Abstract
Objective
This study examined whether health insurance stability was associated with improved type 2 diabetes mellitus (DM) control and reduced racial/ethnic health disparities.
Methods
We utilized electronic medical record data (2005-2013) from two large, urban academic health systems with a racially/ethnically diverse patient population to examine insurance coverage, and three DM outcomes (poor diabetes control, A1c ≥8.0%; very poor diabetes control A1c >9.0%; and poor BP control, ≥ 130/80 mm Hg) and one DM management outcome (A1c monitoring). We used generalized estimating equations adjusting for age, sex, comorbidities, site of care, education, and income. Additional analysis examined if insurance stability (stable public or private insurance over the six-month internal) moderates the impact of race/ethnicity on DM outcomes.
Results
Nearly 50% of non-Hispanic (NH) Whites had private insurance coverage, compared with 33.5% of NH Blacks, 31.5% of Asians, and 31.1% of Hispanics. Overall, and within most racial/ ethnic groups, insurance stability was associated with better glycemic control compared with those with insurance switches or always being uninsured, with uninsured NH Blacks having significantly worse BP control. More NH Black and Hispanic patients had poorly controlled (A1c≥8%) and very poorly controlled (A1c>9%) diabetes across all insurance stability types than NH Whites or Asians. The interaction between insurance instability and race/ethnic groups was statistically significant for A1c monitoring and BP control, but not for glycemic control.
Conclusion
Stable insurance coverage was associated with improved DM outcomes for all racial / ethnic groups, but did not eliminate racial ethnic disparities.
Keywords: Health Insurance, Health Insurance Stability, Health Disparities, Social Determinants of Health
Background
The rising prevalence of type 2 diabetes mellitus (DM) in the United States, particularly among racial/ethnic minorities, and the consequent health care and financial burden it places on the US health care system is of increasing concern.1 By 2050, the Centers for Disease Control and Prevention estimates that one third of US adults will have DM, with racial and ethnic minorities bearing a disproportionate burden of the diabetes epidemic.2 While glycemic control among those diagnosed with diabetes has improved over the years, some studies suggest the disparities in diabetes control and outcomes between Whites and other racial/ethnic groups have either stayed the same or, in the case for Hispanics, widened.3 Access to clinical care and insurance status, which are influenced by system-level policies, are aspects of social determinants of health that impact health outcomes and contribute to health disparities in the United States.4
A growing body of research suggests that insurance stability in general improves clinical care and practice around the management of diabetes5-9; however, most of the existing studies are cross-sectional and therefore limited to examining current insurance coverage and diabetes outcomes instead of insurance changes over time. One such study examined trends in diabetes control by race/ethnicity and education from 1999 to 2006, but only looked at the effects of Medicare coverage and not changes in insurance status overall.3 Another cross-sectional study found an association between insurance coverage, race, socioeconomic status and quality of care for diabetes; however, differences by race/ethnicity and socioeconomic status were not statistically significant across all multivariable analysis.7 Increased health care access through stable health insurance may be a potential solution to improve poor diabetes outcomes in racially/ethnically diverse patients.7 While insurance reforms – beginning at the state level in Massachusetts in 2006 and then expanding nationally with the Affordable Care Act in 2014—have increased rates of insurance coverage, they may increase instability or switches and gaps in coverage, and thereby reduce access to care and the overall quality of an individual’s care.10-12
Very few studies examine insurance stability explicitly as it relates to addressing racial/ethnic health disparities and DM specifically. We aimed to assess DM care outcomes and processes by health insurance stability status among a racially and ethnically diverse patient population. We hypothesized that stable health insurance coverage would improve both the processes and outcomes of DM care and help to reduce racial/ethnic disparities.
Methods
Study Population
We focused our analyses on patients with a diagnosis of type 2 DM receiving care in primary care practices (internal medicine and family medicine) . We utilized data from two large, urban academic health centers and six affiliated community health centers with racially/ethnically diverse patient populations. Both academic health centers provide disproportionate care to those with Medicaid and who are uninsured, and specifically serve populations who benefit from insurance reform and who were at risk of insurance instability. Inclusion criteria were having a type 2 DM diagnosis (ICD9 codes 249, 250, 250.x, 250.x0, 250.x2 on billing records or problem lists) and being aged 18-64 years. We excluded patients once they reached 65 years, due to Medicare eligibility and corresponding lack of risk for loss of insurance. Racial/ethnic groups in the study included: non-Hispanic (NH) Whites, non-Hispanic (NH) Blacks, Asian/Pacific Islanders and Hispanics. Patients were excluded if their race/ethnicity was missing (n=2,335, 12.3%) or in the unspecified “other” (n=689, 3.46%) category.
