Abstract
Correspondence to: F Baum fran.baum@flinders.edu.au
Fran Baum and colleagues discuss the factors that affected prediction of the success of national responses to covid-19 and will influence future pandemic preparedness
Key messages.
The Global Health Security Index predicted that the world in general was not well prepared for the pandemic but did not predict individual country preparedness
Ten factors seem to have contributed to the index failing to predict country responses, including overlooking political, economic, and social contexts and the role of civil society
Future assessments of pandemic preparedness need to take these 10 factors into account by adopting a systems approach which enables a focus on critical system components
Covid-19 has exposed and exacerbated existing flaws in public health systems around the world. Shredded social safety nets and underinvestment in healthcare systems, compounded by conflicts of interest, dismissal of scientific evidence, and failures of political leadership meant many countries were unprepared to deal with the covid-19 pandemic and vulnerable to the next one. Important lessons can be learnt from the various national responses to covid-19 to inform preparedness for future waves or the emergence of new pandemics or epidemics
The Global Health Security Index (GHSI), which measures preparedness for pandemics or epidemics, published its scores in October 2019, just before the covid-19 pandemic was declared.1 The US and UK scored highest on the GSHI, but both countries have done spectacularly badly in response to covid-19, whether measured in deaths or economic damage. The Epidemic Preparedness Index,2 also published in 2019, grouped countries into five levels of preparedness, and also placed the US and the UK and others that have fared poorly in the covid-19 pandemic in the highest categories. The GHSI and the Epidemic Preparedness Index are the only pandemic preparedness indices that cover most countries and thus enable cross country risk assessment. However, both failed to predict national covid-19 preparedness. To understand how to assess pandemic preparedness more accurately, we specifically focus on the GHSI because it includes a wide range of measures and comprehensive country data collection.3
The GHSI takes account of qualitative and quantitative data intended to measure the capacity of 195 countries to deal with disease outbreaks. Based on an expert assessment of structures and processes, the GHSI includes indicators related to geopolitical considerations, national healthcare capacity, and political and economic risk factors. It assesses countries using 140 questions across six domains: prevention, detection and reporting, response, health system, compliance with norms, and risk of infectious disease outbreaks. Scores range from 0 to 100, and a higher GHSI score indicates better preparedness.
The 2019 GHSI report provided prophetic recommendations for “a fast-spreading respiratory disease agent that could have a geographic scope, severity, or societal impact and could overwhelm national or international capacity to manage it.”1 The authors described “severe weaknesses in country abilities to prevent, detect, and respond to health emergencies; severe gaps in health systems; vulnerabilities to political, socioeconomic, and environmental risks that can confound outbreak preparedness and response; and a lack of adherence to international norms.”1 The average overall GHSI score for the 195 countries assessed was 40.2 out of 100, and 51.9 for the 60 high income countries. Less than 7% of countries scored in the highest tier for ability to prevent the emergence or release of pathogens, and less than 5% of countries scored in the highest tier for ability to respond rapidly to and mitigate epidemic spread.1
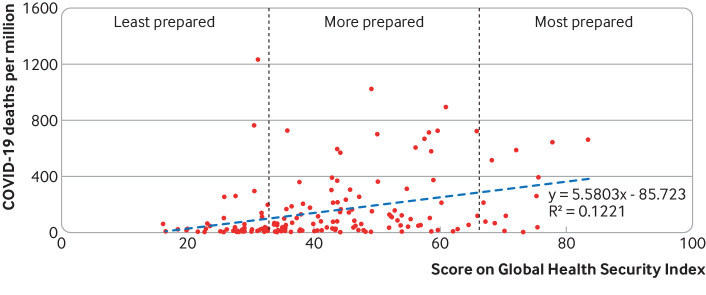
After the US and UK, the Netherlands, Australia, Canada, Thailand, Sweden, Denmark, South Korea, and Finland were the highest scoring countries on the GHSI. A higher GHSI score would be expected to be associated with lower measures of covid-19 burden. However, the GHSI was much less accurate when assessing individual countries. In April 2020 the GHSI score was positively associated with covid-19 cases and deaths, but not related to covid-19 testing rate. As at 19 October 2020, national cumulative death rates from covid-19 were positively related to GHSI score (r=0.35, P<0.001), indicating the persistence of the association (fig 1).
