Abstract
Background:
The novel coronavirus disease (COVID-19) has created obstacles for medical student education, as clinical rotations were temporarily halted. Recent literature shows online electives may provide an alternative learning platform. We developed a tele-ophthalmology student elective for rising third-year (MS3) and fourth-year (MS4) medical students to continue teaching and exposure to the field.
Methods:
A 4-week remote elective was approved by Emory University School of Medicine and offered between April 18, 2020 to May 15, 2020 for rising MS3 and MS4 students. The curriculum consisted of online self-study materials, student presentations, chart review assignments, case-based discussions with faculty, and telehealth experiences. All students were surveyed and tested with questions from USMLE World (UWorld) test bank at the end of the course.
Results:
A total of 18 students enrolled, with 66.7% MS3 and 33.3% MS4 participance. The mean rating of fulfillment of course learning objectives was 8.1/10 (range, 6.7–8.8), with mean ratings of 8.2 for MS3s and 7.7 for MS4s. There was a significant increase in self-reported knowledge in ophthalmology, with an increase from 4.6 to 8.1 for MS3s (p=0.002) and 6.7 to 8.0 for MS4s (p=0.04). Students also reported higher interest in the field, with an increase from 4.9 to 7.8 for MS3s (p=0.01) and 7.5 to 8.7 for MS4s (p=0.1). The students performed significantly higher on the post-course test (94.8%) than UWorld question bank users (74.1%) (p<0.001).
Conclusion:
Our novel ophthalmology elective significantly enhanced self-reported medical student knowledge and interest in the field during a crisis that required transition to remote learning. Further study of student telehealth experience and objective assessment is needed to improve online learning in ophthalmology.
Introduction
The SARS-CoV-2 pandemic began in Wuhan, China near the end of 2019 and led to unprecedented changes in medicine.1–2 As social distancing measures were implemented, medical schools were forced to consider the implications coronavirus (COVID-19) would have on the structure of medical education.3 On March 17th, the Association of American Medical Colleges recommended to pause all medical student clinical activities.4 This led to rising third- and fourth-year medical students to turn to virtual learning, instead of hands-on education in the hospital.
Medical students interested in ophthalmology have been significantly impacted by these changes due to the limited exposure students have to the field.5–7 Ophthalmology is not unique among medical specialties that rely on physical provider-patient interaction. However, common ophthalmic screening can be performed virtually. There is an opportunity for students to be incorporated into telehealth initiatives. Coupled with online learning, this model could teach clinical pearls and familiarize the student with virtual healthcare.
Online learning models have shown to be successful in other fields of medicine.8 In one study, the online platform Zoom© has shown to be effective in team-based learning for pathology, with a 96.5% attendance rate and an 85% satisfaction.9 In another institution, video-conferencing software Google Hangouts© is used to teach clinical anatomy.10 Surgical departments in the United States have been adapting remote curricula in topics such as neurosurgery.8 These efforts highlight the potential of online teaching during this unprecedented time.
It is clear that the absence of medical students in the clinical environment has negatively impacted medical education during COVID-19. Thus, there is a need to restructure ophthalmic medical education. Here, we present a 4-week novel ophthalmology curriculum for clinical medical students, which begins to explore the integration of students into telemedicine platforms and provides both group and self-study sessions.
Methods
This study was approved by the Emory University Institutional Review Board (00000487). Between April 18, 2020 and May 15, 2020, a 4-week tele-ophthalmology elective was offered to Emory University School of Medicine rising third (MS3) and fourth-year (MS4) medical students via the video-conference software Zoom (San Jose, CA). The elective was one of 34 virtual electives offered during COVID-19 to mitigate educational interruptions. Other electives were 1–4 weeks in length and topics ranged from the coronavirus pandemic and epidemiology to specialty-specific courses in medicine and surgery. The course was co-directed by the school’s director of medical student education (E.B.G.) and Grady Memorial Hospital’s chief of ophthalmology (Y.M.K.). The elective was proposed and organized by 2 rising MS4s (S.N.D. and O.E.U.).
Course Curriculum
The elective’s mission was to promote continued learning in ophthalmology through 6 different learning objectives (LOs) (Table 1). There were no course prerequisites required for enrollment. The elective was graded on a pass-fail system. Course requirements included completion of self-study and chart review assignments, a peer presentation, and attendance at all in-class activities and didactics sessions.
