Abstract
Background
Despite an increasing need for multisectoral interventions and coordinations for addressing malnutrition, evidence-based multisectoral nutrition interventions have been rarely developed and implemented in low-income and middle-income countries. To identify key determinants of undernutrition for effectively designing a multisectoral intervention package, a nutrition survey was conducted, by comprehensively covering a variety of variables across sectors, in Niassa province, Mozambique.
Methods
A cross-sectional household survey was conducted in Niassa province, August–October 2019. Anthropometric measurements, anaemia tests of children under 5 years of age and structured interviews with their mothers were conducted. A total of 1498 children under 5 years of age participated in the survey. We employed 107 background variables related to possible underlying and immediate causes of undernutrition, to examine their associations with being malnourished. Both bivariate (χ2 test and Mann-Whitney’s U test) and multivariate analyses (logistic regression) were undertaken, to identify the determinants of being malnourished.
Results
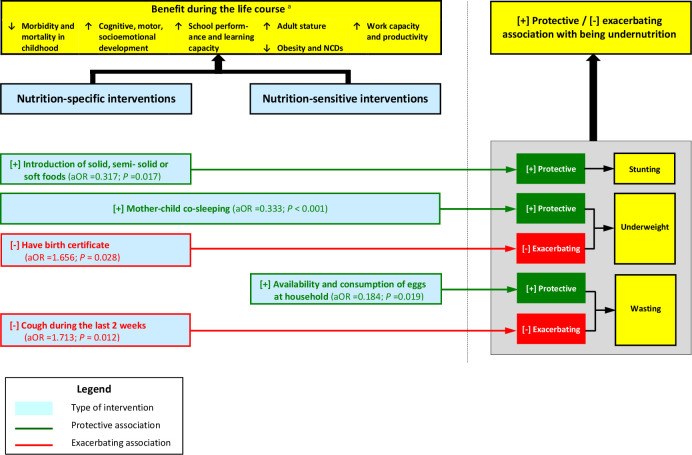
Prevalence rates of stunting, underweight and wasting were estimated at 46.2%, 20.0% and 7.1%, respectively. Timely introduction of solid, semi-solid or soft foods to children of 6–8 months of age was detected as a determinant of being not stunted. Mother–child cosleeping and ownership of birth certificate were a protective factor from and a promoting factor for being underweight, respectively. Similarly, availability and consumption of eggs at the household level and cough during the last 2 weeks among children were likely to be a protective factor from and a promoting factor for being wasted, respectively.
Conclusion
Timely introduction of solid, semi-solid or soft foods could serve as an entry point for the three sectors to start making joint efforts, as it requires the interventions from all health, agriculture and water sectors. To enable us to make meaningful interprovincial, international and inter-seasonal comparisons, it is crucially important to develop a standard set of variables related to being malnourished.
Keywords: nutrition assessment, dietary patterns, malnutrition
What this paper adds?
Despite a rapidly increasing need for multisectoral planning and implementations of nutrition-specific and nutrition-sensitive interventions, multisectoral nutrition surveys covering a spectrum of variables across sectors have been rarely conducted globally.
Timely introduction of solid, semi-solid or soft foods should be a key intervention for childhood stunting in Niassa province, Mozambique, calling for the joint interventions from health, agriculture and water sectors.
To ensure a better-designed package of evidence-based multisectoral interventions, it is recommended that a multi-stakeholder platform proactively work beyond respective sectoral interests in each country so that the initial step could be a joint multisectoral nutrition survey.
Introduction
Undernutrition accounts for 35% of total under-five mortalities globally.1 Thus, malnutrition has been drawing a great deal of attention as a key global development agenda from both developed and developing nations since the launch of the Millennium Development Goals (MDGs) in 2000.2 Under the Sustainable Development Goals, a greater emphasis continues to be placed on the critical need for addressing malnutrition as an unfinished agenda for the post MDG era.3 One of the major reasons that malnutrition remains the unfinished agenda was a significant lack of multisectoral and multistakeholder joint efforts when addressing malnutrition.4 It must be admitted that fragmented efforts previously made by respective sectors (eg, health and agriculture) ended up producing not only inadequate desirable outcomes but also sometimes even intersectoral confusions and conflicts.5 Malnutrition is not an independent issue that could be addressed and resolved by a single sector but a multifaceted complex issue that must be addressed and resolved by multiple sectors (eg, health, agriculture, environment, education, manufacturing and trading).6 7 To encourage and accelerate better integrated or coordinated efforts towards the reduction in prevalence of malnutrition in each country, Scale Up Nutrition (SUN) was launched as a global movement to end malnutrition in 2010. SUN advocates for the importance of and need for multisectoral planning and implementations of necessary interventions, by setting ‘multiple stakeholders come together’ as step 1.8
In Mozambique, where 43%, 15% and 6% of children under 5 years of age suffer from stunting, underweight and wasting, respectively,9 10 undernutrition has been one of the major public health concerns. The prevalence of stunting, in particular, remains extremely high around 42%–43% during the last 12 years, after its reduction from 60% in 1995 to 43% in 2008.11 Also, 2%–3% loss of gross national product in Mozambique is estimated to be attributed to chronic undernutrition.12 Having thoroughly understood the critical need for a multisectoral coordination in addressing high prevalence of malnutrition in the country, the Government of Mozambique (GoM) launched the Technical Secretariat for Food Security and Nutrition (SETSAN), a national multisectoral coordination mechanism for reducing undernutrition as a public health and social problem.13 Yet, despite a series of efforts made by the SETSAN and its participating partners since 2010, the country’s nutritional status has not significantly improved. One of the possible factors to which the inadequate progress in reduction in malnutrition is attributed should be a lack of detailed evidence-based multisectoral programming.
The determinants and underlying causes of malnutrition differ one country to another, and one province to another. Thus, designing a local setting-specific and context-sensitive multisectoral nutrition programme in an evidence-based manner is the key to ensuring more effective and efficient interventions.6 14 Nevertheless, there have been few earlier studies that systematically address the variables related to both nutrition-specific and nutrition-sensitive interventions15 and three underlying causes of undernutrition (household food insecurity, inadequate feeding and caring practices and unhealthy household environment)16 despite its importance and needs.17 18 While some earlier studies employed exclusively the variables related to feeding and caring practices, or water, sanitation and hygiene,19–23 others employed exclusively those related to household food security.24 25 Few employed the variables related to both types of interventions and three types of underlying causes of child undernutrition in a well-balanced manner. The contradiction between an emphasised need for multisectoral interventions and insufficiency of multisectoral nutrition studies is obvious.17 26
To design an evidence-based nutrition programme for Niassa province, the least developed province with the highest malnutrition prevalence in the country, the GoM and Japan International Cooperation Agency jointly conducted a multisectoral nutrition survey in the province. All the ministries responsible for addressing the three types of underlying causes of child undernutrition (ie, Ministry of Health, Ministry of Agriculture and Food Security and Ministry of Public Works, Housing and Water Resources) participated in the survey. No comprehensive multisectoral nutrition survey has been previously conducted in Mozambique. Therefore, the results of the survey will serve as the key foundation not only for designing an upcoming evidence-based multisectoral nutrition programme in Niassa province but also for developing the national technical standard and guidelines for multisectoral nutrition survey. This study is aimed at identifying key nutrition-specific and nutrition-sensitive determinants of child undernutrition, by employing a series of variables across three sectors (health, agriculture and water sanitation and hygiene) in Niassa province. Note that this is the first fully comprehensive multisectoral nutrition household survey in Mozambique.
Methods
Study objectives and study design
A cross-sectional household survey was conducted in two typical rural districts of Niassa province (Majune and Muembe), Mozambique, to estimate prevalence of undernutrition among children under 5 years of age and identify its key determinants in relation to nutrition-specific and nutrition-sensitive interventions across the three sectors (ie, health, agriculture and environment).
Study areas and study group
Majune district is located in the geographic centre of Niassa province and composed of 92 enumeration areas (EAs) for the Census 2017. Muembe district is bordered with Majune district in southeast and composed of 132 EAs. The total populations were estimated at 38 453 and 44 042 in Majune and Muembe, respectively, as of 2017.27 Ajawa is the major ethnic group in the both districts. The most commonly spoken languages in the districts are Ajawa and Macua. Agriculture accounts for the greatest proportion of local industries in the two districts. The both districts are positioned in the extremely rainy highland (annual precipitation 1171 mm and altitude 1500–1600 m). The targets of the study were children under 5 years of age living in Majune and Muembe districts.
Sample size and sampling methods
Demographic and Health Survey 2011 reported 46.8%, 18.2% and 3.7% as the prevalence of stunting, underweight and wasting among children under 5 years of age in Niassa province, respectively.11 Assuming no significant change in those prevalence rates since 2011, the sample sizes were calculated for prevalence of the three types of undernutrition with α (error)=0.05, 1-β (power)=0.80 and d (precision)=0.05, by applying the provincial prevalence as of 2011. This is a reasonable and realistic approach because the aforementioned prevalence rates were the only province-specific ones available and no significant changes were identified at least nationally during the last 12 years.11 As a result, 783 494 and 148 children under 5 years of age were calculated as the sample sizes required for estimating the prevalence of stunting, underweight and wasting, respectively, in the two districts. Then, of the three sample sizes calculated, the greatest one (=783 for stunting) was selected as the common sample size as it satisfied the sample sizes for underweight and wasting, too. Then, a design effect of 1.8 was multiplied, as two-stage sampling was employed for the survey (ie, 783×1.8=1409). Assuming non-response rate of 7.5%28 and cases of unknown child age of 2%–3%, 1556 was determined as the final sample size.
Of a total of 224 EAs (=92+132) in the two districts for the Census 2017, 94 EAs are randomly selected. Then, the number of households having children under 5 years of age to be selected in each of 94 EAs was calculated, by applying probability-proportional-to-size. The list of households for the Census 2017 was not readily available for the both districts.27 Thus, household listing was undertaken in all the 94 selected EAs, to develop the sampling frames from which target households having children under 5 years of age were selected. Then, in proportion to the population size of each selected EA, 7–38 households having children under 5 years of age were randomly selected from the household lists. Two repeated household visits were made, when children under 5 years of age, mothers and other caregivers were either absent or not available upon the initial visits. When a household was totally unavailable despite three visits, a substitute household was adopted by mechanically sampling the next eligible household in the household lists.
By targeting those randomly selected households, anthropometric measurements and anaemia tests of children under 5 years of age and structured interviews with their mothers or other caregivers were conducted during the period from 21 August 2019 to 4 October 2019, the postharvest season in Niassa province.
Anthropometric measurements
Weight measurements were undertaken for the children to the nearest 0.1 kg, using the electronic scale for children and adults (Seca 876, Hamburg, Germany). Their heights were measured to the nearest 0.1 cm, using the stadiometer for children and adults (Seca 213, Hamburg, Germany). Children younger than 2 years of age and unable to stand properly were measured lying down (recumbent length), using the length scale for infants (Seca 416, Hamburg, Germany).
