Abstract
Background
The COVID-19 is a global public health emergency resulting in lockdowns, associated diet and lifestyle changes and constrained public health delivery.
Objective
To investigate the impacts of the COVID-19-induced lockdown in Zimbabwe on nutrition, physical activity, alcohol consumption and smoking among Zimbabwean population aged ≥18 years.
Methods
A cross-sectional online survey was conducted using a structured questionnaire to collect information on demographics (age, gender, place of residence, current employment), food system dimensions, diet and physical activity patterns, stress and anxiety, body image perceptions, lifestyle behaviours like smoking, alcohol intake, screen time and ease of access to health services.
Results
The participants (n=507) were mostly women (63.0%) between the ages of 31 and 40 years (48.1%) and had tertiary education (91.3%). The lockdown resulted in increase in food prices (94.8%) and decrease in availability of nutritious foods (64%). Most (62.5%) of the participants reported a reduction in their physical activity levels. The prevalence of generalised anxiety disorder (GAD) was 40.4% and mostly affecting woman (63.5%, p=0.909), 31–40 years age group (49.6%, p=0.886). Based on the Body Mass Index-based Silhouette Matching Test (BMI-SMT) 44.5% gained weight, 24.3% lost weight and 31.2% did not have weight change. The paired samples t-test showed that there was a significant increase in perceived body weight (p<0.001). More than half (59.6%) reported having difficulties accessing medicinal drugs and 37.8% growth monitoring services.
Conclusions
The lockdown period was associated with increase in food prices, decrease in dietary diversification, elevated GAD symptoms, disrupted diet and consumption patterns. There were low levels of physical activity and perceived weight gained during the lockdown period, thus increasing the risk of overweight and obesity. Further studies incorporating participants of different socioeconomic status are warranted to get more conclusive results.
Keywords: nutrition assessment, malnutrition, mental health, dietary patterns
What this paper adds?
First diet and lifestyle survey in Zimbabwe documenting the impact of COVID-19 initiated lockdown on diet and lifestyles of the urban elite.
The COVID-19-induced lockdown was associated with elevated anxiety, disruptions of food supply chains and consumption patterns.
Most of the participants were less active and gained weight in the lockdown period, thus increasing the risk of overweight and obesity an emerging risk factor for severe COVID-19 complications.
Introduction
The WHO on 11 March 2020 declared the outbreak of the COVID-19 a global pandemic.1 The pandemic started in Wuhan, China, in late December 2019, and has spread globally.2 The WHO situation report 113 reported that as of 12 May 2020, globally, there were 4 088 848 cases and 283 153 deaths due to COVID-19.3 The situation report also showed that the highest cases were in the Americas (1 743 717) and Europe (1 755 790), while Africa had the lowest (46 829).
In order to contain the spread of the virus, national lockdowns characterised by restricted movement and social distancing ‘Staying at Home’ have been the order of the day in many countries.4 5 In Zimbabwe, the government declared a state of national disaster in response to the COVID-19 pandemic on Friday, 27 March 2020, this was followed by a nationwide lockdown on March 30.6 Unfortunately, this has also led to increased vulnerability to food insecurity especially among the urban poor and increased risk of overweight and obesity in the higher income classes.7 This is worrying considering that obesity is a risk factor for severe COVID-19 infection complications.8
Therefore, maintaining healthy body weight and consumption of diverse and nutritious diet is recommended to mitigate COVID-19 infection via the immune boosting mechanism.9 10 Individuals who eat a well-balanced diet tend to be healthier with lower risk of obesity and associated complications. In addition, they will have stronger immune systems and reduced risk of contracting infectious diseases like COVID-19.11 12
Although, the lockdown restrictions have their benefits in ‘flattening the curve’, they also have potential downsides such as increased stress, reduced physical activity, limited availability and access to diverse nutritious foods and health services.13 14 In addition, lockdown-related stress and anxiety has potential to trigger compensatory hyperphagia ‘carbohydrate cravings’ resulting in increased energy intake, thus giving rise to a dangerous vicious cycle.11 15 Unfortunately, this food craving is often associated with the increased risk of developing obesity and cardiovascular diseases and has also been linked with increased risk of more serious complications of COVID-19.16 17
The COVID-19-induced lockdowns are normally characterised with restricted movements and disrupted food supply and accessibility in most settings. Specifically, the COVID-19 control measures and travel restrictions may compromise the ability to maintain physical activity and healthy lifestyles including reduced consumption of diverse and nutritious diets. Although not clearly understood, this can have implications on health and nutrition outcomes. Therefore, this study was designed to investigate the impacts of the COVID-19-induced lockdown in Zimbabwe on nutrition, physical activity and lifestyle patterns among adults in Zimbabwe.
Methods
Study design, setting and participants
The nationwide descriptive cross-sectional study was carried out by a nutrition team from the University of Zimbabwe, using a web-survey (SurveyMonkey, California, USA), from 11 to 25 May 2020. A short online questionnaire was administered with mostly multiple-choice questions and some open-ended questions to capture additional observations. This was a rapid appraisal of the perceptions of adults aged 18 years and above (n=507) regarding the effect of COVID-19 induced lockdown on nutrition, health and lifestyle indicators in the 10 provinces of Zimbabwe. The survey link was disseminated through institutional and private social networks (WhatsApp, Twitter, Facebook) and institutional mailing lists.
