Abstract
Imminent upper airway obstruction due to life-threatening tracheal stenosis of any cause is a challenging situation. We present a challenging case of total thyroidectomy for a malignant, invasive, and highly vascularized thyroid carcinoma that has invaded the surrounding tissues, including the sternum and mediastinum, resulting in compression of the trachea with indentation. The patient presented with a significant symptomatic tracheal stenosis, the narrowest area of that was 4 mm. Airway management in such cases presents a particular challenge to the anesthesiologists, especially considering that the option of tracheostomy is very difficult most of the time due to the highly swollen thyroid and distorted anatomy. A meticulous history of the patient's illness had been taken, and a comprehensive preoperative evaluation was conducted, including construction of a 3D model airway, virtual endoscopy, and transnasal tracheoscopy. On the day of the surgery, the airway was managed through spontaneous respiration using intravenous anesthesia and the high-flow nasal oxygen (STRIVE-Hi) technique. It was then secured with intubation using a straw endotracheal tube (Tritube®) with an internal diameter (ID) of 2.4 mm and an outer diameter of 4.4 mm with the help of a fiberscope and D-MAC blade of a video laryngoscope. At the end of the procedure, the airway was checked with a fiber optic scope, which showed an improvement in the narrowed area. This enabled us to replace the Tritube with an adult cuffed ETT of size 6.5 mm ID, and the patient was transferred intubated to the surgical ICU. Two days later, the patient's tracheal diameter was evaluated with the help of a fiberoptic scope and extubated successfully in the operating theater.
Keywords: tracheal stenosis, STRIVE-Hi, tritube, evone ventilator, flow controlled ventilation, transnasal tracheoscopy, thyroid cancer
Introduction
Thyroid cancer is one of the most common cancers worldwide: in the USA alone, it is considered the sixth most common cancer in women and the first in those between the ages of 20 and 34 years, as per the American Cancer Society's data of 2019.1 Malignant thyroid cancers that invade or compress the airway are considered complex and pose challenges for both surgeons and the anesthesiologists1,2 To operate smoothly on these cases, various methods of airway management during anesthesia have been used and described in the literature, including ECMO, AFOI, STRIVE-Hi, microlaryngoscopy tube, and/or JET ventilation.2–8
In this case report, we describe a novel and improved method of induction and airway management of a thyroid cancer patient with critical tracheal stenosis using the STRIVE-Hi technique through a high-flow oxygen cannula (HFNC) machine, the unique Tribute intubation and Evone ventilator, which achieved a successful anesthetic management of a rare presentation of a malignant, invasive and highly vascularized thyroid mass that had invaded the surrounding tissues including the sternum and mediastinum, resulting in compression, shifting, and indentation of the trachea.
Case Presentation
A 40-year-old male patient, obese, with a BMI of 37, presented to the general surgery clinic complaining of breathing difficulty that had been progressive in nature over the last two months, and thyroid enlargement causing stridor on exertion was noticed on both sides. The nature of the breathlessness was affecting the patient's quality of life. During these two months, the patient had made multiple visits to the ED where he was treated as a case of asthma exacerbation for which symptomatic treatment was provided. He had a past medical history of asthma. An early chest X-ray image taken during a primary health center visit 6 months prior to his general surgery clinic showed tracheal deviation (Figure 1, a) due to thyroid swelling. After a full investigation he had been diagnosed with a thyroid malignancy. The surgeon scheduled the patient for a total thyroidectomy and referred the patient to the difficult airway clinic for airway assessment. An airway examination showed Mallampati class II, a thyromental distance of 5 cm, a large swelling at the front of the neck, and tracheal deviations to the right side. Other airway assessments were normal.
Figure 1.