Biochemical tests
Children of 6–59 months of age were tested for anaemia by the certified nurses, using the rapid blood analyzer HemoCue 301 (Quest Diagnostics, Norrköping, Sweden). Table salt available at households was sampled and tested for iodine, by using the field test kit (MBIK001, MBI Kits International, Tamil Nadu, India).
Household interviews and observations
A total of 107 background variables were employed as the potential determinants of undernutrition among children under 5 years of age. These background variables were selected from those representative of nutrition-specific interventions, nutrition-sensitive interventions and enabling environments, which were defined in the framework for actions to achieve optimum fetal and child nutrition and development.15 Those variables were selected so as to be in line with immediate causes and underlying causes of child undernutrition in the UNICEF’s conceptual framework of the determinants of child undernutrition, too.16Of the 107 variables, five were derived from immediate causes in the conceptual framework (ie, disease symptoms). Thirty-eight, 28 and 8 were derived from three underlying causes of undernutrition in the conceptual framework (ie, household food insecurity, inadequate feeding and caring practices and unhealthy household environment, respectively). And, the rest (28 variables) were sociodemographic and socioeconomic variables. Moreover, we attempted to ensure that a series of these variables were consistent with the independent variables employed in earlier studies.26 29–32
The questions on those background variables were included in the structured questionnaire. Of them, the data on type of and travelling time to drinking water source, type of toilet, presence of soap/ash for handwashing, food storage, utensil maintenance and house building materials were collected through enumerators’ direct observations and measurements. The data on other variables were collected through interviews with mothers and caregivers of children under 5 years of age. Of three locally spoken languages (ie, Ajawa, Macua and Portuguise), the most comfortable one for interviewees was selected as the language for an interview.
Data analysis
The data obtained through household interviews, observations, anthropometric measurements, anaemia tests and iodine tests were entered into a microcomputer. By using Anthro,33 z-scores for height-for-age, weight-for-age and weight-for-height were calculated based on the 2009 WHO standard reference population under 5 years of age.34 Those having been assumed to be under 5 years of age by parents but later found to be older by referring to the home-based records were excluded from the analysis. Wealth index was calculated for each household, by applying socioeconomic variables to principal component analysis, to categorise all the households into wealth index quintiles.35 Household Dietary Diversity Score (HDDS) was calculated by summing up the number of 12 food groups available at and consumed by each household during last 24 hours.36 The values for six standard indicators for Infant and Young Child Feeding (IYCF) were calculated, by using the IYCF indicator measurement guide.37
The statistical analyses were conducted, by using SPSS for Windows, V.22 (IBM/SPSS, Chicago, USA).
Bivariate and multivariate analyses were undertaken to identify the determinants of and risk factors for whether being malnourished (dependent variables). While the dependent variables are dichotomous, the independent variables are composed of interval ratio variables and categorical variables. Therefore, two types of bivariate analyses were employed. First, the associations between 94 categorical variables and whether being malnourished were examined, using χ2 test (Fisher’s exact test). Note that a total of 16 dummy variables were created for the mutually exclusive categorical variables having three or more categories (ie, primary income source, primary birth attendant). The category with the greatest frequency was designated as the reference for the dummy variables. Second, the associations between 13 interval ratio variables and whether being malnourished were examined, using a non-parametric method (Mann-Whitney’s U test), as it was expected and actually confirmed in Levene’s test that those variables were not normally distributed.
The background variables significantly associated with being malnourished (p<0.05 in χ2/Fisher’s exact test or Mann-Whitney’s U test) were selected as the possible independent variables for multivariate analyses. Prior to applying them to multivariate analyses, multicollinearity between those possible independent variables was systematically examined. To address possible multicollinearity between two interval ratio variables, those having a variance inflation factor (VIF) smaller than 10 were selected as the independent variables for multivariate analyses. To examine possible multicollinearity between two categorical variables, χ2 test (Fisher’s exact test) was conducted. When a statistical significance (p<0.05) was detected between them, one having a smaller p value with the dependent variable in χ2 test (Fisher’s exact test) was selected as an independent variable. Similarly, to examine possible multicollinearity between interval ratio and categorical variables, Mann-Whitney’s U test was conducted. When a statistical significance (p<0.05) was detected between them, one having a smaller p value with the dependent variables in Mann-Whitney’s U test was selected as an independent variable.
Ethical consideration
An informed consent to participate in the study was obtained in a written form from mothers or caregivers of children under 5 years of age. Children found to suffer from anaemia through blood tests were guided to the nearest health facilities for medical consultations and treatment. A small pack of iodised salt (approximately 5 g) was provided to households as a substitute for table salt sampled for iodine test.
Results
Undernutrition prevalence
Of 1556 sampled children, 58 were excluded from data analysis since their ages were either unknown and difficult to estimate, or found to be 5 years of age or older. Thus, the data collected from 1498 (=1556–58) children under 5 years of age, their mothers and other caregivers were analysed. Of the 1498 children under 5 years of age, boys (736; 49.1%) and girls (762; 50.9%) were almost equally represented. While children of 0–11 months of age (0 year old) account for the largest proportion (25.6%), those 48–59 months of age (4 years old) account for the smallest (11.6%). The prevalence rates of stunting, underweight and wasting were 46.2% (95% CI 43.6% to 48.8%), 20.0% (95% CI 18.0% to 22.1%) and 7.1% (95% CI 5.9% to 8.6%), respectively (table 1).10
Table 1.
Prevalence of undernutrition among children under 5 years of age in comparison with the previous survey
| Stunting: height-for-age | Underweight: weight-for-age | Wasting weight-for-height | |||||||
| n | % | 95% CI | n | % | 95% CI | n | % | 95% CI | |
| Majune and Muembe district as of 2019 | |||||||||
| (+) Severe (z-score <-3) | 424 | 28.3 | (26.0 to 30.7%) | 135 | 9 | (7.6 to 10.6%) | 56 | 3.6 | (3.7 to 4.8%) |
| (+) Moderate and severe (z-score <-2) | 692 | 46.2 | (43.6 to 48.8%) | 300 | 20 | (18.0 to 22.1%) | 107 | 7.1 | (5.9 to 8.6%) |
| (-) Non-malnourished (z-score ≥ −2) | 806 | 53.8 | (51.2 to 56.4%) | 1198 | 80 | (77.9 to 82.0%) | 1391 | 92.9 | (91.4 to 94.1%) |
| Niassa province as of 2011* | |||||||||
| (+) Severe (z-score <−3) | (n.a.) | 24 | (n.a.) | (n.a.) | 5.1 | (n.a.) | (n.a.) | 1.3 | (n.a.) |
| (+) Moderate and severe (z-score <−2) | (n.a.) | 46.8 | (n.a.) | (n.a.) | 18.2 | (n.a.) | (n.a.) | 3.7 | (n.a.) |
| (-) Non-malnourished (z-score ≥−2) | (n.a.) | 53.2 | (n.a.) | (n.a.) | 81.8 | (n.a.) | (n.a.) | 96.3 | (n.a.) |
| Mozambique as of 2011* | |||||||||
| (+) Severe (z-score <-3) | (n.a.) | 19.7 | (n.a.) | (n.a.) | 4.1 | (n.a.) | (n.a.) | 2.1 | (n.a.) |
| (+) Moderate and severe (z-score <-2) | (n.a.) | 42.6 | (n.a.) | (n.a.) | 14.9 | (n.a.) | (n.a.) | 5.9 | (n.a.) |
| (-) Non-malnourished (z-score ≥ −2) | (n.a.) | 57.4 | (n.a.) | (n.a.) | 85.1 | (n.a.) | (n.a.) | 94.1 | (n.a.) |
*Mozambique Demographic and Health Survey (National Institue of Health 2011).10
Bivariate analyses
Table 2 shows the results of bivariate analyses between child undernutrition and socioeconomic/demographic status.15 Tables 3–5 show the results of bivariate analyses15 37–39 between child undernutrition and variables related to the three types of underlying causes, that are (1) household food insecurity, (2) inappropriate parental feeding and caring practices and (3) unhealthy household environment. In addition, table 6 shows the results of bivariate analyses between child undernutrition and disease symptoms (including anaemia), as the immediate causes.16 They are also categorised into three types of key interventions: (1) nutrition-specific interventions, (2) nutrition-sensitive interventions and (3) enabling environment in tables 3–6.15 A total of 107 background variables examined on their bivariate relationships with child undernutrition, seven were significantly associated with whether being stunted (p<0.05). Similarly, 5 and 10 background variables were significantly associated with whether being underweight and whether being wasted (p<0.05), respectively. Of the seven variables significantly associated with whether being stunted, two were excluded from the independent variables for the logistic regression model for stunting due to their multicollinearity. For the same reason, 3 of 5 and 7 of 10 variables were excluded from the independent variables for the logistic regression models for underweight and for wasting, respectively.
Table 2.
