Abstract
Background:
Literature describing the anatomic characteristics of osteochondral fractures (OCFs) in the knee joint after patellar dislocation is scarce.
Purpose:
To describe the patterns of OCFs in the knee joint after acute or recurrent patellar dislocation in a sample of patients from 2 orthopaedic trauma centers.
Study Design:
Case series; Level of evidence, 4.
Methods:
In this multicenter study, all patients who had International Classification of Diseases, 10th Revision, diagnostic codes S83.0 and M22.0 between 2012 and 2018 were screened. Of the 2181 patients with clinically diagnosed patellar dislocation, 1189 had undergone magnetic resonance imaging (MRI). Patients with diagnosed patellar dislocation and osteochondral fragment verified on MRI scans were included. Demographic and clinical data were collected from electronic patient records. OCF location and size were assessed from MRI scans. Results were further compared in subgroups by sex, skeletal maturity, and primary versus recurrent patellar dislocation.
Results:
An OCF was detected in 134 patients with injured knees, all of whom were included in the final analysis. It occurred in the patella in 63% of patients, in the lateral femoral condyle in 34%, and in both locations in 3%. The median OCF size was 146 mm2 (interquartile range, 105-262 mm2). There was no statistically significant difference in OCF size between patellar and lateral femoral condyle fractures. Patellar OCFs were more frequent in female than male patients (P = .009) and were larger after primary than recurrent dislocation (P = .040).
Conclusion:
OCFs were mainly located in the medial facet of the patella and in the lateral femoral condyle, with these locations accounting for approximately two-thirds and one-third of all OCFs, respectively. Proportion of patellar OCF was higher in female than in male. Patellar OCFs may be larger after primary than recurrent dislocation.
Keywords: osteochondral fracture, patellar dislocation, knee trauma, magnetic resonance imaging
Patellar dislocation is a frequent knee concern that most commonly occurs during adolescence and early adulthood.7,18 Several anatomic risk factors for patellar dislocations have been described, such as a high-lying patella (patella alta), trochlear dysplasia, rotational malalignments, and pronounced valgus malalignment of the knee joint.2,3 Lateral patellar dislocation occurs when a semiflexed knee joint rotates into valgus and the force vector of the extensor apparatus shifts toward the lateral side of the knee joint over the lateral trochlear facet of the femur.1 If the laterally directed force applied to the patella exceeds the strength of the medial stabilizing structures, mainly the medial patellofemoral ligament, they will be damaged, allowing the patella to dislocate over the lateral femoral condyle.1 The lateral edge of the lateral trochlear facet directs high energy toward the vertical ridge and medial facet of the patella during dislocation or as the patella reduces into the groove. This may predispose these areas to chondral or osteochondral lesions after patellar dislocation. Intra-articular osteochondral fractures (OCFs) have been reported to occur concomitantly in 2% to 44% of cases of patellar dislocation.12,18,22
Because cartilage damage in excess of 1 cm2 has been reported to increase the risk for articular degeneration, the presence of OCF has been regarded as a key factor in determining the treatment of a patellar dislocation.6 OCF of the knee has been regarded as a criterion for operative treatment in the acute phase.23,25 If the fracture is treated surgically, the primary procedure is reduction and fixation of the OCF fragment into its original location using biodegradable pins or sutures.8,10,28,29 If refixation is not possible, microfractures, subchondral drilling, or periosteal or abrasion chondroplasty may be considered.9,24
Despite the theoretical basis of the biomechanics of injury mechanism, literature describing the anatomic characteristics of OCFs in the knee joint after patellar dislocation is limited. Previous studies have been conducted in small patient samples, mostly from pediatric populations. The findings of Seeley et al21 and Nietosvaara et al12 addressing 46 and 15 patellar dislocation patients with OCF, respectively, are in line with the prevailing understanding of biomechanics of the OCF injury. These studies showed OCFs occurred most commonly in the medial patellar facet (69% of patients with OCFs) and the lateral condyle of the femur (21%). In 10% of the patients, both the patella and the femur were affected. Previous studies have not accounted for differences in injury patterns among patient subgroups.
