Abstract
Background:
Worldwide disparities in surgical capacity are a significant contributor to health inequalities. Safe surgery and infection prevention and control depend on effective sterile processing (SP) of surgical instruments; however, little is known about SP in low- and middle-income countries (LMICs), where surgical site infection is a major cause of postoperative morbidity and mortality.
Aim:
To appraise and synthesise available evidence on SP in LMICs.
Methods:
An integrative review of research literature was conducted on SP in LMICs published between 2010 and 2020. Studies were appraised and synthesised to identify challenges and opportunities in practice and research.
Results:
Eighteen papers met the inclusion criteria for qualitative analysis. Challenges to advancing SP include limited available evidence, resource constraints and policy-practice gaps. Opportunities for advancing SP include tailored education and mentoring initiatives, emerging partnerships and networks that advance implementation guidelines and promote best practices, identifying innovative approaches to resource constraints, and designing and executing quality assurance and surveillance programmes.
Discussion:
Research investigating safe surgery, including SP, in LMICs is increasing. Further research and evidence are needed to confirm the generalisability of study findings and effectiveness of strategies to improve SP practice in LMICs. This review will help researchers and stakeholders identify opportunities to contribute. The burdens of unsafe surgery transcend geopolitical borders, and the global surgery and research communities are called upon to negotiate historical and present-day inequities to achieve safe surgery for all.
Keywords: Sterile processing, surgical instruments, surgical site infection, infection prevention, low- and middle-income countries, health equity, global health
Background
Worldwide disparities in surgical capacity are a significant contributor to health inequalities. The Lancet Commission on Global Surgery has called attention to the five billion people worldwide who lack access to safe and affordable surgical and anaesthesia care, as well as the millions of people who face catastrophic out-of-pocket expenditures when they do access surgical care (Meara et al., 2015). The cohort followed in the pivotal African Surgical Outcomes Study had a postoperative mortality rate twice that of global averages despite being younger, having lower risk profiles and experiencing fewer postoperative complications (Biccard et al., 2018). Low- and middle-income countries (LMICs) are disproportionately affected by the morbidity, mortality and socioeconomic burdens of untreated surgical conditions and postoperative complications, including disability, infection, longer lengths of stay, re-intervention and productivity losses (GlobalSurg Collaborative, 2018; Meara et al., 2015). Surgical site infection (SSI) is the most common healthcare-associated infection in LMICs, with one meta-analysis finding a pooled cumulative incidence of 5.6 per 100 surgical procedures, at least twice that found in studies examining SSI in the United States and European countries (Allegranzi et al., 2011). A recent global prospective cohort study after gastrointestinal surgery found a much higher incidence of SSI in LMICs (23.2% and 14.0%, respectively) than in high-income countries (HIC) (9.4%) (GlobalSurg Collaborative, 2018). Importantly, many SSIs can be prevented through enhanced clinical surveillance and infection prevention and control (IPC) measures over the perioperative period (Allegranzi et al., 2011; Biccard et al., 2018), including improved processing of surgical instruments.
Sterile processing (SP) is the set of IPC methods, including cleaning, packaging, disinfecting, sterilisation and quality assurance that permit the safe reuse of previously contaminated surgical instruments (World Health Organization [WHO] and Pan American Health Organization [PAHO], 2016). Consistent and effective SP ensures sterility of surgical instruments that come into contact with sterile tissues and the vascular system (WHO and PAHO, 2016). Previous literature has examined challenges associated with access to safe surgery in LMICs, including resource constraints and limitations in surveillance (Allegranzi et al., 2011). Much of the evidence currently available on SP, however, concerns circumstances and practices in HICs (Nyberger et al., 2019; Panta et al., 2019a). While IPC initiatives in LMICs have shown effectiveness in reducing the incidence of SSI (Allegranzi et al., 2018) and in promoting practice changes (Jones et al., 2015), these programmes have not included SP and comparatively little is published about the role of SP in safe surgery and IPC initiatives. The potential negative outcomes of SSI justify the increasing recognition of surgical safety and SP practice as pivotal public and global health issues. This review appraises and synthesises available evidence and identifies challenges of and opportunities for advancing SP in LMICs.
Methods
We completed an integrative review of the literature that has examined SP in LMICs. The integrative review method combines both experimental and non-experimental research on a topic to generate a more encompassing and in-depth understanding (Whittemore and Knafl, 2005). This understanding is achieved by way of a thorough process that reviews, critiques and synthesises the available literature on a focused topic (Callahan, 2010; Torraco, 2005). Integrative reviews have the potential to play a greater role in evidence-based practice (Whittemore and Knafl, 2005) because they contribute to theory development, assess future directions for research, guide policy transformations and advance practice (Callahan, 2010; Torraco, 2005).
Eligibility criteria, information sources and search
We followed the five-stage review process outlined by Whittemore and Knafl (2005) and aligned our review with the 2009 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement (Moher et al., 2009). To be included, papers had to discuss SP in countries classified by the World Bank (2020) into LMIC income groupings according to gross national income per capita. We included qualitative, quantitative and mixed-methods studies as well as other peer-reviewed literature such as analysis papers and reviews. Exclusion criteria included studies examining endoscopy, non-English-language literature, commentaries, editorials and theses. We searched MEDLINE and CINAHL Plus via EBSCOhost (Table 1) as well as PubMed in February 2020 for English-language literature published between February 2010 and February 2020. Ethical approval was not required for this work.
Table 1.