Data collection and tools
A self-administered online questionnaire was developed to collect data on demographics, socioeconomic factors and to explore the impact of COVID-19-induced lockdown restrictions on food system dimensions, diet and physical activity patterns, stress and anxiety, body image perceptions, lifestyle behaviours like smoking, alcohol intake, screen time (TV/ tablet/phone/laptop) and ease of access to health services. The survey was carried out using SurveyMonkey online platform; http://www.surveymonkey.com/, which was accessible through any device with internet connection. The survey was disseminated through partner organisations’ mailing lists, institutional and private social media networks (WhatsApp, Twitter, Facebook and LinkedIn).
Physical activity and lifestyle changes
The perceptions of participants on the impact of COVID-19 on physical activity, screen time, smoking and alcohol consumption were assessed by asking the question: What do you perceive as the impact of the COVID-19 induced lockdown on your physical activity/screen time (TV/tablet/phone/laptop)/smoking/alcohol consumption? The responses were coded as follows: 1=less/decreased, 2=same/did not change, 3=more/increased and 4=not applicable.
Lockdown and food access
In the context of this study, food referred to basic everyday foods that households buy from retail outlets and supermarkets. Foods from the basic food groups also known as ‘everyday foods’ provide the nutrients essential for life and growth. Regarding food prices, we were interested in the generic and broader perceptions of participants on the impact of COVID-19 lockdown on prices of basic everyday foods. This is important considering that food price hikes can have a strong impact on food affordability, hunger and undernourishment and dietary diversification.
Diversified diets
The online questionnaire had the following questions to assess the perceptions of participants regarding the impact of lockdown on their consumption patterns. (1) Has your diet or consumption patterns changed in the last 4 weeks of lockdown? The next set of questions assessed the impact of the COVID-19-induced lockdown (past 4 weeks) on the usual consumption of the following food groups selected based on the Food and Agriculture Organisation (FAO) food groups for assessing household and individual dietary diversity;18 dark green leafy vegetables, other vitamin A-rich fruits and vegetables, other vegetables, other fruits, meat and meat groups, cereal breads and tubers, pulses, legumes, nuts and seeds, dairy products, eggs.19 The responses specific to each food group were coded as follows: 1=less/decreased, 2=same/did not change, 3=more/increased and 4=not applicable.
Generalised anxiety disorder
We used the validated Generalised Anxiety Disorder-7 (GAD-7) scale to assess respondent’s anxiety symptoms.20 Seven questions assessed the frequency of anxiety symptoms over the past 2 weeks on a 4-point Likert scale ranging from 0 (never) to 3 (nearly every day) and the total score of GAD-7 ranged from 0 to 21, with increasing scores indicating more severe functional impairments as a result of anxiety.20 We adopted the cut-off (GAD total score of >9 points) previously used to define the presence of anxiety symptoms.21
Body image perceptions
The perceptions of before lockdown and current body images (4 weeks later) of the participants were assessed using the nine figural BMI-SMT.22 The silhouettes are ranked from the thinnest to the heaviest body size and responses are recorded on a scale from 1 (thinnest) to 9 (heaviest). The Silhouette test was validated for use in populations of African descent.22 23 To assess respondents perceived ideal body size, participants were asked to select a matching figure that best represents how they looked like before the lockdown and how they were looking like the time of the interview. The BMI-SMT silhouette figures are equal in height and increase proportionally in size and are gender specific. In addition, the BMI-SMT provides a reliable and pragmatic method for quantifying body-image perceptions.22
Data analysis
Data collected were entered and analysed using SPSS V.20 (IBM, Armonk, New York, USA). The Shapiro-Wilk test and data visualisations via Q–Q plots were used to test for normality of data. Continuous data were presented as mean±SD, while categorical data were presented as frequencies and percentages. Pearson’s χ2 and Pearson correlation coefficient was used to explore associations for categorical variables and continuous variables, respectively. Paired samples t-test was used to test for difference in means across continuous normally distributed variables. Level of significance was set at p<0.05.
Results
Characteristics of the participants
On 25 May 2020, the online survey was stopped, and the collected data were analysed based on the Helsinki ethical guidelines 24. In total, 507 participants took part in the survey after 2 declined to participate. Most of the participants were between the ages of 31 and 40 years and were women (63.0%) and had tertiary education (91.3%). Most of the participants were employed in the formal sector (73.9%), and most were from Harare (60.5%). Almost all the participants (95.5%) said they did not receive government assistance during the lockdown period. Of those who did receive some form of assistance, 2.5% received food handouts and 2% received financial assistance (table 1).
Table 1.