The aim of the current study was to describe the patterns of OCFs in the knee joint after acute or recurrent patellar dislocation in a sample of patients from 2 orthopaedic trauma centers.
Methods
Patient Sample
In Finland, ethical approval is not required for register-based studies (Medical Research Act, 488/1999; https://www.finlex.fi/en/). Permission to conduct the study was granted by the hospital’s medical directors (research permit R19529). In reporting, we complied with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.27 Patient data for the current multicenter study were collected retrospectively from the electronic patient records of Central Finland Hospital (CFH), Jyväskylä, Finland, and Tampere University Hospital (TAUH), Tampere, Finland. These 2 hospitals serve a population of 700,000 to 800,000 citizens. The electronic search was conducted from the patient records for the years 2012 to 2018 using International Classification of Diseases, 10th Revision, diagnosis codes S83.0 (acute patellar dislocation) and M22.0 (recurrent patellar dislocation). Medical records of identified patients were screened for inclusion.
The study inclusion criteria were diagnosis of patellar dislocation and osteochondral fragment verified on magnetic resonance imaging (MRI) scans. In the study hospitals, MRI is conducted in the orthopaedic department. The physician in the emergency department (ED) is responsible for the primary care of patellar dislocations and assesses the need for referral to the orthopaedic department. Although the guidelines in the study hospitals specify that all patients with primary patellar dislocation be referred for MRI, the final decision of referral lies with the physician in the ED. Thus, if the physician in the ED interprets the injury as nonsevere and the patient does not seek further treatment from the study hospitals, the patient may not be referred to the orthopaedic department and for MRI in the study hospitals. In addition, patients with insurance may seek treatment in private sector hospitals instead of public hospitals despite the referral to the orthopaedic department. In these patients, additional diagnostics and MRI may be organized in the private sector.
An osteochondral fragment was defined as an intra-articular loose body cleaved from the articular surface of the patellofemoral or tibiofemoral joint and containing components of cartilage and bone. Exclusion criteria are presented in Table 1. The electronic search yielded a total of 2373 patients treated during the study period. After the patients’ medical records were screened, 192 patients with no patellar dislocation were excluded. Of the remaining 2181 patients, 1189 had undergone MRI of the knee.
Table 1.
Study Exclusion Criteriaa
| Exclusion Criteria |
|---|
| Previous surgery for patellar dislocation |
| Previous major traumas of the knee joint (ligament ruptures, intra-articular fractures, etc) |
| MRI not performed in study hospitals |
| Loose fragment containing only cartilage or bone |
| Extra-articular medial patellofemoral ligament avulsion fractures |
| Chondral or osteochondral impression fractures with no loose fragment |
| Round-shaped OCF fragment interpreted as an old fracture (ie, did not occur in the most recent dislocation) |
aMRI, magnetic resonance imaging; OCF, osteochondral fracture.
Descriptive data were collected retrospectively from patient records. To control bias attributed to inaccurate use of diagnosis coding, information on the occurrence of previous patellar dislocations was collected from patient records to verify the correct diagnosis of primary or recurrent dislocation. If a patient had several episodes of patellar dislocation, the episode in which the OCF occurred for the first time was selected for final analysis.
MRI Evaluation
MRI was conducted using 1.5- or 3-T scanners with proton density– and T2-weighted turbo spin echo sequences. Slice thickness was set between 2.5 and 3.5 mm, and slice increment was set between 2.8 and 4.0 mm. During imaging, the examined knee was set to 30° of flexion. A coil was used.
