; 120) |
Catastrophic payment for ART services
Table 4 presents information about catastrophic payment for ART services. The percentage of clients incurring a catastrophic payment at the 25% cut-off point for HIV related health care among the study sample was 0.1% (with 95% CI: 0-0.4%). If using the cut-off point of 10%, the percentage with a catastrophic payment for HIV-related health care was 1.5% (with 95% CI: 0.1, 2.9%). When including food and transportation for HIV-related health care, about 3.8% of respondents incurred catastrophic payment of more than 10% of total expenditure (with 95% CI: 1.9%, 5.7%)
Table 4.
Percentage of respondents incurring catastrophic payments.
| Variable | N | % | 95%CI |
|---|---|---|---|
| Proportion with catastrophic payments for health care (all cause) | |||
| >25 | 577 | 2.5 | (0.9, 3.8) |
| >10 | 577 | 9.1 | (3.7, 14.5) |
| Proportion with catastrophic payments for HIV related health care | |||
| >25 | 577 | 0.1 | (0.0-0.4) |
| >10 | 577 | 1.5 | (0.1-2.9) |
| Proportion with catastrophic payments for HIV related health care with food/transportation | |||
| >25 | 577 | 1.0 | (0.0, 2.2) |
| >10 | 577 | 3.8 | (1.9, 5.7) |
Beginning in 2020, clients on SHI will have to pay copayments for all services, including CD4 and Viral Load tests, and funding from the Provincial People’s Committees (or from left-over donor funds) may not be available. Thus, we also assessed HIV-related health expenditures as percentage of total expenditure under this scenario in Figure 1 (ie, where clients have to pay 20% copayment for all services) using the existing SHI fee schedule. Based on this projected scenario, the percentage incurring catastrophic payments of 10% or more would be 37.2% (with 95% CI: 25.9, 48.5) and the percentage incurring a catastrophic payment of 25% or more would be 34.2% (with 95% CI: 23.2, 45.2).
Figure 1.
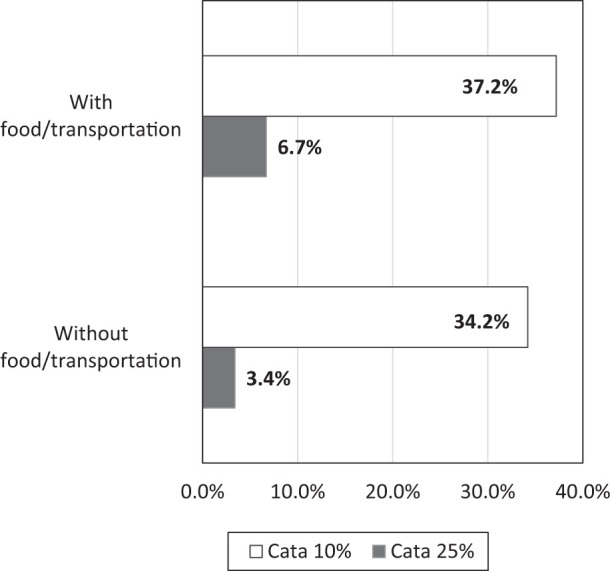
Proportion with catastrophic payments for HIV related health care under scenario estimation.
Discussion
This study generates some of the first estimates of co-payments for health care and ART among ART clients using SHI during a period transition from donor financing to SHI financing. The average OOPE for HIV related outpatient visits was 185 000 VND ($8.04) per year (95% CI: 57 300, 312 000). The average OOPE for HIV related inpatient admission was 37 000 VND ($1.61) per year. The proportion of ARV clients reporting OOPE for outpatient care increased from 3.7% in 201511 to 13.4% in this study. The transition from donor support to SHI as the vehicle for financing ARVs means that clients on ART must enroll in SHI to access ARVs or, if they do not enroll in SHI, pay the full price of ARVs out of pocket. For clients accessing ARVs financed by SHI, the general policies of the broader SHI scheme apply to ART. Thus, clients who are not eligible for government-paid copayments must incur copayments for the ARVs.5 From the distribution of SHI types in this study, only 12.2% of respondents are entitled to free ARV services. However, only 13.4% (95% CI: 5.7%, 28.2%) of clients incurred a payment for outpatient ART care. The in-depth interviews with staff in charge of ARV services identified 3 potential reasons for this low co-payment rate. First, the staff at OPCs often tried to reduce the amount of payment per visits to less than the 200.000VND threshold for incurring a copayment so that the clients did not have to make a payment. Second, OPC staff were aware of the difficult situation of ART clients, and thus they tried to mobilize support from all possible sources to pay for the 20% amount not covered by insurance (ie, funding from the People’s Committee in some provinces and left-over funds from donor sources in some other provinces). Third, the Global Fund was still paying for CD4 and Viral Load tests until the end of September 2019. This helps to explain why the average OOPE for ART outpatient visits was still low, at $8 USD per year.
