Abstract
Background:
It is imperative to acknowledge that COVID-19 poses significant burden on the psychological well-being of people. With implementation of lockdown and measures like quarantine, the mental health of people is affected, and the associated problems may range from depression to suicidal ideation. With this background, the aim of this study was to assess COVID-19 anxiety among general population of the state of Andhra Pradesh.
Materials and Methods:
This cross-sectional study assessed the COVID-19 anxiety among the population of Andhra Pradesh using COVID-19 Anxiety Scale (CAS-7), a seven-item validated psychometric instrument which assesses the cognitive, emotional, and physiological dimensions of COVID-19 anxiety, using a semantic differential scale. The final sample constituted 1,346 participants. Statistical analysis was done using SPSS version 20 software (IBM SPSS statistics for Windows version 20, Armonk, NY, USA).
Results:
The mean age of the study participants was 36.13 ± 10.2 years, and 55.8% were males. The mean CAS-7 score in this study was found to be 18.9 ± 6.4. The item with highest mean scores was: “How concerned are you when people cough or sneeze because of the fear that you may acquire COVID-19?” No significant differences in CAS-7 scores were found based on gender, educational qualification of the participants, while significant differences were observed based on place of residence, presence of COVID-19 affected individuals in close surroundings, tobacco, and alcohol consumption.
Conclusion:
The results of this study inform that it is imperative for authorities and health care professionals to focus on the mental health aspect of COVID-19 and arrange for necessary support mechanisms.
Keywords: Anxiety, COVID-19, health care systems, mental health
Introduction
Coronavirus disease (COVID-19) has been creating a multitude of crises across the globe. In spite of the low case fatality rates, COVID-19 resulted in 461,715 deaths worldwide as on 21st June, 2020.[1] This reflects the magnitude of the pandemic and its contagiousness. COVID-19 demanded non-pharmaceutical interventions like lockdown and social distancing aimed at decreasing the rate of transmission; almost all the countries across the globe resorted to these non-pharmaceutical interventions. The health care delivery systems are continuously being challenged since the beginning of this pandemic in order to provide necessary care for the growing number of COVID-19 cases with an infrastructure and manpower that is not prepared for the pandemic.[2] Although the physical implications of COVID-19 are known and are being actively shared among populations, mental health implications of COVID-19 are relatively less discussed. It is imperative to acknowledge that COVID-19 poses significant burden on the psychological well-being of people.[3,4,5] With implementation of lockdown and measures like quarantine, the mental health of people is affected, and the associated problems may range from depression to suicidal ideation.[6] There have been reports on completed suicides because of fear of COVID-19, stigmatization of COVID-19 affected, etc.[7] In these circumstances, screening the mental health of populations with regard to COVID-19 may help in identification of psychological burden posed by COVID-19 among people and facilitates preparation of necessary health care delivery systems, formulation of targeted behavioral interventions. Few countries have started online mental health services to negotiate the growing mental health concerns among people.[8] Though structured clinical interviews are preferred with regard to mental health, it is not uncommon to use psychometric tools in measuring various attributes of mental health. There is vast scientific literature on psychometric instruments measuring depression, anxiety, resilience, fear, stress, phobia, etc.[9,10,11,12] However, as these psychometric instruments were not developed specifically in the context of COVID-19 derived mental health issues, instruments directed at assessing the mental health burden posed by COVID-19 are required. A good number of validated psychometric tools were made available in the past few months to measure COVID-19 related mental health problems.[13,14,15,16,17,18,19] Among these measures, COVID-19 Anxiety Scale (CAS) is a 7-item psychometric instrument developed in the Indian context aimed at identifying the COVID-19 anxiety among general population.
Andhra Pradesh is a South Indian state with a population of 4.97 Crores according to 2011 census. The state is among the states with more number of COVID-19 confirmed cases, with 8,999 confirmed cases and 106 deaths as on 21st June, 2020.[20] Andhra Pradesh is also among the top five states/UTs in terms of number of COVID-19 tests done.[21] With COVID-19 cases showing a consistent linear trend over the past few weeks and with the lockdown lifted, it is expected that apprehension, anxiety, fear among people will rise. With this background, the aim of this study was to assess COVID-19 anxiety among general population of the state of Andhra Pradesh.
