Abstract
Background:
In the presence of medial meniscus posterior root tear (MMPRT), there is a possibility of reduced compression of meniscal tissue in hyperflexion as the intra-articular mobility of the meniscus increases. This phenomenon can be mimicked during clinical examination.
Purpose:
To describe, evaluate, and validate the diagnostic performance of a new clinical indicator, the Akmese sign, for the diagnosis of an MMPRT.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
In this study, we prospectively enrolled patients aged 18 to 55 years who were scheduled for arthroscopic surgery after a diagnosis of medial meniscal lesion at a single institution between January 2016 and January 2018. All of the patients underwent preoperative examination for the Akmese sign. All surgeries were performed by a single surgeon with more than 5 years of experience in sports injury surgery, who was blinded to the Akmese sign results.
Results:
A total of 273 patients with a mean age of 42.4 ± 5.3 years met the study criteria. The Akmese sign was identified as positive in 33 patients, and MMPRT was confirmed during arthroscopy in 36 cases. The performance parameters of the Akmese sign were a sensitivity of 86.1%, specificity of 99.1%, Youden index of 0.85, and kappa index of 0.88.
Conclusion:
This study showed that the Akmese sign is a useful new physical examination test that can help clinicians distinguish MMPRTs from other meniscal medial meniscal pathology.
Keywords: medial menisci, root tear, Akmese sign, knee, arthroscopy, transtibial technique
Medial meniscus posterior root tear (MMPRT), including root avulsions and radial tears adjacent to the root, is biomechanically similar to total medial meniscectomy.2,25,28 An MMPRT results in medial meniscal extrusion, which dramatically impairs hoop tension, which allows correct intra-articular load transmission16 and for which the medial meniscus is approximately 90% responsible, thereby leading to accelerated degenerative arthritis of the knee.11,14,20,27 Therefore, early diagnosis and repair of the MMPRT play an important role in the prevention of gonarthrosis. There is no specific and sensitive clinical diagnostic sign of MMPRT in the literature. Magnetic resonance imaging (MRI) is a useful diagnostic tool, but the gold standard for MMPRT diagnosis is the arthroscopic view of the meniscus.
The aim of this study was to define a new clinical sign for the diagnosis of MMPRT. During knee flexion, there is limited posterior movement (average, 4 mm) in the medial meniscus, as it is limited by the posterior root of the medial meniscus.4,10,26,27 However, this limitation of movement disappears when there is MMPRT. The hypothesis of this study was that in the knee of a patient with MMPRT, the severe tenderness in the medial joint line during extension or lower flexion angles resolves or becomes minimal during hyperflexion (>90°) because the impingement and extrusion of the medial meniscus is eliminated by the posterior overmobilization of the medial meniscus.
Methods
This single-center, prospective study was conducted at a reference center for sports injuries at a university hospital between January 2016 and January 2018. Institutional review board approval was obtained before the start of the study, and the Standards for Reporting Diagnostic Accuracy Studies guidelines were followed during the study.6
The inclusion criteria for the study were patients diagnosed with a medial meniscal lesion to be treated with arthroscopic surgery, with indications for surgery based on clinical symptoms and findings determined on preoperative knee MRI slices evaluated by the senior author (R.A.). All of the operations were performed by this author, who has more than 5 years of experience in sports injury surgery.
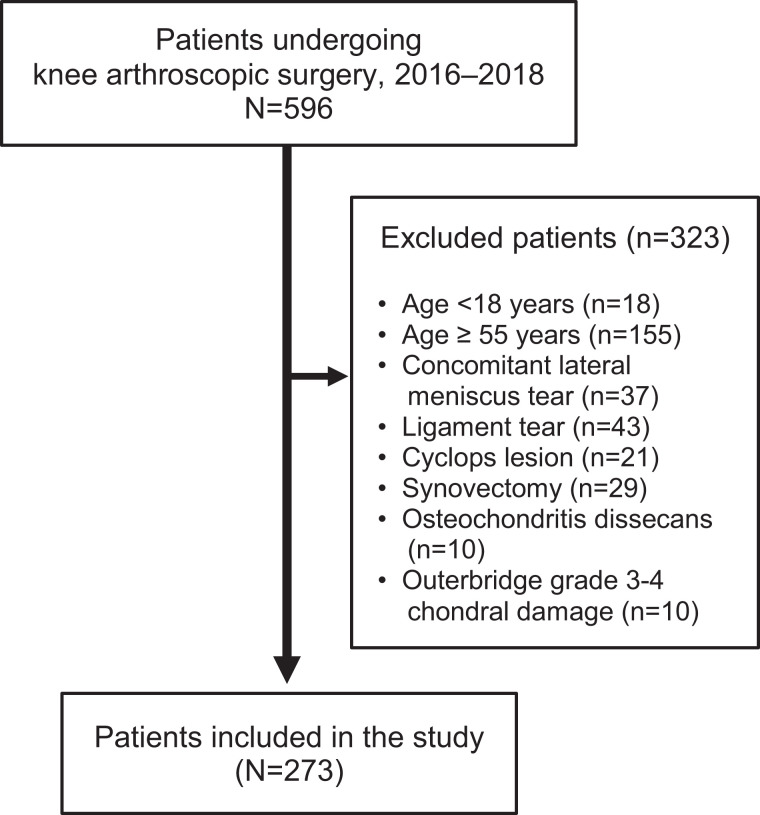
The exclusion criteria were patients younger than 18 years or older than 55 years, concomitant tears of the lateral meniscus, ligament tears, mucoid degeneration of the anterior cruciate ligaments, a cyclops lesion, arthrolysis, synovectomies for pigmented villonodular synovitis of the knee, Outerbridge grade 3 or 4 chondral lesions, Kellgren-Lawrence grade ≥2, articular debridement, or ablation of a foreign body (Figure 1).
