Abstract
The goal of this study was to gain insight on the sexual health needs of men who have sex with men (MSM) who use GPS-based social and sexual networking mobile applications (“apps”) and the future utility of app-based interventions. A health educator promoted HIV testing resources in four popular apps used by MSM. Content analysis was used to identify salient themes that emerged from the conversations. Four major themes were identified: (1) soliciting sexual encounters, (2) relationship building, (3) HIV and STI testing inquiries, and (4) seeking other sexual health information. The results suggest the intervention’s social media based strategy, respect for community culture, and unobtrusive approach was advantageous in establishing credibility and rapport with app users. These results highlight a need for convenient and discreet methods to access accurate sexual health information and suggest that apps provide an alternative, non-traditional venue for sexual health education in addition to HIV testing promotion.
Introduction
Gay, bisexual, and other men who have sex with men (MSM) are disproportionately affected by the HIV epidemic in the United States. MSM make up approximately 3% of the US population (Purcell et al., 2012), yet account for 63% of all new HIV infections and 78% of new infections among men 13 years and older (CDC, 2014). At the end of 2012, MSM accounted for 51% of persons living with a HIV diagnosis and 54% of those living with an AIDS diagnosis in the US (CDC, 2014). Considering these significant disparities, innovative approaches to HIV prevention for MSM are critical.
Academic researchers, health departments, community-based organizations (CBOs), and AIDS service organizations (ASOs) have begun to experiment with innovative mobile phone technologies to deliver HIV education and prevention programming to MSM (Bourne et al., 2011; Free et al., 2013; Lim et al., 2012; Noar & Willoughby, 2012; Reback et al., 2012; Rhodes et al., 2011; Sun, Stowers, Miller, Bachmann, & Rhodes, 2015). One of these technologies has been the use of mobile applications (“apps”). With the ever-increasing prevalence of smartphones and tablets, app use has increased 85% from 2011 to 2012 among Americans (Nielsen Holdings N.V., 2012). In general, MSM have been shown to be early adopters of mobile technologies and have greater use of these technologies than their heterosexual counterparts (Grov, Breslow, Newcomb, Rosenberger, & Bauermeister, 2014; LGBT Market Research and Development Lab, 2015).
Currently, there are over 2.6 million apps available through the Apple and Google Play app stores (Perez, 2015), including apps developed by health professionals to provide HIV and sexually transmitted infection (STI) education and outreach services (Muessig, Pike, LeGrand, & Hightow-Weidman, 2013; Holloway et al., 2014; Swendeman, Comulada, Ramanathan, Lazar, & Estrin, 2015). However, after such apps are created, uptake and use of these apps is limited. A 2013 study of 55 mobile apps related to HIV and STI prevention and care found that the apps were rarely downloaded (median 100–500 downloads), received average customer ratings (3.7 out of 5 stars), and failed to reach a significant number of higher risk individuals (Muessig et al., 2013a).
Utilizing established, popular apps as a medium for interventions could be more effective than creating new apps due to the large number of existing users of some established apps; for example, 3% of US adults—including 11% between the ages of 25 and 34—use social and sexual networking apps such as Tinder and Grindr (Smith & Duggan, 2013). Many of these established apps offer Global Positioning System (GPS)-based networking capabilities (the use of geographic data and technologies to tailor social networking services to a user’s specific location), which allow users of the same app to locate one another based on geographic proximity. Several GPS-based social and sexual networking apps designed specifically for MSM have emerged in recent years and have large numbers of users. Popular apps, such as A4A/Radar, Jack’d, and SCRUFF, as well as Grindr, have garnered millions of downloads and active users, which is far greater than the number of downloads and active users of newly created HIV and STI intervention apps. For example, SCRUFF boasts a community of over 5 million individuals worldwide with over 50 million messages being exchanged each day (Perry Street Software, Inc., n.d.). Through these apps, MSM are able to leverage their GPS capabilities to quickly and easily find partners in close proximity (Gudelunas, 2012; Sun et al., 2015).