Radiologic parameters were examined from patients' MRI scans. Two observers at each hospital (M.U. and J.P.R. in CFH and M.U. and V.P. in TAUH) individually evaluated all MRI scans. Skeletal maturity was determined by examining growth plate maturity. The definition of skeletal maturity was an opening of the physis <5 mm in any section or complete epiphyseal fusion of the distal femur.4
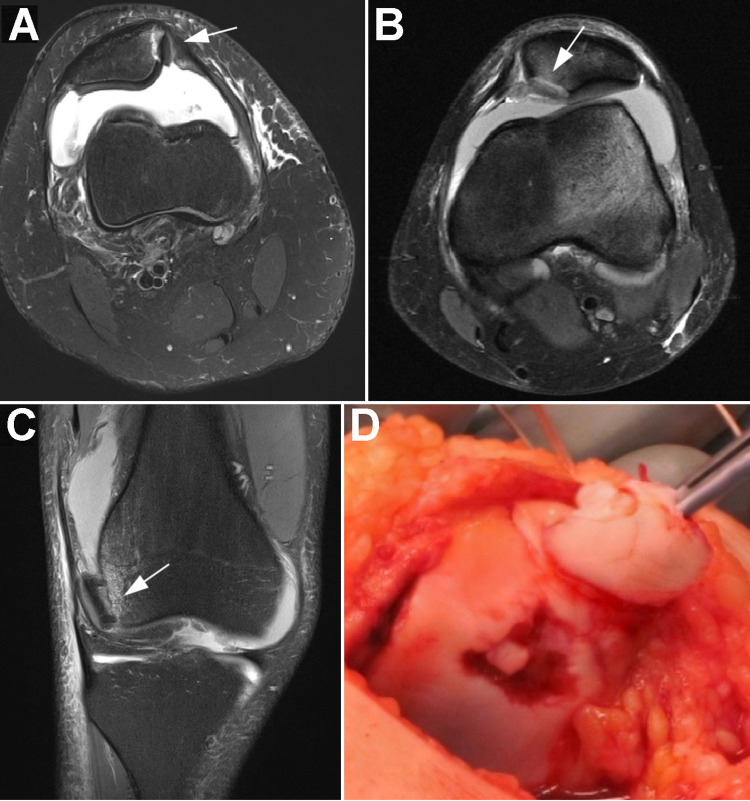
OCF location was categorized according to the anatomic region in the knee joint (Figure 1). Patellar OCFs were divided into 2 regions: medial facet and patellar ridge. An OCF in the patellar ridge was defined as a fracture area extending to the highest edge of the patellar ridge. Femoral condylar OCFs were defined as being located only at the lateral edge of the articular surface of the lateral condyle. If there were discrepancies in OCF location between observers, consensus was achieved by the same 2 observers jointly double-checking the MRI scans of these patients.
Figure 1.
MRI findings of OCFs (arrows): (A) medial facet of the patella, (B) patellar ridge, and (C) lateral femoral condyle. (D) Perioperative image of the OCF in the patellar ridge. MRI, magnetic resonance imaging; OCF, osteochondral fracture.
Three-dimensional diameters of the OCF fragment were measured. The size of the OCF area was estimated by multiplying the longest diameter of the fragment by the second longest. If several fragments had cleaved from the same location, the sizes of these fragments were summed to obtain the total fracture area. Observers’ mean measurements were calculated to report the estimated sizes of the areas of the OCF fragments.