Bivariate analyses between undernutrition and sociodemographic/economic variables
| Background variable | Type of intervention and conditions† | Stunting (N=1498) | Underweight(N=1498) | Wasting (N=1498) | ||||||||||||||
| Nutrition specific | Nutrition sensitive | Enabling | (+) Stunted | (−) Not stunted | P value‡ | (+) Under weight | (−) Not underweight | P value‡ | (+) Wasted | (−) Not wasted | P value ‡ | |||||||
| Environment | ||||||||||||||||||
| N | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |||||||
| Categorical variables | ||||||||||||||||||
| Sex | ||||||||||||||||||
| Female | – | – | – | 332 | 48 | 430 | 53.3 | Ref. | 147 | 49 | 615 | 51.3 | Ref. | 46 | 43 | 716 | 51.5 | Ref. |
| v1: male | – | – | X | 360 | 52 | 376 | 46.7 | 0.038* | 153 | 51 | 583 | 48.7 | 0.478 | 61 | 57 | 675 | 48.5 | 0.108 |
| Total | 692 | 100 | 806 | 100 | 300 | 100 | 1198 | 100 | 107 | 100 | 1391 | 100 | ||||||
| Primary income source | ||||||||||||||||||
| Agriculture or crop sales | – | – | – | 608 | 87.9 | 700 | 86.8 | Ref. | 263 | 87.7 | 1045 | 87.2 | Ref. | 88 | 82.2 | 1220 | 87.7 | Ref. |
| v2: livestock or animal sales | – | – | X | 2 | 0.3 | 2 | 0.2 | 1 | 1 | 0.3 | 3 | 0.3 | 1 | 0 | 0 | 4 | 0.3 | 1 |
| v3: fishing | – | – | X | 3 | 0.4 | 3 | 0.4 | 1 | 1 | 0.3 | 5 | 0.4 | 1 | 1 | 0.9 | 5 | 0.4 | 0.359 |
| v4: unskilled wage labour | – | – | X | 10 | 1.4 | 19 | 2.4 | 0.259 | 3 | 1 | 26 | 2.2 | 0.244 | 3 | 2.8 | 26 | 1.9 | 0.457 |
| v5: skilled wage labour | – | – | X | 15 | 2.2 | 13 | 1.6 | 0.45 | 7 | 2.3 | 21 | 1.8 | 0.479 | 4 | 3.7 | 24 | 1.7 | 0.134 |
| v6: handicrafts, artisanal works | – | – | X | 2 | 0.3 | 3 | 0.4 | 1 | 2 | 0.7 | 3 | 0.3 | 0.263 | 0 | 0 | 5 | 0.4 | 1 |
| v7: charcoal production | – | – | X | 1 | 0.1 | 2 | 0.2 | 1 | 1 | 0.3 | 2 | 0.2 | 0.489 | 0 | 0 | 3 | 0.2 | 1 |
| v8: seller, trader or commercial business | – | – | X | 25 | 3.6 | 25 | 3.1 | 0.666 | 8 | 2.7 | 42 | 3.5 | 0.59 | 5 | 4.7 | 45 | 3.2 | 0.398 |
| v9: salary wage | – | – | X | 23 | 3.3 | 36 | 4.5 | 0.288 | 13 | 4.3 | 46 | 3.8 | 0.74 | 5 | 4.7 | 54 | 3.9 | 0.607 |
| v10: begging and assistance | – | – | X | 0 | 0 | 1 | 0.1 | 1 | 0 | 0 | 1 | 0.1 | 1 | 0 | 0 | 1 | 0.1 | 1 |
| v11: pension and government subsidy | – | – | X | 3 | 0.4 | 2 | 0.2 | 0.667 | 1 | 0.3 | 4 | 0.3 | 1 | 1 | 0.9 | 4 | 0.3 | 0.31 |
| Total | 692 | 100 | 806 | 100 | 300 | 100 | 1198 | 100 | 107 | 100 | 1391 | 100 | ||||||
| Ownership of properties | ||||||||||||||||||
| v12: land for housing, farming or renting | – | – | X | 430 | 62.1 | 507 | 62.9 | 0.789 | 188 | 62.7 | 749 | 62.5 | 1 | 73 | 68.2 | 864 | 62.1 | 0.216 |
| v13: electricity | – | – | X | 109 | 15.8 | 139 | 17.2 | 0.444 | 44 | 14.7 | 204 | 17 | 0.341 | 19 | 17.8 | 229 | 16.5 | 0.687 |
| v14: radio | – | – | X | 280 | 40.5 | 322 | 40 | 0.874 | 115 | 38.3 | 487 | 40.7 | 0.47 | 40 | 37.4 | 562 | 40.4 | 0.609 |
| v15: television set | – | – | X | 66 | 9.5 | 94 | 11.7 | 0.208 | 32 | 10.7 | 128 | 10.7 | 1 | 15 | 14 | 145 | 10.4 | 0.255 |
| v16: mobile phone | – | – | X | 290 | 41.9 | 368 | 45.7 | 0.159 | 118 | 39.3 | 540 | 45.1 | 0.079 | 45 | 42.1 | 613 | 44.1 | 0.761 |
| v17: refrigerator | – | X | X | 7 | 1 | 19 | 2.4 | 0.049‡ | 3 | 1 | 23 | 1.9 | 0.334 | 6 | 5.6 | 20 | 1.4 | 0.008** |
| v18: generator | – | – | X | 4 | 0.6 | 12 | 1.5 | 0.129 | 1 | 0.3 | 15 | 1.3 | 0.22 | 2 | 1.9 | 14 | 1 | 0.319 |
| v19: air conditioner | – | – | X | 4 | 0.6 | 3 | 0.4 | 0.71 | 1 | 0.3 | 6 | 0.5 | 1 | 1 | 0.9 | 6 | 0.4 | 0.405 |
| v20: house ownership | – | – | X | 604 | 87.3 | 687 | 85.2 | 0.261 | 258 | 86 | 1033 | 86.2 | 0.926 | 93 | 86.9 | 1198 | 86.1 | 1 |
| v21: personal computer | – | – | X | 4 | 0.6 | 8 | 1 | 0.403 | 2 | 0.7 | 10 | 0.8 | 1 | 0 | 0 | 12 | 0.9 | 1 |
| v22: bicycle | – | – | X | 318 | 46 | 350 | 43.4 | 0.348 | 139 | 46.3 | 529 | 44.2 | 0.516 | 40 | 37.4 | 628 | 45.1 | 0.13 |
| v23: motorbike | – | – | X | 119 | 17.2 | 149 | 18.5 | 0.543 | 50 | 16.7 | 218 | 18.2 | 0.557 | 19 | 17.8 | 249 | 17.9 | 1 |
| v24: vehicle (car, truck and tractor) | – | – | X | 10 | 1.4 | 11 | 1.4 | 1 | 2 | 0.7 | 19 | 1.6 | 0.284 | 0 | 0 | 21 | 1.5 | 0.394 |
| Mean | SD | Mean | SD | P value§ | Mean | SD | Mean | SD | P value§ | Mean | SD | Mean | SD | P value§ | ||||
| Interval and ratio variables | ||||||||||||||||||
| v25: age (year) | – | – | X | 2.7 | 1.29 | 1.6 | 1.11 | <0.001** | 3 | 1.3 | 1.9 | 1.23 | <0.001** | 2 | 1.42 | 2.1 | 1.33 | 0.274 |
| v26: birth order in sibling (Nth child) | – | – | X | 3 | 2.23 | 3.1 | 2.11 | 0.207 | 2.8 | 2.1 | 3.1 | 2.18 | 0.093 | 3.2 | 2.17 | 3 | 2.16 | 0.195 |
| v27: total number of household members (person) | – | – | X | 5.7 | 2.74 | 5.7 | 2.35 | 0.556 | 5.7 | 2.41 | 5.7 | 2.57 | 0.67 | 6.1 | 2.46 | 5.7 | 2.54 | 0.064 |
| v28: wealth quintile (Nth quintile) | – | – | X | 3 | 1.38 | 3.1 | 1.43 | 0.182 | 3 | 1.38 | 3 | 1.41 | 0.724 | 3.2 | 1.47 | 3 | 1.4 | 0.207 |
*p<0.05, **p<0.01. Categorisation based on the previous review (Black et al. 2013).15
†Categorisation based on the previous review (Black et al. 2013).
‡χ2 test (Fisher’s exact test)
§Mann-Whitney U test.
Table 3.
Bivariate analyses between undernutrition and food security variables
| Background variable | Type of intervention and conditions† | Stunting (N=1498) | Underweight (N=1498) | Wasting (N=1498) | ||||||||||||||
| Nutrition specific | Nutrition sensitive | Enabling environment | (+) Stunted | (−) Not stunted | P value‡ | (+) Under weight | (−) Not underweight | P value‡ | (+) Wasted | (-) Not wasted | P value‡ | |||||||
| N | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |||||||
| Categorical variables | ||||||||||||||||||
| Food availability and consumption | ||||||||||||||||||
| v29: cereal | – | X | – | 685 | 99 | 779 | 99.1 | 0.794 | 298 | 99.3 | 1186 | 99 | 0.749 | 107 | 100 | 1377 | 99 | 0.617 |
| v30: white roots and tubers | – | X | – | 362 | 52.3 | 392 | 48.6 | 0.162 | 152 | 50.7 | 602 | 50.3 | 0.949 | 51 | 47.7 | 703 | 50.5 | 0.616 |
| v31: vegetables (vitamin A rich, leafy, and others) | – | X | – | 570 | 82.4 | 670 | 83.1 | 0.732 | 251 | 83.7 | 989 | 82.6 | 0.732 | 94 | 87.9 | 1146 | 82.4 | 0.183 |
| v32: fruits (vitamin A rich and others) | – | X | – | 84 | 12.1 | 71 | 8.8 | 0.041* | 35 | 11.7 | 120 | 10 | 0.398 | 8 | 7.5 | 147 | 10.6 | 0.409 |
| v33: meats (organ and flesh) | – | X | – | 82 | 11.8 | 111 | 13.8 | 0.28 | 32 | 10.7 | 161 | 13.4 | 0.212 | 16 | 15.9 | 177 | 12.7 | 0.548 |
| v34: eggs | – | X | – | 75 | 10.8 | 82 | 10.2 | 0.674 | 28 | 9.3 | 129 | 10.8 | 0.528 | 4 | 3.7 | 153 | 11 | 0.014* |
| v35: fish and seafood | – | X | – | 265 | 38.3 | 285 | 35.4 | 0.259 | 121 | 40.3 | 429 | 35.8 | 0.16 | 34 | 31.8 | 516 | 37.1 | 0.299 |
| v36: legumes, nuts and seeds | – | X | – | 389 | 56.2 | 409 | 50.7 | 0.038* | 172 | 57.3 | 626 | 52.3 | 0.121 | 46 | 43 | 752 | 54.1 | 0.034* |
| v37: milk and milk products | – | X | – | 24 | 3.5 | 30 | 3.7 | 0.89 | 11 | 3.7 | 43 | 3.6 | 1 | 4 | 3.7 | 50 | 3.6 | 0.791 |
| v38: oils and fats | – | X | – | 270 | 39 | 324 | 40.2 | 0.672 | 116 | 38.7 | 478 | 39.9 | 0.742 | 39 | 36.4 | 555 | 39.9 | 0.539 |
| v39: sweets | – | X | – | 135 | 19.5 | 160 | 19.9 | 0.896 | 56 | 18.7 | 239 | 19.9 | 0.685 | 13 | 12.1 | 282 | 20.3 | 0.043* |
| v40: spices, condiments and beverages | – | X | – | 146 | 21.1 | 161 | 20 | 0.608 | 59 | 19.7 | 248 | 20.7 | 0.749 | 18 | 16.8 | 289 | 20.8 | 0.385 |
| Self-production of crops | ||||||||||||||||||
| v41: maize | – | X | – | 636 | 98.5 | 726 | 98.5 | 1 | 278 | 98.9 | 1084 | 98.4 | 0.784 | 94 | 96.9 | 1268 | 98.6 | 0.178 |
| v42: rice | – | X | – | 166 | 25.7 | 207 | 28.1 | 0.332 | 74 | 26.3 | 299 | 27.1 | 0.822 | 30 | 27 | 343 | 26.7 | 0.406 |
| v43: sorghum | – | X | – | 135 | 20.9 | 146 | 19.8 | 0.639 | 68 | 24.2 | 213 | 19.3 | 0.081 | 25 | 25.8 | 256 | 19.9 | 0.19 |
| v44: cassava | – | X | – | 271 | 42 | 287 | 38.9 | 0.272 | 119 | 42.3 | 439 | 39.8 | 0.454 | 33 | 34 | 525 | 40.8 | 0.199 |
| v45: wheat | – | X | – | 1 | 0.2 | 3 | 0.4 | 0.628 | 0 | 0 | 4 | 0.4 | 0.588 | 0 | 0 | 4 | 0.3 | 1 |
| v46: yams | – | X | – | 143 | 22.1 | 151 | 20.5 | 0.469 | 53 | 18.9 | 241 | 21.9 | 0.289 | 15 | 15.5 | 279 | 21.7 | 0.159 |
| v47: pumpkin | – | X | – | 266 | 41.2 | 282 | 38.3 | 0.271 | 120 | 42.7 | 428 | 38.8 | 0.246 | 35 | 36.1 | 513 | 39.9 | 0.519 |
| v48: spinach and other green leafy vegetables | – | X | – | 61 | 9.4 | 63 | 8.5 | 0.573 | 30 | 10.7 | 94 | 8.5 | 0.292 | 11 | 11.3 | 113 | 8.8 | 0.36 |