Figure 1.
Flow diagram showing the patients included in and excluded from the study.
Akmese Sign
This test is applied during clinical examination. With the patient lying supine, the lower extremity to be examined is brought into a figure-of-4 position. This allows the knee to have a slight varus position (or at least ensure that there is no valgus force on the knee) causing the medial collateral ligament and medial capsule to release. Then, protecting external rotation of the hip and flexion, the medial joint line is palpated for pain/sensitivity while knee flexion is lowered to 10° to 20° (near extension) (Figure 2A). Next, while taking the knee into hyperflexion (110°-130°), the medial joint line is palpated again for pain/sensitivity (Figure 2B). Patients with severe tenderness in angles near extension and minimal or no tenderness in hyperflexion were considered to have a positive Akmese sign (see online Video Supplement 1).
Figure 2.
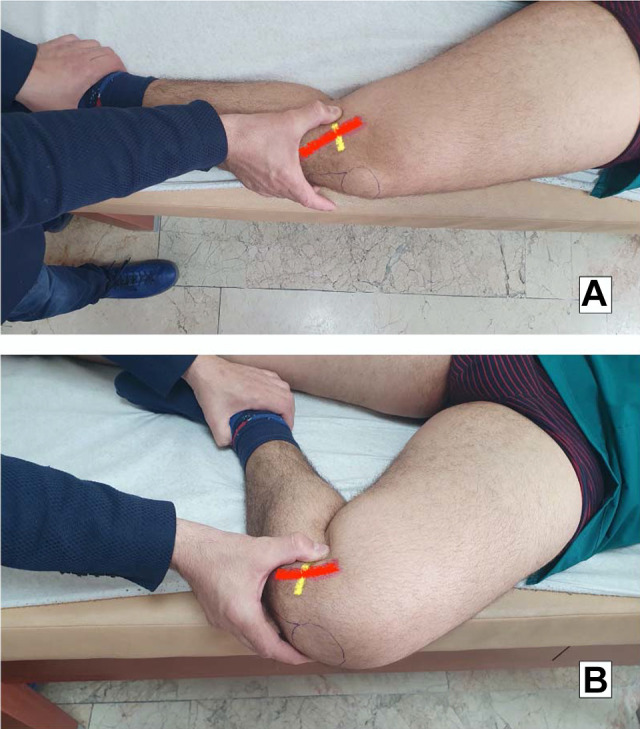
Examination for Akmese sign. The yellow line indicates the joint level, the red line indicates the medial collateral ligament. (A) The leg to be examined is brought into a figure-of-4 position, then the medial joint line is palpated for pain/sensitivity while knee flexion is lowered to 10° to 20° (near extension). (B) While taking the knee into hyperflexion (110°-130°), the medial joint line is palpated again for pain/sensitivity.
All the patients were examined preoperatively for the Akmese sign by a single examiner with 5 years of experience in hip and knee surgery (H.K.), who was blinded to the clinical data and MRI results. The senior author performing the operations was blinded to this information.