Data
We utilized electronic medical record (EMR) and billing data from January 2005 through December 2013. Use of billing records ensured that we captured the payer and insurance type for each point of care. We divided each individual’s longitudinal record of care into two six-month intervals per calendar year (January – June and July – December), which served as the unit of analysis.
Measures
Based on individual insurance coverage at each primary care visit, we categorized insurance stability status as four separate categories during each six month interval: 1) always private (employer based or individual coverage without subsidies); 2) always public (Medicaid, Medicare, or subsidized such as Commonwealth Care13); 3) insurance switch (uninsured to insured; switch between insurance categories; or insured to uninsured); or 4) always uninsured. Switches within the same category, such as one private insurance policy to another with a change in employment, were not considered an insurance switch. The insurance stability status categories were determined by comparing each primary care visit to the previous primary care visit, whether or not the visits were in the same interval. Individuals were included in the analytic data only during those six-month intervals where they had a primary care visit. We selected six-month intervals as the unit of analysis to align with the standard of diabetes care and management (eg, for the study duration, guidelines for A1c or blood pressure monitoring was twice annually).14
We collected the following data for use as covariates in our analyses: the Charlson comorbidity index (CCI); median household income and percentage of residents with high school graduation in the patient’s Census tract; sex; age; and site of care, stratified into three groupings (either one of two medical centers, or a community health center). The CCI, income, high school graduation rate, and age were time varying.
Study outcomes included both process and outcome diabetes management measures established by the National Committee for Quality Assurance (NCQA) during the relevant timeframe of the study.15 The process measure was an indicator for having A1c checked within the six-month interval. Because a large proportion (96.3%) of intervals included a blood pressure measure, we did not examine blood pressure readings as a process measure.
The outcome measures for diabetes management included two dichotomous cutpoints for A1c control, poor diabetes control (A1c ≥8.0%) and very poor diabetes control (>9.0%), based on NCQA guidelines, and one dichotomous variable for blood pressure control, poor blood pressure control (≥ 13/>0/80 mm Hg), based on NCQA guidelines.
Statistics
We used descriptive statistics by race/ethnicity to examine characteristics of the sample, including sociodemographic factors and insurance stability categories. We examined unadjusted prevalences and odds of diabetes and blood pressure control and A1c monitoring based on insurance stability status category, first overall and then stratifying by race/ethnicity, after adjusting for possible confounders. We examined whether insurance stability moderates the impact of race/ethnicity on DM outcomes by including an interaction term between race/ethnicity and insurance stability status in the logistic regression models. The patient-six-month interval was treated as the unit of analysis. We used generalized estimating equations (GEE) to account for correlated measurements from each patient.
Results
Demographics of Study Sample
As shown in Table 1, 14,093 patients were included in the analytical sample, of which 56.5% were women, 56.3% were NH Black, 28.1% were NH White, 6.6% were Hispanic, and 9.1% were Asian. Mean age at the first visit within the dataset was 48.7 years. Mean census tract graduation rate was 86.9% for NH Whites, 82.4% for Asians, 79.8% for NH Blacks and 79.1% for Hispanic patients. Mean Census tract median income was $70,636 for NH Whites, $62,537 for Asians, $50,793 for Hispanics and $49,766 for NH Blacks. All patients had DM as a comorbidity for the CCI calculation; 23.2% of the NH White population had two or more comorbidities on the CCI, followed by 19.9% of Hispanic, 17.6% of NH Black and 13.0% Asian patients. The percentage of non-English speaking patients (based on reported language preference) was 23.4% for the entire study sample, 67.2% for Asian patients, 52.6% of the Hispanic patients, 19.1% of the NH Black patients, and 10.8% of the NH White patients.