| v49: vitamin A rich fruits (mango, apricot, papaya and peach) | – | X | – | 45 | 7 | 51 | 6.9 | 1 | 19 | 6.8 | 77 | 7 | 1 | 11 | 11.3 | 85 | 6.6 | 0.094 |
| v50: banana | – | X | – | 14 | 2.2 | 20 | 1.7 | 0.603 | 5 | 1.8 | 29 | 2.6 | 0.52 | 2 | 2.1 | 32 | 2.5 | 1 |
| v51: other fruits (orange, water melon and melon) | – | X | – | 12 | 1.9 | 16 | 2.2 | 0.707 | 7 | 2.5 | 21 | 1.9 | 0.484 | 3 | 3.1 | 25 | 1.9 | 0.441 |
| v52: pea and beans | – | X | – | 354 | 54.8 | 382 | 51.8 | 0.28 | 160 | 56.9 | 576 | 52.3 | 0.18 | 55 | 56.7 | 881 | 53 | 0.527 |
| v53: nuts and other legumes | X | 169 | 26.2 | 183 | 24.8 | 0.578 | 71 | 25.3 | 281 | 25.5 | 1 | 26 | 26.8 | 326 | 25.3 | 0.719 | ||
| Ownership of agricultural assets | ||||||||||||||||||
| v54: farmland | – | X | – | 641 | 92.6 | 727 | 90.2 | 0.098 | 280 | 93.3 | 1088 | 90.8 | 0.206 | 96 | 89.7 | 1272 | 91.4 | 0.48 |
| v55: home garden | – | X | – | 8 | 1.2 | 9 | 1.1 | 1 | 5 | 1.7 | 12 | 1 | 0.358 | 3 | 1.7 | 14 | 1 | 0.116 |
| v56: milk cow, cattle and bull | – | X | – | 4 | 0.6 | 1 | 0.1 | 0.188 | 2 | 0.7 | 3 | 0.3 | 0.263 | 1 | 0.9 | 4 | 0.3 | 0.31 |
| v57: horse, donkey and mule | – | X | – | 0 | 0 | 1 | 0.1 | 1 | 0 | 0 | 1 | 0.1 | 1 | 0 | 0 | 1 | 0.1 | 1 |
| v58: goat | – | X | – | 20 | 2.9 | 26 | 3.2 | 0.765 | 13 | 4.3 | 33 | 2.8 | 0.188 | 3 | 2.8 | 43 | 3.1 | 1 |
| v59: chicken and other poultry | – | X | – | 226 | 32.7 | 247 | 30.6 | 0.404 | 107 | 35.7 | 366 | 30.6 | 0.096 | 36 | 33.6 | 437 | 31.4 | 0.666 |
| Mean | SD | Mean | SD | P value§ | Mean | SD | Mean | SD | P value§ | Mean | SD | Mean | SD | P value§ | ||||
| Interval and ratio variables | ||||||||||||||||||
| v60: number of months without maize during last 12 months (mo) | X | – | – | 0.6 | 1.73 | 0.7 | 1.93 | 0.147 | 0.6 | 1.77 | 0.6 | 1.86 | 0.483 | 0.8 | 1.92 | 0.6 | 1.84 | 0.361 |
| v61: number of months without cassava during last 12 months (mo) | X | – | – | 2.9 | 4.19 | 2.7 | 4.18 | 0.268 | 3.2 | 4.4 | 2.7 | 4.1 | 0.093 | 3.4 | 4.51 | 2.7 | 4.15 | 0.262 |
| v62: number of months without rice during last 12 months (mo) | X | – | – | 2.9 | 4.42 | 3 | 4.39 | 0.464 | 3 | 4.5 | 2.9 | 4.4 | 0.958 | 3.4 | 4.63 | 2.9 | 4.38 | 0.241 |
| v63: household dietary diversity score (pt) c | X | – | – | 4.5 | 2.01 | 4.3 | 2.1 | 0.069 | 4.4 | 1.97 | 4.4 | 2.08 | 0.312 | 4.1 | 1.97 | 4.4 | 2.06 | 0.06 |
| v64: total number of meals yesterday (meal) | X | – | – | 2.7 | 0.53 | 2.7 | 0.5 | 0.873 | 2.7 | 0.48 | 2.7 | 0.52 | 0.353 | 2.7 | 0.5 | 2.7 | 0.51 | 0.806 |
| v65: farmland size (ha) | X | – | – | 288 | 1010 | 352 | 1067 | 0.463 | 379 | 1352 | 308 | 949 | 0.939 | 522 | 1722 | 307 | 969 | 0.145 |
| v66: home-garden size(m2) | X | – | – | 205 | 363 | 130 | 162 | 0.306 | 121 | 212 | 184 | 295 | 0.364 | 200 | 259 | 158 | 279 | 0.407 |
*p<0.05, **p<0.01.
†Categorisation based on the previous review (Black et al. 2013).15
‡χ2 test (Fisher’s exact test)
§Mann-Whitney U test.
Table 4.
Bivariate analyses between undernutrition and feeding/caring practice variables
| Background variable | Type of intervention and conditions† | Stunting (N=1498) | Underweight(N=1498) | Wasting (N=1498) | ||||||||||||||
| Nutrition specific | Nutrition sensitive | Enabling environment | (+) Stunted | (−) Not stunted | P value‡ | (+) Under weight | (−) Not underweight | P value‡ | (+) Wasted | (−) Not wasted | P value‡ | |||||||
| N | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |||||||
| Categorical variables | ||||||||||||||||||
| Food preparation process | ||||||||||||||||||
| v67: rinse vegetable and fruit with safe water | – | X | – | 548 | 79.2 | 655 | 81.3 | 0.329 | 248 | 82.7 | 955 | 79.7 | 0.291 | 89 | 83.2 | 1114 | 80.1 | 0.528 |
| : Cook meat thoroughly till meat juice is clear | – | X | – | 409 | 59.1 | 483 | 59.9 | 0.752 | 181 | 60.3 | 711 | 59.3 | 0.793 | 75 | 70.1 | 817 | 58.7 | 0.024* |
| v69: store leftovers in cool places§ | – | X | – | 127 | 18.4 | 144 | 17.9 | 0.84 | 51 | 18.8 | 220 | 18.4 | 0.616 | 17 | 15.9 | 254 | 18.3 | 0.604 |
| v70: store staple food in container(s) with cover¶ | – | X | – | 192 | 27.7 | 253 | 31.4 | 0.126 | 84 | 28 | 361 | 30.1 | 0.481 | 35 | 32.7 | 410 | 29.5 | 0.51 |
| v71: store utensils in cabinet after cleaning | – | X | – | 95 | 13.7 | 107 | 13.3 | 0.82 | 48 | 16 | 154 | 12.9 | 0.157 | 23 | 21.5 | 1391 | 92.9 | 0.018* |
| v72: iodised table salt | X | – | 531 | 76.7 | 618 | 76.7 | 1 | 218 | 72.7 | 931 | 77.7 | 0.067 | 75 | 70.1 | 1074 | 77.2 | 0.059 | |
| Food preparation conditions | ||||||||||||||||||
| v73: clean cooking fuel†† | – | X | – | 0 | 0 | 2 | 0.2 | 0.503 | 0 | 0 | 2 | 0.2 | 1 | 0 | 0 | 2 | 0.1 | 1 |
| v74: indoor cooking facility‡‡ | – | X | – | 368 | 53.2 | 485 | 60.2 | 0.07 | 161 | 53.7 | 692 | 57.8 | 0.216 | 68 | 63.6 | 785 | 56.4 | 0.158 |
| Infant and young child feeding | ||||||||||||||||||
| v75: breastfed in 1 hour after birth (n=754)§§ | X | – | – | 223 | 96.1 | 490 | 93.9 | 0.228 | 69 | 93.2 | 644 | 94.7 | 0.587 | 53 | 91.4 | 660 | 94.8 | 0.234 |
| v76: exclusively breastfed (n=156)¶¶ | X | – | – | 22 | 73.3 | 95 | 75.4 | 0.817 | 6 | 66.7 | 111 | 75.5 | 0.692 | 10 | 66.7 | 107 | 75.9 | 0.53 |
| v77: continued breastfeeding at 1 year (n=104)*** | X | – | – | 35 | 94.6 | 54 | 80.6 | 0.078 | 14 | 100 | 75 | 83.3 | 0.212 | 7 | 87.5 | 82 | 85.4 | 1 |
| v78: introduction of solid, semi-solid and/or soft foods (n=132)††† | X | – | – | 13 | 54.2 | 84 | 77.8 | 0.023* | 4 | 50 | 93 | 75 | 0.207 | 5 | 50 | 92 | 75.4 | 0.129 |
| v79: at least four of seven food groups consumed (n=605)‡‡‡ | X | – | – | 18 | 8.9 | 27 | 6.7 | 0.329 | 6 | 9.2 | 39 | 7.2 | 0.614 | 2 | 4.5 | 43 | 7.7 | 0.763 |
| v80: minimum meal frequency (n=605)§§§ | X | – | – | 34 | 16.8 | 68 | 16.9 | 1 | 9 | 13.8 | 93 | 17.2 | 0.6 | 9 | 20.5 | 93 | 16.6 | 0.53 |
| Pre- and post-birth care | ||||||||||||||||||
| v81:≥4 antenatal care visits | – | X | – | 314 | 45.4 | 345 | 42.8 | 0.322 | 50 | 46.7 | 609 | 43.8 | 0.614 | 189 | 27.3 | 236 | 29.3 | 0.421 |
| v82: facility-based delivery | – | X | – | 345 | 49.9 | 421 | 52.2 | 0.378 | 155 | 51.7 | 611 | 51 | 0.947 | 53 | 49.5 | 713 | 51.3 | 0.764 |
| v83: low birth weight (<2500 gram at birth) | X | – | – | 89 | 12.9 | 99 | 11 | 0.262 | 45 | 15 | 132 | 11.1 | 0.072 | 18 | 16.8 | 159 | 11.5 | 0.119 |
| v84: mother–child cosleeping | X | X | – | 636 | 91.9 | 777 | 96.4 | <0.001** | 265 | 88.3 | 1148 | 95.8 | <0.001** | 87 | 90.7 | 1316 | 94.6 | 0.123 |
| Primary attendant for the child’s birth | ||||||||||||||||||
| Skilled birth attendant (physician, nurse and midwife) | – | – | – | 596 | 86.1 | 703 | 87.2 | Ref. | 254 | 84.7 | 1045 | 87.2 | Ref. | 95 | 88.8 | 1204 | 86.6 | Ref. |
| v85: traditional birth attendant | – | X | – | 33 | 5.1 | 35 | 4.7 | 0.709 | 12 | 4.4 | 56 | 5 | 0.875 | 1 | 1 | 67 | 5.2 | 0.084 |
| v86: no health worker attended | – | X | – | 12 | 1.9 | 13 | 1.7 | 0.843 | 5 | 1.8 | 20 | 1.8 | 1 | 278 | 40.2 | 163 | 20.2 | <0.001** |
| v87: Do not know do not remember | – | X | – | 51 | 7.4 | 55 | 6.8 | 0.687 | 29 | 9.7 | 77 | 6.4 | 0.059 | 9 | 8.4 | 97 | 7 | 0.556 |
| Total | 692 | 100 | 806 | 100 | 0.687 | 300 | 100 | 1198 | 100 | 107 | 100 | 1391 | 100 | |||||
| Ownership of home-based records | ||||||||||||||||||
| v88: child vaccination card/handbook | X | – | – | 368 | 53.2 | 436 | 54.1 | 0.755 | 139 | 46.3 | 665 | 55.5 | 0.005* | 42 | 39.3 | 762 | 54.8 | 0.002* |
| v89: maternal health card/handbook | X | – | – | 72 | 10.4 | 85 | 10.5 | 1 | 36 | 12 | 121 | 10.1 | 0.343 | 14 | 13.1 | 143 | 10.3 | 0.33 |
| v90:child health card/handbook | X | – | – | 125 | 18.1 | 127 | 15.8 | 0.24 | 60 | 20 | 192 | 16 | 0.102 | 14 | 2 | 15 | 1.9 | 0.346 |
| v91: maternal and child health card/handbook | X | – | – | 14 | 2 | 15 | 1.9 | 0.853 | 8 | 2.7 | 21 | 1.8 | 0.346 | 3 | 2.8 | 26 | 1.9 | 0.457 |
| v92: birth certificate | X | – | – | 51 | 7.4 | 53 | 6.6 | 0.61 | 30 | 10 | 74 | 6.2 | 0.030* | 13 | 12.1 | 91 | 6.5 | 0.045* |
| v93: any home-based record(s) | X | – | – | 581 | 84 | 679 | 84.2 | 0.887 | 247 | 82.3 | 1013 | 84.6 | 0.377 | 88 | 82.2 | 1172 | 84.3 | 0.583 |
| Mean | SD | Mean | SD | P value¶¶¶ | Mean | SD | Mean | SD | P value¶¶¶ | Mean | SD | Mean | SD | P value¶¶¶ | ||||
| Interval and ratio variables | ||||||||||||||||||
| v94: mother’s current height (cm) | X | – | – | 153.7 | 7.02 | 154.2 | 7.5 | 0.020* | 153.7 | 6.66 | 154.1 | 7.43 | 0.117 | 154.3 | 6.3 | 154 | 7.35 | 0.676 |
*p<0.05,
†Categorisation based on the previous review (Black et al. 2013).15
‡χ2 test (Fisher’s exact test)
§Cool places include: (i) refrigerator and (ii) under shadow.