Determination of MMPRT
A definitive diagnosis of MMPRT was made during arthroscopic examination. Classification of the MMPRT was made using the LaPrade classification system.3
Statistical Analysis
Statistical analyses were performed using SPSS software. Agreement between the Akmese sign and arthroscopic evaluation of the meniscus was determined with the Cohen kappa coefficient, where κ < 0.20 signified no agreement; 0.21 to 0.39, minimal agreement; 0.40 to 0.59, weak agreement; 0.60 to 0.79, moderate agreement, 0.80 to 0.90, strong agreement, and >0.90, almost-perfect agreement. The parameters for the diagnostic performance of the Akmese sign were calculated in relation to arthroscopy, the reference test with sensitivity and specificity with 95% CI, positive and negative predictive value, the Youden index (the closer the index is to +1, the more useful the test), the percentage of well-classified patients (exactitude), and the relationship with positive likelihood (a higher value indicates greater value of the test).
Results
Of the 596 patients initially identified as cases of knee arthroscopy, 273 met the selection criteria. The demographic data and diagnoses of meniscus tear of the study patients are shown in Table 1.
Table 1.
Demographic and Intraoperative Data of Patientsa
| Value | |
|---|---|
| Age, years | 42.4 ± 5.3 |
| Gender | |
| Male | 187 (67.5) |
| Female | 86 (31.5) |
| BMI, kg/m2 | 25.9 ± 2.5 |
| Preoperative varus alignment, deg | 3 ± 2.4 |
| Intraoperative diagnosis | |
| MMPRT | 36 (13.2) |
| No MMPRT | 237 (86.8) |
| Surgical treatment of choice for MMPRT | |
| Fixation with transtibial technique | 32 |
| Partial meniscectomy | 4 |
aData are reported as n (%) or mean ± SD. BMI, body mass index; MMPRT, medial meniscal posterior root tear.
Of the 273 patients, 33 had a positive Akmese sign. In the arthroscopic examination (reference evaluation), MMPRT was observed in 36 of the 273 patients. The agreement between the Akmese sign and arthroscopy, and the sensitivity and specificity values for the test, are shown in Tables 2 and 3.
Table 2.
Correlation Between the Akmese Sign and Arthroscopy for the Diagnosis of an MMPRTa
| MMPRT Arthroscopy + |
MMPRT Arthroscopy – |
Total | |
|---|---|---|---|
| Akmese sign + | 31 | 2 | 33 |
| Akmese sign – | 5 | 235 | 240 |
| Total | 36 | 237 | 273 |
aMMPRT, medial meniscal posterior root tear.
Table 3.
The Statistical Power of the Akmese Signa
| Sensitivity | Specificity | PPV | NPV | Youden index | Kappa | |
|---|---|---|---|---|---|---|
| Akmese sign | 86.1% | 99.1% | 93.9% | 97.9% | 0.85 | 0.88 |
aData are reported as %. NPV, negative predictive value; PPV, positive predictive value.
A post hoc power analysis revealed that the study had 100% power to show the efficacy of the Akmese sign in detecting MMRPT.
Discussion
The most important finding of this study was the defining of a specific and sensitive physical examination test (Akmese sign) in the preoperative diagnosis of MMPRT.
During knee flexion, the lateral meniscus moves posteriorly by 19 mm on average, whereas more limited movement of an average of 4 mm occurs in the medial meniscus. Thus, the medial meniscus is more vulnerable to impingement between the femoral condyle and tibial plateau.4,26,27 The posterior root of the medial meniscus limits posterior overmobilization. However, in hyperflexion of the knee, there is much more posterior mobilization of the medial meniscus in MMPRT than in a meniscus with an intact posterior root.2 The Akmese sign demonstrates pain with direct palpation of the joint line in extension where the meniscus is close to its anatomic position but extruded slightly, and the disappearance of tenderness in hyperflexion where the meniscal tissue is subluxated and not in direct contact with the examiner’s finger (see online Video Supplements 2 and 3). This impingement and medial extrusion of the medial meniscus seen in angles near extension but not in hyperflexion may explain the positive Akmese sign in the presence of MMPRT. The Akmese sign is clinically sound because the posterior overmobilization of the medial meniscus during hyperflexion can only be present in MMPRT, which resolves the impingement and medial extrusion of the meniscus.
MMPRTs are more common than other root tears because the medial meniscus posterior root has the least mobility of all the meniscus roots.13,22,26 Of arthroscopic meniscal repairs or meniscectomies, 10% to 21% have been reported as MMPRT. Increased age, female sex, increased body mass index, and decreased sports activity levels have been associated with a higher incidence of medial root tears.4,12,22 Guermazi et al9 reported that meniscal tears that were combined with severe articular damage were of root tear origin in 76.7% of cases and different origins in 19.7% of cases. The relative association of meniscal damage with root tears was greater than with other types of tears. However, many meniscus root tears cannot be diagnosed in the early period.1,2,8 Some clinical symptoms of MMPRTs have been reported. Habata et al10 reported that patients heard a popping sound of the knee in response to a trivial injury. Patients with MMPRTs may report a history of joint line pain but the mechanical symptoms such as locking, catching, or giving way are less likely to be present.3 Lee et al17 reported that only 14.3% and 9.5% of the patients with MMPRTs complained of knee locking and giving way, respectively. In the same study, McMurray testing was positive in only 57.1% of patients with MMPRTs.17 Seil et al24 reported a new clinical sign that can be used in the diagnosis and clinical follow-up of medial meniscus posterior root lesions. A new varus stress test was performed with the patient fully relaxed and the knee in full extension. As varus stress was applied, the anteromedial joint line was palpated and meniscal extrusion was reproduced. The extrusion disappeared when the knee was returned to normal alignment.