Search strategy for MEDLINE and CINAHL Plus (via EBSCOhost).
| Search | Search string | Records found |
|---|---|---|
| 1 | (MH ‘Surgical Instruments’ OR MH ‘Surgical Equipment’) OR (surgery OR surgical) | 4,231,285 |
| 2 | (MH ‘Sterilization’ OR MH ‘Equipment Contamination’ OR MH ‘Disinfection’ OR MH ‘Decontamination’) OR (‘sterile processing’ OR ‘sterile reprocessing’ OR ‘sterile supply’ OR ‘sterile services’) OR ((sterile OR surgery OR surgical OR instrument OR equipment) N2 (sterilization OR processing OR reprocessing OR cleaning OR disinfection OR decontamination)) | 118,495 |
| 3 | (MH ‘Developing Countries’ OR MH ‘Africa’ OR MH ‘Asia’) OR ((developing OR resource-constrained OR resource-poor OR low income OR low and middle income) N1 (country OR countries OR setting OR settings)) | 226,664 |
| 4 | #1 AND #2 AND #3 | 616 |
| 5 | #4 NOT MH ‘Sterilization, Reproductive’ | 383 |
| 6 | Limit #5 to publications within past 10 years | 96 |
Results
Study selection and characteristics
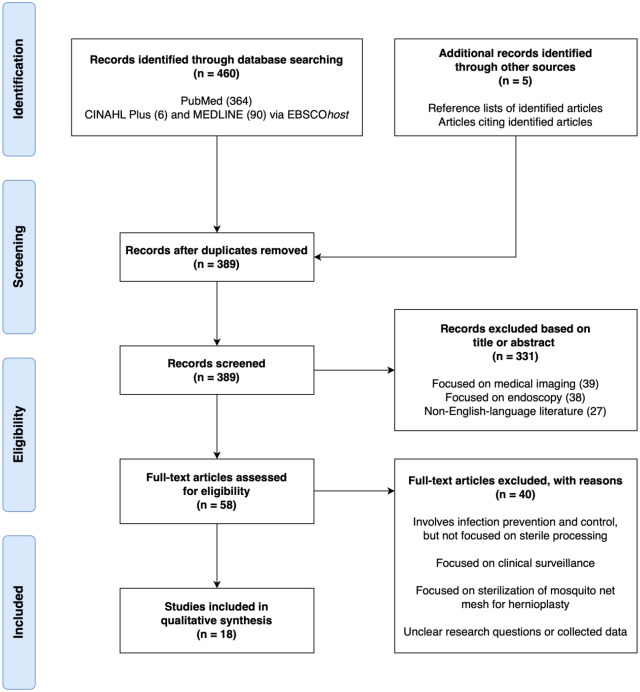
Our study selection process is shown in the PRISMA Statement flow diagram (Figure 1). We identified and screened 389 unique records through database searches, perusal of article reference lists and searching of records that cited articles already identified. A number of papers focused on endoscopy or medical image processing and were therefore outside the scope of this review and not relevant to our objective. After excluding items on the basis of titles or abstracts, we assessed 58 full-text papers examining safe surgery, IPC initiatives and SP practice. We excluded papers that did not focus on LMICs nor include a specific examination of SP.
Figure 1.
PRISMA 2009 (Moher et al., 2009) flow diagram.
Eighteen papers published between 2013 and 2019 met the inclusion criteria and were included in the qualitative synthesis of this integrative review. These papers consisted of 13 empirical studies, as well as five articles that were field experiments, analyses or reviews, and were conducted in or focused on circumstances in LMICs including Pakistan, Sierra Leone, Brazil, India, the Republic of the Congo, Madagascar, Benin, Ethiopia, Tanzania, Nepal and the Republic of Kiribati. Among the 13 studies, three used a quantitative non-randomised design, six used a quantitative descriptive design and four used a mixed-methods design. A summary of study types, locations, designs and key findings is shown in Supplementary Table 1. Study data were analysed through a process of coding, summarising and comparing to identify emergent themes and to categorise data as challenges of SP practice or opportunities to improve SP practice. Within the two categories of challenges and opportunities, papers were further non-exclusively categorised into subthemes.
Quality appraisal and risk of bias across studies
We appraised the methodological quality of included empirical studies with the Mixed Methods Appraisal Tool (MMAT) version 2018 (Hong et al., 2018). We identified concerns related to unknown and unaccounted-for confounders, non-representative samples, non-response bias and incomplete outcome data (Table 2).
Table 2.
Appraisal of included studies (n = 13*) using the Mixed Methods Appraisal Tool (MMAT; Hong et al., 2018).
| Category of study design | Methodological quality criteria | Responses |
||
|---|---|---|---|---|
| Yes | No | Can’t tell | ||
| Screening questions (for all types) (n = 13) | S1. Are there clear research questions? | 13 | 0 | 0 |
| S2. Do the collected data allow to address the research questions? | 13 | 0 | 0 | |
| 1. Qualitative (n = 0) | 1.1. Is the qualitative approach appropriate to answer the research question? | 0 | 0 | 0 |
| 1.2. Are the qualitative data collection methods adequate to address the research question? | 0 | 0 | 0 | |
| 1.3. Are the findings adequately derived from the data? | 0 | 0 | 0 | |
| 1.4. Is the interpretation of results sufficiently substantiated by data? | 0 | 0 | 0 | |
| 1.5. Is there coherence between qualitative data sources, collection, analysis and interpretation? | 0 | 0 | 0 | |
| 2. Quantitative randomised controlled trials (n = 0) | 2.1. Is randomisation appropriately performed? | 0 | 0 | 0 |
| 2.2. The groups are comparable at baseline | 0 | 0 | 0 | |
| 2.2. Are the groups comparable at baseline? | 0 | 0 | 0 | |
| 2.4. Are outcome assessors blinded to the intervention provided? | 0 | 0 | 0 | |
| 2.5 Did the participants adhere to the assigned intervention? | 0 | 0 | 0 | |
| 3. Quantitative non-randomised (n = 3) | 3.1. Are the participants representative of the target population? | 3 | 0 | 0 |
| 3.2. Are measurements appropriate regarding both the outcome and intervention (or exposure)? | 3 | 0 | 0 | |
| 3.3. Are there complete outcome data? | 2 | 1 | 0 | |
| 3.4. Are the confounders accounted for in the design and analysis? | 2 | 1 | 0 | |
| 3.5. During the study period, is the intervention administered (or exposure occurred) as intended? | 3 | 0 | 0 | |
| 4. Quantitative descriptive (n = 6) | 4.1. Is the sampling strategy relevant to address the research question? | 6 | 0 | 0 |
| 4.2. Is the sample representative of the target population? | 5 | 1 | 0 | |
| 4.3. Are the measurements appropriate? | 6 | 0 | 0 | |
| 4.4. Is the risk of non-response bias low? | 5 | 1 | 0 | |
| 4.5. Is the statistical analysis appropriate to answer the research question? | 6 | 0 | 0 | |
| 5. Mixed methods (n = 4) | 5.1. Is there an adequate rationale for using a mixed methods design to address the research question? | 4 | 0 | 0 |
| 5.2. Are the different components of the study effectively integrated to answer the research question? | 4 | 0 | 0 | |
| 5.3. Are the outputs of the integration of qualitative and quantitative components adequately interpreted? | 4 | 0 | 0 | |
| 5.4. Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? | 4 | 0 | 0 | |
| 5.5. Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? | 4 | 0 | 0 | |
The MMAT is not intended to appraise non-empirical studies. The five field experiments, analyses and reviews included in this review were not appraised with the MMAT.