Table 1.
Tele-ophthalmology course learning objectives.
| 1 | To familiarize students with components of the history and physical specific to ophthalmology. |
| 2 | To learn differences between tele-visits and in-person ambulatory ophthalmology visits. |
| 3 | To identify “high-risk” ophthalmic conditions prioritized in televisits. |
| 4 | To become acquainted with the management of high-risk ophthalmic conditions. |
| 5 | To extract relevant data from medical records for tele-ophthalmology visits. |
| 6 | To engage with ophthalmology faculty and/or patients through Zoom. |
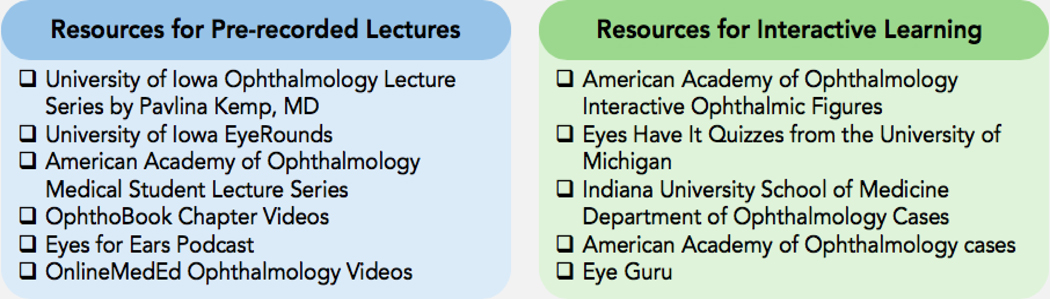
The first component of the course was online self-directed learning, which consisted of pre-recorded lectures and interactive online activities (Figure 1). The first week provided an introduction to the eye and covered topics on red eye and acute vision loss. The second week focused on chronic vision loss, systemic disease, glaucoma, and retinal diseases. The third week concentrated on orbital trauma and oculoplastic surgery. The final week was devoted to pediatric ophthalmology, neuro-ophthalmology, and ocular oncology. Students were required to submit proof of completion of interactive online activities.
Figure 1:
Resources utilized for self-study activities.
The second component was student presentations held twice a week. Each student gave a 15-minute case-based session to teach fellow students about an ophthalmic disease. They were tasked to discuss if the case was “high-risk” and should be seen emergently, urgently, or remotely via telemedicine. Topics chosen by MS4 course organizers included bacterial conjunctivitis, corneal ulcer, uveitis, age-related macular degeneration, diabetic retinopathy, retinal detachments, retinal vascular occlusions, primary open and angle closure glaucoma, ocular chemical burns, ptosis, lacrimal disease, nystagmus, strabismus, diplopia, ischemic optic neuropathies, optic neuritis, and ocular melanoma. Presentations were evaluated by the MS4 course organizers, with additional 5 minutes of live feedback from peers.
The third component was case-based discussions led by department faculty. There were 8 discussions: Acute vision loss, red eye, chronic vision loss, oculoplastic surgery, ocular trauma, neuro-ophthalmology, pediatric ophthalmology, and ocular oncology. Each session was 1 hour. Students were required to attend each session with audio and video settings turned on and participate in discussions. Faculty were provided with open-access American Academy of Ophthalmology (AAO) faculty discussion slides but were permitted to use their own presentations.
The fourth component was optional telehealth observations at Emory Eye Center, offered in the fourth week. All interested students were required to complete the Emory Healthcare “Telehealth for Providers” online training. Each visit started with a video discussion between the patient and ophthalmic technician, who asked if the patient would be comfortable with a learner present. If so, the technician e-mailed the Zoom link of the virtual room to the student and formed a 3-screen Zoom conference. The student took the history and performed a focused ophthalmic exam, as the technician recorded the findings and conducted additional tests. Once the technician exited, the faculty member virtually entered the room. The student presented the findings and repeated parts of the exam requested. Each encounter was followed by a 5-minute feedback session with the technician and faculty member.
The fifth component was chart review activities. All students with access to the electronic medical record (EMR) platform engaged in remote chart review projects aimed at helping the residents working at the Grady Eye Center during the COVID-19 outbreak. Through review of medical records, students created lists of patients with “high-risk” conditions who required prompt evaluation. Each student was assigned 15 patient charts per week and assignments were reviewed by the MS4 course organizers for completion.