MRI has become increasingly used to diagnose MMPRTs owing to the absence of highly specific and sensitive clinical signs. However, making an accurate diagnosis with MRI is often dependent on the quality of the imaging and the skill of the radiologist.3 The sensitivity of 3-T MRI in the identification of posterior root tears is 77% and specificity is 73%.21 T2-weighted sequences are generally considered to be the best images for the visualization of tears, given their maximum specificity and sensitivity values.18 The presence of medial meniscal extrusion has been described as a finding that is highly correlated with the presence of an MMPRT.5,21 Extrusion is diagnosed when the meniscal body is displaced >3 mm past the tibial articular surface on a midcoronal image. Over 50% of patients with medial meniscal extrusion on MRI will have MMPRTs.7,20 Another important MRI finding in an MMPRT is the “ghost sign” seen on sagittal images. This is the absence of an identifiable meniscus in the sagittal plane or a high signal replacing the normal dark meniscal signal.15,20,23 Other signs of medial meniscus posterior root lesions include a radial linear defect at the posterior bony insertion of the meniscus roots on axial imaging and vertical linear defects on coronal imaging.15 Lee et al19 proposed that MMPRTs would not be difficult to diagnose if the diagnosis were based on 3 different discriminatory features on MRI-plane images together with the clinical symptoms. The 3 discriminatory MRI features were stated to be the ghost sign from the sagittal plane (detection rate of 100%), the vertical linear defect on the coronal plane (100%), and the radial linear defect on the axial plane (94%).
The gold standard for the diagnosis of a meniscus root lesion is direct visualization during arthroscopy.21 However, this is an intraoperative diagnosis, and to be able to diagnose MMPRT preoperatively, an accurate clinical sign is needed. The Akmese sign defined in this study seems to be an accurate physical examination that can be used easily on all patients with meniscal problems. However, caution should be paid when examining patients with limited range of motion at the hip or ligamentous laxity/trauma in the collateral ligaments.
The strong points of this study are the large number of patients and the validation of the Akmese sign compared with the reference test of arthroscopy. In daily clinical practice, this simple clinical sign can be investigated to suggest the presence of an MMPRT and to guide the radiologist, and then the surgeon, in the management of these lesions.
There were some limitations to this study, primarily that the tests were subjective in nature, depending solely on the pain perception level of the patients. This could be a potential limiting factor affecting the test results. Moreover, for this study we had only 1 examiner, which may have decreased the reproducibility of the test. Future studies are planned for inter- and intraobserver evaluation of the Akmese sign. The tenderness tests were used only on patients with meniscal problems, thus giving an exclusion ratio up to 54%. However, this choice was made deliberately in order to ensure homogeneity of the cohort. The results of the Akmese sign are not known in patients with ligament injuries, especially in those with medial collateral lesions, where knee kinematics are severely affected, limiting the specificity and sensitivity of the sign. In addition, patients with knee pathologies other than medial meniscal pathologies, Kellgren-Lawrence grade ≥2, and Outerbridge grade 3 and 4 chondral lesions were excluded; these kinds of knees may show different characteristics with the Akmese sign.
Conclusion
The Akmese sign is a new, useful, physical examination that should be used in the preoperative evaluation of the knee, which has high specificity and sensitivity for distinguishing MMPRTs from other medial meniscal pathology.
A Video Supplement for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/2325967120975511.
Footnotes
Final revision submitted July 13, 2020; accepted July 31, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Ankara University (04-249-18).