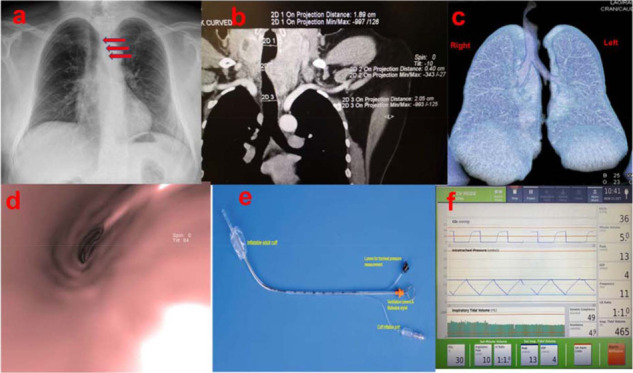
(a) Chest X-ray showing tracheal deviation at the tbl4–T5 level. (b) & (c) Coronal cut contrast- enhanced MDCT showing narrowing at the tbl4–T5 level, along with an enlarged thyroid. (d) 3D Reconstruction of MDCT with virtual endoscopy showing tracheal narrowing. (e) Straw ETT (Tritube) used for the initial intubation. (f) CO2, intratracheal pressure, and tidal volume readings during the procedure.
Investigations
CT scan
Multi-detector computed tomography before and after intravenous administration of 90 ml of Omnipaque non-ionic contrast medium was carried out. It revealed a thyroid gland appreciably enlarged in an uneven manner, predominately the left thyroid lobe, with significant displacement, compression, and deviation, as well as reduced caliber of the related portion of the trachea and a significantly reduced air column within. Inferiorly, there was evidence of retrosternal extension of approximately 2.8 cm. In addition, a rather well-defined soft-tissue mass lesion was epi-centered over the body of the sternum, and the lower aspect of the manubrium-sternal angle bulged on either side of the sternal body; its metastatic nature and underlying lytic destructive osseous pathology were noted.
Multiple well-defined pulmonary nodules were seen in both lungs, the largest 9 mm in diameter in the left lower lobe, likely of a metastatic nature. Displacement and compression of the trachea was noted.
A 3-D construction and virtual endoscopy (VE)
Three-dimensional reconstruction (3-D) was carried out on the raw data of the MDCT scan of the chest, including the lower neck, comprising VRT volume-rendering techniques, SSD shaded surface display, VR virtual reality/endoscopy, and TTP tissue transparent projections. It showed a sizable, irregular, uneven enlargement of the thyroid gland starting from the level of the hyoid bone superiorly, while its inferior aspect showed appreciable retrosternal extension. It resulted in significant deviation, rotation, and displacement of the related proximal trachea to the right, reducing its caliber from side to side, averaging a minimum of approximately 4–5 mm (Figure 1, b & c).
Suspected tracheomalacia was probably due to prolonged compression by the enlarged thyroid. Proximally and distally, the tracheal caliber averages were approximately 2 cm.
Significant encroachment upon the trachea, compromising its lumen, irregular walls with no line of cleavage, and possible microscopic/minimal infiltrations due to irregularities were noted on the virtual endoscopy (VE) (Figure 1, d). This helped us in the diagnosis and proper management of this difficult case.
A destructive lytic sternal sizable lesion was noted involving the lower manbriu–sternal junction and body of the sternum.
Fine needle aspiration was performed and suggested follicular thyroid carcinoma.
Transnasal Tracheoscopy (Figure 2, a, b, & c)
Figure 2.
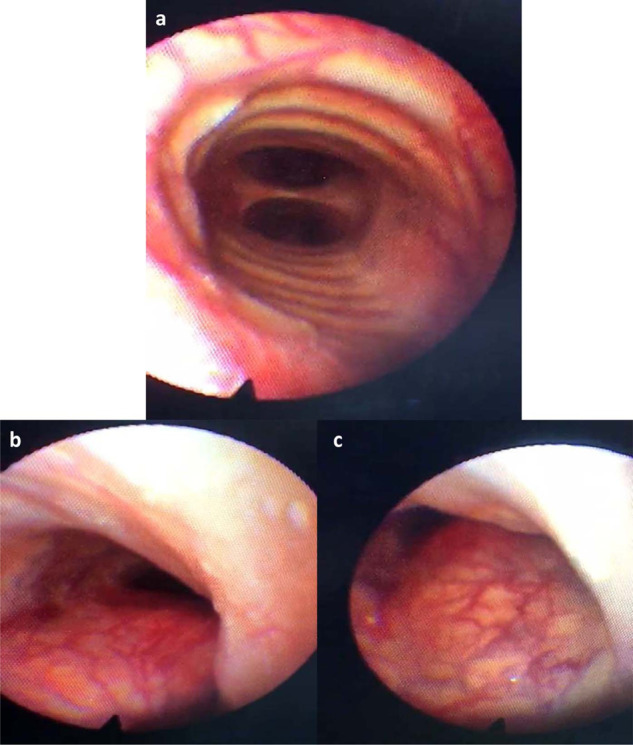
(a) shows the carina at the level below the stenosed area of the trachea, while (b) & (c) show the stenosed area in the trachea at the level of tracheal rings 5–6. The figures were obtained from fiber optic tracheoscopy.