¶Materials of containers include: (i) plastic and (ii) metal.
**p<0.01.
††Clean cooking fuel includes: (i) electricity; (ii) gas; and (iii) solar energy (WHO 2016).38
‡‡Indoor cooking facility includes: (i) kitchen in a house and (ii) kitchen in a separate building. (Malla and Timilsina).39
§§Applicable only for children 0–24 months of age (n=754) (WHO 2010).37
¶¶Applicable only for children 0–5 months of age (n=156) (WHO 2010).37
***Applicable only for children 12–15 months of age (n=104) (WHO 2010).37
†††Applicable only for children 6–8 months of age (n=132) (WHO 2010).37
‡‡‡Seven food groups are composed of: (i) grains/roots/tubers; (ii) legumes/nuts; (iii) milk products; (iv) flesh foods; (v) eggs; and (vi) other fruits and vegetables. Applicable only for children 6–23 months of age (n=605) (WHO 2010).37
§§§Minimum meal frequency is defined as: (i) 2 (meal/day) for breastfed children 6–8 months of age; (ii) 3 (meal/day) for breastfed children 9–23 months of age; and (iii) 4 (meal/day) for non-breastfed children 6–23 months of age. Applicable only for children 6–23 months of age (n=605) (WHO 2010).37
¶¶¶Mann-Whitney U test.
Table 5.
Bivariate analyses between undernutrition and household environment variables
| Background variable | Type of intervention and conditions† | Stunting (N=1498) | Underweight(N=1498) | Wasting (N=1498) | ||||||||||||||
| Nutrition specific | Nutrition sensitive | Enabling environment | (+) Stunted | (−) Not stunted | P value ‡ | (+) Under-weight | (−) Not underweight | P value ‡ | (+) Wasted | (−) Not wasted | P value‡ | |||||||
| N | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |||||||
| Categorical variables | ||||||||||||||||||
| Type of water source for drinking and cooking | ||||||||||||||||||
| Not improved type of source of water§ | – | – | – | 264 | 38.2 | 307 | 38.1 | Ref. | 108 | 36 | 463 | 38.6 | Ref. | 38 | 35.5 | 533 | 38.3 | Ref. |
| v95: improved type of source of water¶ | – | X | – | 428 | 61.8 | 499 | 61.9 | 1 | 192 | 64 | 735 | 61.4 | 0.425 | 69 | 64.5 | 858 | 61.7 | 0.606 |
| Total | 692 | 100 | 806 | 100 | 300 | 100 | 1198 | 100 | 107 | 100 | 1391 | 100 | ||||||
| Availability of water at water source | ||||||||||||||||||
| On and off†† | – | – | – | 119 | 17.2 | 166 | 20.6 | Ref. | 51 | 17 | 234 | 19.5 | Ref. | 14 | 13.1 | 271 | 19.5 | Ref. |
| v96: 24 hours a day ‡‡ | – | X | – | 573 | 82.8 | 640 | 79.4 | 0.099 | 249 | 83 | 964 | 80.5 | 0.366 | 93 | 86.9 | 1120 | 80.5 | 0.124 |
| Total | 692 | 100 | 806 | 100 | 300 | 100 | 1198 | 100 | 107 | 100 | 1391 | 100 | ||||||
| Type of sanitation facility and excreta disposal | ||||||||||||||||||
| Not improved type of sanitation facility §§ | – | – | 638 | 92.2 | 752 | 93.3 | Ref. | 269 | 89.7 | 1121 | 93.6 | Ref. | 100 | 93.5 | 1290 | 92.7 | Ref. | |
| v97: improved type of sanitation facility ¶¶ | – | X | – | 54 | 7.8 | 54 | 6.7 | 0.424 | 31 | 10.3 | 77 | 6.4 | 0.024* | 7 | 6.5 | 101 | 7.3 | 1 |
| Total | 692 | 100 | 806 | 100 | 300 | 100 | 1198 | 100 | 107 | 100 | 1391 | 100 | ||||||
| Domestic water treatment | ||||||||||||||||||
| Inappropriate or no water treatment | – | – | – | 528 | 76.3 | 589 | 73.1 | Ref. | 226 | 75.3 | 891 | 74.4 | Ref. | 78 | 72.9 | 1039 | 74.7 | Ref. |
| v98: appropriate water treatment | – | X | – | 164 | 23.7 | 217 | 26.9 | 0.171 | 74 | 24.7 | 307 | 25.6 | 0.767 | 29 | 27.1 | 352 | 25.3 | 0.73 |
| Total | 692 | 100 | 806 | 100 | 300 | 100 | 1198 | 100 | 107 | 100 | 1391 | 100 | ||||||
| Hand washing practices | ||||||||||||||||||
| v99: wash hand with soap or ash after toilet | – | X | – | 269 | 38.9 | 327 | 40.6 | 0.525 | 117 | 39 | 479 | 40 | 0.792 | 42 | 39.3 | 554 | 39.8 | 1 |
| v100: wash hand with soap or ash before cooking | – | X | – | 263 | 38 | 315 | 39.1 | 0.709 | 114 | 38 | 464 | 38.7 | 0.842 | 41 | 38.3 | 537 | 38.6 | 1 |
| v101: wash hand with soap or ash before eating | – | X | – | 249 | 36 | 304 | 37.7 | 0.519 | 115 | 38.3 | 438 | 36.6 | 0.593 | 40 | 37.4 | 513 | 36.9 | 0.918 |
| Mean | SD | Mean | SD | P value *** | Mean | SD | Mean | SD | P value*** | Mean | SD | Mean | SD | P value*** | ||||
| Interval and ratio variables | ||||||||||||||||||
| v102: total time for water collection (min) ††† | – | X | – | 57.6 | 58.7 | 54.4 | 60.2 | 0.096 | 55 | 58.5 | 56 | 59.8 | 0.638 | 67.9 | 73.8 | 55 | 58.3 | 0.277 |
*p<0.05, **p<0.01.
†Categorisation based on the previous review (Black et al. 2013).15
‡χ2 test (Fisher’s exact test)
§Types of not improved source of water include: (i) unprotected well; (ii) unprotected spring; (iii) surface water (eg, river, lake and reservoir); (iv) vendor-provided water (eg, truck and cart); and (v) bottled water.
¶Types of improved source of water include: (i) piped private household connection indoor/in yard; (ii) public standpipe; (iii) protected well (protected hand-dug well); (iv) protected spring; and (v) rain water collection.
**p<0.01.
††For instance, water is available only when public water attendant is on duty.
‡‡Includes 37 cases of ‘Do not know/do not remember’.
§§Types of not improved sanitation facilities include: (i) flush toilet not connected to sewerage system; (ii) latrine without slab; (iii) joint installation with other households; and (vi) outdoor defecation.
¶¶Types of improved sanitation facilities include: (i) flush toilet connected to sewerage system/septic tank; (ii) ventilated latrine/pit; (iii) toilet connected to pit/latrines with slab; and (iv) other non-sewered sanitation systems.
***Mann-Whitney U test.
†††The number of minutes spent reaching a water source and waiting there was measured by making enumerators physically walk.
Table 6.