References
- 1. Ahn JH, Lee YS, Chang J-Y, Chang MJ, Eun SS, Kim SM. Arthroscopic all inside repair of the lateral meniscus root tear. Knee. 2009;16(1):77–80. [DOI] [PubMed] [Google Scholar]
- 2. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus: similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–1931. [DOI] [PubMed] [Google Scholar]
- 3. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–3030. [DOI] [PubMed] [Google Scholar]
- 4. Bin S-I, Kim J-M, Shin S-J. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20(4):373–378. [DOI] [PubMed] [Google Scholar]
- 5. Choi C-J, Choi Y-J, Lee J-J, Choi C-H. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy. 2010;26(12):1602–1606. [DOI] [PubMed] [Google Scholar]
- 6. Cohen JF, Korevaar DA, Altman DG, et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open. 2016;6(11):e012799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17–23. [DOI] [PubMed] [Google Scholar]
- 8. Feucht MJ, Salzmann GM, Bode G, et al. Posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):119–125. [DOI] [PubMed] [Google Scholar]
- 9. Guermazi A, Hayashi D, Jarraya M, et al. Medial posterior meniscal root tears are associated with development or worsening of medial tibiofemoral cartilage damage: the multicenter osteoarthritis study. Radiology. 2013;268(3):814–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Habata T, Uematsu K, Hattori K, Takakura Y, Fujisawa Y. Clinical features of the posterior horn tear in the medial meniscus. Arch Orthop Trauma Surg. 2004;124(9):642–645. [DOI] [PubMed] [Google Scholar]
- 11. Hein CN, Deperio JG, Ehrensberger MT, Marzo JM. Effects of medial meniscal posterior horn avulsion and repair on meniscal displacement. Knee. 2011;18(3):189–192. [DOI] [PubMed] [Google Scholar]
- 12. Hwang B-Y, Kim S-J, Lee S-W, et al. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40(7):1606–1610. [DOI] [PubMed] [Google Scholar]
- 13. Jones AO, Houang MTW, Low RS, Wood DG. Medial meniscus posterior root attachment injury and degeneration: MRI findings. Australas Radiol. 2006;50(4):306–313. [DOI] [PubMed] [Google Scholar]
- 14. Kan A, Oshida M, Oshida S, Imada M, Nakagawa T, Okinaga S. Anatomical significance of a posterior horn of medial meniscus: the relationship between its radial tear and cartilage degradation of joint surface. Sports Med Arthrosc Rehabil Ther Technol. 2010;2(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kim SB, Ha JK, Lee SW, et al. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27(3):346–354. [DOI] [PubMed] [Google Scholar]
- 16. Koenig JH, Ranawat AS, Umans HR, DiFelice GS. Meniscal root tears: diagnosis and treatment. Arthroscopy. 2009;25(9):1025–1032. [DOI] [PubMed] [Google Scholar]
- 17. Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25(9):951–958. [DOI] [PubMed] [Google Scholar]
- 18. Lee SY, Jee W-H, Kim J-M. Radial tear of the medial meniscal root: reliability and accuracy of MRI for diagnosis. AJR Am J Roentgenol. 2008;191(1):81–85. [DOI] [PubMed] [Google Scholar]
- 19. Lee YG, Shim J-C, Choi YS, Kim JG, Lee GJ, Kim HK. Magnetic resonance imaging findings of surgically proven medial meniscus root tear: tear configuration and associated knee abnormalities. J Comput Assist Tomogr. 2008;32(3):452–457. [DOI] [PubMed] [Google Scholar]
- 20. Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33(10):569–574. [DOI] [PubMed] [Google Scholar]
- 21. Magee T. MR findings of meniscal extrusion correlated with arthroscopy. J Magn Reson Imaging. 2008;28(2):466–470. [DOI] [PubMed] [Google Scholar]
- 22. Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):849–854. [DOI] [PubMed] [Google Scholar]
- 23. Papalia R, Vasta S, Franceschi F, D’Adamio S, Maffulli N, Denaro V. Meniscal root tears: from basic science to ultimate surgery. Br Med Bull. 2013;106(1):91–115. [DOI] [PubMed] [Google Scholar]
- 24. Seil R, Dück K, Pape D. A clinical sign to detect root avulsions of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2072–2075. [DOI] [PubMed] [Google Scholar]
- 25. Shybut TB, Vega CE, Haddad J, et al. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament–deficient knee. Am J Sports Med. 2015;43(4):905–911. [DOI] [PubMed] [Google Scholar]
- 26. Thompson WO, Thaete FL, Fu FH, Dye SF. Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med. 1991;19(3):210–216. [DOI] [PubMed] [Google Scholar]
- 27. Vedi V, Spouse E, Williams A, Tennant SJ, Hunt DM, Gedroyc WMW. Meniscal movement: an in-vivo study using dynamic MRI. J Bone Joint Surg Br. 1999;81(1):37–41. [DOI] [PubMed] [Google Scholar]
- 28. Vyas D, Harner CD. Meniscus root repair. Sports Med Arthrosc Rev. 2012;20(2):86–94. [DOI] [PubMed] [Google Scholar]