Challenges to sterile processing practice
Limited available research
There is little available evidence on SP in LMICs. Much of the research has taken place recently, with the majority of papers (n = 12, 67%) published in or after 2017. Moreover, several papers were pilot or preliminary studies. Numerous authors contended that presurgical care, which includes SP, has been overlooked in IPC research (O’Hara et al., 2015) and that SP in LMICs has been understudied compared to HICs (Fast et al., 2017; Forrester et al., 2018c; Panta et al., 2019a).
Resource constraints
All papers discussed circumstances or implications of resource constraints in LMICs. Although IPC principles are universally applicable (Oosthuysen et al., 2014), limitations in infrastructure, equipment, finances and human resources are widely recognised as hindering IPC and SP practice in LMICs (Ayub Khan et al., 2018; Boubour et al., 2016; Fast et al., 2017; Forrester et al., 2018c).
Several authors discussed how constraints of supplies and equipment vital to SP practice, including warm water, instrument brushes, detergent or soap, sterilisation indicators and personal protective equipment, make it difficult to carry out adequate SP (Fast et al., 2017; O’Hara et al., 2015). These researchers frequently observed inaccessible, dysfunctional and unmaintained autoclaves in LMIC healthcare facilities. As such, manual instrument cleaning is common in LMICs amid resource constraints but remains much less effective than automated cleaning (Costa et al., 2018; Oosthuysen et al., 2014). Inadequate cleaning has been associated with bioburden and debris retention (Fast et al., 2017) as well as biofilm formation, particularly in complex-design instruments that are impractical to clean manually (Costa et al., 2018). Ultimately, instruments that remain contaminated cannot be sterilised effectively.
Resource limitations strain the IPC and SP workforce in LMICs. Healthcare workers (HCWs) may take on multiple and occasionally discordant roles, such as working in laundry or morgue areas in addition to SP, and furthermore, few have post-basic or formal education in IPC (Fast et al., 2017; Zimmerman et al., 2013). Where and when training is available, it may be inadequate (Forrester et al., 2018c). Few facilities have dedicated areas for SP and resource materials, such as procedural manuals and flow charts, are often unavailable (Panta et al., 2019b). Moreover, challenges related to funding, administrative and infrastructure have been perceived by HCWs as barriers to workforce and professional development opportunities and, in turn, may preclude evidence-based practice and patient safety culture (Ayub Khan et al., 2018).
The surgical capabilities of LMIC health facilities are impeded by deficiencies in the condition and ongoing maintenance of resources on hand, particularly that of valuable surgical instruments and equipment (Forrester et al., 2018c). O’Hara et al. (2015) found that in nine hospitals across seven LMICs, all nine of the single most-used autoclaves examined had been used for over 16 years, none had been regularly maintained and three had never been quality assured. In Nepalese hospitals, Panta et al. (2019b) associated inadequate maintenance of pressure and outmoded autoclaves with a high rate of failed steam sterilisation, while Munakomi et al. (2018) observed striking wear and tear, including joint changes, stains, loosening, rust and fractures, in surgical instruments used for less than one year. Without suitable processing equipment and procedures, instrument functionality and integrity decline and the risk of poor outcomes is increased (Fast et al., 2017; Munakomi et al., 2018).
Disconnects between evidence, guidelines and practice
Fourteen papers discussed SP and IPC practice shortcomings with respect to established guidelines and policy. Authors generally agreed that SP policy is not well defined in LMICs (Forrester et al., 2018c; Panta et al., 2019a). LMIC healthcare facilities have been found to not meet WHO standards for SP (Fast et al., 2017) and to lack IPC government standards and accreditation (Weinshel et al., 2015). Poor IPC practices, such as inconsistent sterilisation of instruments between patient use and reuse of single-use instruments, have been attributed to knowledge gaps and poor guideline adherence (Oosthuysen et al., 2014).
Several authors highlighted consequential policy-practice gaps. Costa et al. (2018) noted that policy standards in Brazil required only cleaning, and not necessarily disinfection and sterilisation, before returning loaned instrument sets. During SP training and mentoring programmes in Ethiopian and Tanzanian hospitals, Fast et al. (2019a, 2019b) found that workers were apprehensive about using enzymatic detergents or soapy water in place of corrosive 0.5% chlorine solutions, a recommendation in alignment with recent changes to WHO (WHO and PAHO, 2016) evidence-based guidelines. In Ethiopia, this stemmed from differences between national guidelines and WHO global guidelines, while in Tanzania, implementing this practice change could have impacted accreditation from government inspectors, not all of whom had received and adopted recently updated guidelines. To address this gap, an SP educator worked with the Ethiopian government to revise national guidelines to caution against the use of chlorine solutions and clarified the guidelines with hospitals involved in the Safe Surgery 2020 initiative (Fast et al., 2019b).