Sociodemographic characteristics of the participants
| Variable | n | % |
| Age category (years) | ||
| 18–30 | 117 | 26.0 |
| 31–40 | 216 | 48.1 |
| 41–49 | 69 | 15.4 |
| 50+ | 47 | 10.5 |
| Gender | ||
| Male | 166 | 37.0 |
| Female | 283 | 63.0 |
| Highest education level attained | ||
| No formal education | 2 | 0.4 |
| Primary (approximately 7 years) | 0 | 0.0 |
| O’ level (approximately 11 years) | 26 | 5.8 |
| A’ level (approximately 13 years) | 11 | 2.5 |
| Tertiary (colleges, polytechnic and university) | 410 | 91.3 |
| Employment status | ||
| Not employed | 37 | 8.2 |
| Informal sector | 51 | 11.4 |
| Formal sector | 332 | 73.9 |
| Students | 29 | 6.5 |
| Residence | ||
| Urban province | 328 | 73.1 |
| Rural province | 121 | 26.9 |
| Lockdown support from government, NGOs, religious groups and or private sector | ||
| Yes | 20 | 4.4 |
| No | 429 | 95.6 |
| If yes, specify: | ||
| Financial assistance | 9 | 2.0 |
| Food handouts | 11 | 2.5 |
| Grocery voucher | 1 | 0.2 |
| Not applicable | 428 | 95.3 |
| Number of people staying at home, median and IQR | 4 (3:6) |
NGOs, non-governmental organisations.
Lockdown and food access
Figure 1 shows that the lockdown resulted in glaring increases in food prices. This was reported by 94.8% of the study participants. In addition, 64% reported a decrease in availability of diverse and nutritious foods, while 43.9% mentioned that the quality of foods sold in their areas had decreased. These results show a disturbing picture where food security of most households appears to be compromised due to extortionate prices, availability of less nutritious food choices with poor quality (possible safety concerns as well).
Figure 1.
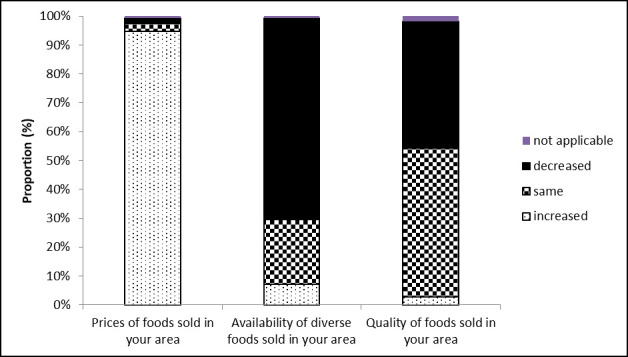
Effect of COVID-19-induced lockdown on food prices, availability and diversity (n=438).
Implications of lockdown on dietary diversity
The results show that 96.6% (n=490) of the participants reported that their diet and consumption patterns have changed during the COVID-19-induced lockdown. Concerning individual food groups, 57.8% of the participants stated that there was a decrease in consumption of ‘other vitamin A-rich fruits and vegetables’ (figure 2). There was also a decrease in the intake of ‘other vegetables’ (48.5%), ‘other fruits’ (64.9%), ‘nuts and seeds’ (45.0%), ‘cereals breads and tubers’ (41.1%) and ‘dairy products’ (44.9%). Interestingly, we observed an increase in consumption of ‘dark green leafy vegetables’ (33.72%). However, ‘egg’ consumption largely remained the same (41.8%) as well as ‘meat and meat group’ (46.2%). The reported consumption patterns are reflective of a disrupted food system and prevailing food access restrictions during the lockdown. Overall, there appears to be a trend where consumption of nutritious foods was reduced, while alcohol consumption was high.
Figure 2.
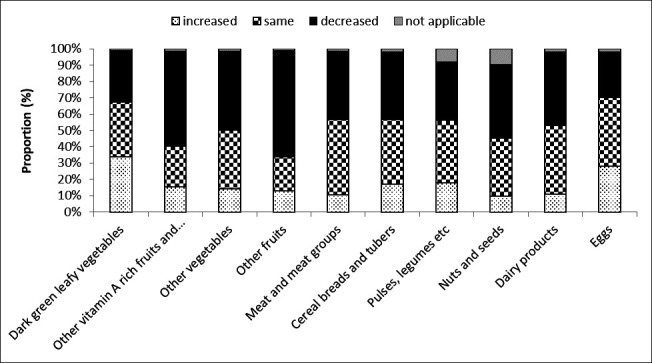
Effect of COVID-19-induced lockdown on consumption of various food groups (n=427).
Lifestyle-related habits change during the COVID-19-induced lockdown
Figure 3 shows that most (76.4%) of the participants reported to having increased stress and anxiety, while 89.1% reported increased screen time spent on TV/tablet/cell phone/laptop and 62.5% indicated that the lockdown resulted in reduction in their physical activity levels (62.9%). Surprisingly a relatively high proportion (46.7%) of the participants indicated that their alcohol consumption increased during the lockdown period. In addition, the participants also reported an increase in smoking (45.9%). The results show a disturbing trend of decreased physical activity, increased time spent on sedentary activities and relatively high proportion of participants who reported increase in alcohol intake and smoking.