Student Assessment
An anonymous electronic post-course survey was made on Google Forms (Mountain View, CA) and distributed to students via email (Table S1). Each survey had 20 questions, including 11 10-point Likert scale questions. All students completed an electronic informed consent. Each survey contained baseline demographic characteristics, such as perceived knowledge level and interest in ophthalmology. Questions about LOs and free-response feedback were incorporated. Students who participated in a televisit were asked to comment on their experiences. An anonymous post-course multiple-choice test was also distributed (Table S2). The test consisted of 15 multiple choice questions selected from the United States Medical Licensing Exam World (UWorld) Step 2 Clinical Knowledge (CK) question bank (Dallas, TX). This subscription-based board review question bank is commonly used by clinical students nationwide.11 Each question evaluated a topic covered by the curriculum. The answer and mean user score for each question were obtained by the medical student course organizers, who had personal access to the question bank.
Statistical Analysis
The survey and test data were visualized on Microsoft Excel (Microsoft, Seattle, WA). Descriptive data analysis on student characteristics of interest was conducted. Preliminary Shapiro-Wilk tests revealed non-parametric distribution for all data groups and subgroups. Thus, the Mann Whitney U test was used for independent continuous data, Wilcoxon signed rank test for paired continuous data, and Fisher’s exact test for categorical data. All analyses were conducted using XLSTAT for Microsoft Excel (Addinsoft, Paris, France), with a p-value of significance set at 0.05.
Results
A total of 18 students enrolled in the 4-week elective. All students completed the course survey and test. Eleven students (61.1%) were women and 7 were men. Eleven (61.1%) students identified as white. There were 12 rising MS3s and 6 rising MS4s. The mean (SD) age was 24.8 (2.1) years. Most students were comfortable using Zoom. Age and gender of students were not significantly different between groups. A higher number of MS4s planned to apply to ophthalmology residency and reported higher baseline interest compared to MS3s, yet the difference did not meet statistical significance for either endpoint. However, MS4s reported a significantly higher baseline knowledge in the field than MS3s (p=0.02). Baseline class characteristics are provided in Table 2.
Table 2.
Baseline characteristics of 18 students in the tele-ophthalmology course.
| Characteristic | Class (n=18) | MS3 (n=12, 66.7%) | MS4 (n=6, 33.3%) | P |
|---|---|---|---|---|
| Mean Age- years (range) a | 24.8 (2.1) | 24.4 (2.4) | 25.5 (1.0) | 0.07 |
| Female sex- no./total no. (%) a | 11 (61.1) | 7 (58.3) | 4 (66.7) | 1.0 |
| Race- no. White/ total no. (%) a | 11 (61.1) | 5 (41.2) | 6 (100.0) | 0.1 |
| Planning to apply to ophthalmology residency- no./total no. (%) a | 8 (44.4) | 4 (33.3) | 4 (66.7) | 0.3 |
| Perceived knowledge in ophthalmology (SD) b,c | 5.3 (1.7) | 4.6 (1.1) | 6.7 (2.1) | 0.02 |
| Interest in ophthalmology (SD) b,c | 5.8 (2.8) | 4.9 (2.9) | 7.5 (1.8) | 0.07 |
| Comfort level using Zoom teleconferencing (SD) b,c | 9.2 (1.1) | 9.0 (1.2) | 9.5 (0.8) | 0.4 |
MS3: Third-year medical student. MS4: Fourth-year medical student.
Comparison using Fisher’s exact test between MS3 and MS4.
10-point Likert scale, with 1 indicating low and 10 indicating high.
Comparison using Mann Whitney U test between MS3 and MS4.
Fulfillment of Learning Objectives
The majority of students favorably reviewed the course and its fulfillment of LOs, with a mean overall rating of 8.1 (range, 6.7–8.8). The ratings (SD) were 8.6 (1.3), 7.3 (1.5), 8.8 (1.2), 8.6 (1.4), 8.3 (1.6), and 6.7 (10) for LOs 1–6, respectively. MS3s reported equal or higher ratings across all LOs compared to MS4s, with mean overall ratings of 8.2 for MS3s and 7.7 for MS4s. A statistically larger number of MS3s reported the course met LO5 “extracting data from electronic patient charts” compared to MS4s, with ratings of 8.8 and 7.5 for MS3s and MS4s, respectively (p=0.02) (Table S3).