Materials and Methods
This cross-sectional study to assess the COVID-19 anxiety among the population of Andhra Pradesh was conducted in June, 2020. Ethical approval for the study was obtained from the Institutional Review Board [03-20-IRB-GEMS] on 4/4/2020. COVID-19 anxiety scale (CAS-7), developed in the Indian context by Chandu VC et al., was used to assess the COVID-19 specific anxiety among general population.[18] The eligibility criteria for participation in this study were the ability to read Telugu, more than 18 years of age, and no previously known mental health problems. The scale was administered online viz. Google forms, first to the known contacts of the authors, and then these known contacts were asked to share the form among their contacts. The focus of the study was mainly limited to the districts of Srikakulam, Vizianagaram, Visakhapatnam, East Godavari, West Godavari, Krishna, and Guntur. The study period was determined apriori as 1 week, from 11th June to 18th June 2020, and the responses collected during this period were intended to be included in the analysis. CAS-7 is a brief 7 item instrument with good psychometric properties which assesses the cognitive, emotional, and physiological dimensions of anxiety using a semantic differential scale. The minimum and maximum possible scores on CAS-7 are 7 and 28, respectively. The following demographic data were collected along with the COVID-19 anxiety scale: age; gender; place of residence; educational background; any known contact with COVID-19 affected individual in the past 2 weeks; any known COVID-19 cases in the close surroundings of the participants (within 2 km); current tobacco and alcohol consumption status. All the participants were informed about the study details and expressed consent by voluntarily participating in the study. Statistical analysis was done using SPSS version 20 software. Descriptive statistics, Independent samples t-test, one-way analysis of variance (ANOVA) were employed in data analysis.
Results
The mean age of the study participants was 36.13 ± 10.2 years, and 55.8% were males. Table 1 shows the descriptive statistics of the background characteristics of the study population. The mean CAS-7 score in this study was found to be 18.9 ± 6.4. Table 2 shows item wise mean scores for CAS-7 based on age group, place of residence, presence of known COVID-19 cases in surroundings, tobacco and alcohol consumption status. The two items with highest mean scores were: “How concerned are you when people cough or sneeze because of the fear that you may acquire COVID-19?”; “How afraid are you of acquiring COVID-19 when going into the public?” There was a statistically significant difference in the COVID-19 anxiety scores based on the place of residence, presence of known COVID-19 cases in the surroundings, age group of the participants, and their current tobacco, alcohol consumption status. No significant differences in CAS-7 scores were found based on gender and educational qualification [Table 3]. Older participants showed significantly higher CAS-7 scores compared to younger individuals. Higher CAS-7 scores were observed among participants who reported identification of COVID-19 affected individuals within their close surroundings. Current smokers and alcohol consumers demonstrated higher COVID-19 anxiety compared to non-users. CAS-7 scores were observed to be the highest among the population from Guntur and Krishna districts of Andhra Pradesh, while the least anxiety scores were reported from the districts of Srikakulam and Vizianagaram [Figure 1]. Since there was no reported use of tobacco and alcohol among females, the association between tobacco, alcohol consumption and CAS-7 scores was also checked exclusively among males; significant difference was observed between users and non-users in the stratified analysis as well [Figure 2].
Table 1.
Descriptive statistics of the background characteristics of the study population
| Variable | Category | n (%) |
|---|---|---|
| Age (years) | 18-30 | 856 (63.59) |
| 31-40 | 270 (20.05) | |
| 41-50 | 125 (9.28) | |
| >50 years | 95 (7.05) | |
| Gender | Female | 594 (44.13) |
| Male | 752 (55.86) | |
| Education (highest qualification at the time of data collection) | Secondary school | 132 (9.8) |
| Bachelor’s degree | 796 (59.13) | |
| Master’s degree | 418 (31.05) | |
| Presence of known COVID-19 cases in the close surroundings | Yes | 129 (9.58) |
| No | 1217 (90.41) | |
| Current tobacco user | Yes | 183 (13.59) |
| No | 1163 (86.4) | |
| Current alcohol consumer | Yes | 136 (10.1) |
| No | 1210 (89.89) |
Table 2.