Statistical Analysis
Data are presented as frequencies with percentages or as medians with interquartile ranges (IQRs). Subgroup analyses by sex, skeletal maturity, and primary versus recurrent patellar dislocation were performed separately. Differences in OCF location between the subgroups were examined using a chi-square test. Normality of continuous variables (age and OCF size) was tested using a Shapiro-Wilk test. Given that normality of the variables was violated (Shapiro-Wilk test; P < .05), a nonparametric approach was applied in further analysis. Mann-Whitney U tests were performed to examine differences in OCF size between the subgroups. A Kruskal-Wallis test was used to compare ages among patients with different OCF locations. The association between age and OCF size was examined by calculating Spearman correlation coefficients. Statistical analyses were performed using R Version 3.6.1 (R Foundation for Statistical Computing).15
Results
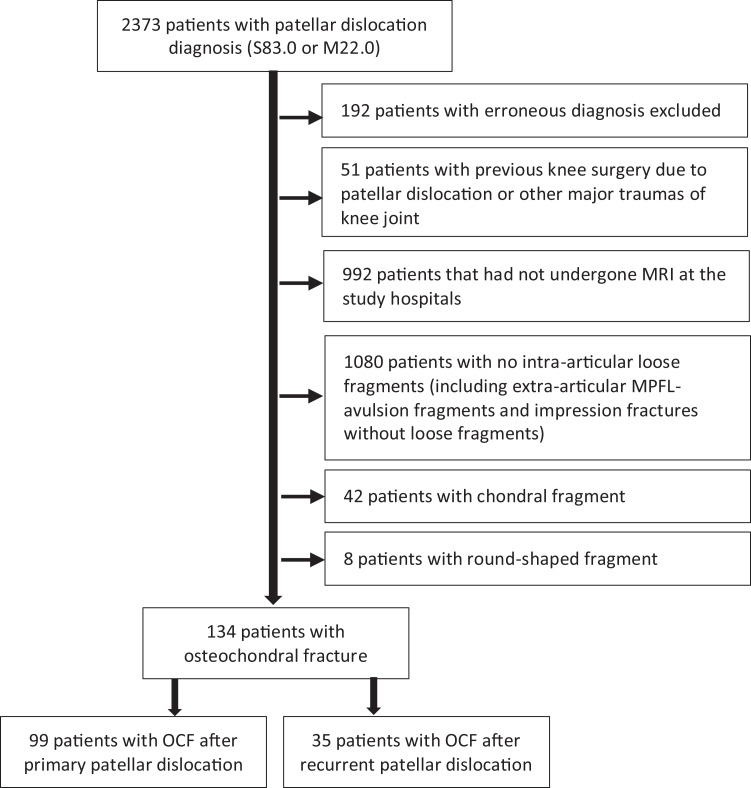
Of 1189 patients who had undergone MRI, 134 (11%) eligible patients with OCF were identified (Figure 2, Table 2). The sample consisted of 99 (74%) patients with OCF after primary patellar dislocation and 35 (26%) with OCF after recurrent patellar dislocation. The median age of the included patients was 17 years (IQR, 14-22 years), with female patients slightly in the majority (55%). Two-thirds of the patients were skeletally mature. Of 992 patients who had not undergone MRI and thus were excluded, 62% were female and the median age was 24 years (IQR, 19-33 years).
Figure 2.
Flowchart of patient selection. MPFL, medial patellofemoral ligament; MRI, magnetic resonance imaging; OCF, osteochondral fracture.
Table 2.
Patient Characteristicsa (N = 134)
| No. (%) | |
|---|---|
| Age, y | 17 (14-22)b |
| Female | 74 (55.2) |
| Left knee affected | 85 (63.4) |
| Skeletally mature | 88 (65.7) |
| OCF occurrence | |
| Primary PD | 99 (73.9) |
| Recurrent PD | 35 (26.1) |
aOCF, osteochondral fracture; PD, patellar dislocation.
bMedian (interquartile range).
In 85 (63%) patients, the OCF was located in the patella: in the medial facet in 62 (46%) patients and in the patellar ridge in 22 (16%) patients (Figure 3). The lateral femoral condyle was affected in 46 (34%) patients. Four patients (3%) had an OCF in the femur and patella. The median OCF size was 146 mm2 (IQR, 105-262 mm2) and was 137 mm2 (IQR, 105-235 mm2) in the patella and 173 mm2 (IQR, 105-278 mm2) in the femur. Observed differences in OCF sizes among the locations were not statistically significant (P = .363).
Figure 3.