Fig 1.
Relation between Global Health Security Index score and number of covid-19 deaths up to 19 October 2020 (Our World in Data: https://ourworldindata.org/coronavirus)1
Why didn’t the GHSI predict national performance more accurately?
We propose 10 factors that may account for the failure of the GHSI to predict performance in the covid-19 pandemic and provide guidance for the development of a new index on preparedness.
Limited consideration of globalisation, geography, and global governance
The GSHI measures the performance of individual nations. However, given the increasingly globalised and interconnected social and economic world, viruses can spread rapidly despite seemingly good preparedness. The GHSI did not consider the importance of geography. For example, islands nations such as Australia, New Zealand, and Pacific island states could close their borders in an attempt to prevent the virus from entering the country. Major air transport hubs in particular posed risks for increased disease transmission. The GSHI also did not consider the contribution of regional organisations (eg the European Union) or global organisations (eg the G20) to coordinating national responses. Failure to coordinate efforts to stem the spread and impact of the virus has yielded considerable chaos, including shortages of critical commodities such as personal protective equipment, poorly managed population movements, and lack of standardisation of key trade policies. Thus, disease control may be only as effective as practices within the poorest performing countries.4
Bias to high income countries
Researchers in US institutions developed the GHSI, advised by a panel of international experts. Critics of the GHSI argued the experts’ emphasis on biosafety over other capacities reflects a bias to high income countries.4 5 6 For example, there is tension between biosecurity focused, authoritarian approaches to public health and more comprehensive, social determinants driven, participatory and rights based approaches, which require effective community participation.7 The pandemic has highlighted the importance of the latter and the need to involve a broad range of experts from different backgrounds, including civil society, to develop and implement an effective response to a public health crisis.
Failure to assess health system capacity
Nations with universal publicly funded health systems that were not financially distressed and had strong public health capacity seem to have been relatively well prepared for covid-19: these include Thailand, Vietnam, Australia, and New Zealand. Conversely, the pandemic highlighted the weaknesses of fragmented systems relying on for-profit healthcare providers, such as in the US. Covid-19 exposed fragile and chronically underfunded public health systems and weak pandemic preparedness activities. England outsourced testing and tracing to private companies with no relevant experience, which created a fragmented system separate from existing health service, university, and veterinary laboratories and from those experienced in contact tracing in local government or sexual health clinics. The tracing system in particular performed poorly, using a telephone based system that ignored the importance of the local knowledge of contact tracers, termed “shoe leather epidemiology.”8 The result was an ineffective and fragmented programme which hampered efforts to control the outbreak. These factors also highlight the importance of being able to draw on a well functioning public health system.9 Vietnam, whose public health system emphasises care, solidarity, and community responsibility, has had low covid-19 cases and death rates although it scored low on the GHSI (50th place; score 49.1).
Role of political leadership
The GHSI measures trust in government, but it overlooked the role that political leadership and ideology plays in shaping public health responses.10 The GHSI rated New Zealand lower than many other high income countries (35th place; score 54.0). Yet many praise Prime Minster Ardern’s strong political leadership during the covid-19 crisis, especially her empathic and clear communication to the public and evidence based response. By contrast, other leaders, including in the US and Brazil, failed to accept scientific public health advice, including mask wearing and social distancing, promoted unproved therapies, and criticised the World Health Organization. In the UK, rated second highest on the GHSI, the covid-19 response was hampered by the process of leaving the European Union, which dominated the attention of politicians and efforts of civil servants.11 The perils of populist leaders in pandemic responses have been previously highlighted.12
Assessing political leadership and philosophy may risk politicising the index and opening it to criticism from countries with low scores. However, existing frameworks for assessing the quality of a country’s governance,13 effectiveness,14 and transparency can be drawn on.15 Examples of poor governance during covid-19 include the growing concern about corruption in the procurement of essential equipment and the absence of transparency when contracting with private companies.16 Given the vital importance of trust during a pandemic, political leaders who promote transparent government are more likely to mount a more effective response.