CAS-7 Item wise means scores of the study participants
| Item | Factor | Mean±SD | Median |
|---|---|---|---|
| How afraid are you of acquiring COVID-19 when going into the public? | Fear of social interaction | 3.3±0.6 | 3 |
| How frequently are you feeling worried that you have acquired COVID-19? | Illness anxiety | 2.4±0.73 | 2 |
| How frequently is your sleep getting affected because of thoughts relating to COVID-19? | Illness anxiety | 1.9±0.3 | 2 |
| How frequently are you avoiding conversations on COVID-19 related information out of fear/anxiety? | Fear of social interaction | 2.2±0.61 | 2 |
| How worried are you of acquiring COVID-19 when an unknown person is coming closer to you? | Fear of social interaction | 2.8±0.9 | 3 |
| How anxious are you getting when knowing information on COVID-19? | Fear of social interaction | 2.5±1.1 | 3 |
| How concerned are you when people cough or sneeze because of the fear that you may acquire COVID-19? | Fear of social interaction | 3.6±0.2 | 4 |
Table 3.
Differences in mean CAS-7 scores based on background characteristics
| Variable | Category | n | CAS-7 Score Mean±SD | P value |
|---|---|---|---|---|
| Age (years)ƚ | 18-30 | 856 | 18.2±7.1 | 0.001* |
| 31-40 | 270 | 19.3±4.8 | ||
| 41-50 | 125 | 20.7±6.7 | ||
| >50 years | 95 | 21.6±4.3 | ||
| Gender§ | Female | 594 | 18.68±7.2 | 0.28 |
| Male | 752 | 19.07±6.16 | ||
| Education (highest qualification at the time of data collection) ƚ | Secondary school | 132 | 18.91±7.3 | 0.08 |
| Bachelor’s degree | 796 | 18.63±6.8 | ||
| Master’s degree | 418 | 19.41±5.2 | ||
| Presence of known COVID-19 cases in the close surroundings§ | Yes | 129 | 22.6±4.2 | 0.001* |
| No | 1217 | 18.5±7.8 | ||
| Current tobacco user§ | Yes | 183 | 221. ±5.3 | 0.001* |
| No | 1163 | 18.4±6.7 | ||
| Current alcohol consumer§ | Yes | 136 | 21.9±4.9 | 0.001* |
| No | 1210 | 18.5±7.2 |
ƚOne-way Analysis of Variance; §Independent samples t-test; P ≤ 0.05 considered statistically significant; * denotes statistical significance
Figure 1.
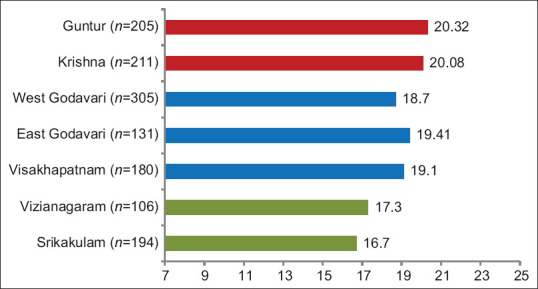
Differences in CAS-7 scores based on place of residence (CAS-7 scores <18 – Green; >18 < 20 – Blue; >20 – Red). *14 participants from districts other than those described in this figure were removed from the bar chart
Figure 2.
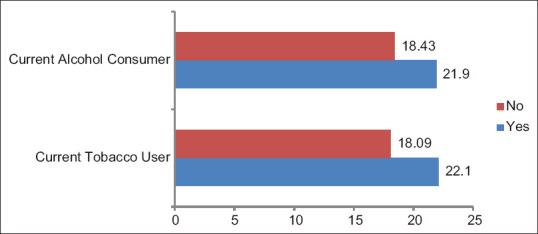
Association between current tobacco, alcohol consumption status and CAS-7 scores in the male stratum (n = 752)
Discussion
This is the first study which attempted to report the COVID-19 anxiety exclusively among Andhra Pradesh population. It was observed from this study that substantial degree of anxiety regarding COVID-19 is existent among the state's population with distinction between its districts. The districts with highest CAS-7 scores are among the districts with highest number of COVID-19 cases.[20] In the literature, it is an established notion that symptoms of mental health problems such as anxiety, depression, and stress are common among females compared to males.[22,23] However, no significant difference between males and females was observed in this study which is contradicting with findings reported by Doshi D et al.[24] in India and Broche-Perez Y et al.[25] in Cuba. No differences in COVID-19 anxiety scores were observed based on the educational qualification of the study participants. Chandu VC et al. reported a consistent decrease in COVID-19 anxiety scores with increase in educational qualification.