Studies suggest that use of GPS-based social and sexual networking apps may facilitate higher risk sexual partnerships among MSM. A 2012 study of 375 Grindr users in metropolitan Los Angeles revealed that 46.1% of participants reported any unprotected anal intercourse and 38.9% reported any unprotected receptive anal intercourse in the past 3 months (Landovitz et al., 2012). Further, 70% of those reporting unprotected anal intercourse believed they were “unlikely” or “very unlikely” to ever acquire HIV infection (Landovitz et al., 2012). Another study of 7,184 MSM visiting the Los Angeles Gay & Lesbian Center for STI screening revealed that those who used GPS-based social and sexual networking apps to meet sexual partners had greater odds of testing positive for chlamydia and gonorrhea (Beymer et al., 2014). In a recent study of 295 MSM app users, Holloway and colleagues (2015) found that users with acquaintances met through social and sexual apps were more likely to have had more sexual partners in the past 30 days and nearly four times as likely to have engaged in unprotected anal intercourse with the last partner they met on the app. These findings lend credence to previous research purporting that MSM who solicit partners through Internet-based mediums (including apps) are more likely to report unprotected anal intercourse, more sexual partners, and a history of STI infection when compared to their counterparts who meet partners in physical spaces (Garofalo, Herrick, Mustanski, & Donenberg, 2007; Ogilvie, 2008; Rhodes et al., 2002).
Considering the possible health risks facing app users, interest in harnessing established GPS-based social and sexual networking apps for HIV prevention and education has emerged (Holloway et al., 2014; Muessig et al., 2013b; Sun et al., 2015; The Social Science Research Lab, 2013). In particular, two studies investigating the acceptability of using established apps have shown that between 64–80% of study participants felt apps were acceptable media for HIV and STI education and prevention activities (Holloway et al., 2014 and Sun et al., 2015). Further, a San Diego community clinic reported their social networking strategy, utilizing Grindr, resulted in increases in MSM getting tested for HIV and other STDs at the clinic, identification of one preliminary positive HIV result, and linking several known positives to HIV-related care (The Social Science Research Lab, 2013). These efforts demonstrate that GPS-based social and sexual networking apps may be effective modes to increase HIV testing, care linkage, and treatment adherence among MSM.
Although these studies show promise for interventions that use existing and popular apps, the specific sexual health needs of users, as identified by the app users themselves, require further attention. The goal of this qualitative study was to understand sexual health needs of MSM who use GPS-based social and sexual networking apps by documenting and describing the interactions between app users and a health educator for MAP’T (Mobile Apps for Prevention & Testing), an intervention designed by our community-based participatory research partnership to promote HIV testing among MSM using established GPS-based social and sexual networking apps (Sun et al., 2015). We sought to gain insights into the future utility of app-based HIV prevention interventions.
Methods
Between August 2013 and October 2014, a trained health educator promoted local HIV testing resources using 4 popular GPS-based social and sexual networking apps geared towards MSM - A4A/Radar, Grindr, Jack’d, and SCRUFF. These apps were chosen due to their high use in the study’s 16-county catchment area in north central North Carolina and diversity of typical app users. The health educator was a member of the local gay community and had an “insider’s” understanding of communities of gay and bisexual men, other MSM, and transgender persons. He was knowledgeable about the apps, comfortable talking and offering sound and sex-positive advice about sensitive issues, and understood the importance of remaining discreet. During the intervention, the health educator created a biographical profile on each of the four apps (see Figure 1 for example). The profile information provided was consistent across all four apps and each profile included his actual picture from the waist up where he was clothed in business casual attire. The health educator provided his age, height, weight, and race, as well as information regarding his affiliation with a local ASO and his purpose for using the app (HIV and STI testing promotion and education) on each profile page. He logged into the apps Monday through Friday between the hours of 8:30am and 5pm. The health educator did not target users and only responded after an app user contacted him. This approach was respectful of the culture of the app user community as it is inappropriate to target users with unsolicited HIV-related messages. Based on user inquiries, the health educator compiled informative, user-friendly responses to questions about HIV and STIs and about testing. He also provided reputable resources about various sexual health topics based on user needs and priorities.
Figure 1.