Inpatient service utilization declined compared to a survey conducted in 2015 utilizing a similar methodology. The percentage of clients with any HIV-related inpatient admittance in last year in this study was only 3% compared to 5% reported in the 2015 study.11 However, these differences are not statistically significantly different, so it is difficult to draw conclusions about trends in inpatient care and OOPE for inpatient care among ART clients from these studies.
Previous studies have suggested to use catastrophic out of pocket spending as indicator to measure financial protection for universal health coverage.17,18 This study also examined catastrophic payment with large expenditure defined as 10% and 25% of total expenditure14 as an indicator to measure financial protection for ARV clients when switching into the domestic health insurance scheme. Due to the current low rate of incurring a copayment and relatively small amount of overall OOPE, utilization of HIV/AIDS treatment has not yet created a large financial burden on clients on ART. This points to successful mitigation of the potential financial burden of accessing ART during the transition from donor financing to SHI financing: only 0.1% currently experienced HIV related- catastrophic payment at the 25% threshold. However, further monitoring is needed because the GF support for laboratory tests and Provincial People’s Committee support for copayments is being or has been withdrawn. Further, reforms in the delivery of ART, such as multi-month dispensing of ARVs, may make it more difficult to limit the amount of payment per visits to less than the 200.000VND. These factors may cause copayments among ART clients to increase. Based on the projected scenario when ART clients would have to pay for all the laboratory test, the proportion of incurring HIV-related catastrophic payment at 25% increased to 3.4% and catastrophic payment at 10% increased to 34.2%.
This survey was a cross-sectional study which was administered in health facilities among SHI clients; thus, the study sample may be subjected to selection bias. First, we interview only clients who came to health facilities at the study time, clients who were sick, staying at home or admitted to hospital would not be able to join the study. Therefore, the study sample may not capture the sub-groups of population with higher utilization of health services due to their worse health status. Second, the study sample included only ART clients using the SHI scheme for their services, therefore, these estimations may not applicable for the entire population of all ART clients. Third, this study used total expenditure as a tool to estimate poverty, catastrophic payment and impoverishment. Previous studies have showed that this method can be subject to bias as respondents might not be able to remember their expenditures correctly.19
Conclusion
The findings show that the transition from donor-financed ART to SHI-financed ART is not causing financial hardship for ART clients: about 1 in 8 clients on SHI-financed ART incurred OOPE, but the amount of OOPE was affordable for all clients and represented less than 5% of total expenditures. However, as other donor and domestic sources of financing end, clients’ OOPE for ART will likely be higher on average. The study confirmed the benefit of SHI in protecting PLHIV from severe financial consequences of healthcare payments during the transition from donor-financed ART to SHI-financed ART, but further action may be necessary to limit OOPE after the transition is fully completed, including ensuring that all PLHIV are enrolled in SHI. Further studies are also needed to measure forgone care for HIV/AIDS care and health care among PLHIV.
Acknowledgments
The authors would like to thank Le Tu Hoang (HUPH) for help in designing and programming the survey instruments. HFG Vietnam team helped facilitate the entire process as well as providing specific comments on the objectives of the survey and interpretation of the results. Thanks to USAID Vietnam for financial and technical support throughout the analyses presented in this report. The opinions expressed herein are those of the authors and do not necessarily reflect the views of the United States Agency for International Development or Abt associates
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the United States Agency for International Development through the Health Finance and Governance Project.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author contributions: VTHL and BJ conceptualized the study and initial hypothesis. All authors conducted data collection. VTHL and BJ conducted analysis and interpretation. VTHL and BJ prepared the manuscript. All authors provided intellectual input and contributed to the development of the manuscript. All authors have read and approved the final manuscript.