[18] Nevertheless, these findings have to be interpreted in light of the fact that all the study participants have completed secondary school and nearly 90% have either bachelor's degree or master's degrees. A certain level of education is warranted to enable people to access various sources, understand the shared information, and critically evaluate the accuracy of information; beyond that, people with different levels of educational qualifications may fall in the same category with regard to their disease related anxiety. This is the first study which attempted to categorize people based on presence of COVID-19 affected individuals in their neighborhood. People with known COVID-19 cases in their neighborhood demonstrated significantly higher CAS-7 scores. Given the highly contagious nature of SARS CoV-2, this finding could be because of the general apprehension that they may have come in contact with the affected people as the study subjects attempt to recall. In this study, COVID-19 anxiety scores increase with age which is consistent with the international experiences from Italy[26] and Russia, Belarus.[27]
Subjects reporting current tobacco and/or alcohol consumption had higher COVID-19 anxiety scores. Though the direction of this association could not be revealed based on the design of the study, it is documented in literature that anxiety results in inclination for substance use.[28] Vardavas CI and Nikitara K reported in a systematic review that tobacco is linked with unwarranted progression in the severity of COVID-19.[29] A possible reason for increased CAS-7 scores among tobacco and alcohol consumers could be increased emphasis by World Health Organization and the central, local governments on spreading awareness to refrain from tobacco and alcohol use as these habits make the individual more prone for getting infected with SARS CoV-2. Getting aware of the predisposition and being unable to quit the habit may lead to dissonance among the individuals, and the conflict may by the reason for increased anxiety. Nevertheless, it is clear that the two pandemics “COVID-19” and “addiction” are on a verge of collision which only makes the situation more verse in terms of catering to the needs of the population.[30] The understanding of differences in COVID-19 anxiety and fear across different categories of the sociodemographic variables goes a long way in identification of vulnerable populations and facilitation of the provision of necessary mental health services. The findings of this study are important from a primary care perspective as early identification of COVID-19 impact on mental health among populations is warranted both in reducing COVID-19 transmission and in avoiding burden on the health care systems post COVID-19. These findings also inform the preparation of psychoeducational materials to alleviate COVID-19 specific fear and anxiety among populations.
The limitations of this study include collection of data through Google forms online among an arguably convenient sample. Further, all the study participants have completed secondary school education which makes the findings of this study less generalizable for subjects with lesser or no educational background. Nevertheless, this is the first study which provides a district wise picture of COVID-19 anxiety and extracts the most common fears among public by analyzing the item wise responses.
Conclusion
It is thoroughly established that epidemics are associated with mental health problems. In the COVID-19 context, the magnitude of these problems would only be more severe given the rate of transmission of SARS-CoV-2. In these circumstances, it is imperative that authorities and health care professionals focus on the mental health aspect of COVID-19 and arrange for necessary support mechanisms. It is also important to acknowledge that health care professionals are vulnerable for COVID-19 associated mental health concerns being a part of the frontline workers in combating COVID-19. Hence, documentation of COVID-19 posed mental health burden using validated psychometric tools is the need of the hour.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. Coronavirus disease 2019 (COVID-19): Situation report-153. 2020. [Last accessed on 2020 Jun 22]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200621-covid-19-sitrep-153.pdf?sfvrsn=c896464d_2 .