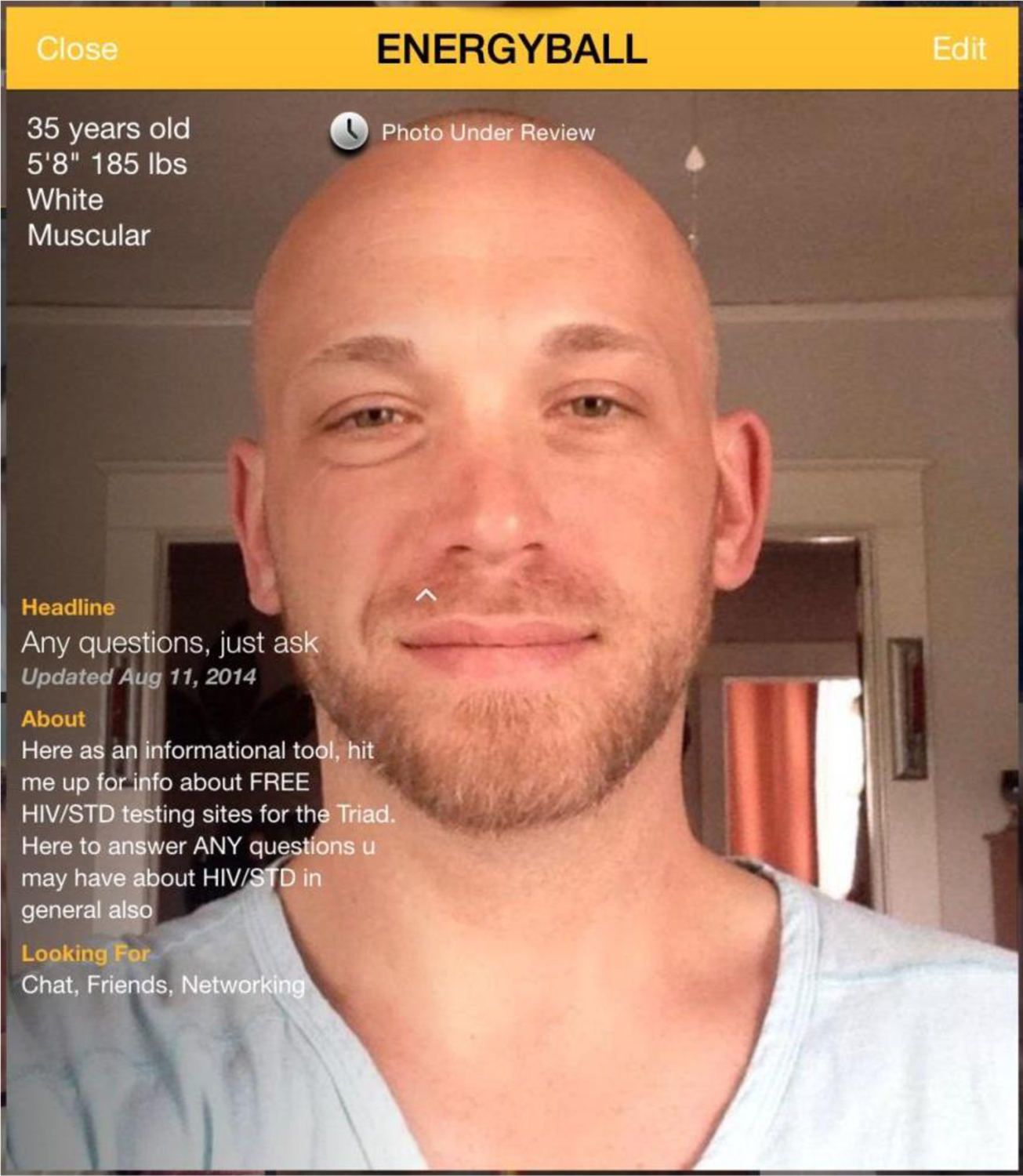
Health Educator Profile on Grindr
Data Collection and Analysis
Prior to data collection, Institutional Review Board (IRB) approval, including a waiver of informed consent, was obtained from the Wake Forest School of Medicine. Interactions between app users and the health educator were captured through screen-shot images from the health educator’s mobile device and stored on a password-protected computer. Screen-shot images allowed text, photograph, and “emoticon”—a sequence of keyboard symbols meant to represent facial expressions—analysis. All screen-shot images were uploaded to ATLAS.ti 7.0 for data analysis. Two team members used content analysis (Weiss, 1994) to code the screenshots and identify salient themes that emerged. After coding was complete, the entire research team reviewed results for validation and refinement; discrepancies were resolved via discussion.