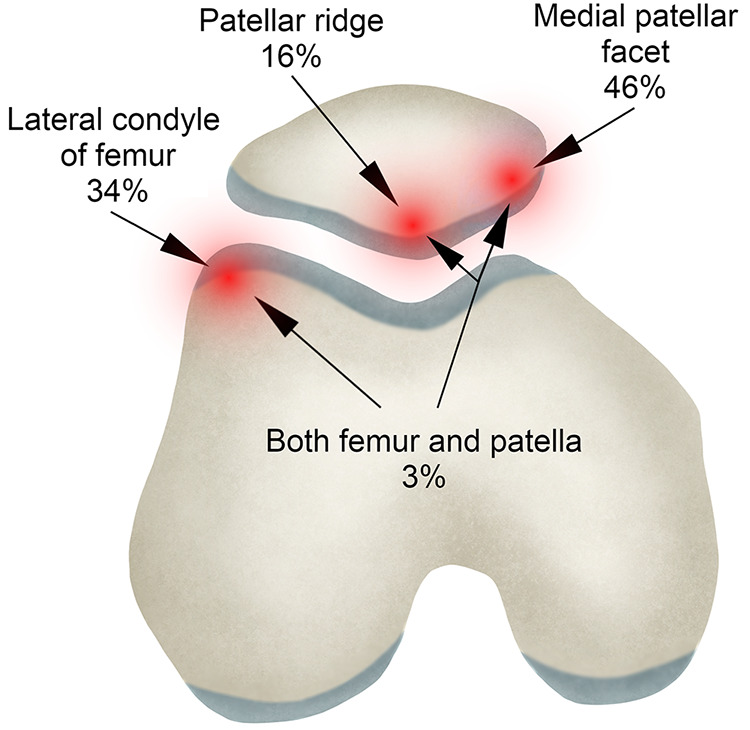
Distribution of osteochondral fracture locations in an axial view of the patellofemoral joint.
Before subgroup analysis was performed, the patients with an OCF in the femur and patella were excluded because they were too few in number. Inspection of the differences in the location of the OCF (patellar vs femur) between subgroups by sex, skeletal maturity, and primary versus recurrent dislocation revealed a significant difference by sex (Table 3). The proportion of patellar versus femoral OCFs was higher in female (76%) than male patients (53%; χ2 = 6.87; df = 1; P = .009) (Figure 4). The other subgroup analyses showed no differences in OCF location. Furthermore, patellar OCF size was larger in patients with primary than with recurrent patellar dislocations (147 mm2 in primary vs 119 mm2 in recurrent; P = .040). Femoral OCF size did not differ between the patients with primary and recurrent patellar dislocations. In addition, no significant differences between any of the other subgroups were observed for OCF size in the patella or femur. Patient age was not significantly associated with OCF size (ρ = –0.02; P = .841) or location (P = .279).
Table 3.
Numerical Representations and Statistics on Location and Size of OCFs in Subgroup Analysisa
| Sex | Skeletal Maturity (Physes) | OCF Occurrence | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OCF | Female | Male | P Value | Open | Closed | P Value | Primary PD | Recurrent PD | P Value |
| Locationb | .009 | .543 | .252 | ||||||
| Patella | 54 (76) | 31 (53) | 28 (61) | 57 (68) | 66 (66) | 19 (56) | |||
| Femur | 17 (24) | 28 (47) | 18 (39) | 27 (32) | 30 (34) | 15 (44) | |||
| Size,c mm2 | |||||||||
| Patella | 131 (107-221) | 176 (106-261) | .446 | 169 (111-262) | 131 (105-229) | .392 | 147 (113-263) | 119 (71-167) | .040 |
| Femur | 148 (114-214) | 181 (92-330) | .880 | 129 (95-264) | 188 (125-301) | .306 | 163 (101-277) | 174 (125-277) | .766 |
aValues are presented as No. (%) or median (interquartile range). OCF, osteochondral fracture; PD, patellar dislocation.
bDifferences in location of OCFs were tested using a chi-square test.
cDifferences in size of OCFs were tested using the Mann-Whitney U test.
Figure 4.