Transnasal tracheoscopy was conducted one day prior to the surgical procedure at the voice and swallowing clinic (using 4% lidocaine as a topical anesthesia to anesthetize the vocal cords) by the laryngology surgeon. The procedure showed a highly vascularized mucosa covering a large mass occupying the left side of the trachea starting from the cricoid region to the level of the 7th tracheal ring (Figure 2, a, b, & c). A very narrow slit was noticed on the right side, which helped him to breathe and measured approximately 4 mm. However, the fiberscope diameter (3 mm) could bypass the mass, and the carina was reached safely and successfully.
The patient's blood work, including thyroid function tests, was unremarkable.
Management
Surgery
An ENT surgeon attended the induction of anesthesia and was ready to perform tracheostomy at any stage. Ultrasound marking of the neck anatomical structure was performed in the operating theater (OT) to facilitate tracheostomy if indicated. In the OT, the patient was initially connected to ASA standard monitoring in addition to the BIS. The plan was to start with the STRIVE-Hi technique using a HFNC machine. The flow started at 30 L/min, and sedation began with target controlled infusion (TCI) of propofol (3 mcg/ml for 5 minutes, then increased gradually to 1 mcg/ml every 2.5 minutes up to 7 mcg/ml), and dexmedetomidine infusion started at 40 mcg/h, was continued until the patient slept and was breathing spontaneously, while the inspiratory flow was raised gradually to 70 mL/min.6
The vocal cords were sprayed with xylocaine 4% to anesthetize the glottic and subglottic areas.
A fiberoptic scope was then inserted passing the vocal cord and the tracheal stenotic area successfully. A Tritube was inserted using a C-Mac video laryngoscope (Karle-Storze) with a D- Blade while keeping the fiberoptic scope in place to confirm the position of the Tritube cuff (Figure 1, e).
Tritube cuff placement was then confirmed by fiberoptic scope (below the lesion and above the carina). Subsequently, the tube was attached to an Evone ventilator, followed by Rocuronium and Remifentanil infusion (TCI mode).
The patient underwent total thyroidectomy. Surgery continued for more than 6 hours using the Evone ventilator, with optimal oxygenation and ventilation (FIO2 = 30%, inspiration flow 10 L/min, I: E ratio = 1:1, peak pressure: 13 cm H2O, EEP = 4 cm H2O) (Figure 1, f).
Intraoperative findings
Intraoperative findings showed a large, highly vascular thyroid tumor compressing the trachea, with indentation and without invasion. After removal of the mass, minimal improvement of the stenosis was noticed due to tracheomalacia, so the decision was made to replace the Tribute with classic cuffed ETT size 6.5 mm (ID), using a fiberoptic scope and C-MAC and the video-assisted fiberoptic intubation technique.
Optimal oxygenation and ventilation were maintained for another two hours before transferring the patient to surgical intensive care unit (SICU) using an anesthesia machine ventilator and cuffed ETT size 6.5 mm (ID).