Table 1. Demographic characteristics by race/ethnicity of patients with diabetes at 2 large urban health care systems, 2005-2013.
| Variable | Total patient sample | Non-Hispanic White | Hispanic | Black/African American | Asian/Asian Pacific Islander |
| Total samplea | 14093 | 3954 (28.1) | 924 (6.6) | 7928 (56.3) | 1287 (9.1) |
| Age, years, mean (SD) b | 48.7 (10.5) | 49.9 (10.1) | 46.8 (11.0) | 48.2 (10.6) | 49.6 (10.4) |
| Sex | |||||
| Male | 6135 (43.5) | 2022 (51.1) | 452 (48.9) | 3114 (39.3) | 547 (42.5) |
| Female | 7958 (56.5) | 1932 (48.9) | 472 (51.1) | 4814 (60.7) | 740 (57.5) |
| Charlson Comorbidity Index, weightedb,c | |||||
| 1 | 11268 (81.1) | 2958 (76.8) | 727 (80.1) | 6496 (82.4) | 1087 (87.0) |
| 2+ | 2624 (18.9) | 895 (23.2) | 181 (19.9) | 1385 (17.6) | 163 (13.0) |
| Census tract high school graduate or higher, %, mean (SD)b | 82.0 (10.5) | 86.9 (10.1) | 79.1 (11.0) | 79.8 (9.6) | 82.4 (11.3) |
| Census tract income, 2014 $, mean (SD) b | 56849.3 (25538.2) | 70635.6 (27749.3) | 50792.6 (23196.8) | 49765.9 (21029.4) | 62537.0 (26767.4) |
| Language | |||||
| English | 10589 (76.6) | 3373 (89.2) | 434 (47.4) | 6368 (80.9) | 414 (32.8) |
| Non-English | 3241 (23.4) | 407 (10.8) | 482 (52.6) | 1503 (19.1) | 849 (67.2) |
| Locationb | |||||
| Academic center 1 | 6792 (48.2) | 1406 (35.5) | 442 (47.8) | 4686 (59.1) | 258 (20.1) |
| Community health centers | 4319 (30.6) | 1117 (28.3) | 277 (30.0) | 2375 (30.0) | 550 (42.7) |
| Academic center 2 | 2982 (21.2) | 1431 (36.2) | 205 (22.2) | 867 (10.9) | 479 (37.2) |
Results are frequency (%) unless otherwise indicated.
a. Data presented at the patient level.
b. Variable based on data from first date of medical records.
c. Index range of 0 – 17 conditions.
Insurance Status by Race/Ethnicity
