Sir,
World Health Organization acclaims the practise of exclusive breastfeeding up to 6 months of life for all infants and then supplemented breast feeding is recommended until at least 2 years of age. It is now unanimously accepted that there is no commercial formula that can equivalent with breast milk. In addition to the suitable amounts of carbohydrate, fat, and protein, it also provides vitamins, minerals, hormones, and digestive enzymes. Breast milk also contains antibodies and lymphocytes from the mother that help the baby resist infections.[1]
Breast milk donation is endorsed and recommended as first alternative when it is not possible for the mother to breastfeed their hospitalized babies or if their mothers do not have sufficient milk production and any other condition where mothers may not be able to feed their babies. WHO and UNICEF jointly recommend that the use of human milk banks should be made available in appropriate situations. The largest group of recipients are premature infants who derive very substantial benefits from it. Human milk protects premature infants from necrotizing enterocolitis and from sepsis, two devastating medical conditions. Despite the benefits and importance of breastfeeding for both babies and mothers, the breast milk donation practice and the implementation and the establishment of breast milk banks have not yet developed in our nation.[2] This study focuses on identifying knowledge and perception among postnatal mothers about Human Breast Milk Bank establishment and its donation.
A cross-sectional study was conducted to assess the knowledge and perception on Human Milk Bank among postnatal mothers of a women and child care hospital of a in a tertiary care center. Sample size was calculated by assuming 50% of the mothers may have favorable perception toward human milk donation with 10% relative precision and 95% confidence interval. 100 consecutive postnatal mothers were enrolled in the study after obtaining Institute Research committee and Ethical committee approval. All postnatal mothers except who were critically ill were included in the study. A structured questionnaire was used to collect data on knowledge and perception of postnatal mothers.
Results showed 90% of the participants belong to age group of 20–30 years. Mean age was 26 ± 3 Years. 83% of them were from rural domicile, 77% of them had basic education, almost half of the (52%) participants were unemployed, remaining participants were either semi-skilled (28%) or unskilled (30%), 88% of the participants belonged to Hindu religion. 68% of the women showed willingness to use donor milk or donate breast milk if need arises. With regard to maternal perception regarding human milk donation and banking 71% of the postnatal mothers had favorable perception.[Figure 1]. Table 1 shows maximum number of participants were willing to donate and had positive perception toward milk banking.
Figure 1.
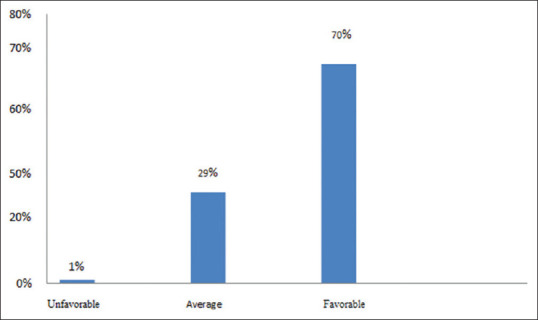
Perception level of postnatal mothers
Table 1.
Maternal perception on human milk donation n=100
| Items | Agree n (%) | Dis agree n (%) |
|---|---|---|
| I believe that human milk donation can Save babies. | 90 | 10 |
| I believe that human milk contains all essential nutrients required for healthy existence and complete development of baby | 95 | 5 |
| I believe that donating breast milk is good for mother’s health too as it reduces the breast engorgement. | 87 | 13 |
| I believe that donating breast milk does not cause malnutrition to mother or her baby. | 72 | 18 |
| I believe that there is nothing wrong in donating milk in case of excess production of milk. | 85 | 15 |
| I believe that my baby should get only my milk and not others. | 29 | 71 |
| I believe that my milk should be given only to my baby and not to others. | 18 | 72 |
| I am interested to donate milk but I am scared of expressing it using the machine. | 48 | 52 |
| I believe that culture/caste/religion do not have any role in milk donation. | 80 | 20 |
| I believe that it is good to donate milk to babies who are struggling to survive. | 89 | 11 |
| I feel very happy that my donated milk is the reason for the survival of a sick baby. | 81 | 19 |
| I will donate milk only to my family members and friend’s babies and not to any strangers. | 19 | 81 |
| I believe that if I am giving my milk to other babies then it may not be sufficient to my baby. | 28 | 72 |
This study explored that most of the participants had positive attitude toward human milk donation and banking despite poor educational background which has been supported by many other studies. Furthermore, this study findings reflects only the perception of the women and not the practice which may be altered when need arises among them due to influence of the personal factors and family members.
India is the maximum contributor to the worldwide birth cohort, neonatal mortality rate, and low birthweight. Of the 27 million infants born in India annually, one-third of the proportion similarly prematurity contribute 35% in neonatal death which can be improved by achievable health care interventions. These comprise kangaroo mother care, prevention and treatment of neonatal infections, neonatal resuscitation, and breastfeeding. Among these interventions, breastfeeding has been recognized as the single most powerful intervention.[3]
Literature supports the need of setting up more human milk bank as 13–15% of babies born in India are pre-term and their survival rate will be improved by donor milk and reduces the problem related to formula feeds and infections.[4] There is a need to have additional lactation counsellors and devoted team in hospital to make sure accessibility of quality lactation support to mothers and new born babies. Need for continuous support to mothers for breastfeeding has been reaffirmed globally which in turn encourages mothers to donate milk.[5]
Education and counselling the mothers during antenatal period can help them to develop positive attitude toward exclusive breast feeding and to understand its benefits to the mother and baby. Further it can help to develop irrepressible belief in the significance of breastfeeding and inform them about the motives for donating milk and how to donate their excess milk.
Human breast milk delivers bio active benefits which cannot be replaced by any other source of nutrition, the human milk banking concept to be widely educated to all our Indian communities for the acceptability.
Financial support and sponsorship
Under Golden Jubilee short term Research Award for Undergraduate Students (GJ-STRAUS) Rs. 10, 000 Received from Institute.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
Authors acknowledge the Contribution of support received for analysis of data from Dept. of Statistics and Demography, JIPMER, Puducherry-06.
References
- 1.Kimani ME, Wanjohi MN, Kamande EW, Macharia TN, Mwaniki E, Zerfu T, et al. Perceptions on donated human milk and human milk banking in Nairobi, Kenya. Matern Child Nutr. 2019;15:12842. doi: 10.1111/mcn.12842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mondkar J, Chugh SR, Shanbhag S, Khan A, Manuhar Sinha M, Dasgupta R, et al. Understanding barriers and facilitators for human milk banking among service providers, mothers, and influencers of preterm and sick neonates admitted at two health facilities in a metropolitan city in India. Breastfeed Med. 2018;13:694–701. doi: 10.1089/bfm.2018.0103. [DOI] [PubMed] [Google Scholar]
- 3.Nangia S, Sachdeva RC, Sabharwal V. Human milk banking: An Indian experience. NeoReviews. 2018;19:e201–10. [Google Scholar]
- 4.Jahan Y, Atiqur SM, Chowdhury AS, Chowdhury S, Moshiur R. Mothers’ knowledge and attitudes toward breast milk banking in developing countries. Ann Pregnancy Care. 2017;1:1002. [Google Scholar]
- 5.Abhulimhen BI, Okonkwo IR, Ideh RC, Okolo AA. Mothers’ perception of the use of banked human milk for feeding of the infants. Niger J Paed. 2015;42:223–7. [Google Scholar]