Outcome
Six days later, he was extubated in the OT. His tracheal diameter was evaluated again with the help of a fiberscope, and there was good improvement of tracheal size. The patient had an uneventful postoperative recovery period and was discharged. The histopathology report was consistent with follicular thyroid carcinoma. The patient was then followed up monthly for three months in the general surgery clinic and received postoperative radioactive iodine. There was marked improvement in the patient's quality of life, as his episodes of breathlessness, which had been present before the surgery, subsided post total thyroidectomy. He was then referred to thoracic surgery for pulmonary nodules and sternal lesions.
Discussion
Patients with invasive thyroid cancer may have a distorted airway due to tumor compression, paralyzed vocal cords, or an intraluminal tumor invading the airway, with a potential for hemorrhage and airway distress.5 This poses equal and considerable challenges for both the anesthetist and the surgeon and requires a comprehensive preoperative evaluation for the patient and proper communication between them pre-, intra-, and postoperatively.
Managing airway compression or invasion due to a thyroid tumor has been described in the literature through different techniques, including ECMO, direct laryngoscope, and classic ETT, AFOI, HFNC, jet ventilation, and/or the STRIVE-Hi technique.2–5
ECMO comes with potential complications such as vascular injury and hemorrhage, thromboembolism, lipid deposition on the oxygenation membrane due to propofol infusion, bleeding due to heparinization, sequestration of other drugs in the circuit, and mechanical failure resulting in hypoxia.9,10,11 In our case, we were able to avoid the need for ECMO due to our extensive preoperative evaluation using VE and awake bronchoscopy, through which we were able to approximate the space present at the narrowest part of the stenosed tracheal lumen, and by using a straw endotracheal tube with an outer diameter of 4.4 mm. Moreover, we have described a technique that can be utilized in centers where ECMO machines are not available.
Classic ETT and AFOI in this case would have been untenable as the stenosed portion of the trachea would hinder the proper insertion of the ETT. Using jet ventilation in a patient with such significant stenosis would have resulted in inadequate oxygen saturation levels.
In this case, the STRIVE-Hi through HFNO machine was used, and intubation performed with a very small Tritube endotracheal tube with an ID on 2.4 mm and OD of 4.4 mm, considered a special technique, overcame narrow tracheal lesion. The patient was connected to an Evone ventilator, which depended upon flow-control ventilation (FCV) through active inspiration and expiration, maintaining smooth ventilation with stable lung and gas parameters for a long surgery of more than 6 hours. All of this was performed without causing a significant increase in airway resistance, as described in a number of papers that utilized a small classic ETT, which posed a considerable challenge in managing those cases, leading to changing the tube sizes multiple times in some of them.8
Learning Points
1- Tracheal stenosis can pose a challenge to the surgeon as well as the anesthesiologist.
2- VE and 3D reconstruction as well as transnasal tracheoscopy are important tools in the diagnosis of airway pathology.
3- Ventilation through straw (Tritube) and FCV is very useful in such critical airways.
4- Multidisciplinary teams consisting of surgeons (thyroid surgeon and laryngology surgeon), radiologists, and anesthesiologists are crucial in difficult airway management.
A careful history, proper clinical examination, and appropriate investigation are key to avoiding incorrect or missed diagnoses that could make patient's lives extremely difficult.
Conclusion
A careful history, proper clinical examination, and appropriate investigation are key to avoiding incorrect or missed diagnoses that could make patient's lives extremely difficult, as seen in this case. Critical tracheal stenosis due to invasive thyroid cancer can be challenging for anesthesiologists, but with a holistic preoperative evaluation and a clear plan and backup plan, successful intubation can be made possible on even the toughest of cases. Using the STRIVE-Hi technique with Tritube ETT and the Evone ventilator is considered one of the options for anesthetists to manage this kind of procedure. Larger and comprehensive studies exploring a wide range of cases similar to this one are needed to confirm this technique and the use of a ventilator and to raise the level of expertise in this technique.
Conflicts of interest
There are no conflicts of interest.
Patient consent
Consent obtained. Patient was informed and permission was received to use the intraoperative snapshot of the patient's vitals and tidal volume.