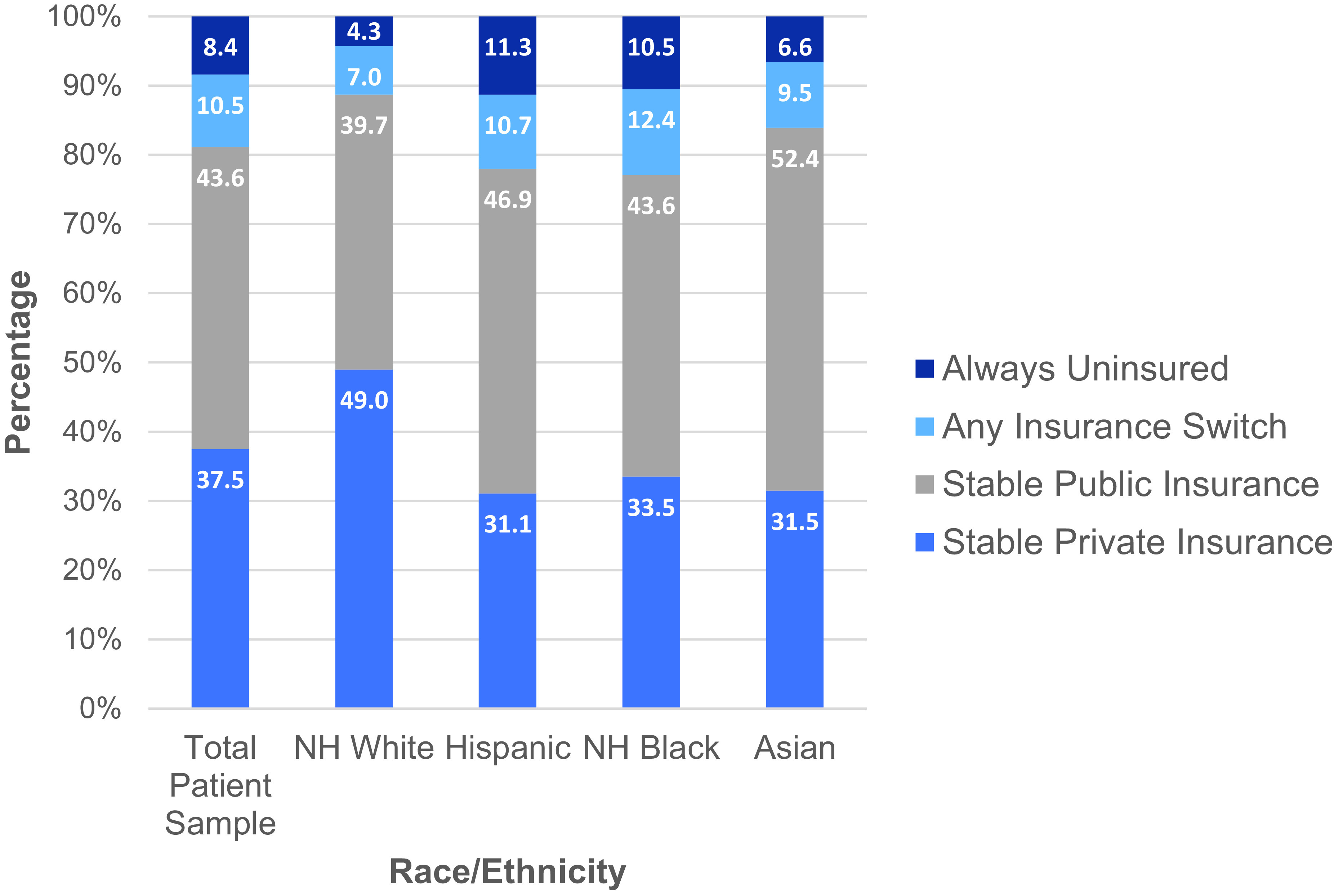
Figure 1 provides the insurance stability status of the total patient sample and by race/ethnicity. Most patients had either stable private insurance (37.5%) or stable public insurance (43.6%); with a similar percentage experiencing any insurance switch (10.5%) and being uninsured (8.4%) in the interval. Nearly half of NH White patients (49.0%) had stable private insurance, compared with 33.5% of NH Blacks, 31.5% of Asians, and 31.1% of Hispanics. 52.4% of Asians, 46.9% of Hispanics, 39.7% NH of Whites and 43.6% of NH Blacks had stable public insurance. 10.7% of Hispanics and 12.4% of NH Blacks experienced insurance switches and, 11.3% and 10.5%, respectively, were uninsured. Meanwhile, 4.3% of NH Whites and 6.6% of Asians were uninsured.
Figure 1. Insurance status by race/ethnicity.
Diabetes-related Outcomes by Race/Ethnicity and Insurance Category
Table 2 provides the raw rates of A1c and blood pressure outcome and process measures by race/ethnicity and insurance stability category. Overall, and within most racial/ ethnic groups, those with stable private or public insurance had better A1c control and better BP control than those with insurance switches or always uninsured. In analyses adjusted for clustering, Hispanics and NH Blacks had the highest percentages of poor control (A1c ≥8.0%) and very poor control (A1c>9.0%) A1c readings across all insurance stability types, compared with NH Whites, despite similar rates of A1c monitoring across all groups (all P significant, P<.001).
Table 2. Raw proportions for blood pressure and A1c process and outcome measures among patients with diabetes by race/ethnicity and insurance instability category from academic and community health centers, 2005-2013.