Several papers further discussed how institutions and governments have taken action to address policy-practice gaps. O’Hara et al. (2015) reported that hospital sites valued participating in a pilot study and one hospital initiated a review of autoclave maintenance and testing policy as a result. A comprehensive IPC programme was implemented at a national scale in the Republic of Kiribati after shortcomings were identified following the severe acute respiratory syndrome epidemic in 2002–2003 (Zimmerman et al., 2013). Moreover, a number of authors underscored that policy aimed at improving practice should recognise and address local realities because some IPC guidelines are not contextually appropriate nor feasible in resource-constrained settings (Forrester et al., 2018a, 2018c). For instance, the relative lack of improvement seen in the use of detergents, disinfectants and sterilisation indicators after an SP training programme in Ethiopian hospitals was attributed to persisting resource constraints (Fast et al., 2019b). Accordingly, Forrester et al. (2018c) contended that long-term and sustained improvements depend on meaningful investments in infrastructure and staffing.
Opportunities to strengthen sterile processing practice
Education, training and mentoring
Nine papers discussed education, training and mentoring in relation to SP workers’ practice in LMICs. Shortcomings in education were identified as barriers to effective IPC and SP practice (Ayub Khan et al., 2018; Fast et al., 2017; Forrester et al., 2018c) but importantly also serve as opportunities to implement strategies to improve SP through education, training, and mentoring (Fast et al., 2018, 2019b, 2019a; Forrester et al., 2018a). Several authors presented the development and outcomes of SP educational initiatives. After SP education courses at 25 hospitals in Benin, Ethiopia and Tanzania, statistically significant improvements were observed in participants’ SP knowledge test scores, and clinically significant and sustained improvements in SP practice were seen in post-training hospital assessments (Fast et al., 2018, 2019a, 2019b). These clinical improvements included decreased exposure of instruments to corrosive 0.5% chlorine solutions and workflow reorganisation with the use of a three-step cleaning system (Fast et al., 2018), pre-use instrument inspections and post-use soaking in soap and water (Fast et al., 2019b), and increased cleaning of gross organic material before sterilisation and increased use of chemical sterile indicators to monitor sterilisation (Fast et al., 2019a). At a hospital in Ethiopia, Forrester et al. (2018a) worked with hospital leadership and staff to develop workflow process maps relevant to operating room procedures to improve adherence to critical steps of the WHO Surgical Safety Checklist (SSC). After implementation, statistically and clinically significant improvements in the use of chemical sterile indicators in instrument trays were observed.
Capacities relating to SP and IPC were illustrated by researchers as multidimensional, spanning social and economic capital, human resources, knowledge, skills and infrastructure (Fast et al., 2017; Forrester et al., 2018c; Zimmerman et al., 2013). In their evaluation of the impact of a comprehensive IPC programme on workers’ practice at a hospital in the Republic of Kiribati, Zimmerman et al. (2013) found statistically significant associations between workers’ self-reported knowledge, application ability and levels of confidence, suggesting that the education and training components of the programme positively impacted clinical practice.
Building partnerships to advance practices, guidelines and policy
Six papers highlighted the value of collaborative partnerships and networks to strengthen SP practice. A few authors discussed initiatives that have been developed to improve surgical care in LMICs, including the Safe Surgery 2020 initiative (Fast et al., 2019b), Global Surgery 2030 plan (Fast et al., 2018), WHO SSC and Clean Cut programme (Forrester et al., 2018a). These researchers have collaborated with organisations, including Assist International, the Lifebox Foundation and the GE Foundation, that provide operational and financial support for global health initiatives.
Several authors presented the work of organisations that provide frontline education and capacity-building initiatives at healthcare facilities in LMICs. In the Republic of Congo, Madagascar, Benin, Ethiopia and Tanzania, collaboration between Sterile Processing Education Charitable Trust (SPECT), Mercy Ships and local researchers enabled the delivery of SP training and mentoring programmes (Fast et al., 2017, 2018, 2019a, 2019b). In Ethiopia, a network of researchers and scientists from Jimma University, Stanford University and the Lifebox Foundation collaborated to develop surgical safety and workflow quality improvement programmes (Forrester et al., 2018a) and SSI surveillance (Forrester et al., 2018b) in hospitals.
Notably, most (n = 16, 89%) included papers were authored or co-authored by researchers and professionals based in LMICs. A number of authors underscored the importance that research and practice initiatives fully partner and build capacity with local researchers, professionals and leaders. This approach is recognised as vital to ensure programme feasibility and relevance as well as research capacity building (Fast et al., 2019a, 2019b; Forrester et al., 2018a, 2018c).
Innovative approaches in resource-constrained settings
Five papers discussed the potential for innovative approaches that address resource constraints to build surgical capacity. These strategies include locally produced enzymatic detergents, onsite generation of distilled water, and affordable or reusable sterile indicators (Forrester et al., 2018c). Sterilisation indicators include internal and external chemical indicators, which undergo visible changes when exposed to established parameters such as specific temperature thresholds, and biological indicators, which contain resistant spores, of which a specific proportion should be killed to verify effective sterilisation. These indicators are vital to sterility assurance; however, indicator testing is inconsistent in LMICs and biological indicators are particularly scarce (Panta et al., 2019b). Accordingly, strategies that address these particular resource constraints are likely to provide a high return.
Two authors presented unique approaches to infrastructure and practice. Boubour et al. (2016) reported on a pilot study of a self-contained SP unit repurposed from a shipping container that simulated contamination, and after steam sterilisation, verification of effective sterilisation with chemical and biological sterile indicators across 61 trials. Devadiga et al. (2015) conducted a secondary analysis of local data to analyse resource constraints affecting SP at a facility in India and found that the facility change to packaging sterilised instruments in non-woven fabrics reduced the proportion of re-sterilisation. Although initial purchase costs for non-woven fabrics were more expensive, the sizable surgery caseload and reduced need to re-sterilise instruments proved the change was cost-effective.