Results
This analysis included 673 unique interactions between the health educator and app users. Due to app users’ penchant for pseudonyms and anonymous profiles high and the possibility of users with multiple accounts across the 4 apps, the unique interactions do not reflect necessarily 673 unique app users. The analysis of the data revealed four themes prevalent in the interactions: (1) solicitation for sexual encounters by users and sensitive redirection by the health educator were used to initiate conversations, (2) relationship building was key to intervention success, (3) users had HIV and STI testing inquiries, and (4) users sought sexual health education. Each theme is described below. Table 1 illustrates example interactions between the health educator and users.
Table 1.
Illustrative conversations from mobile app transcripts
| Soliciting sexual encounters | |
| Interaction that evolved to sexual health inquires |
App user: Are you looking for anything? Wouldn’t mind blowing you Interventionist: No thanks man, not why I’m here. If you ever have any questions about testing, testing sites, HIV/AIDS, STD that you would like to ask me feel free to ask App user: K. What’s the chances of catching something from oral sex |
| Persistence in spite of disclosure |
App user: Wassup Interventionist:Working man, that is actually why I am on this app App user: I know you told me before. I would like to get to know you tho…No? Interventionist: Sorry man, that is not why I am here |
| Relationship building | |
| Casual conversation |
App User: How are you this morning? Interventionist: Great thanks, just working. Yourself? App User: I’m very well. About to make some coffee here at the house. Interventionist: Nice, having coffee myself App user: Sounds lovely |
| Support and confiding | App User: I am not [too] long ago finding out myself that I now live with HIV and [it’s] just nice to see we have good people out there teaching others about the disease :) |
| HIV and STI testing inquires | |
| Seeking free testing options | App user: I see you are here to answer questions. I was wondering where I can go to get/free STD testing here in GSO. Thanks |
| Concerns about privacy | App user: Hi. I just heard about you from someone on here. I am interested in being tested for HIV/STD but I am fearful someone at a testing place may know me. I also work for a major lab and am fearful about my testing going there. Is there anyway I can get confidential testing not linked to my name and where can I get tested for free or very cheaply? |
| Seeking other sexual health education | |
| Oral sex inquiries | App user: So if someone is sucking me and he have HIV I can not get it right? What if I brush my teeth and floss and my gum bleed like 1 hour before I suck someone [but] by that time [I’m] not bleeding anymore? |
| Questions about PrEP | App user: What are you thoughts about Truvada once daily for HIV prevention…How harsh are the side effects? |
Soliciting Sexual Encounters
Solicitation of sexual encounters was a salient theme in interactions (32%, n = 215) that users initiated with the health educator. Pictures, emoticons, and sexually explicit messages were used to convey interest in a sexual relationship. These interactions were expected due to the nature of the apps; thus, they served as conversation starters. The health educator used his reply to these messages to explain his role as a resource for HIV testing information and prevention. Following a sexually explicit comment from a user the health educator would respond with something like, “I am not tryin’ to mislead anyone, so I am going to be upfront from the start. This is strictly a work profile, not a personal one. I am a MAP’T health educator for the prevention of HIV/AIDS/STDS.”
User responses were varied following the health educator’s disclosure. Some users (24%, n = 52) stopped the interaction immediately with no further contact with the health educator or persisted in their attempts despite the health educator’s disclosure. For several other users, over time interactions often evolved from attempting to “flirt” with the health educator and suggesting having sex to covering topics about local testing services and other sexual health related topics.