Figure 3.
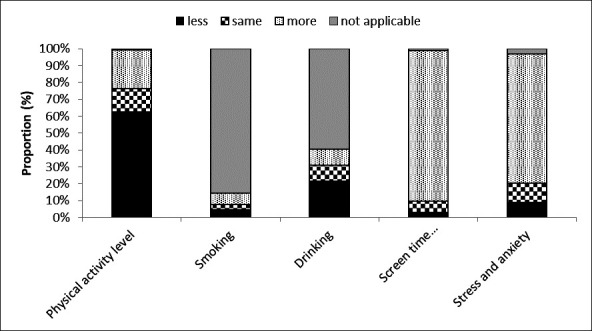
Physical activity and selected lifestyle indicators during the lockdown (n=421).
GAD and COVID-19
Concerning stress and anxiety, participants mostly reported that they were psychologically affected by the COVID-19 pandemic and associated lockdown restrictions (figure 4). Specifically, 97.1% of the respondents testified that COVID-19 pandemic and lockdown restrictions had increased their stress and anxiety levels.
Figure 4.
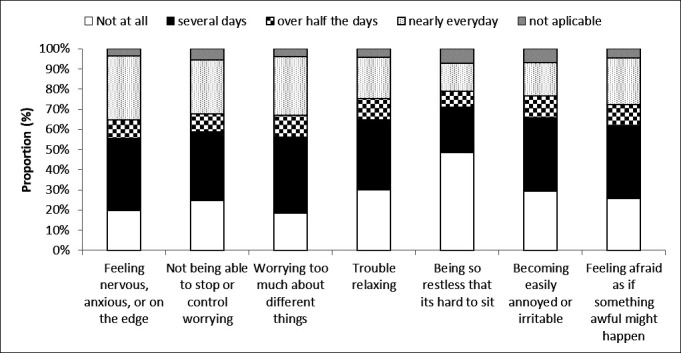
Stress and anxiety during COVID-19-induced lockdown (n=409).
The prevalence of GAD in this study was 40.4% and mostly affected women (63.5%, p=0.909), 31–40 years age group (49.6%, p=0.886) (table 2). The Cronbach’s alpha for the GAD scale in our study was 0.926, which indicates a high level of internal consistency for our scale with this study population. There was a significantly large level of physical inactivity among respondents and participants with GAD symptoms (71.5%, p=0.030). Majority of the respondents with GAD symptoms indicated that smoking increased (55.2%, p=0.133), screen time spent on TV, laptop, phone (92.5%, p=0.062) also increased among participants with GAD symptoms. Although alcohol intake decreased (54%), we observed a non-significant association between GAD and alcohol intake in this study (p=0.898).
Table 2.
GAD and selected participant characteristics
| Variable | Total n (%) |
GAD symptoms n (%) |
P value* | |
| No | Yes | |||
| Age category, years | ||||
| 18–30 | 91 (26.8) | 52 (25.7) | 39 (28.5) | 0.886 |
| 31–40 | 167 (49.3) | 99 (49.0) | 68 (49.6) | |
| 41–49 | 47 (13.9) | 30 (14.9) | 17 (12.4) | |
| 50+ | 34 (10.0) | 21 (10.4) | 13 (9.5) | |
| Sex | ||||
| Male | 126 (37.2) | 76 (37.6) | 50 (36.5) | 0.909 |
| Female | 213 (62.8) | 126 (62.4) | 87 (63.5) | |
| Highest education level attained | ||||
| Primary and below | 16 (4.7) | 8 (4.0) | 8 (5.8) | 0.718 |
| O and A levels | 9 (2.7) | 5 (2.5) | 4 (2.9) | |
| Tertiary | 314 (92.6) | 189 (93.6) | 125 (91.2) | |
| Employment status | ||||
| Not employed | 29 (8.6) | 18 (8.9) | 11 (8.0) | 0.406 |
| Informal sector | 36 (10.6) | 19 (9.4) | 17 (12.4) | |
| Formal sector | 252 (74.3) | 155 (76.7) | 97 (70.8) | |
| Students | 22 (6.5) | 10 (5.0) | 12 (8.8) | |
| Residence | ||||
| Urban province | 254 (74.9) | 162 (80.2) | 92 (67.2) | 0.007* |
| Rural province | 85 (25.1) | 40 (19.8) | 45 (32.8) | |
| Weight change (pre vs post lockdown) | ||||
| Lost weight | 82 (25.3) | 42 (21.8) | 40 (30.5) | 0.143 |
| Gained weight | 148 (45.7) | 89 (46.1) | 59 (45.0) | |
| Weight did not change | 94 (29.0) | 62 (32.1) | 32 (24.4) | |
*p Value based on Pearson’s χ2 test, *significant at p<0.05.
GAD, generalised anxiety disorder.