Several authors discussed unique educational approaches aimed at sustaining practice changes. Fast et al. (2019b) discussed incorporating a training of trainers component into an SP training course at 12 Ethiopian hospitals that enabled these trainers to educate an additional 254 workers. Forrester et al. (2018a) adapted process mapping, a visual diagramming technique, to surgical workflows at an Ethiopian teaching hospital and observed improvements in adherence to IPC including the use of chemical sterile indicators as well as the WHO SSC, intended to facilitate overall quality improvement and to guide teams toward feasible short-, medium- and long-term achievements (Forrester et al., 2018a).
Quality assurance and surveillance programmes
Four papers discussed the role of quality assurance and epidemiologic surveillance programmes in improving evaluation of practice. Several authors underscored the importance of the use of chemical and biological sterilisation indicators (Forrester et al., 2018c; Panta et al., 2019b) and verification of autoclave parameters (O’Hara et al., 2015) as crucial steps to evaluate the effectiveness of instrument sterilisation. These authors contend that SP programmes in LMICs would benefit from more consistent sterile indicator use. Class 5 chemical indicators are less expensive than biological indicators, yield more immediate results, and provide a good combination of reliability and affordability as long as they achieve high sensitivity and specificity. Resource constraints continue to limit the use of biological indicators in LMICs; however, strategies to improve the supply and use of biological indicators, at least weekly as the gold standard for sterility assurance, would be especially high-yield interventions (Panta et al., 2019b).
At an Ethiopian hospital, Forrester et al. (2018b) demonstrated value in a quality improvement programme that combined SSI prevention (i.e. the Clean Cut programme) and both inpatient and outpatient surveillance. The Clean Cut programme aims to reduce SSI and has six process standards including appropriate skin preparation, sterile field maintenance, effective and verified SP, antibiotic prophylaxis, standardised swab counts and use of the WHO SSC. Forrester et al. (2018b) found that additional direct inpatient follow-up, versus chart review alone, detected more postoperative complications, including SSI, re-intervention and mortality. Furthermore, surveillance programmes may aid the identification of infectious agents and susceptibility patterns (Zimmerman et al., 2013).
Discussion
This review underscored a number of important findings on the role of SP in safe surgery and the state of SP in LMICs. Although research on SP in LMICs remains limited compared to HICs, more evidence has emerged in the past three years as the importance of SP to safe surgery is being increasingly recognised. Further practice and research initiatives are needed to amass more robust data that accurately reflect LMIC circumstances, address uncertainties and clarify the effectiveness of interventions (Conradie et al., 2018; Meara et al., 2015). As a result, key opportunities exist to improve equity in research capacity building and in the mutuality of partnerships that uplift lived and local experience and knowledge. The African Surgical Outcomes Study (ASOS) is a research initiative that generates local data to inform research and practice (Conradie et al., 2018). ASOS has facilitated African researchers’ increased participation in global health research and provided crucial data on surgical outcomes.
All included studies underscored that resource constraints remain a central and persisting barrier to effective SP in LMICs. In some countries, sterile services departments, which centralise and standardise SP methods, do not exist (WHO and PAHO, 2016). Without the necessary processing equipment, trained personnel and organised processes, effective sterilisation cannot be achieved. Longer-term objectives will require further research evidence, broader investments and decisive governmental involvement. In the short term, however, the findings of numerous included studies suggest that simple refits to address specific, high-yield areas, including workflows as well as instrument cleaning, may yield the most impactful headway in SP practice. In addition, quality improvement and surgical surveillance initiatives show promise to identify the root causes of issues and to develop innovative and feasible interventions. Finally, the involvement and harnessing of a wide array of expertise in many studies, including engineering, business and public policy, truly speaks to the interdisciplinary nature of global health.
There are a number of opportunities to harmonise institutional policies, clinical guidelines, best available evidence and SP practice in LMICs. Several studies showed that training and education programmes improved SP and surgical workers’ knowledge, awareness, teamwork and SP practices in the short term, yielding clinically significant effects. These findings are consistent with the results of a Cochrane overview of systematic reviews in which implementation strategies targeted at HCWs in LMICs found to have moderate- or high-certainty evidence of effectiveness when compared to no intervention included educational meetings, practice facilitation, audit and feedback interventions, and educational outreach and tailored interventions (Pantoja et al., 2017).
To improve surgical and anaesthesia care, a variety of partnerships need to be built between governments, intergovernmental and non-governmental organisations, researchers, surgical teams, community stakeholders and non-profit organisations. National Surgical, Obstetrics and Anaesthesia Plans (NSOAPs), designed to unite these entities, have gained momentum recently and driven progress in safe surgery, obstetrics and anaesthesia across sub-Saharan Africa. The first Tanzanian NSOAP launched in March 2018 and outlined priorities over a period of seven years across six comprehensive domains, including service delivery, infrastructure, workforce, information management and technology, finance and governance (Ministry of Health, Community Development, Gender, Elderly and Children, 2018). Much of the policy direction was shaped by the work of community stakeholders, researchers and surgical teams, which represented a significant harmonisation of previously fragmented initiatives. With that said, the greatest ongoing and unresolved challenges facing the sustainability of NSOAP are public and private funding as well as definitive government support (Sonderman et al., 2019).
Studies included in this review underscored concepts of capacity building and community development. Researchers reported that SP and IPC educational initiatives built foundational and transferable knowledge, skills and confidence, and inspired workers to make a difference through their practice. In addition, approaches including mentoring and the training of trainers represent more sustainable approaches to capacity building. Significant barriers, however, remain for patients and communities in LMICs to hold systems accountable for patient safety, surgical outcomes and financing flows, including sociodemographic hierarchies and limitations in health literacy (Meara et al., 2015; WHO, 2017). Notably, the Community Health and Information Network (CHAIN) in Uganda is a ground-breaking civil society organisation that was established in 2004. CHAIN aims to improve healthcare safety and quality by supporting patients and communities to become more informed participants in healthcare through capacity-building programmes including community events, text messaging, media campaigns and forums between community members and health professionals (WHO, 2017).