Relationship Building
In over half of the interactions (56%, n = 377), users sought to know more about the health educator or to share with him information about themselves; these relationship-building exchanges helped to establish trust so that the health educator could then successfully provide information about HIV and STI testing and other sexual health topics. For example, upon learning the health educator’s reasons for using the apps, some users questioned his sexual orientation and HIV status. Users asked “Are you even gay?” or “Are you poz?” The health educator responded by affirming his sexual orientation as a gay man and truthfully answering questions about his HIV status. Some users expressed appreciation for the health educator’s presence on the app and his efforts to provide HIV testing information. For instance, one user commented: “I appreciate what you are doing to make yourself and the information available by networking on this site.”
In all interactions, the health educator’s approach was friendly, met the communication expectations of the app, and was never dismissive of questions and comments received from the users, even those that were sexually explicit. Instead, the health educator used these interactions to invite open dialogue and questions. Some users disclosed their HIV and STI statuses, risk behaviors, and HIV and STI exposure fears to the health educator. Given the disclosure of these personal matters, the health educator became a confidante and source of information and support for some users. However, it should be noted that not all interactions involved discussion of HIV, risks, and testing. Some interactions included discussion of topics such as school, work, and physical exercise or brief exchanges in which the users simply said hello or complimented the health educator’s appearance on his app profile. Although these topics were not directly related to the health educator’s intended purpose for using the app, these interactions appeared important in helping to build the health educator’s reputation and establish him as a member of the community among the app users. A few users contacted the health educator again several times to chat, obtain information, or follow up regarding test results.
HIV and STI Testing Inquiries
About 43% of (n = 287) users sought information regarding local HIV and STI testing resources or broader sexual health topics. Users had many questions about the cost and scheduling of HIV and STI testing. For instance, users desired access to free or affordable testing and also inquired about venues that offered same day appointments or testing at various times throughout the week. Users also expressed concerns related to confidentiality and privacy at traditional testing sites such as public health departments and at the offices of their primary care providers, as well as at diagnostic labs. For example, a user had specific questions regarding the confidentiality of his result: “Say something is positive, will they not tell me on the phone? I am married so I need to keep this totally discreet”. The health educator was able to provide information about the preservation of privacy and confidentiality during HIV and STI testing and diagnosis.
Seeking Other Sexual Health Information
In addition to HIV and STI testing, interactions highlighted users’ interest in broader sexual health topics, including: specific sexual behaviors (e.g., how to prepare for and have receptive anal sex), risk reduction strategies (e.g., HIV prevention in serodiscordant partnerships), HIV/AIDS and STI symptoms, and sexual function (e.g., ejaculation issues). Oral sex and pre-exposure prophylaxis (PrEP) were particularly prominent subjects in the interactions. Users inquired about the relative risk of HIV and STI transmission during oral sex in comparison to unprotected anal intercourse whereas others were concerned with the risks of specific behaviors such as “rimming” (oral-anal contact) and swallowing ejaculate. Other users wanted to learn more about PrEP access and availability. Users also had questions about costs and potential side effects of PrEP.
Discussion
This is the first study, to our knowledge, to explore the content of an intervention using existing and commonly used GPS-based social and sexual networking apps. Here we highlight four key lessons gained from our efforts. First, the health educator’s status as a member of the gay community was important in establishing his credibility among the users (e.g., he understood behavioral expectations and culture established by users of the app and knew common language). He was open about his sexual orientation, and his “insider” knowledge and respect for the community allowed him to connect with the users in a way that may not have been possible if he was a community outsider, starting when users initiated contact him and as relationships were built with users. The health educator was straightforward about his intentions for using the app, yet he engaged users in dialogue on a variety of topics, in addition to HIV and STI testing and sexual health.
Second, the health educator’s approach of not targeting users was key to establishing trust with the community of app users. Targeted approaches have been used in previous HIV prevention efforts for MSM using GPS-based social and sexual networking apps; for example, a community clinic reported linking Grindr and A4A/Radar users to local HIV and STI testing and primary care services through a targeted approach. Users did not initiate communications with the health educator; rather, representatives of the community clinic identified those at elevated risk based on their analyses of app profiles and initiated communication. As a result, some users expressed negative feelings about being contacted through the app; they felt “singled out” as high risk, “promiscuous”, and/or “diseased” (The Social Science Research Lab, 2013). In contrast, the MAP’T health educator never initiated contact with users nor was his presence advertised or promoted on the apps; he waited until he was directly contacted allowing him to meet users “where they are” and engaged in conversations at the pace of each user - building trust, discussing priorities, and offering guidance. Further, users contacting the health educator were able to see his role as a health educator and affiliation with a local AIDS service organization in his app profile. Thus, the intervention’s purpose was made explicitly clear to users seeking interaction.