| Total patient sample | Non-Hispanic Whiteb | Hispanicb | Black/African Americanb | Asian/Asian Pacific Islanderb | ||
| Instability (6-Category) a | n, 6-month intervals | %, 6-month intervals | %, 6-month intervals | %, 6-month intervals | %, 6-month intervals | %, 6-month intervals |
| Poor diabetes control, A1c ≥8.0% | ||||||
| Overall | 74,016 | 27.0 | 24.5 | 30.1 | 29.5 | 16.4 |
| Stable private insurance | 27,514 | 25.5 | 23.8 | 27.7 | 28.0 | 15.5 |
| Stable public insurance | 32,230 | 25.7 | 24.3 | 30.4 | 27.8 | 15.5 |
| Any insurance switches | 7,779 | 31.4 | 28.7 | 29.2 | 33.6 | 20.0 |
| Always uninsured | 6,493 | 34.5 | 27.9 | 36.0 | 36.9 | 22.4 |
| Very poor diabetes control, >9.0% | ||||||
| Overall | 74,016 | 17.1 | 15.2 | 19.4 | 19.1 | 9.1 |
| Stable private insurance | 27,514 | 15.7 | 14.5 | 18.4 | 17.4 | 8.6 |
| Stable public insurance | 32,230 | 16.6 | 15.2 | 19.7 | 18.6 | 8.5 |
| Any insurance switches | 7,779 | 20.6 | 19.4 | 19.3 | 22.1 | 11.9 |
| Always uninsured | 6,493 | 21.1 | 16.7 | 20.9 | 22.9 | 12.0 |
| A1c process (not monitored) | ||||||
| Overall | 90,111 | 23.5 | 27.8 | 24.3 | 21.3 | 23.6 |
| Stable private insurance | 33,444 | 23.3 | 27.7 | 25.6 | 20.4 | 21.1 |
| Stable public insurance | 39,498 | 24.4 | 28.2 | 23.9 | 22.8 | 24.1 |
| Any insurance switches | 9,514 | 22.8 | 29.4 | 22.7 | 20.4 | 27.1 |
| Always uninsured | 7,655 | 20.8 | 23.5 | 23.9 | 19.3 | 26.2 |
| Poor BP control, ≥ 130/80 mm Hg | ||||||
| Overall | 87,567 | 55.5 | 52.8 | 49.1 | 60.4 | 37.6 |
| Stable private insurance | 32,073 | 56.0 | 54.8 | 49.7 | 60.2 | 38.3 |
| Stable public insurance | 38,672 | 53.6 | 49.9 | 47.8 | 59.2 | 37.0 |
| Any insurance switches | 9,306 | 57.9 | 55.0 | 53.4 | 61.6 | 38.8 |
| Always uninsured | 7,516 | 60.0 | 54.7 | 48.8 | 64.7 | 36.8 |
a. Data presented based on the 6-month interval, note that some patients may be moving in and out of insurance categories throughout the study period.
b. We performed a test of the differences in unadjusted outcome rates across insurance types within each race/ethnic group, treating Stable Private Insurance as the reference group, accounting only for clustering of observations at the patient level.
Stable private: Always privately insured; Stable public: Always publicly insured (Medicare, Medicaid and/or subsidized); Any insurance switches: includes gain (uninsured to insured), switch but not loss or gain (switch between private, Medicare, Medicaid, and subsidized categories), and insurance loss (insured to uninsured); Always uninsured: No insurance at any point within 6-month interval.
Total # of patients=12470 for the A1c process outcome: 3325 White, 803 Hispanic, 7195 Black,1147 Asian patients were included in analysis.
Table 3 provides the adjusted odds ratios of diabetes-related outcome and process measures by insurance stability category with stable private insurance as the reference group. For the total patient population, any switch in insurance and always being uninsured within a six-month interval was associated with greater odds of poor (AOR 1.14, 95% CI 1.06, 1.23; AOR 1.41, 95% CI 1.28, 1.54) and very poor diabetes (AOR 1.16, 95% CI 1.07, 1.26; AOR 1.32, 95% CI 1.19, 1.26) control compared with having stable private insurance. These findings were statistically significant for NH Black patients (AOR 1.16, 95% CI 1.06, 1.27, AOR 1.44, 95% CI 1.29, 1.60, respectively). Always being uninsured within a six-month interval was associated with a statistically significant increased odds of poor diabetes control compared with stable private insurance among Asians (AOR 1.48, 95% CI 1.04, 2.11) and Hispanics (AOR 1.46, 95% CI 1.03, 2.08). The interaction between insurance instability and racial/ethnic groups was not statistically significant for either of the poor A1c control outcomes. For the A1c process measure, any switch in insurance or being uninsured was significantly associated with better A1c monitoring (lower odds of A1c not being monitored) compared to having stable private insurance for the total patient population.
Table 3. Adjusteda odds ratio of diabetes-related outcomes and process measures by insurance stability within 6-month interval for patients from academic and community health centers, 2005-2013.