The results show that those individuals who exhibited GAD symptoms had reduced intake of vitamin A-rich fruits and vegetables (69.1%, p=0.005), other vegetables (58.8%, p=0.001), other fruits (80.1%, p<0.001), meat and meats (54.9%, p=0.001), cereals, bread and tubers (56.7%, p<0.001), pulses and legumes (55.9%, p<0.001), nuts and seeds (60.8%, p=0.006), milk and dairy (60.3%, p<0.001), eggs (42.2%, p<0.001) compared with their less anxious counterparts.
Body weight and image perceptions
Almost half (48%) thought they had gained weight, while 25.8% and 25.5% thought they had lost weight and weight did not change, respectively. However, based on the nine figural BMI-SMT to determine perceived anthropometry, 44.5% gained weight, 24.3% lost weight and 31.2% did not have weight change. The average size before lockdown was 5.0±1.6 compared with 5.2±1.8 during lockdown. The paired samples t-test showed that there was a significant increase in perceived body size when comparing pre and during lockdown body size (p<0.001). Based on the BMI-SMT, we found that highest perceived weight gain during the lockdown was in the age group 31–40 years (48.9%, p=0.568), women (62.6%, p=0.062), participants with tertiary qualifications (92.5%, p=0.533), formal sector employees (75.3%, p=0.107), and individuals who did not have GAD symptoms (60.1%, p=0.143).
Ease of access to health services
Over half (59.9%) said drugs and medication were not easily available during lockdown compared with 19.8% who said the drugs and medication were still easily available. Over half (58.6%) said doctor’s appointments and review visits were not easily available and 7.97% said appointments and review visits were still easily available. Concerning immunisation and growth monitoring, 37.8% said this service was not easily available compared with 19% who mentioned that the services were still easily available (figure 5).
Figure 5.
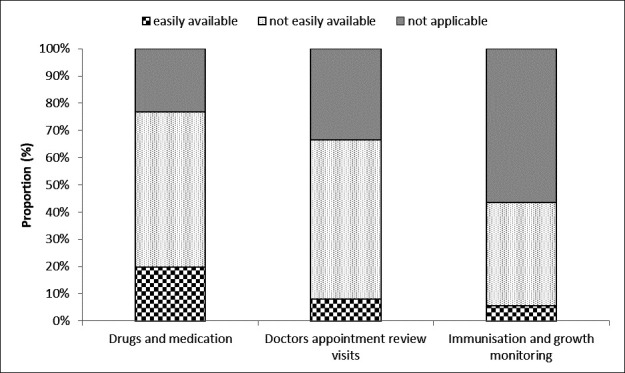
Availability of medication and access to selected health services during lockdown (n=390).
Discussion
In the present study, we provided for the first-time data on the effect of the COVID-19 lockdown on nutrition, anxiety, physical activity and lifestyle patterns in Zimbabwe. However, there are still lots of unknowns concerning the COVID-19 pandemic that is still ongoing, thus, our data need to be confirmed and investigated in future population studies.
The lockdown period (4 weeks) was associated with increases in food prices and decrease in dietary diversification. The increases in food prices are reflective of the negative impact of COVID-19 and lockdowns on agriculture and food supply systems.25 This often results in artificial shortages, inflated prices and compromised food security and access to healthy food options particularly on the vulnerable low-income households. This is disturbing considering the importance of optimum nutrition for well-functioning immune system in these times of COVID-19.26 Therefore, increases in food prices reduce access to diverse and nutritious foods, which ultimately makes it difficult for individuals to maintain thriving immune systems. Healthy diets help to avoid deficiencies of the nutrients that play an essential role in immune cell triggering, interaction, differentiation or functional expression.27 Considering that there is currently no known cure, the Hippocrates 400 BC philosophy of, ‘let thy food be thy medicine, and let medicine be thy food’ is vindicated as consumption of varied and nutritious foods will guarantee a healthy immune system.28
Unfortunately, the current study also showed a disturbing picture of high alcohol consumption (46.7%) and decreased consumption of nutritious foods. It is tempting to speculate that the surge in alcohol use during the early days of the lockdown could have been due to increased stress during this period. There was heightened uncertainty, fear, job losses and loneliness (from social isolation) though this remains to be proven for our communities.29 30 However, a more probable explanation, is the fact that, although bottle stores and night clubs were closed, there was no restriction on the sale of alcohol from supermarkets and liquor outlets in Zimbabwe.31 This is contrary to the very strict no-alcohol policies that were enforced in other countries like South Africa.32 The consumption of less diverse foods during the lockdown period is worrying, considering the role of nutritious foods in boosting immunity.26 28 Furthermore, alcohol consumption is linked with reduce immune function among drinkers33 and risk of getting obese a known risk factor for developing severe COVID-19 symptoms.8 17
The effect of COVID-19 pandemic on nutrition and dietary intake goes beyond the individual and the community to reach national and global levels.27 Therefore, there are crucial policy implications for national governments centred around the need to stop the spread of COVID-19 using lockdowns, and on the other side, the glaring need to prevent and deal with the negative impacts of such policy decisions on food security and livelihoods. According to Siche, the COVID-19 pandemic food demand and thus food security are greatly affected due to mobility restrictions, reduced purchasing power and with a greater impact on the most vulnerable population groups. It remains the responsibility of the governments to create a supportive policy environment to enhance the physical and mental health of individuals in the context of COVID-19 pandemic, without also neglecting the potential risk of ‘lockdown associated obesity’ during lockdowns. Naja and Hamadeh gave recommendations on how to provide nutrition demands in the context of COVID-19 using a multilevel framework for action adapted from the ecological model of health behaviour. There are economic arguments that prolonged lockdown is not sustainable in the long run, as this will lead to economic slump that ultimately creates negative health consequences ‘poverty-infection complex’, which create more non-COVID-19-related deaths than confinement would save from this disease.34 Governments are encouraged to make evidence and informed decisions to ensure responsible lockdown exit strategies.