Importance of context overlooked
Consideration of context is key to the accurate assessment of health interventions.17 18 Yet to allow for cross country comparisons, indices often reduce complex systems to a standard set of measures that overlook important differences, such as dynamic political, economic, and social structures and systems6
The context can include the degree of centralisation of power. New Zealand and Vietnam have centralised governments, and both fared well in response to covid-19. Some federated states including India, the US, Belgium, Australia, and South Africa have pandemic responses that have varied in effectiveness across the country and point to the value of national coordination. Italy’s regional structure allowed it to largely contain the pandemic in the north of the country during the first wave.19 However, this containment broke down in the summer as Italians went on holiday20 and exposed weaknesses in the regional health infrastructure and preparedness in regions that had escaped the initial wave.21 Future predictive work would benefit from a qualitative, context assessment of each country, informed by a range of expertise.
Limits of national wealth as predictive factor
The GHSI report noted a positive correlation between gross domestic product (GDP) (0.37) and GDP per capita (0.44) and the GHSI score.1 But national wealth may not be the only or main determinant of health security. Lower income countries may allocate their scarce resources more appropriately and tailored to context.5 6 In Rwanda, a strong health system, rapid lockdown, and effective contact testing and testing of staff at national borders and those working in public spaces, such as banks and bars, have kept cases low and no deaths have been recorded.22 Similarly, despite Vietnam’s low GDP it has had a highly effective pandemic response. Such outcomes confirm earlier analyses that low income countries can use their resources efficiently and innovatively to achieve good health.23
No examination of inequalities within countries
The covid-19 pandemic has heightened pre-existing inequalities in many countries. Most nations reported minority populations being most vulnerable. In the US, black, Hispanic, and Native American people were more susceptible to infection, severe illness, hospitalisation, and death.24 25 26 In Australia, recently arrived migrants faced greater risk,27 while minority ethnic groups bore a high burden in the UK.28 In South Africa most infection hot spots arose in high density, overcrowded settlements with poor access to water and other basic services and heavy reliance on cramped private taxi transport in the absence of any public transport.29 In Brazil, social inequities and structural racism placed pregnant and postpartum black women at higher risk of death.30 Everywhere, marginalised people and those living in precarious situations tend to fall through the cracks in the social safety nets, find it harder to isolate when required, and cannot avoid settings where the risks of infection are high. Marginalised people also face the risk of losing their jobs and housing, fail to qualify for social security, and face food insecurity. Future iterations of the GHSI should include measures of the scale and nature of inequalities within a country.
Importance of social security provisions
The covid-19 pandemic has highlighted the importance of social security provisions to protect people from losing their jobs and homes, yet the GHSI does not consider them in its assessment. Government support to people and businesses affected by covid-19 has been important. For example, in many high income countries, unemployment benefits and job and income support schemes have protected many from extreme poverty, whereas in most low and middle income countries such income protection does not exist. In India the absence of government support forced tens of thousands of migrant workers to return to their home villages. Some died and many faced police harassment and hunger. In many countries the availability of sick leave has been an effective public health measure as people without this provision have found it difficult to follow public health advice to self-isolate. Including measures of social protection would improve future indices.
Civil society capacity not assessed
The GHSI did not assess the capacity of civil society organisation to assist in pandemic responses. Social solidarity built on civil society engagement can offer protection even where trust in government is weak. For example, in South Africa, Cape Town’s community action networks are working to both ameliorate the consequences of lockdown and reduce local transmission. Using social media, they built local relationships based on trust and challenged divisive individualism by creating a collective consciousness for responses to covid-19 related issues.31 Societies can also create political space for civil society and social movement activists to protest human rights abuses, which often increase under the cover of exceptional or emergency pandemic measures.32 Future exercises should include civil society perspectives and their potential to respond to pandemics.
Gap between capacity and its application not assessed
Although the GHSI assessed the theoretical capacity of a country to respond to a pandemic it did not examine the actual capacity and willingness to respond. For example, the US scored high on applied epidemiology training programmes (indicators 2.3.1) but political intervention prevented the Centres for Disease Control and Prevention from applying epidemiological science to responses to the pandemic. A complex system is only as strong as its weakest point. Preparedness assessments based on system critical components discussed here work best.
Conclusion
The GHSI report accurately predicted that the world was not well prepared for a pandemic. However, the complex country responses to covid-19 and biases within the GHSI limited the accuracy of its predictions for specific countries. To strengthen the predictive capabilities of global indices, a diverse team of experts should be used to assess the complex set of factors that shape a country’s capacity to respond.