| Concurrent Insurance Stability Groupb | n (6-month intervals) | Adjusted Odds Ratio (95% CI) | ||||
| Total patient sample | Non-Hispanic White | Hispanic | Black/African American | Asian/Asian Pacific Islander | ||
| Poor diabetes control (A1c ≥8.0%) | ||||||
| Stable private insurance | 27514 | Ref | Ref | Ref | Ref | Ref |
| Stable public insurance | 32230 | 1.00 (.94, 1.07) | 1.03 (.91 ,1.16) | 1.12 (.84 ,1.49) | .98 (.90, 1.07) | 1.01 (.80, 1.27) |
| Any insurance switches | 7779 | 1.14 (1.06, 1.23) | 1.05 (.89, 1.23) | 1.12 (.82, 1.53) | 1.16 (1.06, 1.27) | 1.18 (.89, 1.58) |
| Always uninsured | 6493 | 1.41 (1.28, 1.54) | 1.22 (.98, 1.51) | 1.46 (1.03, 2.08) | 1.44 (1.29, 1.60) | 1.48 (1.04, 2.11) |
| Interaction race*insurance stability P=.67. | ||||||
| Very poor diabetes control, >9.0% | ||||||
| Stable private insurance | 27514 | Ref | Ref | Ref | Ref | Ref |
| Stable public insurance | 32230 | 1.02 (0.95, 1.10) | 1.00 (.87,1.14) | 1.07 (.78, 1.47) | 1.03 (.94, 1.14) | 1.01 (.77, 1.31) |
| Any insurance switches | 7779 | 1.16 (1.07, 1.26) | 1.15 (.96 1.37) | .99 (.68 ,1.44) | 1.18 (1.06, 1.30) | 1.27 (.90, 1.78) |
| Always uninsured | 6493 | 1.32 (1.19, 1.47) | 1.14 (.89, 1.45) | 1.18 (.79, 1.76) | 1.38 (1.22, 1.55) | 1.38 (.94, 2.03) |
| Interaction race*insurance stability P=.85 | ||||||
| A1c not monitored | ||||||
| Stable private insurance | 33444 | Ref | Ref | Ref | Ref | Ref |
| Stable public insurance | 39498 | .99 (.93, 1.05) | .88 (.78, .98) | .90 (.69, 1.17) | 1.07 (.99, 1.17) | 1.01 (.82, 1.26) |
| Any insurance switches | 9514 | .78 (.72, .83) | .76 (.65, .88) | .70 (.52, .94) | .77 (.70, .85) | 1.04 (.82, 1.31) |
| Always uninsured | 7655 | .86 (.78 ,.94) | .78 (.65, .95) | .88 (.63, 1.22) | .86 (.77, .96) | 1.17 (.86, 1.60) |
| Interaction race*insurance stability P=.005 | ||||||
| Poor BP control, ≥ 130/80 mm Hg | ||||||
| Stable private insurance | 32073 | Ref | Ref | Ref | Ref | Ref |
| Stable public insurance | 38672 | .89 (.85, 0.94) | .81 (.74, .89) | .85 (.69, 1.06) | .94 (.88, 1.01) | .90 (.76, 1.07) |
| Any insurance switches | 9306 | .99 (.93,1.05) | .95 (.83, 1.07) | 1.09 (.84, 1.41) | 1.03 (.95, 1.11) | .92 (.75, 1.12) |
| Always uninsured | 7516 | 1.00 (.92, 1.07) | .86 (.72, 1.02) | .84 (.63, 1.13) | 1.10 (1.00, 1.21) | .76 (.59, .98) |
| Interaction race*insurance stability P=.01 | ||||||
a. Adjusted for time, age, sex, comorbidities, site of care, education, income and race.
b. Data presented based on the 6-month interval, note that some patients may be moving in and out of insurance categories throughout the study period.
Stable private: Always privately insured; Stable public: Always publicly insured (Medicare, Medicaid and/or subsidized); Any insurance switches: includes gain (uninsured to insured), switch but not loss or gain (switch between private, Medicare, Medicaid, and subsidized categories), and insurance loss (insured to uninsured); Always uninsured: No insurance at any point within 6-month interval.
Total # of patients = 12470 for the A1c process outcome: 3325 White, 803 Hispanic, 7195 Black and 1147 Asian patients were included in the analysis.
There was a significant interaction between insurance instability and racial/ethnic groups for the outcomes of A1c monitoring and BP control. The interpretation of the interactions is difficult, as it appears that the effect of being uninsured on increasing the likelihood of A1c monitoring was strongest among NH Whites, whereas the effect of having switches on increasing the likelihood of monitoring was strongest in Hispanics. For BP control, stable public insurance was significantly associated with better BP control (lower odds of poor BP control) compared to stable private insurance for the total patient sample. This finding was statistically significant in NH Whites. NH Blacks who were always uninsured had higher odds of poor BP control compared to those with stable private insurance, while Asians who were uninsured had significantly better BP control compared to those with stable private insurance.