Third, it has been suggested that the internet and social media provide the promise of reaching large numbers of people with targeted automated messages that follow programmed algorithms (Rhodes, Bowie, & Hergenrather, 2003; Bull & McFarlane, 2011); however, this intervention moves beyond information transfer and seeks to change behavior through individualized HIV prevention and education messaging and a level of social support. Much of the success of this intervention was the health educator’s skills to identify with, build trust, and offer appropriate and personalized guidance to social media users. This approach may be more appropriate than programmed responses based on entered data, particularly given that social media users are increasingly targeted by and suspicious of bots and fake identities (Isaacson, 2011). Automated interventions may not be as successful as interventions that include a real health educator who is crafting messages designed to develop trusting relationships, offer social support, promote testing, and problem solve real and perceived barriers.
Fourth, users expressed diverse sexual interests and needs. The purpose of the MAP’T intervention was to promote HIV and STI testing among MSM who use GPS-based social and sexual networking apps. However, users also expressed interest in topics regarding sexual function, sexual partnerships, specific types of sexual behavior, and PrEP. This finding about the need for broad sexual health information aligns with extant research regarding the unique needs of MSM using apps. One qualitative study of 22 young Black MSM, found that the men desired app content that addressed (1) information about STIs and HIV testing; (2) drug and alcohol use; (3) safer sex practices; (4) sexuality and relationships; (5) resources for gay-friendly providers; and (6) support groups in general and groups for HIV positive men (Muessig et al., 2013b). Our study highlighted the need for app interventions to be tailored to the specific needs of individuals within the community. These issues may affect HIV and STI prevention efforts and highlight the importance of future sexual health-specific app interventions for MSM being comprehensive and inclusive in their approach.
Finally, the results suggest that apps can be used as alternative venues for sexual health education and information. These findings align with previous literature that explored and documented the feasibility of non-traditional venues, such as in-home sex-toy parties and adult retail stores, for sex education and health promotion (Fisher et al., 2010; Herbenick & Reece, 2007). While there are some challenges to using apps, especially newly developed ones (Muessig et al., 2013a; Sun et al., 2015), using established, popular apps might reach populations at increased risk for HIV and other STIs. Studies have shown that app users generally view apps as appropriate platforms for sexual health information (Holloway et al., 2014; Muessig et al., 2013b; Sun et al., 2015). Many users in our study were comfortable contacting the health educator for information regarding disease transmission and sexual behaviors. These inquiries suggest that users may have limited people they feel comfortable reaching out to regarding sexual health issues and are in need of credible information from a reliable source. Utilizing health educators and interventionists in a space that is familiar, comfortable, and accessible to app users could help provide opportunities to clarify misconceptions regarding sexual health topics and issues.
Limitations
Some limitations should be noted when considering the findings of this study. The study is limited to one geographical area in northcentral North Carolina. Although this region of North Carolina has a catchment area of more than 1.3 million people, the generalizability of these results is limited. Future studies should consider the unique needs of MSM in the region or catchment area under study. Second, the 673 interactions described in the study do not necessarily reflect 673 unique app users. It is possible that users have multiple profiles across the four apps and could have contacted the health educator using under different profile names. Further, some users contacted the health educator on multiple occasions to ask additional questions or follow up on prior conversations. Finally, demographic data was not collected from the app users. While some app users include profile pictures and other pertinent identifying information, some users may create profiles without identifying information using pseudonyms and ‘fake’ profile pictures to maintain anonymity. Although factors such as age and race/ethnicity of each app user was not collected, we know that each app used in this pilot targeted diverse users. Future research should explore app use by demographic variables including age and race/ethnicity systematically.