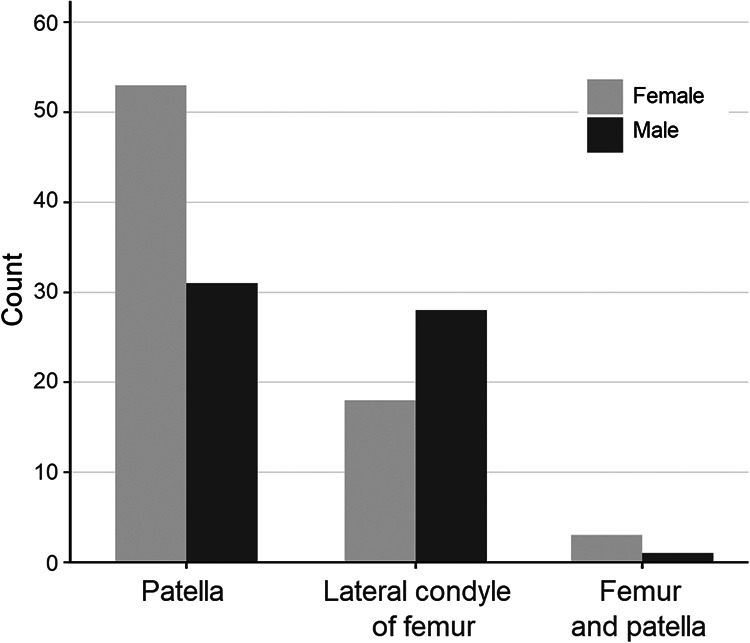
Differences between male and female patients in the distribution of osteochondral fracture locations.
Discussion
In this series, intra-articular OCFs after patellar dislocation were most commonly located in the medial facet of the patella or lateral edge of the lateral femoral condyle. The finding is in line with the prevailing assumption regarding the injury mechanism; that is, during patellar dislocation and relocation, the medial patellar facet and lateral femoral condyle are exposed to high energy, causing kissing contusions and possible OCF.1,12 Despite the large variation in the sizes of the OCF fragments, the size did not vary significantly by location.
Seeley et al21 reported similar results in their study of 46 patients with OCFs after patellar dislocation, of whom 76% had an OCF in the patella, 24% had an OCF in the lateral femoral condyle, and 6.5% had a combined injury. In the current study, the proportion of patellar OCFs was slightly lower and that of lateral femoral condyle OCFs was slightly higher. However, our sample and the sample studied by Seeley and colleagues were markedly different. Their study comprised cases of primary patellar dislocation in a pediatric population with a mean age of 15 years, among whom 85% had open growth plates (although criteria were not defined) and the majority were male.21 In this study, we did not limit patient ages; instead, we included all patients with OCFs. The patients in our sample were also notably older (median age, 17 years; IQR, 14-22 years), and 34.3% had open growth plates. However, our groups of patellar and femoral OCFs did not differ in age, skeletal maturity, or the proportions of primary and recurrent dislocations. Our results are in line with those of Nietosvaara et al,12 who found that patellofemoral joint morphology remains constant during growth. Thus, physical stress on the joint is equally distributed during growth. It is reasonable to assume that the same may apply to the biomechanics of patellar dislocation.
Sillanpää et al22 studied the incidence of patellar dislocation in male conscripts with a mean age of 20 years. In their study, all patellar dislocations occurred in sports or sports-related military training. Although we did not observe the actual injury mechanism or situation, the findings of Sillanpää et al suggested that patellar dislocations and concomitant OCFs occurring during late adolescence and early adulthood might be closely related to sports, in which the patellofemoral joint is exposed to high energy with rapid changes in the directions of force vectors.
The subgroup analysis revealed significant differences between male and female patients in the location of OCFs. In female patients, patellar OCFs were more frequent than were femoral OCFs, whereas in their male counterparts the 2 OCF locations were equally distributed. The difference between the sexes in the distribution of OCF locations in our study contrasts with the distribution of OCF locations in the male-majority sample studied by Seeley et al.21 However, their results might be explained by their small sample size. The sex distribution in the current study sample is in line with previously reported sex distributions of patients with patellar dislocation.5,7,12,18 The finding might suggest that the sexes are at equal risk for OCFs.