Global health inequities
One of the most salient findings in this review may be the striking disparities in surgical capacity in LMICs compared to HICs. Several authors discussed the moral imperative to address global health disparities as underlying their research as well as the need for continued advocacy in practice and research capacity building to achieve safe surgery for all.
The health inequalities stemming from disparities in surgical capacity are fundamentally rooted in social inequities and injustices. Global poverty and health disparities between poor and rich countries have roots in colonialism, neocolonialism and uneven processes of globalisation (Labonté, 2018; Rushton and Williams, 2012). It is vital that research and safe surgery initiatives negotiate both the legacies of colonialism as well as the inequities of the neocolonial present in the Global South and LMICs that impede access to healthcare and safe surgery. In both practice and research capacity building, global health partners are called upon to question power relations and counter the inequities that persist in global health (Beran et al., 2017).
Similarities and differences with the results of previous reviews
A systematic review conducted by Oosthuysen et al. (2014) of IPC in global oral healthcare facilities included a focus on SP practice and also found that resource constraints as well as gaps in knowledge and adherence to established guidelines continue to hinder IPC practice in LMICs. In a scoping review of SP in LMICs, Forrester et al. (2018c) similarly found discrepancies between SP practice and evidence-based guideline recommendations. Based on the findings of their strategies, they proposed that further staff education and more defined policies could reduce workforce and workspace challenges, and moreover underscored the importance of integrating local knowledge and capacity building to sustain initiatives. In a review of the effectiveness of steam sterilisation in global health facilities, Panta et al. (2019a) similarly found a high proportion of sterilisation failures in LMICs and an overall need for more research evidence, as no studies covered all categories of health facilities (e.g. hospitals, dental offices and other outpatient clinics).
In this integrative review, we have consolidated up-to-date research literature, including eight studies examining IPC and SP published since the scoping review by Forrester et al. (2018c). Based on recent evidence, we have presented opportunities that may be leveraged to improve SP in LMICs, including education and training initiatives that have demonstrated effectiveness as well as quality assurance and surveillance programmes that show promise. We have also summarised included papers (Supplementary Table 1) and appraised the available evidence using the MMAT (Table 2).
Quality appraisal and risk of bias across studies
The studies included in this review are susceptible to numerous biases (Boutron et al., 2019; Higgins et al., 2013). Selection bias may have resulted from non-probability sampling and small sample sizes that generated non-representative samples. In studies that conducted interviews and observations, bias related to data collection may have skewed what, how and when data were collected. Reporting or publication biases may have resulted from selective reporting, such as when unfavourable or supposedly non-significant results were not reported by participants in studies, or when uninteresting results were not disseminated by researchers. Finally, experimental mortality and loss to follow-up in several studies present concerns.
Limitations
There are several limitations to this review. The integrative review methodology has inherent weaknesses in rigour, primarily because it consolidates both experimental and non-experimental research, and if conducted without systematic methods, is susceptible to bias (Whittemore and Knafl, 2005). We chose the integrative review methodology because given the relative dearth of research on this topic, synthesising studies of several designs yields the most comprehensive and up-to-date evidence. We made efforts to enhance the rigour of this review by aligning our review with the PRISMA Statement and appraising studies with the MMAT. While we endeavoured to find as much literature as possible with our search, it is possible that we missed literature, particularly research published in the languages of LMICs because we included only English-language literature. Finally, this review was conducted with Global North lenses that simply cannot fully account for the circumstances and lived experiences of HCWs and communities in LMICs.
Implications for research
We have synthesised up-to-date evidence, including research that demonstrates the potential for education initiatives to improve SP practice and underscores the value of collaborative networks (e.g. NSOAPs) and sustainable capacity building. Further research and evidence, including randomised and controlled experimental studies, are needed to confirm the generalisability of study findings and effectiveness of strategies to improve SP practice in LMICs. Our review will help researchers and stakeholders identify opportunities to contribute.
Conclusions
The research evidence on SP in LMICs remains limited but has recently made headway. This integrative review provides insight into the challenges to and opportunities for advancing SP in LMICs and may inform planning and analysis of future studies. Further research and safe surgery initiatives are needed to amass more localised data, build SP capabilities through strategies including education and quality assurance improvements, and advance collaborative partnerships and networks. The global surgery and research communities’ advocacy and practice can work toward reducing global health inequities to achieve safe surgery for all.
Supplemental Material
Supplemental material, SupplementaryTable for Sterile processing in low- and middle-income countries: an integrative review by Alexander Cuncannon, Aliyah Dosani and Olive Fast in Journal of Infection Prevention
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article: OF is Chair of Sterile Processing Education Charitable Trust.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Partial funding for this research was provided by Assist International as part of the Safe Surgery 2020 initiative funded by the GE Foundation.
Peer review statement: Not commissioned; blind peer-reviewed.
ORCID iDs: Alexander Cuncannon  https://orcid.org/0000-0002-5946-1181
https://orcid.org/0000-0002-5946-1181
Aliyah Dosani  https://orcid.org/0000-0001-6817-3571
https://orcid.org/0000-0001-6817-3571
Availability of data and materials: All data generated or analysed during this study are included in this published article and its supplementary files.
Supplemental material: Supplemental material for this article is available online.