Bivariate analyses between undernutrition and disease symptoms (including micronutrient deficiency)
| Background variable | Type of intervention and conditions† | Stunting (N=1498) | Underweight (N=1498) | Wasting (N=1498) | ||||||||||||||
| Nutrition specific | Nutrition sensitive | Enabling environment | (+) Stunted | (−) Not stuntd | P value ‡§ | (+) Under weight | (−) Not underweight | P value ‡ | (+) Wasted | (−) Not wasted | P value‡ | |||||||
| N | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |||||||
| Categorical variables | ||||||||||||||||||
| Low birth weight | ||||||||||||||||||
| (−) Not low birth weight:≥2500 [g) | – | – | – | 601 | 67.1 | 714 | 89 | Ref. | 255 | 85 | 1060 | 88.9 | Ref. | 89 | 83.2 | 1226 | 88.5 | Ref. |
| v103: (+) Low birth weight:<2500 (g) | X | – | – | 89 | 12.9 | 88 | 11 | 0.262 | 45 | 15 | 132 | 11.1 | 0.072 | 18 | 16.8 | 159 | 11.5 | 0.119 |
| Total | 660 | 100 | 773 | 100 | 283 | 100 | 1150 | 100 | 105 | 100 | 1328 | 100 | ||||||
| Anaemia§ | ||||||||||||||||||
| (-) Without anaemia: haemoglobin concentration ≥110 (g/L) | – | – | – | 291 | 45.5 | 309 | 49.9 | Ref. | 125 | 44.8 | 475 | 48.5 | Ref. | 39 | 44.8 | 561 | 47.9 | Ref. |
| v104: (+) With anaemia: haemoglobin concentration <110 (g/L) | X | – | – | 348 | 54.5 | 310 | 50.1 | 0.128 | 154 | 55.2 | 504 | 51.5 | 0.278 | 48 | 55.2 | 610 | 52.1 | 0.657 |
| Total | 660 | 100 | 773 | 100 | 283 | 100 | 1150 | 100 | 105 | 100 | 1328 | 100 | ||||||
| Diarrhoea during the last 2 weeks | ||||||||||||||||||
| (−) Without diarrhoea | – | – | – | 463 | 70.2 | 528 | 68.3 | Ref. | 200 | 70.7 | 791 | 68.8 | Ref. | 67 | 63.8 | 924 | 69.6 | Ref. |
| v105: (+) With diarrhoea | X | – | – | 197 | 29.8 | 245 | 31.7 | 0.456 | 83 | 29.3 | 359 | 31.2 | 0.566 | 38 | 36.2 | 404 | 30.4 | 0.228 |
| Total | 660 | 100 | 773 | 100 | 283 | 100 | 1150 | 100 | 105 | 100 | 1328 | 100 | ||||||
| Cough during the last 2 weeks | ||||||||||||||||||
| (-) Without cough | – | – | – | 386 | 58 | 436 | 55.8 | Ref. | 155 | 53.6 | 667 | 57.6 | Ref. | 48 | 45.3 | 774 | 57.8 | Ref. |
| v106: (+) with cough | X | – | – | 279 | 42 | 345 | 44.2 | 0.424 | 134 | 46.4 | 490 | 42.4 | 0.232 | 58 | 54.7 | 566 | 42.2 | 0.014* |
| Total | 665 | 100 | 781 | 100 | 289 | 100 | 1157 | 100 | 106 | 100 | 1340 | 100 | ||||||
| Fever during the last 2 weeks | ||||||||||||||||||
| (−) Without cough | – | – | – | 386 | 58 | 436 | 55.8 | Ref. | 155 | 53.6 | 667 | 57.6 | Ref. | 48 | 45.3 | 774 | 57.8 | Ref. |
| v107: (+) with fever | X | – | – | 270 | 40.7 | 393 | 59.3 | 0.065 | 116 | 40.6 | 435 | 37.6 | 0.377 | 45 | 42.5 | 506 | 37.8 | 0.351 |
| Total | 663 | 100 | 781 | 100 | 286 | 100 | 1158 | 100 | 106 | 100 | 1338 | 100 | ||||||
*Categorisation based on the previous review (Black et al. 2013).15
†χ2 test (Fisher’s exact test)
‡A total of 1258 children were tested for anaemia as a result of exclusion of 240 children (=138 children under 6 months of age+102 children having rejected blood sampling).
§p<0.05, **p<0.01.
Multivariate analyses
As the results of bivariate analyses and multicollinearity testing, five, two and three background variables were employed as the independent variables for the logistic regression models for stunting, underweight and wasting, respectively. Simultaneous variable entry was applied to logistic regression analyses. Table 7 shows their results. Timely introduction of solid, semi-solid or soft foods to children was the only independent variable whose OR was significant (p<0.05) in the logistic regression model for stunting. This implies that introduction of solid, semi-solid or soft foods to children at the age of 6–8 months is likely to have reduced the risk of becoming stunted by 68.3% (= (1–0.317)×100). In the logistic regression model for underweight, a significant OR (p<0.05) was detected for both two independent variables, that is, mother–child cosleeping and ownership of birth certificate. Mother–child cosleeping is likely to have reduced the risk of becoming underweight by 66.7% (= (1–0.333)×100). Those having birth certificate are 1.656 times more likely to be underweight. Of 113 birth certificate holders, 103 (91.2%) owned it as the only home-based record. A birth certificate does include not the data and information related to maternal and child health but exclusively the name, sex and date of birth of a child and his/her parents’ names.40 Thus, ownership of birth certificate implies either absence or extreme lack of opportunities for parents to practice self-monitoring and self-care of their maternal and child health. Two independent variables whose ORs were significant (p<0.05) were detected in the logistic regression model for wasting (availability and consumption of eggs generally household members and cough during the last 2 weeks). It was found availability and consumption of eggs were protective against becoming wasted, by indicating 91.6% (= (1–0.184)×100) reduction of risk of becoming wasted. Cough during the last 2 weeks was highly associated with being wasted, by producing a greater OR (ie, adjusted OR=1.713).
Table 7.
Logistic regressions on being malnourished with background variables
| Logistic regression model | Type of intervention and conditions† | Adjusted | 95% CI | P value | ||
| Nutrition specific | Nutrition sensitive | Enabling environment | OR | |||
| Logistic regression for stunting | ||||||
| v1: sex (dummy variable for ‘male’) | – | – | X | 1.482 | 0.573 to 3.830 | 0.417 |
| v17: ownership of refrigerator | – | X | X | 0 | 0 | 0.999 |
| v25: age (year) | – | – | X | 6.617 | 0.017 to 2550.7 | 0.534 |
| v32: availability and consumption of fruits (vitamin A rich and other fruits) | – | X | – | 1.001 | 0.198 to 5.055 | 0.999 |
| v79: introduction of solid, semi-solid and/or soft foods | X | – | – | 0.317 | 0.124 to 0.812 | 0.017 * |
| Logistic regression for underweight | ||||||
| v84: mother–child cosleeping | X | X | – | 0.333 | 0.212 to 0.524 | <0.001 ** |
| v92: ownership of birth certificate | X | – | – | 1.656 | 1.057 to 2.596 | 0.028 * |
| Logistic regression for wasting | ||||||
| v34: availability and consumption of eggs | – | X | – | 0.184 | 0.045 to 0.754 | 0.019 * |
| v86: delivery not attended by health workers | X | – | – | 1.45 | 0.330 to 6.383 | 0.623 |
| v106: cough during the last 2 weeks | X | – | – | 1.713 | 1.128 to 2.603 | 0.012 * |
*p<0.05, **p<0.01.
†Categorisation based on the previous review (Black et al. 2013).15
Discussion
All the three types of undernutrition prevalence rates are at the similar level to both provincial and national prevalence as of 2011 (table 1). This implies that there has been probably neither an improvement nor a worsening in prevalence of all three forms of child undernutrition during 8 years from 2011 to 2019. In particular, very high prevalence of stunting (46.2%) we identified is in line with its Mozambique’s national trend that prevalence of stunting stays around 42%–43% during the last 12 years.11 This should be attributable not only to inadequate multisectoral coordination and fragmented efforts by relevant sectors and stakeholders but also to generally slower progress of reduction in prevalence of stunting than in those of underweight and wasting.41
This study identified timely introduction of solid, semi-solid or soft foods to children as the only significant determinant of or risk factors for being stunted (p<0.05) (table 7). Several studies reported that timely introduction of solid, semi-solid or soft foods at the age of 6–8 months provides children with significant protection against becoming stunted.42–44 Thus, the results of our study are consistent to these earlier studies. Yet, giving solid, semi-solid or soft foods to children 6–8 months of age needs to be supported by mothers’ previous exclusive breastfeeding practices at the age of 0–5 months. In other words, giving solid, semi-solid or soft foods not accompanied by previous exclusive breastfeeding may often involve premature introduction of those foods prior to 6 months of age. A multicountry study in Africa reported that infants suffering from diarrhoea and respiratory infections were significantly likely to be introduced solid, semi-solid or soft foods prematurely between the age of 3 and 5 months.45 As stunting, diarrhoea and respiratory infections are mutually attributable,46 47 the importance of timely introduction of solid, semi-solid or soft foods at the appropriate age must be rehighlighted. This is also because timely introduction of solid, semi-solid or soft foods plays a key role in smoothly responding to an additional energy requirement derived from the increase in child’s activities during 6–8 months of age. In our study, of 97 children 6–8 months of age given solid, semi-solid or soft foods, 79 (81.4%) used to be exclusively breastfed during 0–5 months of age (p<0.05 in χ2/Fisher’s exact test). Thus, a majority of mothers and other caregivers giving solid, semi-solid or soft foods to their children of 6–8 months of age in Majune and Muembe districts have been continuously practising appropriate infant feeding since their childrens’ births.
Mother–child cosleeping serves not just as the general proxy for desirable caring attitude, but rather as a reliable channel that ensures breastfeeding timely and frequently enough during night time and nap time. Several earlier studies indicated that mothers’ physical contacts through cosleeping with their children predict feeding in response to early hunger cues.48–50 Mother–child cosleeping, however, may increase the risks of Sudden Unexpected Death in Infancy (SUDI), through regulating infant’s breathing by the rocking movement of the mother’s chest while breathing.51 Thus, while mother–child cosleeping is generally recommended not only for ensuring timely and adequate breastfeeding but also for facilitating physiological, cognitive and socioemotional development of children, efforts to minimise the risks of SUDI should be carefully made. A typical example of those efforts is to avoid cosleeping on sofa or couch which increases the likelihood of child’s breathing regulation.52 The enumerators employed for this survey rarely observed sofa and couch during household visits. Thus, the risks of SUDI to be derived from mother–infant cosleeping in the two districts should be quite limited.
The ownership of a birth certificate largely implies non-ownership of health-related home-based record (eg, child vaccination, maternal health card, child health card, maternal and child health card). Those having their children’s birth certificates might think it is unnecessary to have health-related home-based records, assuming as if a birth certificate sufficed all requirements as an all-round home-based record unique to their children (eg, eligibility for school enrollment). Of 1498 children under 5 years of age, 341 (22.8%) did not have health-related home-based records (ie, either only birth certificate or no home-based record). In view of the WHO’s recommendation of health-related home-based records as an effective tool for maternal and child health,53 the recent commitment of the Mozambican Ministry of Health to developing a nationally standardised home-based record for maternal and child health is highly valued.