Other vital indicators needed in future global indices to assess a country’s likely capacity for a robust response to a pandemic include the extent of inequities in a country, the strength of social protection and public health response capacity, the geographic context, and exposure to globalisation. Qualitative assessment of a country’s capacities in terms of its political leadership’s willingness to accept scientific advice and the strength of its civil society to protect human rights and foster trust is also important. Existing measures of corruption and trust should be used in future indices. The need for cross border cooperation and joint planning of future assessments of global pandemic preparedness point to the need to examine the capacity of supra-national organisations. The crucial lesson from the covid-19 pandemic is that an effective response does not rely just on a strong public health system but also requires a society that is fair and offers all its citizens and residents social and economic security.
Contributors and sources: FB conceived the article and wrote the first draft. The team builds on an existing network of researchers—the Punching Above Weight Network, which has considered why some countries achieve higher health status than their economic performance would suggest. TF and JF contributed to the first draft, conducted the quantitative analysis, and read and approved the final version. CM contributed to the first draft and approved the final version. MA, WDeC, SF, CG, PHC, NTH, LL, MM, JP, HS, and EV commented on each draft and approved the final manuscript.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare. CM’s time was funded by a grant from the World Bank.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of a collection launched at the Prince Mahidol Awards Conference (PMAC) in January 2021. Funding for the articles, including open access fees, was provided by PMAC. The BMJ commissioned, peer reviewed, edited, and made the decision to publish these articles. David Harper and an expert panel that included PMAC advised on commissioning for the collection. Rachael Hinton and Kamran Abbasi were the lead editors for The BMJ.
References
- 1.Nuclear Threat Initiative. Global Health Security Index website. Johns Hopkins Center for Health Security and The Economist Intelligence Unit, 2019.
- 2. Oppenheim B, Gallivan M, Madhav NK, et al. Assessing global preparedness for the next pandemic: development and application of an Epidemic Preparedness Index. BMJ Glob Health 2019;4:e001157. 10.1136/bmjgh-2018-001157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Boyd MJ, Wilson N, Nelson C. Validation analysis of Global Health Security Index (GHSI) scores 2019. BMJ Glob Health 2020;5:e003276. 10.1136/bmjgh-2020-003276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aitken T, Chin KL, Liew D, Ofori-Asenso R. Rethinking pandemic preparation: Global Health Security Index (GHSI) is predictive of COVID-19 burden, but in the opposite direction. J Infect 2020;81:318-56. 10.1016/j.jinf.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dalglish SL. COVID-19 gives the lie to global health expertise. Lancet 2020;395:1189. 10.1016/S0140-6736(20)30739-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Razavi A, Erondu N, Okereke E. The Global Health Security Index: what value does it add? BMJ Glob Health 2020;5(e002477):e002477. 10.1136/bmjgh-2020-002477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Loewenson R, Accoe K, Bajpai N, et al. Reclaiming comprehensive public health. BMJ Glob Health 2020;5:e003886. 10.1136/bmjgh-2020-003886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Koo D, Thacker SB. In snow’s footsteps: Commentary on shoe-leather and applied epidemiology. Am J Epidemiol 2010;172:737-9. 10.1093/aje/kwq252. [DOI] [PubMed] [Google Scholar]
- 9. Scally G, Jacobson B, Abbasi K. The UK’s public health response to covid-19. BMJ 2020;369:m1932. 10.1136/bmj.m1932. [DOI] [PubMed] [Google Scholar]
- 10. Tesh S. Hidden arguments: political ideology and disease prevention policy. Rutgers University Press, 1988. [Google Scholar]
- 11.Hopkin J. Brexit thinking poisoned the government’s response to COVID-19. LSE, 2020. https://blogs.lse.ac.uk/brexit/2020/06/09/brexit-thinking-poisoned-the-governments-response-to-covid-19/