Ophthalmology Knowledge and Interest
Overall, the mean (SD) baseline self-reported ophthalmic knowledge of the class was 5.3 (1.7), with ratings of 4.6 (1.1) by MS3s and 6.7 (2.1) by MS4s (Table 3). There was a significant increase in self-reported knowledge following course completion, with a mean (SD) class rating of 8.1 (1.1) (p<0.001). Students from both academic years reported significant enhancement in knowledge, with final reported ratings of 8.1 (0.9) (p=0.002) and 8.0 (1.4) (p=0.04) for MS3s and MS4s, respectively.
Table 3.
Baseline and post-course comparison of ophthalmology interest and knowledge by student academic year.
| Study Group | Mean Baseline Knowledge (SD) | Mean Post-Course Knowledge (SD) | P a | Mean Baseline Interest (SD) | Mean Post-Course Interest (SD) | P a |
|---|---|---|---|---|---|---|
| Class (n=18) | 5.3 (1.7) | 8.1 (1.1) | <0.001 | 5.8 (2.8) | 8.1 (1.3) | 0.003 |
| MS3 (n=12, 66.7%) | 4.6 (1.1) | 8.1 (0.9) | 0.002 | 4.9 (2.9) | 7.8 (1.3) | 0.01 |
| MS4 (n=6, 33.3%) | 6.7 (2.1) | 8.0 (1.4) | 0.04 | 7.5 (1.8) | 8.7 (1.2) | 0.1 |
MS3: Third-year medical student. MS4: Fourth-year medical student.
Comparison using Wilcoxon signed rank test.
Similar to baseline knowledge, the mean (SD) baseline interest of the class was rated at 5.8 (2.8), with mean MS3 rating of 4.9 (2.9) and mean MS4 rating of 7.5 (1.8) (Table 3). A 2.3 point-increase in ophthalmology interest was observed, with a final mean (SD) class rating of 8.1 (1.3) (p=0.003). Both student groups reported an increase in interest in the field, with final mean (SD) ratings of 7.8 (1.3) and 8.7 (1.2) for MS3s and MS4s, respectively. The 2.9-point increase in MS3 interest was significantly higher than baseline rating (p=0.01). However, the 1.2-point increase in MS4 interest did not achieve significance (p=0.1).
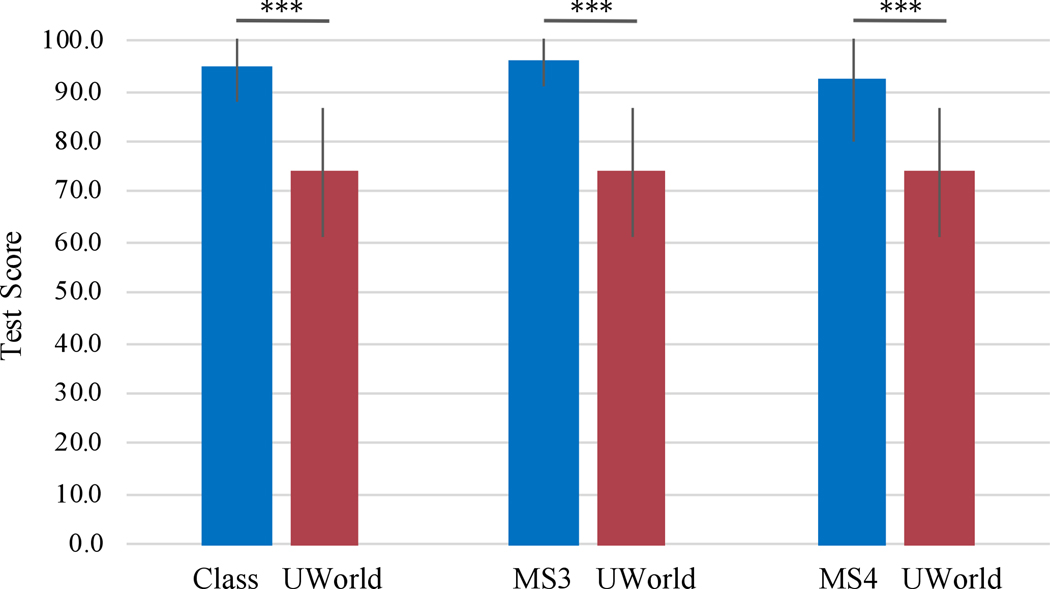
For the post-course test, the mean class score (SD) was 94.8 (7.1), with a range of 77.8–100.0. The mean score for UWorld users for the 15-question test was 74.1 (12.9), with a range of 50.0–94.0. Overall, the class performed significantly higher than the average UWorld user (p<0.001). This significance persisted when the class were grouped by academic year (Figure 2). The class demonstrated higher scores than UWorld users for each topic. There was no significant difference between MS3 (SD) and MS4 (SD) performance, which were 96.1 (5.3) and 92.2 (12.2), respectively (p=0.35).