In patellar dislocation, the main medial stabilizing structure of the patella, the medial patellofemoral ligament, has been shown to be injured in practically every case.13,14,17,26 After primary patellar dislocation and medial patellofemoral ligament injury, the biomechanics of patellar dislocation alter with recurrent dislocations, as the patella is more easily able to move laterally. As a result, the patella may dislocate after low-energy trauma with lower impact on the articular surfaces of the patellofemoral joint. In the current study, patellar OCFs resulting from recurrent patellar dislocation were significantly smaller than those after primary dislocation. A similar trend was observed in femoral OCFs, although the difference was not statistically significant. Nevertheless, OCF location did not differ between primary and recurrent patellar dislocations. It has been hypothesized that, rather than actual dislocation of the patella, an OCF may occur after spontaneous relocation of the patella with mild flexion of the knee joint after lateral patellar dislocation.11,12,16,19,20 Thus, after injury of the stabilizing structures during dislocation of the patella, the biomechanics of spontaneous reduction of the patella are the same in primary and recurrent dislocations, causing equal OCF risk. However, the difference in size of the OCFs between those occurring in primary and recurrent dislocations suggests that there may be differences in the biomechanics of the injury, with the higher impact on the articular surfaces occurring in primary dislocations causing larger OCFs.
This study has several strengths. First, this is the largest study to be conducted on the injury patterns of patients with patellar dislocation with OCF. Previous literature consists of small case series, and the majority of the studies that have examined patellar dislocation excluded patients with OCF. Second, this study was performed as a multicenter study in the catchment area of 2 hospital districts in Finland, allowing for the inclusion of more patients from a wider geographic area and for generalization of the results. The screening of all patients treated for patellar dislocation in the 2 hospitals mitigated selection bias in our sample. Third, 2 independent evaluators blinded to each other’s results performed the MRI-based estimates of OCF size and location. This method enhanced the consistency and reliability of the assessment. Fourth, to promote homogeneity of the injury of interest, relatively strict OCF criteria were set. A homogeneous study population provides more precise and reliable results that well-represent patients meeting the inclusion criteria. The main limitation of the study was the retrospective study design. Despite the hospital guidelines, almost a half of the patients were not referred for MRI. Thus, we did not have a complete picture of all injuries. However, the patients who did not undergo MRI in the study hospitals were older than were patients in the study. In addition, we did not examine the trauma mechanism or joint laxity of the patients, which could have influenced interpretation of the results.
Conclusion
OCFs after patellar dislocation were located at the medial patellar facet in approximately two-thirds of patients and at the lateral femoral condyle in one-third. OCF location differed by sex, with female patients showing a higher proportion of patellar than femoral OCFs. OCFs may be larger after primary dislocation than after recurrent dislocation.
Footnotes
Final revision submitted September 10, 2020; accepted October 2, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Beasley LS, Vidal AF. Traumatic patellar dislocation in children and adolescents: treatment update and literature review. Curr Opin Pediatr. 2004;16:29–36. [DOI] [PubMed] [Google Scholar]
- 2. Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev. 2018;26:8–15. [DOI] [PubMed] [Google Scholar]
- 3. Diederichs G, Issever AS, Scheffler S. MR imaging of patellar instability: injury patterns and assessment of risk factors. Radiographics. 2010;30:961–981. [DOI] [PubMed] [Google Scholar]
- 4. Dvorak J, George J, Junge A, Hodler J. Age determination by magnetic resonance imaging of the wrist in adolescent male football players. Br J Sports Med. 2007;41:45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114–1121. [DOI] [PubMed] [Google Scholar]