Discussion
The purpose of this study was to explore whether insurance stability is associated with diabetes care outcomes and processes among a racially/ethnically diverse population receiving care at two urban health care systems. This analysis allows an explicit examination of health insurance stability as a lever to reduce racial/ethnic health disparities in diabetes care and management. Our findings suggest that insurance stability is associated with improved diabetes control as measured by A1c outcome measures for our patient population overall. Poor diabetes outcomes, as defined by A1c measurements, were more likely in patients who were always uninsured or who experienced changes in their insurance status, compared with patients who had stable private insurance. Our study did not demonstrate that insurance stability reduced or eliminated ethnic/racial health disparities in diabetes outcome measures.
This study highlights differences in insurance stability by race and the negative impacts of being uninsured. In particular, Hispanic patients in our sample experienced the highest rates of not being insured, similar to national trends.16 These national trends may be attributed to the influence of immigration status on access to clinical care, with fewer noncitizen immigrants having Medicaid or employer-based insurance, depending on the type of employment (ie, hourly wage jobs).16 Similarly, NH Black patients also experienced high rates of being uninsured and having insurance switches. Types of employment, fluctuations in employment status within these groups, and differences in availability of employer sponsored health insurance as well as immigration status could be potential drivers in the differences observed in the types of insurance prevalent among each racial/ethnic group. Additional barriers exist for access and participation in employee-based insurance such as temporary employment, cost, and lack of agency to apply for benefits, which may be based in cultural beliefs and health literacy. For example, NH Whites had the highest prevalence of private insurance compared with other racial/ethnic groups in our patient sample---with Hispanics and Asians having the highest rates of stable public insurance status. Also noteworthy is the smaller number of uninsured in our study sample from health care systems providing care to underserved populations (~10%) compared with concurrent national data, 19.3%-20.5% from 2005-2013 according to data from the Centers for Disease Control and Prevention.17 This reflects the positive impact of Massachusetts’ Medicaid expansion in 2006-07 on increasing the population with stable insurance coverage. It also underscores the Affordable Care Act and additional health care reform as an effective strategy to increase insurance access.18,19
This study also includes unexpected findings, with contradictory results for the relationship between insurance status and BP and glycemic control. For example, among Asians, being uninsured was associated with better BP control yet worse glycemic control. These findings among Asians may in part relate to small samples sizes. However, the findings also relate to the differences in the effectiveness of the standard of care and the complexities of the treatment of hypertension and diabetes. For example, diabetes requires modification of a set of behaviors including exercise and diet as well as medication adherence, and therefore insurance alone may not be sufficient if there is no coverage for behavior management. These findings warrant further investigation.
The fact that poor diabetes management is still present in those with stable private and public insurance categories also highlights the need for more programs and systems (eg, insurance coverage for case management and behavioral interventions) to address DM care among those who have insurance. Once patients leave the clinical setting, societal context and other social factors also play a role in the engagement of behaviors (eg, diet and physical activity) and other factors (eg, stress) that contribute to disease management and progression.
This study provided a unique opportunity to link insurance coverage data with clinical outcomes to compare gaps and changes in insurance status by racial/ethnic groups. Specifically, data on insurance switches and gaps are not typically found in administrative databases of individual insurance providers and clinical outcomes such as A1c and blood pressure are not available in all-payer claims databases. Additionally, the study findings highlight the importance of stable public insurance (ie, Medicaid) as a safety net for vulnerable populations given the similar outcomes demonstrated for stable private (ie, employer-based coverage) and public insurance among all racial/ethnic groups, independent of income differences between the groups in the study.
Overall, this study aligns with recent literature on the influence of insurance reform on clinical outcomes. Results from a 2015 study demonstrated that Massachusetts Health reform was not found to be associated with lower racial and ethnic disparities in hospital admission rates.20 A 2017 study examining the relationship between insurance switches and new physician and emergency department visits found insurance switches to be common and associated with increased physician visits and increased utilization of the emergency department temporarily among those with public insurance.21 Another study looking at churning, or transitions in and out of Medicaid, found an association between insurance changes and disruptions in access and continuity of care, leaving low-income, working adults who are more susceptible to income and employment changes more vulnerable to disruptions in care.22
In our study, the association of insurance switches and poor (A1c ≥8.0%) and very poor diabetes (>9.0%) control among NH Black patients and the total patient population is noteworthy. While this insurance stability category combines any type of change in insurance status (switch between insurance types, insurance loss, and insurance gain), it emphasizes the burden to patients associated with insurance instability and changes. For example, a switch in insurance classification can signify changes in co-pays, new providers, new medications, and overall changes in coordination of care. These burdens can therefore introduce delays and other unseen costs in seeking services in populations that are already more vulnerable due to social circumstances.