Figure 2.
Test results of the overall class, MS3s, MS4s, and UWorld users. Error bars reflect standard deviation. Comparison using Mann Whitney U test. MS3: Third-year medical student. MS4: Fourth-year medical student. UWorld: USMLE World Step 2 Clinical Skills question bank. ***p<0.001.
Telehealth Experience and Chart Review Activities
Eleven out of 18 (61.1%) students observed a telehealth experience. When the class was stratified by telehealth observation, there were no significant differences in baseline parameters and most LO ratings between observers and non-observers. However, LO5, “extracting relevant data from electronic patient charts” was rated significantly higher by telehealth participants, with a mean (SD) score of 9.0 (1.4) compared to 7.9 (1.6) for non-participants (p=0.03). Ten (90.9%) telehealth observers responded to the open-response questions. Seven students highlighted positive interactions with faculty. Five students suggested areas of improvement, including increasing the number of visits and providing students with the patient charts prior to each visit.
Fifteen out of 18 (83.3%) students engaged with patient care virtually through participation in the chart review activities. The weekly chart assignments aided residents and faculty in triaging which patients needed to be seen urgently in clinic or via telehealth visits. While helpful to the residents, these chart review activities received mixed reviews from students. Two students enjoyed this component of the course, citing its utility in offering an introduction to the EMR system prior to starting clinical rotations. However, two students did not see educational benefit in the chart review activities, and one additional student suggested coupling chart review activities with telehealth visits for increased student engagement.
Qualitative Responses
A total of 17 (94.4%) students delivered open-response feedback. Fourteen students praised the chosen self-study learning materials, 7 students applauded the course organization, 5 students liked case-based discussions, 5 students reported they enjoyed peer presentations, and 3 students appreciated the flexibility of the course schedule. There were several suggestions for improvement. Eleven students mentioned increasing time with faculty members. Three students suggested making peer presentations more interactive, either by having a faculty liaison or the presenter calling on other students.
Discussion
A month-long remote course was successfully implemented during COVID-19 to promote learning in ophthalmology. There was a significant increase in self-reported knowledge for MS3s and MS4s. In addition, self-reported interest in ophthalmology increased significantly for MS3s. The class performed significantly higher in ophthalmology questions than UWorld Step 2 CK question bank users. Our study suggests remote electives may have great potential to enhance student education, knowledge, and interest in ophthalmology.
Overall, the course was well-received. Open-response survey questions demonstrated high student satisfaction with course organization and quality of teaching materials. Students praised the utility of peer presentations and faculty discussions. An area of improvement was standardizing faculty discussions. Though faculty were provided with cases, they were encouraged to utilize their own materials to permit innovative teaching. The feedback suggests that a structured approach to learning is favored. It also advocates for a centralized curriculum in the field. An open-source website with pre-recorded lectures, standardized slides, and questions for discussion can augment our elective, as well as virtual learning across institutions. Additional course improvements could be made via faculty feedback on student engagement.
Over half of the class participated in a televisit. Many students noted the number of telehealth experiences should be increased to once or twice per week. This is not surprising, as these observations were only offered in the last week due to technical difficulties. Thus, each student was only able to observe a single visit. Pairing students with clinicians at least a week prior to the visit can also enhance the experience. Seven students chose to not observe a visit. This cannot be attributed to low self-reported interest alone, as a stratified analysis showed no significant difference between televisit participants and non-participants. This result may be due to scheduling conflicts outside of the elective, as students were asked to sign up towards the end of the third week. It is also possible that students were not quarantined in a space to conduct a professional virtual visit, preferring self-study activities.