References
- Allegranzi B, Nejad SB, Combescure C, Graafmans W, Attar H, Donaldson L, Pittet D. (2011) Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 377(9761): 228–241. [DOI] [PubMed] [Google Scholar]
- Allegranzi B, Aiken AM, Zeynep Kubilay N, Nthumba P, Barasa J, Okumu G, Mugarura R, Elobu A, Jombwe J, Maimbo M, Musowoya J, Gayet-Ageron A, Berenholtz SM. (2018) A multimodal infection control and patient safety intervention to reduce surgical site infections in Africa: a multicentre, before–after, cohort study. Lancet Infectious Diseases 18(5): 507–515. [DOI] [PubMed] [Google Scholar]
- Ayub Khan MN, Verstegen DML, Bhatti ABH, Dolmans DHJM, van Mook WNA. (2018) Factors hindering the implementation of surgical site infection control guidelines in the operating rooms of low-income countries: a mixed-method study. European Journal of Clinical Microbiology & Infectious Diseases 37: 1923–1929. [DOI] [PubMed] [Google Scholar]
- Beran D, Byass P, Gbakima A, Kahn K, Sankoh O, Tollman S, Witham M, Davies J. (2017) Research capacity building—obligations for global health partners. Lancet Global Health 5(6): e567–e568. [DOI] [PubMed] [Google Scholar]
- Biccard BM, Madiba TE, Kluyts HL, Munlemvo DM, Madzimbamuto FD, Basenero A, Gordon CS, Youssouf C, Rakotoarison SR, Gobin V, Samateh AL, Sani CM, Omigbodun AO, Amanor-Boadu SD, Tumukunde JT, Esterhuizen TM, Le Manach Y, Forget P, Elkhogia AM, Mehyaoui RM, Zoumeno E, Ndayisaba G, Ndasi H, Ndonga AKN, Ngumi ZWW, Patel UP, Ashebir DZ, Antwi-Kusi AA, Mbwele B, Sama HD, Elfiky M, Fawzy MA, Pearse RM. and African Surgical Outcomes Study (ASOS) investigators. (2018) Perioperative patient outcomes in the African Surgical Outcomes Study: a 7-day prospective observational cohort study. Lancet 391: 1589–1598. [DOI] [PubMed] [Google Scholar]
- Boubour J, Jenson K, Richter H, Yarbrough J, Oden ZM, Schuler DA. (2016) A Shipping Container-Based Sterile Processing Unit for Low Resources Settings. PLoS One 11(3): e0149624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutron I, Page M, Higgins J, Altman D, Lundh A, Hróbjartsson A. (2019) Chapter 7: Considering bias and conflicts of interest among the included studies. In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, Welch V. (eds) Cochrane Handbook for Systematic Reviews of Interventions. Oxford: Cochrane Centre; Available at: https://training.cochrane.org/handbook/current/chapter-07 (accessed 13 March 2020). [Google Scholar]
- Callahan JL. (2010) Constructing a Manuscript: Distinguishing Integrative Literature Reviews and Conceptual and Theory Articles. Human Resource Development Review 9(3): 300–304. [Google Scholar]
- Conradie A, Duys R, Forget P, Biccard B. (2018) Barriers to clinical research in Africa: a quantitative and qualitative survey of clinical researchers in 27 African countries. British Journal of Anaesthesia 121(4): 813–821. [DOI] [PubMed] [Google Scholar]
- Costa DM, Lopes LKO, Vickery K, Watanabe E, Vasconcelos LSN, de OL, de Paula MC, Melo DS, Hu H, Deva AK, Tipple AFV. (2018) Reprocessing safety issues associated with complex-design orthopaedic loaned surgical instruments and implants. Injury 49(11): 2005–2012. [DOI] [PubMed] [Google Scholar]
- Devadiga G, Thomas V, Shetty S, Setia M. (2015) Is non-woven fabric a useful method of packaging instruments for operation theatres in resource constrained settings? Indian Journal of Medical Microbiology 33(2): 243–243. [DOI] [PubMed] [Google Scholar]
- Fast O, Fast C, Fast D, Veltjens S, Salami Z, White MC. (2017) Limited sterile processing capabilities for safe surgery in low-income and middle-income countries: experience in the Republic of Congo, Madagascar and Benin. BMJ Global Health 2: e000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fast O, Fast C, Fast D, Veltjens S, Salami Z, White M. (2018) Mixed methods evaluation of the impact of a short term training program on sterile processing knowledge, practice, and attitude in three hospitals in Benin. Antimicrobial Resistance & Infection Control 7: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fast O, Uzoka F-M, Cuncannon A, Fast C, Dosani A, Nyanza EC, Fast D, Maduka T. (2019. a) The impact of a sterile processing program in Northwest Tanzania: a mixed-methods study. Antimicrobial Resistance & Infection Control 8: 183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fast OM, Gebremedhin Teka H, Alemayehu/Gebreselassie M, Fast CMD, Fast D, Uzoka F-ME. (2019. b) The impact of a short-term training program on workers’ sterile processing knowledge and practices in 12 Ethiopian hospitals: a mixed methods study. PLoS One 14(5): e0215643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrester JA, Koritsanszky LA, Amenu D, Haynes AB, Berry WR, Alemu S, Jiru F, Weiser TG. (2018. a) Developing Process Maps as a Tool for a Surgical Infection Prevention Quality Improvement Initiative in Resource-Constrained Settings. Journal of the American College of Surgeons 226(6): 1103–1116.e3. [DOI] [PubMed] [Google Scholar]
- Forrester JA, Koritsanszky L, Parsons BD, Hailu M, Amenu D, Alemu S, Jiru F, Weiser TG. (2018. b) Development of a Surgical Infection Surveillance Program at a Tertiary Hospital in Ethiopia: Lessons Learned from Two Surveillance Strategies. Surgical Infections 19(1): 25–32. [DOI] [PubMed] [Google Scholar]
- Forrester JA, Powell BL, Forrester JD, Fast C, Weiser TG. (2018. c) Surgical Instrument Reprocessing in Resource-Constrained Countries: A Scoping Review of Existing Methods, Policies, and Barriers. Surgical Infections 19(6): 593–602. [DOI] [PubMed] [Google Scholar]
- GlobalSurg Collaborative. (2018) Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: a prospective, international, multicentre cohort study. Lancet Infectious Diseases 18(5): 516–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Ramsay C, Reeves BC, Deeks JJ, Shea B, Valentine JC, Tugwell P, Wells G. (2013) Issues relating to study design and risk of bias when including non-randomized studies in systematic reviews on the effects of interventions. Research Synthesis Methods 4(1): 12–25. [DOI] [PubMed] [Google Scholar]
- Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M-P, Griffiths F, Nicolau B, O’Cathain A, Rousseau M-C, Vedel I. (2018) Mixed Methods Appraisal Tool (MMAT) version 2018. Available at: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf (accessed 13 March 2020). [DOI] [PubMed]
- Jones M, Gower S, Whitfield A, Thomas S. (2015) Evaluation of practice change in Tanzanian health professionals 12 months after participation in an Infection Prevention and Management Course. Journal of Infection Prevention 16(5): 200–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labonté R. (2018) Reprising the globalization dimensions of international health. Globalization and Health 14(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, Ameh EA, Bickler SW, Conteh L, Dare AJ, Davies J, Merisier ED, El-Halabi S, Farmer PE, Gawande A, Gillies R, Greenberg SLM, Grimes CE, Gruen RL, Ismail EA, Kamara TB, Lavy C, Lundeg G, Mkandawire NC, Raykar NP, Riesel JN, Rodas E, Rose J, Roy N, Shrime MG, Sullivan R, Verguet S, Watters D, Weiser TG, Wilson IH, Yamey G, Yip W. (2015) Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386: 569–624. [DOI] [PubMed] [Google Scholar]
- Ministry of Health, Community Development, Gender, Elderly and Children. (2018) National surgical, obstetric and anaesthesia plan (NSOAP) 2018–2025. United Republic of Tanzania: Ministry of Health, Community Development, Gender, Elderly and Children; Available at: https://6cde3faa-9fe6-4a8d-a485-408738b17bc2.filesusr.com/ugd/d9a674_4daa353b73064f70ab6a53a96bb84ace.pdf (accessed 13 March 2020). [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339: b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munakomi S, Shah R, Shrestha S. (2018) A pilot study comparing pattern of damage sustained among instruments from different surgical units in a tertiary care centre in Nepal – reappraising the role of instrument reprocessing in retaining their value. F1000Research 7: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyberger K, Jumbam DT, Dahm J, Maongezi S, Makuwani A, Kapologwe NA, Nguhuni B, Mukhopadhay S, Iverson KR, Maina E, Kisakye S, Mwai P, Hellar A, Barash D, Reynolds C, Meara JG, Citron I. (2019) The Situation of Safe Surgery and Anaesthesia in Tanzania: A Systematic Review. World Journal of Surgery 43: 24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara NN, Patel KR, Caldwell A, Shone S, Bryce EA. (2015) Sterile reprocessing of surgical instruments in low- and middle-income countries: A multicenter pilot study. American Journal of Infection Control 43(11): 1197–1200. [DOI] [PubMed] [Google Scholar]
- Oosthuysen J, Potgieter E, Fossey A. (2014) Compliance with infection prevention and control in oral health-care facilities: a global perspective. International Dental Journal 64(6): 297–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panta G, Richardson AK, Shaw IC. (2019. a) Effectiveness of autoclaving in sterilizing reusable medical devices in healthcare facilities. Journal of Infection in Developing Countries 13(10): 858–864. [DOI] [PubMed] [Google Scholar]
- Panta G, Richardson AK, Shaw IC, Chambers S, Coope PA. (2019. b) Effectiveness of steam sterilization of reusable medical devices in primary and secondary care public hospitals in Nepal and factors associated with ineffective sterilization: A nation-wide cross-sectional study. PLoS One 14(11): e0225595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantoja T, Opiyo N, Lewin S, Paulsen E, Ciapponi A, Wiysonge CS, Herrera CA, Rada G, Peñaloza B, Dudley L, Gagnon M-P, Marti SG, Oxman AD. (2017) Implementation strategies for health systems in low-income countries: an overview of systematic reviews. Cochrane Database of Systematic Reviews 9: CD011086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rushton S, Williams OD. (2012) Frames, Paradigms and Power: Global Health Policy-Making under Neoliberalism. Global Society 26(2): 147–167. [Google Scholar]
- Sonderman KA, Citron I, Mukhopadhyay S, Albutt K, Taylor K, Jumbam D, Iverson KR, Nthele M, Bekele A, Rwamasirabo E, Maongezi S, Steer ML, Riviello R, Johnson W, Meara JG. (2019) Framework for developing a national surgical, obstetric and anaesthesia plan. BJS Open 3(5): 722–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torraco RJ. (2005) Writing Integrative Literature Reviews: Guidelines and Examples. Human Resource Development Review 4(3): 356–367. [Google Scholar]
- Weinshel K, Dramowski A, Hajdu Á, Jacob S, Khanal B, Zoltán M, Mougkou K, Phukan C, Inés Staneloni M, Singh N. (2015) Gap analysis of infection control practices in low- and middle-income countries. Infection Control & Hospital Epidemiology 36(10): 1208–1214. [DOI] [PubMed] [Google Scholar]
- Whittemore R, Knafl K. (2005) The integrative review: updated methodology. Journal of Advanced Nursing 52(5): 546–553. [DOI] [PubMed] [Google Scholar]
- World Bank. (2020) World Bank country and lending groups. Washington, DC: World Bank; Available at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed 13 March 2020). [Google Scholar]
- World Health Organization. (2017) Patient Safety: Making health care safer. Geneva: WHO; Available at: https://apps.who.int/iris/bitstream/handle/10665/255507/WHO-HIS-SDS-2017.11-eng.pdf (accessed 13 March 2020). [Google Scholar]
- World Health Organization and Pan American Health Organization (2016) Decontamination and reprocessing of medical devices for health-care facilities. Geneva: WHO; Available at: http://apps.who.int/iris/bitstream/handle/10665/250232/9789241549851-eng.pdf (accessed 13 March 2020). [Google Scholar]
- Zimmerman PA, Yeatman H, Jones M, Murdoch H. (2013) Evaluating infection control: a review of implementation of an infection prevention and control program in a low-income country setting. American Journal of Infection Control 41(4): 317–321. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, SupplementaryTable for Sterile processing in low- and middle-income countries: an integrative review by Alexander Cuncannon, Aliyah Dosani and Olive Fast in Journal of Infection Prevention