- 12. McKee M, Gugushvili A, Koltai J, et al. Are populist leaders creating the conditions for the spread of COVID-19? Comment on “A scoping review of populist radical right parties’ influence on welfare policy and its implications for population health in Europe.” Int J Health Policy Manage 2020.. [Epub ahead of print.] 10.34172/ijhpm.2020.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greer SL, Wismar M, Figueras J, et al. Governance: a framework. In: Greer SL, Figueras J, Wismar M, eds. Strengthening health system governance. Open University Press, 2016: 27-56. [Google Scholar]
- 14.World Bank. Worldwide governance indicators 2020. https://info.worldbank.org/governance/wgi/
- 15.Transparency International. Corruption perceptions index 2020. https://www.transparency.org/en/cpi#
- 16.Good Law Project. COVID-19 2020. https://goodlawproject.org/issues/covid-19/
- 17. Pawson R, Tilley R. Realistic evaluation. Sage, 1997. [Google Scholar]
- 18.Poland B, Frohlich KL, Cargo M. Context as a fundamental dimension of health promotion program evaluation. Health promotion evaluation practices in the Americas. Springer, 2008: 299-317 10.1007/978-0-387-79733-5_17. [DOI] [Google Scholar]
- 19. Boccia S, Cascini F, McKee M, Ricciardi W. How the Italian NHS is fighting against the COVID-19 emergency. Front Public Health 2020;8:167. 10.3389/fpubh.2020.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Casini L, Roccetti M. A cross-regional analysis of the COVID-19 spread during the 2020 Italian vacation period: reasults from three computational models are compared. Sensors (Basel) 2020;20:E7319. 10.3390/s20247319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Paterlini M. Covid:19: Italy has wasted the sacrifices of the first wave, say experts. BMJ 2020;371:m4279. 10.1136/bmj.m4279. [DOI] [PubMed] [Google Scholar]
- 22. Condo J, Uwizihiwe JP, Nsanzimana S. Learn from Rwanda’s success in tackling COVID-19. Nature 2020;581:384. 10.1038/d41586-020-01563-7. [DOI] [PubMed] [Google Scholar]
- 23. Balabanova D, Mills A, Conteh L, et al. Good health at low cost 25 years on: lessons for the future of health systems strengthening. Lancet 2013;381:2118-33. 10.1016/S0140-6736(12)62000-5. [DOI] [PubMed] [Google Scholar]
- 24. Moore JT, Ricaldi JN, Rose CE, et al. COVID-19 State, Tribal, Local, and Territorial Response Team Disparities in incidence of COVID-19 among underrepresented racial/ethnic groups in counties identified as hotspots during June 5-18, 2020—22 states, February-June 2020. MMWR Morb Mortal Wkly Rep 2020;69:1122-6. 10.15585/mmwr.mm6933e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The Covid Tracking Project. Racial data dashboard. Atlantic Monthly Group, 2020. https://covidtracking.com/race/dashboard
- 26.Wood D. As pandemic deaths add up, racial disparities persist—and in some cases worsen. NPR 2020 Sep 23. https://www.npr.org/sections/health-shots/2020/09/23/914427907/as-pandemic-deaths-add-up-racial-disparities-persist-and-in-some-cases-worsen?t=1611567042072
- 27.Commonwealth of Australia. Department of Health. Coronavirus (COVID-19) current situation and case numbers 2020. https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-current-situation-and-case-numbers#cases-and-deaths-by-age-and-sex
- 28. Martin CA, Jenkins DR, Minhas JS, et al. Leicester COVID-19 consortium Socio-demographic heterogeneity in the prevalence of COVID-19 during lockdown is associated with ethnicity and household size: Results from an observational cohort study. EClinicalMedicine 2020;25:100466. 10.1016/j.eclinm.2020.100466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Karim A. No water, no room: containing an outbreak in South Africa. Bhekisisa, 2020. [Google Scholar]
- 30. Santos DS, Menezes MO, Andreucci CB, et al. Disproportionate impact of COVID-19 among pregnant and postpartum black women in Brazil through structural racism lens. Clin Infect Dis 2020;ciaa1066. [Epub ahead of print.] 10.1093/cid/ciaa1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scheepers E, Lakhani E, Armstrong K. Making a community action net (work): organising in the times of COVID-19. OpenGlobalRights, 2020.
- 32.United Nations. Human Rights. COVID-19: Exceptional measures should not be cover for human rights abuses and violations – Bachelet 2020. https://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=25828