It is important to acknowledge concerns regarding trainee involvement in the virtual ophthalmic exam. Tele-ophthalmology poses many challenges to ophthalmologists. Lack of access to diagnostic equipment restricts patient management strategies. Most providers do not have previous telehealth training, so some may not precept a learner until they are comfortable with using the virtual platform. Due to similar reasons, some patients may not wish to have a trainee in the virtual room. As the comfort levels of patients and providers improve, so will the opportunities for trainees.
The lessons learned in this course are not only applicable to crises that require transition to remote learning, but also for contemporary medical education. The utility of in-person lectures compared to online lectures has been debated.12–14 Prior to COVID-19, many medical schools had witnessed a decline in student attendance, likely in part due to increased emphasis on licensing exams by residency programs.15–17 In the ever-changing landscape of medical education, remote courses may become permanent or combined with clinical experiences.18–20 At our institution, for example, we created an in-person/telehealth hybrid model for the MS3 ophthalmology curriculum.21 Though we have not offered the elective to a second cohort, our course design offers an alternative to the traditional “away” rotation. As the entire curriculum can be conducted remotely, it can aid students without ophthalmology programs at their home institution. It can also provide mentorship and career development opportunities to faculty, who wish to train the next generation of ophthalmologists.
Our study’s strengths include its large sample size and current relevance of remote medical education. To our knowledge, this is the first distance-learning 4-week course in ophthalmology implemented during COVID-19. With a sample size of 18 students between two academic years, we were able to collect substantial quantitative and qualitative information on course effectiveness and areas of improvement.
The largest limitation of our study is the lack of a pre-course survey. Our results were acquired from post-hoc reflection, limiting internal validity. However, comparison of post-test results with UWorld users provides an objective assessment of student performance and increases external validity. The test bank users may also be limited as a control group. Most UWorld users test their ophthalmology knowledge with randomly generated questions across multiple topics, compared to our students who took a short ophthalmology-specific quiz. Additionally, our study may be subject to selection bias. Given these students chose our particular elective, they were likely more interested in ophthalmology compared to the medical student population. This is evident from the moderate MS3 and high MS4 self-reported baseline interest. In spite of limitations, the improvement in self-reported knowledge and interest underscores the success of our curriculum.
In summary, we present a remote ophthalmology curriculum for medical students shown to be successful during COVID-19. This curriculum may be helpful to educators worldwide, who wish to introduce the field to students or integrate an online curriculum with a clinical ophthalmology course. Studies of telehealth experience and objective assessment are needed to further explore the potential of remote learning in ophthalmology, as COVID-19 continues to transform medical education.
Supplementary Material
Acknowledgements:
The authors thank Pavlina Kemp, MD and other educators who have contributed to open-access ophthalmology medical student education platforms incorporated in this study.
Funding: This work was supported by an unrestricted departmental grant to the Emory Eye Center from Research to Prevent Blindness (New York, NY) and by National Eye Institute Core Grant P30 EY006360.
Footnotes
Conflict of Interest: None declared.
References:
- 1.Centers for Disease Control and Prevention. 2020. Coronavirus Disease 2019 (COVID-19) In The U.S. [online] Available at: <https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html> [Accessed 21 May 2020]
- 2.Rose S. Medical Student Education in the Time of COVID-19. JAMA. March 2020. doi: 10.1001/jama.2020.5227 [DOI] [PubMed] [Google Scholar]
- 3.Miller DG, Pierson L, Doernberg S. The Role of Medical Students During the COVID-19 Pandemic. Annals of Internal Medicine. 2020. doi: 10.7326/m20-1281 [DOI] [PubMed] [Google Scholar]