- 6. Guettler JH, Demetropoulos CK, Yang KH, Jurist KA. Osteochondral defects in the human knee: influence of defect size on cartilage rim stress and load redistribution to surrounding cartilage. Am J Sports Med. 2004;32:1451–1458. [DOI] [PubMed] [Google Scholar]
- 7. Hsiao M, Owens BD, Burks R, Sturdivant RX, Cameron KL. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med. 2010;38:1997–2004. [DOI] [PubMed] [Google Scholar]
- 8. Koëter S, van Loon C, van Susante J. Lateral femoral condyle osteochondral fracture caused by a patella luxation: advantages and disadvantages of PLA fixation. Eur J Orthop Surg Traumatol. 2006;16:268–270. [Google Scholar]
- 9. Lee BJ, Christino MA, Daniels AH, Hulstyn MJ, Eberson CP. Adolescent patellar osteochondral fracture following patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2013;21:1856–1861. [DOI] [PubMed] [Google Scholar]
- 10. Li Z-X, Song H-H, Wang Q, Guo D-M. Clinical outcomes after absorbable suture fixation of patellar osteochondral fracture following patellar dislocation. Ann Transl Med. 2019;7(8):173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Milgram J. Tangential osteochondral fracture of the patella. J Bone Joint Surg Am. 1943;25:271–280. [Google Scholar]
- 12. Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14:513–515. [DOI] [PubMed] [Google Scholar]
- 13. Nomura E, Horiuchi Y, Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee. 2002;9:139–143. [DOI] [PubMed] [Google Scholar]
- 14. O’Reilly M, O’Reilly P, Bell J. Sonographic appearances of medial retinacular complex injury in transient patellar dislocation. Clin Radiol. 2003;58:636–641. [DOI] [PubMed] [Google Scholar]
- 15. R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2019. [Google Scholar]
- 16. Rorabeck C, Bobechko W. Acute dislocation of the patella with osteochondral fracture: a review of eighteen cases. J Bone Joint Surg Br. 1976;58:237–240. [DOI] [PubMed] [Google Scholar]
- 17. Sanders TG, Morrison WB, Singleton BA, Miller MD, Cornum KG. Medial patellofemoral ligament injury following acute transient dislocation of the patella: MR findings with surgical correlation in 14 patients. J Comput Assist Tomogr. 2001;25(6):957–962. [DOI] [PubMed] [Google Scholar]
- 18. Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ. Incidence of first-time lateral patellar dislocation: a 21-year population-based study. Sports Health. 2018;10:146–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Savarese A, Lunghi E. Traumatic dislocations of the patella: problems related to treatment. Chir Organi Mov. 1990;75(1):51–57. [PubMed] [Google Scholar]
- 20. Scheller S, Mårtenson L. Traumatic dislocation of the patella: a radiographic investigation. Acta Radiol Suppl. 1974;336:1–160. [PubMed] [Google Scholar]
- 21. Seeley MA, Knesek M, Vanderhave KL. Osteochondral injury after acute patellar dislocation in children and adolescents. J Pediatr Orthop. 2013;33:511–518. [DOI] [PubMed] [Google Scholar]
- 22. Sillanpää P, Mattila VM, Iivonen T, Visuri T, Pihlajamäki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40:606–611. [DOI] [PubMed] [Google Scholar]
- 23. Smith TO, Donell S, Song F, Hing CB. Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Database Syst Rev. 2015;2:CD008106. [DOI] [PubMed] [Google Scholar]
- 24. Spahn G, Kirschbaum S. Operative treatment of deep chondral defects of the patella: results after abrasive arthroplasty and periosteal arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2005;13:352–356. [DOI] [PubMed] [Google Scholar]
- 25. Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res. 2007;455:93–101. [DOI] [PubMed] [Google Scholar]
- 26. Vainionpää S, Laasonen E, Pätlälä H, Rusanen M, Rokkannen P. Acute dislocation of the patella: clinical, radiographic and operative findings in 64 consecutive cases. Acta Orthop Scand. 1986;57:331–333. [DOI] [PubMed] [Google Scholar]
- 27. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Int Med. 2007;147:573–577. [DOI] [PubMed] [Google Scholar]
- 28. Walsh SJ, Boyle MJ, Morganti V. Large osteochondral fractures of the lateral femoral condyle in the adolescent: outcome of bioabsorbable pin fixation. J Bone Joint Surg Am. 2008;90:1473–1478. [DOI] [PubMed] [Google Scholar]
- 29. Zhou S, Cai M, Huang K. Treatment of osteochondral fracture of the lateral femoral condyle with TWINFIX Ti suture anchor “X”-shaped internal fixation under arthroscopy: a surgical technique and three cases report. Orthop Surg. 2020;12(2):679–685. [DOI] [PMC free article] [PubMed] [Google Scholar]