ORCID iDs: Lan Thi Hoang Vu  https://orcid.org/0000-0001-8528-357X
https://orcid.org/0000-0001-8528-357X
Quyen Thi Tu Bui  https://orcid.org/0000-0002-5061-8488
https://orcid.org/0000-0002-5061-8488
Hien Nguyen Thi  https://orcid.org/0000-0002-1787-237X
https://orcid.org/0000-0002-1787-237X
References
- 1. Keiser P, Nassar N, Kvanli MB, Turner D, Smith JW, Skiest D. Long-term impact of highly active antiretroviral therapy on HIV-related health care costs. J Acquir Immune Defic Syndr. 2001;27:14-19. doi: 10.1097/00126334-200105010-00003 [DOI] [PubMed] [Google Scholar]
- 2. Jordan R, Gold L, Cummins C, Hyde C. Systematic review and meta-analysis of evidence for increasing numbers of drugs in antiretroviral combination therapy. BMJ. 2002;324:757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Todini N, Hammett TM, Fryatt R. Integrating HIV/AIDS in Vietnam’s Social Health Insurance Scheme: experience and lessons from the health finance and governance project, 2014–2017. Health Syst Reform. 2018;4:114-124. doi: 10.1080/23288604.2018.1440346 [DOI] [Google Scholar]
- 4. Government of Vietnam. Report No. 413 / BC-CP of September 20, Reporting to the National Assembly on the Implementation of Social Health Insurance Assigned by National Assembly’s Resolution No. 68/2013 / QH13; 2019. [Google Scholar]
- 5. Dao HL, Fuenzalida-Puelma HL, Hurt KL, Somanathan A, Tandon A. Moving toward Universal Coverage of Social Health Insurance in Vietnam: Assessment and Options (English). Directions in Development; Human Development. Washington, DC: World Bank Group; http://Documents.Worldbank.Org/Curated/En/383151468138892428/Moving-toward-Universal-Coverage-of-Social-Health-Insurance-in-Vietnam-Assessment-and-Options [Google Scholar]
- 6. The Ministry of Health. Circular No. 15/2015/TT-BYT: providing guidance on medical examination and treatment covered by Health Insurance for HIV-positive people and people using HIV/AIDS-related health care services. 2015. Accessed January 10, 2020 https://thuvienphapluat.vn/van-ban/The-thao-Y-te/Thong-tu-15-2015-TT-BYT-kham-chua-benh-bao-hiem-y-te-doi-nguoi-nhiem-HIV-AIDS-279733.aspx
- 7. The Prime Minister. Decision No: 2188 /QD-TTg: regulating the payment for the centralized procurement of ARV using Health Insurance Fund and support for ARV users. 2016. Accessed January 10, 2020 https://thuvienphapluat.vn/van-ban/Bao-hiem/Quyet-dinh-2188-QD-TTg-thanh-toan-thuoc-khang-virut-HIV-mua-sam-tap-trung-cap-quoc-gia-2016-329879.aspx
- 8. Resolution 20-NQ / TW 2017 enhances people’s health in the new situation. 2017. Accessed January 14, 2021 https://thuvienphapluat.vn/van-ban/The-thao-Y-te/Nghi-quyet-20-NQ-TW-2017-tang-cuong-cong-tac-bao-ve-cham-soc-nang-cao-suc-khoe-nhan-dan-365599.aspx
- 9. Tran BX, Duong AT, Nguyen LT, et al. Financial burden of health care for HIV/AIDS patients in Vietnam. Trop Med Int Health. 2013;18:212-218. doi: 10.1111/tmi.12032 [DOI] [PubMed] [Google Scholar]
- 10. Barennes H, Frichittavong A, Gripenberg M, Koffi P. Evidence of high out of pocket spending for HIV care leading to catastrophic expenditure for affected patients in Lao People’s Democratic Republic. PLoS One. 2015;10:e0136664. doi: 10.1371/journal.pone.0136664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Johns B, Chau LB, Hanh KH, et al. The importance of assessing out-of-pocket payments when the financing of antiretroviral therapy is transitioned to domestic funding: findings from Vietnam. Trop Med Int Health. 2017;22:908-916. doi: 10.1111/tmi.12897 [DOI] [PubMed] [Google Scholar]
- 12. USD to VND Exchange Rate. Bloomberg.com. Accessed September 1, 2019 https://www.bloomberg.com/quote/USDVND:CUR
- 13. Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111-117. doi: 10.1016/S0140-6736(03)13861-5 [DOI] [PubMed] [Google Scholar]
- 14. Wagstaff A, Flores G, Hsu J, et al. Progress on catastrophic health spending in 133 countries: a retrospective observational study. Lancet Global Health. 2018;6:e169-e179. doi: 10.1016/S2214-109X(17)30429-1 [DOI] [PubMed] [Google Scholar]
- 15. StataCorp LP. Stata Statistical Software: Release 16. StataCorp LLC. Published online 2019. [Google Scholar]
- 16. Little RJA. Missing-data adjustments in large surveys. J Bus Econ Stat. 1988;6:287-296. doi: 10.1080/07350015.1988.10509663 [DOI] [Google Scholar]
- 17. Wagstaff A, van Doorslaer E. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993-1998. Health Econ. 2003;12:921-934. doi: 10.1002/hec.776 [DOI] [PubMed] [Google Scholar]
- 18. Boerma T, Eozenou P, Evans D, Evans T, Kieny M-P, Wagstaff A. Monitoring progress towards universal health coverage at country and global levels. PLoS Med. 2014;11:e1001731. doi: 10.1371/journal.pmed.1001731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lu C, Chin B, Li G, Murray CJ. Limitations of methods for measuring out-of-pocket and catastrophic private health expenditures. Bull World Health Organ. 2009;87:238-244. doi: 10.2471/BLT.08.054379 [DOI] [PMC free article] [PubMed] [Google Scholar]