The COVID-19-induced lockdown has resulted in disruptions in consumption patterns (96.6%) and elevated anxiety levels (40.4%). Regarding the implications of lockdown on diet and consumption patterns, participants reported a reduction in intake of fruits and vegetables except for ‘dark green leafy vegetables’. This decrease is disturbing considering that WHO recommends an average consumption of 400 g of fresh fruits and vegetables per day will boost the immune system. Therefore, the observed increase in consumption of dark leafy vegetables is commendable and reflects the utilisation of home or backyard nutrition gardens that are common in most households in Zimbabwe.35
In this study, the prevalence of GAD was 40.4% and mostly affecting women and the 31–40 years age group. Hence the finding that carbohydrate intake also decreased is surprising, considering that we expected this to increase due to the stress and sugar cravings in stressful lockdown conditions.16 The current findings reveal that among participants with GAD symptoms, there was reduced physical activity and alcohol intake, while an increase in smoking and screen time (TV, laptop and phone). In addition, continuously hearing or reading about the COVID-19 can be stressful and can lead towards overeating, mostly sugary foods ‘comfort foods’.36 A study in China also observed that constantly thinking about COVID-19, particularly among younger people and healthcare workers, increases GAD symptoms and the risk of mental illness.37
With respect to physical activity, we observed that most of the participants were less active and gained weight in the lockdown period, thus increasing the risk of overweight and obesity. The perceived weight gain by participants was higher in women (p=0.062), participants with tertiary qualifications (p=0.533), formal sector employees (p=0.107). These results paint a picture of the dangers of obesity-associated severe COVID-19 complications in typical formally employed persons with a tertiary qualification. Considering that there is growing evidence showing that obesity is a key risk factor in this crisis.8 It is strongly recommended that individuals should increase physical activity levels and reduce the consumption of energy-dense ‘junk’ food that predisposes to weight gain and susceptibility to COVID-19.38 Thus, studies to investigate the impact of consumption of unhealthy diets and low physical activity and anxiety on the susceptibility to COVID-19 and recovery are warranted.
We reported reduction in access to medical doctors (58.6%), drugs (59.9%), immunisations and growth monitoring (37.8%) during the lockdown period. This has negative long-term implications as individuals will develop reluctance to access preventative health services. In addition, disruptions in drug supply chains are likely associated with defaulters on immunisation schedules among children and this may lead to future fatal outbreaks of preventable diseases such as measles polio and diphtheria.39
Limitations
The limitations of online surveys have been extensively discussed in the scientific literature.40 41 However, equally important are papers that raised the importance of collecting useful data on the impacts of COVID-19 on various aspects to inform public policy.37 42 Considering that COVID-19 has lots of unknowns,43 44 online surveys offer perfect opportunities to collect real-time data to monitor and understand the rapidly evolving COVID-19 epidemiology in various settings.45 The main limitation of the current study is that although our survey had respondents from all the 10 provinces of Zimbabwe, online surveys tend to be restricted to individuals with access to internet with potential under representation of people from lower socioeconomic groups and rural settings. However, due to the lockdown travel restrictions, the online survey was the only option to collect this critical dietary and physical activity data. Although the BMI-SMT has its limitations with respect to collective objective anthropometry data, in the current lockdown context, it remains a useful alternative. It is crucial that this rapid assessment went on at the most critical period of the COVID-19 pandemic, to inform programme and policy decisions. Interestingly, evidence is gathering indicating that web-based surveys are equivalent to conventional face to face interviews.46 47 There is growing concern that COVID-19 could deepen food insecurity, malnutrition in Africa. Unfortunately, in our current study, we did not collect data to understand the different food groups and how they are affected by the hike in prices, this may have helped to clearly understand the impact of lockdown on food access and household food security issues.
Conclusions
The lockdown period was associated with increases in food prices and decrease in dietary diversification. In addition, the COVID-19-induced lockdown has resulted in disrupted consumption patterns and elevated GAD symptoms. Participants indicated that their physical activity levels decreased and perceived weight gain in the lockdown period, thus increasing the risk of overweight and obesity. However, there are still lots of unknowns concerning the COVID-19 pandemic, as such future studies incorporating participants of different socioeconomic status are warranted.