- 2.Mahmood S, Hasan K, Colder Carras M, Labrique A. Global preparedness against COVID-19: We must leverage the power of digital health. JMIR Public Health Surveill. 2020;6:e18980. doi: 10.2196/18980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. 2020;89:531–42. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. 2020;14:779–88. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y, Zhang H, Ma X, Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: A longitudinal study of college students in China. Int J Environ Res Public Health. 2020;17:3722. doi: 10.3390/ijerph17103722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Killgore WDS, Taylor EC, Cloonan SA, Dailey NS. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020;291:113216. doi: 10.1016/j.psychres.2020.113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goyal K, Chauhan P, Chhikara K, Gupta P, Singh MP. Fear of COVID 2019: First suicidal case in India! Asian J Psychiatr. 2020;49:101989. doi: 10.1016/j.ajp.2020.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ifdil I, Fadli RP, Suranata K, Zola N, Ardi Z. Online mental health services in Indonesia during the COVID-19 outbreak. Asian J Psychiatr. 2020;51:102153. doi: 10.1016/j.ajp.2020.102153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–39. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 10.Costantini M, Musso M, Viterbori P, Bonci F, Del Mastro L, Garrone O, et al. Detecting psychological distress in cancer patients: Validity of the Italian version of the Hospital Anxiety and Depression Scale. Support Care Cancer. 1999;7:121–7. doi: 10.1007/s005200050241. [DOI] [PubMed] [Google Scholar]
- 11.Knappe S, Klotsche J, Strobel A, Lebeau RT, Craske MG, Wittchen HU, et al. Dimensional anxiety scales for DSM-5: Sensitivity to clinical severity. Eur Psychiatry. 2013;28:448–56. doi: 10.1016/j.eurpsy.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Haktanir A, Lenz AS, Can N, Watson JC. Development and evaluation of Turkish language versions of three positive psychology assessments. Int J Adv Couns. 2016;38:286–97. [Google Scholar]
- 13.Lee SA. How much “Thinking” about COVID-19 is clinically dysfunctional? Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.04.067. doi: 10.1016/j. bbi. 2020.04.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SA. Coronavirus anxiety scale: A brief mental health screener for COVID-19 related anxiety. Death Stud. 2020;44:393–401. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- 15.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: Development and initial validation? Int J Ment Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00270-8. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arpaci I, Karataş K, Baloǧlu M. The development and initial tests for the psychometric properties of the COVID-19 Phobia Scale (C19P-S) Pers Individ Dif. 2020;164:110108. doi: 10.1016/j.paid.2020.110108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, Asmundson GJG. Development and initial validation of the COVID stress scales. J Anxiety Disord. 2020;72:102232. doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chandu VC, Pachava S, Vadapalli V, Marella Y. Development and Initial Validation of the COVID-19 Anxiety Scale. Indian J Public Health. 2020;64(Supplement):S201–S204. doi: 10.4103/ijph.IJPH_492_20. [DOI] [PubMed] [Google Scholar]
- 19.Costantini A, Mazzotti E. Italian validation of CoViD-19 Peritraumatic Distress Index and preliminary data in a sample of general population. Riv Psichiatr. 2020;55:145–51. doi: 10.1708/3382.33570. [DOI] [PubMed] [Google Scholar]
- 20.COVID-19 Statewise status. #IndiaFightsCorona COVID-19. Government of India. [Last accessed on 2020 June 22]. Available from: https://www.mygov.in/covid-19/
- 21.COVID-19 Statewise status. #IndiaFightsCorona COVID-19. Government of India. [Last accessed on 2020 June 22]. Available from: https://www.mygov.in/covid-19/
- 22.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8:2861. doi: 10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doshi D, Karunakar P, Sukhabogi JR, Prasanna JS, Mahajan SV. Assessing coronavirus fear in indian population using the fear of COVID-19 scale. Int J Ment Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00332-x. doi: 10.1007/s11469-020-00332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Broche-Pérez Y, Fernández-Fleites Z, Jiménez-Puig E, Fernández-Castillo E, Rodríguez-Martin BC. Gender and fear of COVID-19 in a Cuban population sample. Int J Ment Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00343-8. doi: 10.1007/s11469-020-00343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Leo D, Trabucchi M. COVID-19 and the fears of Italian senior citizens. Int J Environ Res Public Health. 2020;17:3572. doi: 10.3390/ijerph17103572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gritsenko V, Skugarevsky O, Konstantinov V, Khamenka N, Marinova T, Reznik A, et al. COVID 19 Fear, stress, anxiety, and substance use among russian and belarusian university students. Int J Ment Health Addict. 2020:1–7. doi: 10.1007/s11469-020-00330-z. doi: 10.1007/s11469-020-00330-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boehm MA, Lei QM, Lloyd RM, Prichard JR. Depression, anxiety, and tobacco use: Overlapping impediments to sleep in a national sample of college students. J Am Coll Health. 2016;64:565–74. doi: 10.1080/07448481.2016.1205073. [DOI] [PubMed] [Google Scholar]
- 29.Vardavas CI, Nikitara K. COVID-19 and smoking: A systematic review of the evidence. Tob Induc Dis. 2020;18:20. doi: 10.18332/tid/119324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dubey MJ, Ghosh R, Chatterjee S, Biswas P, Chatterjee S, Dubey S. COVID-19 and addiction. Diabetes Metab Syndr. 2020;14:817–23. doi: 10.1016/j.dsx.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]