Conclusion
This study highlights the utility of an app-based HIV and sexual health intervention that respects community culture and maintains an unobtrusive approach for establishing credibility and rapport with users. The results underscore the need for convenient and discreet methods to access accurate sexual health information and suggest that apps provide an alternative, non-traditional venue for sexual health education in addition to HIV testing promotion. Accordingly, these findings have important public health intervention implications. The results show it is possible to leverage the technology of mobile devices and the popularity of GPS-based social and sexual networking apps for sexual health interventions. These apps are a promising platform for providing sexual health education and geographically specific HIV and STD testing referrals.
Acknowledgments
Funding Source: National Institute of Mental Health (Grant #R01MH092932)
References
- Benotsch EG, Kalichman S, & Cage M (2002). Men who have met sex partners via the Internet: Prevalence, predictors, and implications for HIV prevention. Archives of Sexual Behavior, 31(2), 177–183. [DOI] [PubMed] [Google Scholar]
- Beymer MR, Weiss RE, Bolan RK, Rudy ET, Bourque LB, Rodriguez JP, & Morisky DE (2014). Sex on demand: geosocial networking phone apps and risk of sexually transmitted infections among a cross-sectional sample of men who have sex with men in Los Angeles county. Sexually Transmitted Infections, 90(7), 567–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourne C, Knight V, Guy R, Wand H, Lu H, & McNulty A (2011). Short message service reminder intervention doubles sexually transmitted infection/HIV re-testing rates among men who have sex with men. Sexually Transmitted Infections, 87(3), 229–231. [DOI] [PubMed] [Google Scholar]
- Bull SS, & McFarlane M (2000). Soliciting sex on the Internet: What are the risks for sexually transmitted diseases and HIV? Sexually Transmitted Diseases, 27(9), 545–550. [DOI] [PubMed] [Google Scholar]
- Bull S, & McFarlane M (2011). Technology-based health promotion. Los Angeles, CA: Sage. [Google Scholar]
- Centers for Disease Control and Prevention. (2014). HIV among Gay and Bisexual Men [Fact sheet]. Retrieved from http://www.cdc.gov/hiv/pdf/HIV-MSM-english-508.pdf
- Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, & … Haines A (2013). The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review. Plos Medicine, 10(1), 1–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Herrick A, Mustanski BS, &Donenberg GR (2007). Tip of the Iceberg: Young men who have sex with men, the Internet, and HIV risk. American Journal of Public Health, 97(6), 1113–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudelunas D (2012). There’s an App for that: The uses and gratifications of online social networks for gay men. Sexuality & Culture, 16(4), 347–365. [Google Scholar]
- Holloway IW, Rice E, Gibbs J, Winetrobe H, Dunlap S, & Rhoades H (2014). Acceptability of smartphone application-based HIV prevention among young men who have sex with men. AIDS and Behavior, 18(2), 285–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloway IW, Pulsipher CA, Gibbs J, Barman-Adhikari A, & Rice E (2015). Network Influences on the Sexual Risk Behaviors of Gay, Bisexual and Other Men Who Have Sex with Men Using Geosocial Networking Applications. AIDS and Behavior, 19(Suppl. 2), S112–S122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacson A (2011, May). Are You Following a Bot?: How to manipulate social movements by hacking Twitter. The Atlantic: Retrieved from http://www.theatlantic.com/magazine/archive/2011/05/are-you-following-a-bot/308448/ [Google Scholar]
- Landovitz RJ, Tseng CH, Weissman M, Haymer M, Mendenhall B, Rogers K, Veniegas R, … Shoptaw S (2013). Epidemiology, sexual risk behavior, and HIV prevention practices of men who have sex with men using GRINDR in Los Angeles, California. Journal of Urban Health, 90(4), 729–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim MC, Hocking JS, Aitken CK, Fairley CK, Jordan L, Lewis JA, &Hellard ME (2012). Impact of text and email messaging on the sexual health of young people: a randomised controlled trial. Journal of Epidemiology & Community Health, 66(1), 69–74. [DOI] [PubMed] [Google Scholar]