Financial support and sponsorship
None
Abbreviations
ECMO–Extracorporeal Membrane Oxygenation
AFOI–Awake Fiberoptic Intubation
ETT–Endotracheal tube
STRIVE-HI–Spontaneous Respiration using IntraVEnous anesthesia and HIgh-Flow nasal oxygen
FCV–Flow Controlled Ventilation
HFNC–High-Flow Nasal Cannula
HFNO–High-Flow Nasal Oxygenation
VE–Virtual Endoscopy
ID–Inner Diameter
OD–Outer Diameter
FiO2–Fraction of inspired Oxygen
EEP–End-Expiratory Pressure, can be positive (PEEP) and negative (NEEP)
BMI–Body Mass Index
D-MAC–Doerges Macintosh
References
- 1. Cancer.Net. (2019). Thyroid Cancer - Statistics. [online] Available from: https://www.cancer.net/cancer-types/thyroid-cancer/statistics [Accessed 18 Oct. 2019]
- 2. Yamaguchi K, Fujimoto K, Koide Y, Kurahashi K. Safe induction of anesthesia in 3 patients with severe tracheal stenosis caused by thyroid cancer. Masui. 2013; 62(1):78–82. [PubMed]
- 3. Sajid B, Rekha K. Airway management in patients with tracheal compression undergoing thyroidectomy: A retrospective analysis. Anesth. Essays Res. 2017; 11(1):110–116. [DOI] [PMC free article] [PubMed]
- 4. Liou J, Chow L, Chan K, Tsou M. Successful anesthetic management of a patient with thyroid carcinoma invading the trachea with tracheal obstruction, scheduled for total thyroidectomy. J. Chin. Med. Assoc. 2014; 77(9):496–499. [DOI] [PubMed]
- 5. Price D, Wong R, Randolph G. Invasive thyroid cancer: Management of the trachea and esophagus. Otolaryngol. Clin. North Am. 2008; 41(6):1155–1168. [DOI] [PMC free article] [PubMed]
- 6. Booth A, Vidhani K, Lee P, Thomsett C. SponTaneous Respiration using IntraVEnous anaesthesia and Hi-flow nasal oxygen (STRIVE Hi) maintains oxygenation and airway patency during management of the obstructed airway: An observational study. Br. J. Anaesth. 2017; 118(3):444–451. [DOI] [PMC free article] [PubMed]
- 7. Cho J, Jeong M, Choi J, Cho J, Lee H, Kim D, Kim K, Seo J. Anesthetic consideration for patients with severe tracheal obstruction caused by thyroid cancer -A report of 2 cases-. Korean J. Anesthesiol. 2010; 58(4):396–400. [DOI] [PMC free article] [PubMed]
- 8. Lee P, Booth A, Vidhani K. Spontaneous respiration using intravenous anesthesia and high-flow nasal oxygen (STRIVE Hi) management of acute adult epiglottitis. A A Pract 2018; 10(4):73–75. [DOI] [PMC free article] [PubMed]
- 9. Jeong YI, Jun IG, Ha SS, Kwon HJ, Lee YM. Extracorporeal membrane oxygenation for the anesthetic management of a patient with a massive intrathoracic goiter causing severe tracheal obstruction with positional symptoms: A case report. Med. (Baltim.) 2019; 98(42):e17650. doi:10.1097/MD.0000000000017650. [DOI] [PMC free article] [PubMed]
- 10. Kim SH, Song S, Kim YD, et al. Outcomes of extracorporeal life support during surgery for the critical airway stenosis. ASAIO J. 2017; 63(1):99–103. doi:10.1097/MAT.0000000000000458. [DOI] [PubMed]
- 11. Foong TW, Ramanathan K, Chan KKM, MacLaren G. Extracorporeal membrane oxygenation during adult noncardiac surgery and perioperative emergencies: A narrative review. J. Cardiothorac. Vasc. Anesth. 2021; 35(1):281–297. [DOI] [PubMed]
- 12. Avenia N, Vannucci J, Monacelli M, et al. Thyroid cancer invading the airway: Diagnosis and management. Int. J. Surg. 2016; 28 Suppl 1:S75–S78. doi:10.1016/j.ijsu.2015.12.036. [DOI] [PubMed]