In this study, availability of eggs at households and their consumption generally by household members was measured as a food security variable for calculating HDDS. On the other hand, consumption of eggs by each child under 5 years of age was separately measured as a feeding/caring practice variable for calculating the IYCF minimum diet diversity. Thus, availability and consumption of eggs generally at household level are defined and measured differently from child-specific consumption of eggs, in this study. There is a possibility that eggs might have been consumed exclusively by the household members other than children at some households. In view of this, of 148 studied children of 6–59 months of age whose households had readily available eggs and actually consumed them, 114 (77.0%) actually ate eggs during the last 24 hours (p<0.05 in χ2/Fisher’s exact test). Thus, mothers and caregivers of children of 6–59 months of age in Majune and Muembe districts tend to proactively practice introduction of eggs during complementary feeding, as far as eggs are readily available at households. Several studies reported that early introduction of eggs in complementary feeding significantly improved growth and nutritional status of young children.54 Thus, the results of our study support those earlier studies. Yet, instability of egg production and supplies in Niassa province55 are likely to make it generally difficult for households in Majune and Muember districts to access and consume eggs.
A significantly positive association between having cough during the last 2 weeks and being wasted (adjusted OR = 1.713) implies that appetite reduced by respiratory infections might have caused inadequate food intake and digestion, and thereby acute undernutrition. There are a number of earlier studies on the causality between cough and undernutrition.47 56–58 Particularly, severe acute malnutrition (z-score for weight-for-height < −3) is often accompanied by cough and fever. Thus, the association between having cough and being wasted we identified not only is in line with the results of those earlier studies but also signals a certain need for therapeutic feeding.
Figure 1 shows the hypothetical process of becoming malnourished based on the findings of our study. None of the determinants of and risk factors for whether being malnourished we identified was common across three types of undernutrition (ie, stunting, underweight and wasting) (table 7). This probably does not necessarily indicate that each determinant contributes exclusively to a specific type of undernutrition. For instance, mother–child cosleeping was significantly associated with both being stunted and being underweight in bivariate analyses. Yet, due to possible multicollinearity, it was excluded from the independent variables in the logistic regression model for stunting.
Figure 1.
Hypothetical process of becoming stunting, underweight and wasted. oOR, adjusted OR. Adapted from Black et al. 2013
Some could be critical about adopting such a great number of independent variables. Yet, in a total absence of a standard set of variables and indicators for identifying the determinants of and risk factors for child undernutrition, taking all the possible variables, was an inevitable choice. In fact, mother–child cosleeping, a variable never employed in earlier studies, was identified as a determinant of and risk factor for whether being underweight in this study. Note that this was one of the key findings we reached by broadly screening all possible determinants.
This study has limitations in generalisability of determinants of and risk factors for child undernutrition due to employment of a cross-sectional study as the study design. We must particularly admit that possible overestimation of household food security status might have prevented this study from thoroughly identifying all the possible food-security-related determinants and risk factors. Generally, diverse food crops (including livestock products) are more available, accessible and affordable during the study period from August to October than yearly average.59 Thus, household food security we measured may not be representative of its year-round status. A further study is necessary to more precisely estimate associations between food security variables and undernutrition, as seasonal variation of food security data is generally greater than that of feeding and caring practice data and household environment data.
Conclusion
This study identified that timely introduction of solid, semi-solid or soft foods to children of 6–8 months of age as a determinant of being not stunted. Mother–child cosleeping and ownership of birth certificate were a protective factor from and a promoting factor for being underweight, respectively. Similarly, availability and consumption of eggs at the household level and cough during the last 2 weeks among children were a protective factor from and a promoting factor for being wasted, respectively.
Note that the aforementioned determinants and risk factors are likely to be very applicable neither to other provinces of Mozambique and other countries nor to different seasons. This is because causality and association between undernutrition and its background factors vary according to local settings and seasons. To enable us to make meaningful interprovincial, international and interseasonal comparisons, it is crucially necessary to develop a standard set of variables and indicators related to immediate and underlying causes of child undernutrition. Yet, it is reality that the numbers and types of independent variables employed for multivariate analysis largely differ between the studies. Some studies employed less than 10 independent variables,29 60 other employed more than 30.26 30 Moreover, the types and definitions of those variables are not consistent and standardised enough to allow us to meaningfully compare the data between the studies. Thus, it is an urgent task to develop an internationally standardised set of variables and indicators. SUN has proposed a standard set of 79 indicators from eight technical domains.61 Yet, they are the indicators appropriate not for identifying determinants and risk factors but rather for monitoring policy milestones and operational progress. Therefore, WHO, as the UN specialised agency responsible for health, should take responsibility for undertaking the task in collaboration with other key partners such as Food and Agriculture Organisation, UNICEF and SUN.
Conducting a multisectoral nutrition survey jointly between several key ministries (ie, typically, ministry of health, ministry of agriculture and ministry of public works) provides them with an invaluable opportunity to open a policy dialogue and further attempt to design, implement, monitor and evaluate a multisectoral nutrition programme in a joint or coordinated manner. Timely introduction of solid, semi-solid or soft foods, a possible key intervention we identified, could serve as a great entry point for the three sectors to start making joint efforts. To appropriately introduce solid, semi-solid or soft foods to a child, food production, water for cooking and feeding practising need to be undertaken by agriculture, water and health sectors, respectively. Though 54 of 61 SUN member countries (88.5%) set up national multistakeholder platform,62 it is not clear whether those platforms facilitate conducting multisectoral nutrition surveys as the joint efforts among the stakeholders. To ensure a better-designed package of evidence-based multisectoral interventions, it is recommended that the multistakeholder platform proactively work beyond sectoral interests in each country and that its initial step be to jointly conduct a multisectoral nutrition survey.
Acknowledgments
The authors gratefully thank Jaime Fernandes, Hannah Danzinger Silva and Maxwell Odhiambo for their support to data collection, and Toshiyasu Murai for his valuable technical supports to data analysis. The authors also thank Japan International Cooperation Agency (JICA) for its funding support to the study. This work is sincerely dedicated to all the children and their parents and caregivers in Niassa province of Mozambique.
Footnotes
Contributors: All the authors made substantial intellectual contributions to the study. HA, MN, JPML, MM, SN and HH conceptualised and designed the study. HA, MN, JPML, MM and EA took responsibility for data collection. HA and MN analysed and interpreted the data. HA drafted and finalised the manuscript. RM, AA, NT, DB, JV and AJC critically commented and revised manuscript. All the authors reviewed and approved the final version of the manuscript.
Funding: This work was supported by Japan International Cooperation Agency (JICA).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The study protocol was submitted to the National Committee for Bioethics of Ethics, the Mozambican Ministry of Health, for its ethical clearance. The Committee officially approved the study protocol accordingly (Ref: 279/CNBS/19). An informed consent to participate in both anthropometric measurements and structured household interviews were obtained in written form from the parents of each sampled schoolchild.
Provenance and peer review: Not commissioned; externally peer reviewed by Wondu Garoma Berra, Wollrga University, Ethiopia.
Data availability statement: Data are available upon reasonable request. The anonymised datasets used and analysed during the current study are available from the corresponding author on reasonable request. Please email: hirotsugu.aiga@nagasaki-u.ac.jp for data requests.
References
- 1. Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 2008;371:243–60. 10.1016/S0140-6736(07)61690-0 [DOI] [PubMed] [Google Scholar]
- 2. United Nations (UN) Millennium development goal 1 - Eradicate extreme poverty and hunger. New York: UN, 1990. Available: http://www.un.org/millenniumgoals/poverty.shtml [Accessed 5 Nov 2020].
- 3. United Nations (UN) Sustainable development goal 2 - End hunger, achieve food security and improved nutrition, and promote sustainable agriculture. New York: UN, 2015. Available: https://sustainabledevelopment.un.org/sdg2 [Accessed 5 Nov 2020].
- 4. Horton R. Maternal and child undernutrition: an urgent opportunity. Lancet 2008;371:179. 10.1016/S0140-6736(07)61869-8 [DOI] [PubMed] [Google Scholar]
- 5. Haddad L. How should nutrition be positioned in the post-2015 agenda? Food Policy 2013;43:341–52. 10.1016/j.foodpol.2013.05.002 [DOI] [Google Scholar]
- 6. World Bank Improving nutrition through multisectoral approaches. Washington DC: World Bank, 2013. Available: https://openknowledge.worldbank.org/bitstream/handle/10986/16450/75102revd.pdf?sequence=5&isAllowed=y [Accessed 5 Nov 2020].
- 7. Quisumbing AR, Ahmed A, Gilligan DO, et al. Randomized controlled trials of multi-sectoral programs: lessons from development research. World Dev 2020;127:104822. 10.1016/j.worlddev.2019.104822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Scale-Up Nutrition (SUN) Monitoring, evaluation, accountability, learning (meal) 2016 baseline assessment of key indicators dashboard guidance note. Geneva: sun. http://scalingupnutrition.org/wp-content/uploads/2017/11/DashboardGuidanceNote-_EN.pdf. 2015
- 9. United Nations Children’s Fund (UNICEF) The state of the world’s children 2019. Children, food and nutrition. New York: UNICEF, 2019. Available: https://www.unicef.org/sites/default/files/2019-12/SOWC-2019.pdf [Accessed 5 Nov 2020].
- 10. National Institute of Statistics (NIS) Mozambique demographic and health survey 2011. Maputo: NIS (in Portuguese), 2011. Available: https://dhsprogram.com/pubs/pdf/FR266/FR266.pdf [Accessed 5 Nov 2020].
- 11. World Bank World development indicators. Washington DC: World Bank, 2020. Available: https://databank.worldbank.org/source/world-development-indicators [Accessed 5 Nov 2020].
- 12. The Government of Mozambique (GoM) Multi-sectoral plan for chronic malnutrition reduction in Mozambique 2011-2015 (2020). Maputo: GoM, 2010. Available: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.359.8988&rep=rep1&type=pdf [Accessed 5 Nov 2020].
- 13. Michaud-Létourneau I, Pelletier DL. Perspectives on the coordination of multisectoral nutrition in Mozambique and an emerging framework. Food Policy 2017;70:84–97. 10.1016/j.foodpol.2017.07.001 [DOI] [Google Scholar]
- 14. Nomura M, Takahashi K, Reich MR. Trends in global nutrition policy and implications for Japanese development policy. Food Nutr Bull 2015;36:493–502. 10.1177/0379572115611288 [DOI] [PubMed] [Google Scholar]
- 15. Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013;382:427–51. 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- 16. United Nations Children’s Fund (UNICEF) Improving child nutrition: the achievable imperative for global progress. New York: UNICEF, 2013. Available: https://www.unicef.org/publications/files/Nutrition_Report_final_lo_res_8_April.pdf [Accessed 5 Nov 2020].