Acknowledgments
First, we are very grateful to the respondents for accepting to join our rapid appraisal and for sharing their perspectives and insights into perceived effects of the COVID-19 in their communities. Great thank you to Ms Tavonga Muderedzwa for assistance in setting up the online poll.
Footnotes
Contributors: Conception, design and data collection of study: TMM and PC, data curation: PC. Data analysis and/or interpretation of data: PC and TMM. Drafting the manuscript: TMM. Revising the manuscript critically for important intellectual content: PC. Resources: TMM and PC. All authors read and approved the final manuscript for submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The study was conducted based on the ethical principles of respect, justice and confidentiality summarised in the 2013 Declaration of Helsinki 24. The study obtained ethical clearance from the Medical Research Council of Zimbabwe (MRCZ/B/1920). Electronic informed consent was obtained from all participants prior to completing the survey.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: The anonymised datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. Please email: tmatsungo@gmail.com for data requests.
References
- 1. Ghebreyesus TA. WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020, 2020. Available: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020
- 2. Wang C, Horby PW, Hayden FG, et al. A novel coronavirus outbreak of global health concern. Lancet 2020;395:470–3. 10.1016/S0140-6736(20)30185-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. WHO Coronavirus disease (COVID-19) situation report – 113, 2020. Available: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200512-covid-19-sitrep-113.pdf?sfvrsn=feac3b6d_2
- 4. JC-H YAP. COVID-19 Science Report: Social Distancing & Lockdowns, 2020. Available: 10.25540/vcvz-yg51 [DOI]
- 5. Sarwal R, Sarwal T. Mitigating COVID-19 with Lockdowns: a possible exit strategy, 2020. Available: 10.2139/ssrn.3563538 [Accessed 29 Mar 2020]. [DOI]
- 6. Herald Breaking: 21 days lockdown to start Monday, 2020. Available: https://www.herald.co.zw/breaking-21-days-lockdown-to-start-monday/
- 7. Rundle AG, Park Y, Herbstman JB, et al. COVID-19-Related school Closings and risk of weight gain among children. Obesity 2020;28:1008–9. 10.1002/oby.22813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sattar N, McInnes IB, McMurray JJV. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation 2020;142:4–6. 10.1161/CIRCULATIONAHA.120.047659 [DOI] [PubMed] [Google Scholar]
- 9. WHO Nutrition advice for adults during the COVID-19 outbreak, 2020. Available: http://www.emro.who.int/nutrition/nutrition-infocus/nutrition-advice-for-adults-during-the-covid-19-outbreak.html
- 10. Restrepo M. Health status and the role of nutrition on SARS-CoV/Covid-19, 2020. Available: https://nakedfoodmagazine.com/health-status-covid-19/
- 11. Muscogiuri G, Barrea L, Savastano S, et al. Nutritional recommendations for CoVID-19 quarantine. Eur J Clin Nutr 2020;74:850–1. 10.1038/s41430-020-0635-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shi Y, Wang Y, Shao C, et al. COVID-19 infection: the perspectives on immune responses. Cell Death Differ 2020;27:1451–4. 10.1038/s41418-020-0530-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hobbs JE. Food supply chains during the COVID‐19 pandemic. Canadian Journal of Agricultural Economics/Revue canadienne d'agroeconomie 2020;68:171–6. 10.1111/cjag.12237 [DOI] [Google Scholar]
- 14. Galanakis CM. The food systems in the era of the coronavirus (COVID-19) pandemic crisis. Foods 2020;9:523. 10.3390/foods9040523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Razzoli M, Pearson C, Crow S, et al. Stress, overeating, and obesity: insights from human studies and preclinical models. Neurosci Biobehav Rev 2017;76:154–62. 10.1016/j.neubiorev.2017.01.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020;180:934–43. 10.1001/jamainternmed.2020.0994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Muscogiuri G, Pugliese G, Barrea L, et al. Commentary: Obesity: The “Achilles heel” for COVID-19? Metabolism 2020;108:154251 10.1016/j.metabol.2020.154251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kennedy G, Ballard T, Dop M. FAO guidelines for measuring household and individual dietary diversity, 2013. Available: http://www.fao.org/3/i1983e/i1983e00.htm
- 19. Swindale A, Bilinsky P. Household dietary diversity score (HDDS) for measurement of household food access: indicator guide. Washington, DC: Food and Nutrition Technical Assistance III Project (FANTA); 2006. https://www.fantaproject.org/monitoring-and-evaluation/household-dietary-diversity-score [Google Scholar]
- 20. Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 21. Wang Y, Chen R. Reliability and validity of generalized anxiety scale-7 in inpatients in Chinese General Hospital. J Clin Psychiatr 2018;28:168–71. [Google Scholar]
- 22. Pulvers KM, Lee RE, Kaur H, et al. Development of a culturally relevant body image instrument among urban African Americans. Obes Res 2004;12:1641–51. 10.1038/oby.2004.204 [DOI] [PubMed] [Google Scholar]