- Muessig KE, Pike EC, LeGrand S, &Hightow-Weidman LB (2013a). Mobile Phone Applications for the Care and Prevention of HIV and Other Sexually Transmitted Diseases: A Review. Journal Of Medical Internet Research, 15(1), e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muessig KE, Pike EC, Fowler B, Legrand S, Parsons JT, Bull SS, & … Hightow-Weidman LB (2013b). Putting Prevention in Their Pockets: Developing Mobile Phone-Based HIV Interventions for Black Men Who Have Sex with Men. AIDS Patient Care & STDs, 27(4), 211–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen Holdings NV (2012). State of the media: The social media report. New York, NY. [Google Scholar]
- Noar SM, & Willoughby JF (2012). eHealth interventions for HIV prevention. AIDS Care, 24(8), 945–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogilvie GS, Taylor DL, Trussler T, Marchand R, Gilbert M, Moniruzzaman A, &Rekart ML (2008). Seeking sexual partners on the Internet: A marker for risky sexual behaviour in men who have sex with men. Canadian Journal of Public Health, 99(3), 185–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez S (2015, January 13). Report: Google Play’s App Store And Developer Community Grew Faster Than Apple’s In 2014. Retrieved July 20, 2015, from http://techcrunch.com/2015/01/13/google-plays-app-store-and-developer-community-grew-faster-than-apples-in-2014/
- Perry Street Software, Inc. (n.d.). SCRUFF. Retrieved July 14, 2015, from Google Play website: https://play.google.com/store/apps/details?id=com.appspot.scruffapp
- Reback CJ, Grant DL, Fletcher JB, Branson CM, Shoptaw S, Bowers JR, Charania M, &Mansergh G (2012). Text messaging reduces HIV risk behaviors among methamphetamine-using men who have sex with men. AIDS and Behavior, 16(7), 1993–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Bowie DA, &Hergenrather KC (2003). Collecting behavioural data using the World-Wide Web: Considerations for researchers. Journal of Epidemiology and Community Health, 57(1), 68–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, DiClemente RJ, Cecil H, Hergenrather KC, & Yee LJ(2002). Risk among men who have sex with men in the United States: A comparison of an Internet sample and a conventional outreach sample. AIDS Education and Prevention, 14(1), 41–50. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Bowie DA, & Hergenrather KC (2003). Collecting behavioural data using the world wide web: considerations for researchers. Journal of Epidemiology and Community Health, 57(1), 68–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Duncan J, Vissman AT, Miller C, Wilkin AM, & … Eng E (2010). A pilot intervention utilizing Internet chat Rooms to prevent HIV risk behaviors among men who have sex with men. Public Health Reports, 125(Suppl. 1), 29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Vissman AT, Stowers J, Miller C, McCoy TP, Hergenrather KC, Wilkin AM, … Eng E (2011). A CBPR partnership increases HIV testing among men who have sex with men (MSM): outcome findings from a pilot test of the CyBER/testing Internet intervention. Health Education & Behavior, 38(3), 311–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A, & Duggan M (2013, October). Online Dating & Relationships. Washington, DC: Pew Research Center. [Google Scholar]
- Sun CJ, Stowers J, Miller C, Bachmann LH, & Rhodes SD (2015). Acceptability and Feasibility of Using Established Geosocial and Sexual Networking Mobile Applications to Promote HIV and STD Testing Among Men Who Have Sex with Men. AIDS and Behavior, 19(3), 543–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendeman D, Comulada WS, Ramanathan N, Lazar M, & Estrin D (2015). Reliability and Validity of Daily Self-Monitoring by Smartphone Application for Health-Related Quality-of-Life, Antiretroviral Adherence, Substance Use, and Sexual Behaviors Among People Living with HIV. AIDS and Behavior, 19(2), 330–340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendeman D, & Rotheram-Borus MJ (2010). Innovation in sexually transmitted disease and HIV prevention: Internet and mobile phone delivery vehicles for global diffusion. Current Opinion in Psychiatry, 23(2), 139–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RS (1994). Learning from Strangers: The art and method of qualitative interview studies. New York, NY: The Free Press. [Google Scholar]
- Winetrobe H, Rice E, Bauermeister J, Petering R, & Holloway IW (2014). Associations of unprotected anal intercourse with Grindr-met partners among Grindr-using young men who have sex with men in Los Angeles. AIDS Care, 26(10), 1303–1308. [DOI] [PubMed] [Google Scholar]