- 17. Aiga H, Matsuoka S, Kuroiwa C, et al. Malnutrition among children in rural Malawian fish-farming households. Trans R Soc Trop Med Hyg 2009;103:827–33. 10.1016/j.trstmh.2009.03.028 [DOI] [PubMed] [Google Scholar]
- 18. Reinhardt K, Fanzo J. Addressing chronic malnutrition through multi-sectoral, sustainable approaches: a review of the causes and consequences. Front Nutr 2014;1:1–11. 10.3389/fnut.2014.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vella V, Tomkins A, Borghesi A, et al. Determinants of child nutrition and mortality in north-west Uganda. Bull World Health Organ 1992;70:637–43. [PMC free article] [PubMed] [Google Scholar]
- 20. Kikafunda JK, Walker AF, Collett D, et al. Risk factors for early childhood malnutrition in Uganda. Pediatrics 1998;102:e45. 10.1542/peds.102.4.e45 [DOI] [PubMed] [Google Scholar]
- 21. Delpeuch F, Traissac P, Martin-Prével Y, et al. Economic crisis and malnutrition: socioeconomic determinants of anthropometric status of preschool children and their mothers in an African urban area. Public Health Nutr 2000;3:39–47. 10.1017/S1368980000000069 [DOI] [PubMed] [Google Scholar]
- 22. Mozumder AB, Barkat-E-Khuda , Kane TT, et al. The effect of birth interval on malnutrition in Bangladeshi infants and young children. J Biosoc Sci 2000;32:289–300. 10.1017/S0021932000002893 [DOI] [PubMed] [Google Scholar]
- 23. Sakisaka K, Wakai S, Kuroiwa C, et al. Nutritional status and associated factors in children aged 0-23 months in Granada, Nicaragua. Public Health 2006;120:400–11. 10.1016/j.puhe.2005.10.018 [DOI] [PubMed] [Google Scholar]
- 24. Martorell R, Leslie J, Moock PR. Characteristics and determinants of child nutritional status in Nepal. Am J Clin Nutr 1984;39:74–86. 10.1093/ajcn/39.1.74 [DOI] [PubMed] [Google Scholar]
- 25. Chowdhury MRK, Rahman MS, Khan MMH, et al. Risk factors for child malnutrition in Bangladesh: a multilevel analysis of a nationwide population-based survey. J Pediatr 2016;172:194–201. 10.1016/j.jpeds.2016.01.023 [DOI] [PubMed] [Google Scholar]
- 26. Aiga H, Abe K, Andrianome VN, et al. Risk factors for malnutrition among school-aged children: a cross-sectional study in rural Madagascar. BMC Public Health 2019;19:773. 10.1186/s12889-019-7013-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. National Institute of Statistics (NIS) Mozambique population and housing census dataset. Maputo: NIS, 2017. [Google Scholar]
- 28. Anderson J. Mozambique - CGAP Smallholder Household Survey 2015, Building the evidence base on the agricultural and financial lives of smallholder households. Washington DC: World Bank, 2018. Available: https://microdata.worldbank.org/index.php/catalog/2556 [Accessed 5 Nov 2020].
- 29. Thorne CJ, Roberts LM, Edwards DR, et al. Anaemia and malnutrition in children aged 0-59 months on the Bijagós Archipelago, Guinea-Bissau, West Africa: a cross-sectional, population-based study. Paediatr Int Child Health 2013;33:151–60. 10.1179/2046905513Y.0000000060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nkurunziza S, Meessen B, Van Geertruyden J-P, et al. Determinants of stunting and severe stunting among Burundian children aged 6-23 months: evidence from a national cross-sectional household survey, 2014. BMC Pediatr 2017;17:176. 10.1186/s12887-017-0929-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Blaney S, Menasria L, Main B, et al. Determinants of undernutrition among young children living in Soth Nikum district, Siem Reap, Cambodia. Nutrients 2019;11:685. 10.3390/nu11030685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ghosh S, Spielman K, Kershaw M, et al. Nutrition-specific and nutrition-sensitive factors associated with mid-upper arm circumference as a measure of nutritional status in pregnant Ethiopian women: implications for programming in the first 1000 days. PLoS One 2019;14:e0214358. 10.1371/journal.pone.0214358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. World Health Organization (WHO) WHO anthro survey analyser – quick guide. Geneva: WHO, 2019. https://www.who.int/nutgrowthdb/about/06062019_Anthro_QuickGuide.pdf?ua=1 [Google Scholar]
- 34. World Health Organization (WHO), United Nations Children’s Fund (UNICEF) WHO child growth standards and the identification of severe acute malnutrition in infants and children. Geneva: WHO, 2009. https://apps.who.int/iris/bitstream/handle/10665/44129/9789241598163_eng.pdf?ua=1 [PubMed] [Google Scholar]
- 35. Rutstein SO, Johnson K. The DHS Wealth Index - DHS Comparative Reports No. 6. Calverton MD: ORC Macro, 2004. https://dhsprogram.com/pubs/pdf/CR6/CR6.pdf (accessed November 5, 2020). [Google Scholar]
- 36. Food and Agriculture Organization of the United Nations (FAO) Guidelines for measuring household and individual dietary diversity. Rome: FAO, 2010. http://www.fao.org/3/i1983e/i1983e00.pdf [Google Scholar]
- 37. World Health Organization (WHO) Indicators for assessing infant and young child feeding practices Part 1 definitions. Geneva: WHO, 2010. https://apps.who.int/iris/bitstream/handle/10665/43895/9789241596664_eng.pdf;jsessionid=EF4E25E3BECC1BA11B78538196B0B375?sequence=1 [Google Scholar]
- 38. World Health Organization (WHO) Burning opportunity: clean household energy for health, sustainable development, and wellbeing of women and children. Geneva: WHO, 2016. https://apps.who.int/iris/bitstream/handle/10665/204717/9789241565233_eng.pdf?sequence=1&isAllowed=y [Google Scholar]
- 39. Malla S, Timilsina GR. Household cooking fuel choice and adoption of improved cookstoves in developing countries. Washington DC: World Bank, 2014. http://documents1.worldbank.org/curated/en/542071468331032496/pdf/WPS6903.pdf [Google Scholar]
- 40. Ministry of justice (MoJ), birth certificate form. Maputo: MoJ; 2017 (in Portuguese). Available: https://data.unicef.org/crvs/mozambique/ [Accessed 5 Nov 2020].
- 41. World Health Organization (WHO) Childhood stunting: challenges and opportunities - Report of a webcast colloquium on the operational issues around setting and implementing national stunting reduction agendas. Geneva: WHO, 2014. https://apps.who.int/iris/bitstream/handle/10665/107026/WHO_NMH_?sequence=1 [Google Scholar]
- 42. Kumar D, Goel NK, Mittal PC, et al. Influence of infant-feeding practices on nutritional status of under-five children. Indian J Pediatr 2006;73:417–21. 10.1007/BF02758565 [DOI] [PubMed] [Google Scholar]
- 43. Meshram II, Arlappa N, Balakrishna N, et al. Trends in the prevalence of undernutrition, nutrient and food intake and predictors of undernutrition among under five year tribal children in India. Asia Pac J Clin Nutr 2012;21:568–76. [PubMed] [Google Scholar]
- 44. Dhami MV, Ogbo FA, Osuagwu UL, et al. Stunting and severe stunting among infants in India: the role of delayed introduction of complementary foods and community and household factors. Glob Health Action 2019;12:1638020. 10.1080/16549716.2019.1638020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Issaka A, Agho K, Page A, et al. Factors associated with early introduction of formula and/or solid, semi-solid or soft foods in seven Francophone West African countries. Nutrients 2015;7:948–69. 10.3390/nu7020948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Checkley W, Buckley G, Gilman RH, et al. Multi-country analysis of the effects of diarrhoea on childhood stunting. Int J Epidemiol 2008;37:816–30. 10.1093/ije/dyn099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kinyoki DK, Manda SO, Moloney GM, et al. Modelling the Ecological Comorbidity of Acute Respiratory Infection, Diarrhoea and Stunting among Children Under the Age of 5 Years in Somalia. Int Stat Rev 2017;85:164–76. 10.1111/insr.12206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hewlett BS, Lamb ME, Shannon D, et al. Culture and early infancy among central African foragers and farmers. Dev Psychol 1998;34:653–61. 10.1037/0012-1649.34.4.653 [DOI] [PubMed] [Google Scholar]
- 49. Konner M. Hunter-gatherer infancy and childhood: The! Kung and others. In Hunter-Gatherer Childhoods. Routledge: Oxford, 2017. [Google Scholar]
- 50. Little E, Legare C, Carver L. Mother–Infant physical contact predicts responsive feeding among U.S. breastfeeding mothers. Nutrients 2018;10:1251 10.3390/nu10091251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Trevathan WR, McKenna JJ. Evolutionary environments of human birth and infancy: insights to apply to contemporary life. Child Environ 1994;11:88–104. [Google Scholar]
- 52. Waynforth D. Mother-Infant co-sleeping and maternally reported infant breathing distress in the UK millennium cohort. Int J Environ Res Public Health 2020;17:2985. 10.3390/ijerph17092985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. World Health Organization (WHO) WHO recommendations on home-based records for maternal, newborn and child health. Geneva: WHO, 2018. https://www.who.int/publications/i/item/who-recommendations-on-home-based-records-for-maternal-newborn-and-child-health [PubMed] [Google Scholar]
- 54. Iannotti LL, Lutter CK, Stewart CP, et al. Eggs in early complementary feeding and child growth: a randomized controlled trial. Pediatrics 2017;140:e20163459. 10.1542/peds.2016-3459 [DOI] [PubMed] [Google Scholar]
- 55. Bah E, Gajigo O. Improving the poultry value chain in Mozambique, working paper series N° 309. Abidjan: African Development Bank, 2019. https://pdfs.semanticscholar.org/fb5c/e581c93750bae799246a37738cebd36285e6.pdf [Google Scholar]
- 56. Jackson S, Mathews KH, Pulanić D, et al. Risk factors for severe acute lower respiratory infections in children: a systematic review and meta-analysis. Croat Med J 2013;54:110–21. 10.3325/cmj.2013.54.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Mwaniki EW, Makokha AN. Nutrition status and associated factors among children in public primary schools in Dagoretti, Nairobi, Kenya. Afr Health Sci 2013;13:39–46. 10.4314/ahs.v13i1.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Nalwanga D, Musiime V, Kizito S, et al. Mortality among children under five years admitted for routine care of severe acute malnutrition: a prospective cohort study from Kampala, Uganda. BMC Pediatr 2020;20:182. 10.1186/s12887-020-02094-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Food and Agriculture Organization of the United Nations (FAO) Crop calendar. Rome: FAO, 2020. http://www.fao.org/agriculture/seed/cropcalendar/ [Google Scholar]
- 60. Rahman MS, Mushfiquee M, Masud MS H. Association between malnutrition and anemia in under-five children and women of reproductive age: Evidence from Bangladesh demographic and health survey 2011. PLoS One 2019;14:e0219170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Scale-Up Nutrition (SUN) Monitoring, evaluation, accountability, learning (meal) document list – document B: Lists of indicators and data sources. Geneva: SUN, 2018. http://scalingupnutrition.org/wp-content/uploads/2018/03/MEAL-Results-Framework-and-Indicator-Lists-EN_MARCH2018.pdf [Google Scholar]
- 62. Scale-Up Nutrition (SUN) Monitoring, evaluation, accountability, learning (meal) sun countries dashboard. Geneva: SUN, 2019. https://scalingupnutrition.org/progress-impact/monitoring-evaluation-accountability-and-learning-meal/ [Google Scholar]