- 23. Yepes M, Viswanathan B, Bovet P, et al. Validity of silhouette showcards as a measure of body size and obesity in a population in the African region: a practical research tool for general-purpose surveys. Popul Health Metr 2015;13:35. 10.1186/s12963-015-0069-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. WMA WMA Declaration of Helsinki-Ethical principles for medical research involving human subjects, 2013. Available: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ [PubMed]
- 25. Siche R. What is the impact of COVID-19 disease on agriculture? Sci. agropecu 2020;11:3–6. 10.17268/sci.agropecu.2020.01.00 [DOI] [Google Scholar]
- 26. Butler MJ, Barrientos RM. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav Immun 2020;87:53–4. 10.1016/j.bbi.2020.04.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Naja F, Hamadeh R. Nutrition amid the COVID-19 pandemic: a multi-level framework for action. Eur J Clin Nutr 2020;74:1117–21. 10.1038/s41430-020-0634-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jayawardena R, Sooriyaarachchi P, Chourdakis M, et al. Enhancing immunity in viral infections, with special emphasis on COVID-19: a review. Diabetes Metab Syndr 2020;14:367–82. 10.1016/j.dsx.2020.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kim JU, Majid A, Judge R, et al. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. Lancet Gastroenterol Hepatol 2020. 10.1016/S2468-1253(20)30251-X. [Epub ahead of print: 04 Aug 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Da BL, Im GY, Schiano TD. COVID-19 hangover: a rising tide of alcohol use disorder and Alcohol-Associated liver disease. Hepatology 2020. 10.1002/hep.31307. [Epub ahead of print: 05 May 2020]. [DOI] [PubMed] [Google Scholar]
- 31. Bhebhe N. Covid-19 lockdown: president Mnangagwa advised to ban alcohol sales. Harare, Zimbabwe: My Zimbabwe News, 2020. [Google Scholar]
- 32. Matzopoulos R, Walls H, Cook S, et al. South Africa's COVID-19 alcohol sales ban: the potential for better policy-making. Int J Health Policy Manag 2020. 10.34172/ijhpm.2020.93. [Epub ahead of print: 10 Jun 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hamer M, Kivimäki M, Gale CR, et al. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK. Brain Behav Immun 2020;87:184–7. 10.1016/j.bbi.2020.05.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gilbert M, Dewatripont M, Muraille E, et al. Preparing for a responsible lockdown exit strategy. Nat Med 2020;26:643–4. 10.1038/s41591-020-0871-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mutambara J, Satambara T, Masvongo J. Impacts of nutritional gardens on health of communal households; a case study of Nyanga North district. GJAS 2013;3:579–84. 10.15580/GJAS.2013.3.062013681 [DOI] [Google Scholar]
- 36. Yılmaz C, Gökmen V. Neuroactive compounds in foods: occurrence, mechanism and potential health effects. Food Res Int 2020;128:108744. 10.1016/j.foodres.2019.108744 [DOI] [PubMed] [Google Scholar]
- 37. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 2020;288:112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. De Lorenzo A, Romano L, Di Renzo L, et al. Obesity: a preventable, treatable, but relapsing disease. Nutrition 2020;71:110615. 10.1016/j.nut.2019.110615 [DOI] [PubMed] [Google Scholar]
- 39. Nelson R. COVID-19 disrupts vaccine delivery. Lancet Infect Dis 2020;20:546. 10.1016/S1473-3099(20)30304-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nayak MSDP, Narayan KA. Strengths and weakness of online surveys. J Empir Res Hum Res Ethics 2009;4:37–48. [Google Scholar]
- 41. Buchanan EA, Hvizdak EE. Online survey tools: ethical and methodological concerns of human research ethics committees. J Empir Res Hum Res Ethics 2009;4:37–48. 10.1525/jer.2009.4.2.37 [DOI] [PubMed] [Google Scholar]
- 42. Betsch C. How behavioural science data helps mitigate the COVID-19 crisis. Nat Hum Behav 2020;4:438. 10.1038/s41562-020-0866-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Anguelov R, Banasiak J, Bright C, et al. The big unknown: the asymptomatic spread of COVID-19. Biomath 2020;9:2005103 10.11145/j.biomath.2020.05.103 [DOI] [Google Scholar]
- 44. Grech V. Unknown unknowns - COVID-19 and potential global mortality. Early Hum Dev 2020;144:105026. 10.1016/j.earlhumdev.2020.105026 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 45. Geldsetzer P. Use of rapid online surveys to assess people's perceptions during infectious disease outbreaks: a cross-sectional survey on COVID-19. J Med Internet Res 2020;22:e18790. 10.2196/18790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. van Gelder MMHJ, Bretveld RW, Roeleveld N. Web-Based questionnaires: the future in epidemiology? Am J Epidemiol 2010;172:1292–8. 10.1093/aje/kwq291 [DOI] [PubMed] [Google Scholar]
- 47. Ekman A, Dickman PW, Klint Å, et al. Feasibility of using web-based questionnaires in large population-based epidemiological studies. Eur J Epidemiol 2006;21:103–11. 10.1007/s10654-005-6030-4 [DOI] [PubMed] [Google Scholar]