- 4.Whelan A, Prescott J, Young G, et al. Interim guidance on medical students’ participation in direct patient contact activities: principles and guidelines. 2020. AAMC. [online] Available at: <https://lcme.org/wp-content/uploads/filebase/March-30-2020-Interim-Guidance-on-Medical-Students-Participation-in-Direct-Patient-Contact-Activities.pdf> [Accessed 21 May 2020]
- 5.Shah M, Knoch D, Waxman E. The State of Ophthalmology Medical Student Education in the United States and Canada, 2012 through 2013. Ophthalmology. 2014;121(6):1160–1163. doi: 10.1016/j.ophtha.2013.12.025 [DOI] [PubMed] [Google Scholar]
- 6.Graubart EB, Waxman EL, Forster SH, et al. Ophthalmology Objectives for Medical Students: Revisiting What Every Graduating Medical Student Should Know. Ophthalmology. 2018;125(12):1842–1843. doi: 10.1016/j.ophtha.2018.08.032 [DOI] [PubMed] [Google Scholar]
- 7.Succar T, Grigg J, Beaver HA, Lee AG. Advancing ophthalmology medical student education: International insights and strategies for enhanced teaching. Surv Ophthalmol. 2020;65(2):263–271. doi: 10.1016/j.survophthal.2019.08.006 [DOI] [PubMed] [Google Scholar]
- 8.Dawoud RA, Philbrick B, Mcmahon JT, et al. Letter to the editor regarding “Challenges of Neurosurgery Education During the Coronavirus Disease 2019 (COVID-19) Pandemic: A U.S. Perspective” and a Virtual Neurosurgery Clerkship for Medical Students. World Neurosurg. 2020. doi: 10.1016/j.wneu.2020.05.085 [DOI] [Google Scholar]
- 9.Gaber DA, Shehata MH, Amin HA. Online Team‐ Based Learning Sessions as Interactive Methodologies During The Pandemic. Med Educ. 2020. doi: 10.1111/medu.14198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moszkowicz D, Duboc H, Dubertret C, Roux D, Bretagnol F. Daily medical education for confined students during COVID ‐19 pandemic: A simple videoconference solution. Clin Anat. 2020. doi: 10.1002/ca.23601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giordano C, Hutchinson D, Peppler R. A Predictive Model for USMLE Step 1 Scores. Cureus. 2016;8(9):e769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Billings-Gagliardi S, Mazor KM. Student Decisions about Lecture Attendance: Do Electronic Course Materials Matter? Acad Med. 2007;82(10 Suppl):S73–76. doi: 10.1097/acm.0b013e31813e651e [DOI] [PubMed] [Google Scholar]
- 13.Gupta A, Saks NS. Exploring medical student decisions regarding attending live lectures and using recorded lectures. Med Teach. 2013;35(9):767–771. doi: 10.3109/0142159x.2013.801940 [DOI] [PubMed] [Google Scholar]
- 14.Kauffman CA, Derazin M, Asmar A, Kibble JD. Relationship between classroom attendance and examination performance in a second-year medical pathophysiology class. Adv Physiol Educ. 2018;42(4):593–598. doi: 10.1152/advan.00123.2018 [DOI] [PubMed] [Google Scholar]
- 15.Chen DR, Priest KC, Batten JN, et al. Student perspectives on the “Step 1 climate” in preclinical medical education. Acad Med. 2019;94(3):302–304. doi: 10.1097/ACM.0000000000002565 [DOI] [PubMed] [Google Scholar]
- 16.Ikonne U, Campbell AM, Whelihan KE, Bay RC, Lewis JH. Exodus From the Classroom: Student Perceptions, Lecture Capture Technology, and the Inception of On-Demand Preclinical Medical Education. J Am Osteopath Assoc. 2018;118(12):813. doi: 10.7556/jaoa.2018.174 [DOI] [PubMed] [Google Scholar]
- 17.National Resident Matching Program Data Release and Research Committee. 2018. Results of the 2018 NRMP Program Director Survey. [online] Available at: <https://www.nrmp.org/wp-content/uploads/2018/07/NRMP-2018-Program-Director-Survey-for-WWW.pdf> [Accessed 21 May 2020]
- 18.Wu DJ, Greenberg PB. Self-Directed Preclinical Course in Ophthalmic Surgery. J Surg Educ. 2016; 73(3):370–374 [DOI] [PubMed] [Google Scholar]
- 19.Zuckerman SL, Mistry AM, Hanif R, et al. Neurosurgery Elective for Preclinical Medical Students: Early Exposure and Changing Attitudes. World Neurosurg. 2016;86:120–126. doi: 10.1016/j.wneu.2015.08.081 [DOI] [PubMed] [Google Scholar]
- 20.Reznich CB, Anderson WA. A Suggested Outline for Writing Curriculum Development Journal Articles: The IDCRD Format. Teach Learn Med. 2001;13(1):4–8. doi: 10.1207/S15328015TLM1301_2 [DOI] [PubMed] [Google Scholar]
- 21.Graduation Requirements for the MD Degree. Emory University School of Medicine; <https://med.emory.edu/education/programs/md/student-236-handbook/academics/graduation-requirements.html> [Accessed May 21, 2020] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.