A significant interaction was found for race/ethnicity and insurance stability category for BP control, suggesting a differential influence of insurance stability by race/ethnicity. There was an association between stable public insurance and better BP control among the total patient population and NH Whites compared with having stable private insurance. Among NH Blacks, always being uninsured was associated with higher odds of poor BP control and conversely, among Asians, always being uninsured was associated with better BP control.
A1c is a widely used and standard practice of care to monitor diabetes.23 Our data suggest that disparities exist in the monitoring of A1c among different racial/ethnic groups.24 Specifically, a significant interaction was found for race/ethnicity and insurance stability category for the A1c process measure, suggesting a differential influence of insurance stability by race/ethnicity. An unexpected study finding includes better A1c monitoring for patients experiencing any insurance switch or being uninsured for the NH White and NH Black patients and total patient population. One possible explanation for these findings is the increased likelihood for A1c testing in uninsured or newly insured patients who seeks medical care with new providers.
Study Limitations
Although this study adds to the research literature by examining health disparities, insurance stability, and DM outcomes using a large, diverse, patient sample, there are limitations worth noting. The study is restricted in its applicability to patients who are receiving primary care and cannot be extrapolated to those patients who cease to seek care due to insurance loss, insurance switches, or any other circumstances not explored in this study. The study findings therefore may underestimate the influence of insurance loss and switches on diabetes outcomes and care.
Another limitation of this study is our inability to control for other social factors that influence access to care (ie, co-pays and deductibles, transportation, living conditions, built-environment, immigration status, etc.). This study assumes that those who are insured will seek care, however, other social circumstances may prevent patients from seeking care regularly and as recommended by their primary care physician. Some but not all studies demonstrate race, independent of insurance and socioeconomic status, as a significant predictor of diabetes and glycemic control, and social conditions as more impactful in shaping health overall.25,26 A growing body of intervention research is exploring the influence of assessing for individual-level social factors and addressing social needs in order to improve clinical care and patient outcomes.27-29 More research and innovation is needed in this area, however.
Conclusion
Overall, this study makes a significant contribution to the research literature by exploring how insurance stability status is associated with racial/ethnic health disparities in diabetes care and management. While our study findings underscore the importance of insurance status stability in diabetes management, particularly for glycemic control, for the examined patient population overall, it does not support the notion that health insurance stability is a sufficient strategy to reduce racial/ethnic health disparities in diabetes outcomes. Further research needs to explore and address other social factors and determinants of health that impact diabetes management and control in order to eliminate existing disparities by race/ethnicity.
Acknowledgments
The project described was supported by the National Center for Advancing
Translational Sciences and National Institute on Minority Health and Health Disparities, National Institutes of Health (UL1TR001064 and R01MD007735, respectively). NRK is supported in part by a Senior VA Health Services Research & Development Service Research Career Scientist award (#02-066-1).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; the U.S. Department of Health and Human Services or the Department of Veterans Affairs.
This research was approved by the Tufts Health Sciences Campus Institutional Review Board for the Protection of Human Subjects.
References
- 1.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033-1046. 10.2337/dc12-2625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Number of Americans with diabetes projected to double or triple by 2050. Atlanta, GA: Center for Disease Control. 2010. Oct. Last accessed October 25, 2020 from https://www.cdc.gov/media/pressrel/2010/r101022.html
- 3.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of medicare coverage. Ann Intern Med. 2009;150(8):505-515. 10.7326/0003-4819-150-8-200904210-00005 10.7326/0003-4819-150-8-200904210-00005 [DOI] [PubMed] [Google Scholar]
- 4.Healthy People 2020. Washington, DC: U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Last accessed October 25, 2020 from https://www.healthypeople.gov/
- 5.Brooks EL, Preis SR, Hwang S-J, et al. Health insurance and cardiovascular disease risk factors. Am J Med. 2010;123(8):741-747. 10.1016/j.amjmed.2010.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gold R, DeVoe J, Shah A, Chauvie S. Insurance continuity and receipt of diabetes preventive care in a network of federally qualified health centers. Med Care. 2009;47(4):431-439. 10.1097/MLR.0b013e318190ccac 10.1097/MLR.0b013e318190ccac [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu R, Shi L, Rane S, Zhu J, Chen C-C. Insurance, racial/ethnic, SES-related disparities in quality of care among US adults with diabetes. J Immigr Minor Health. 2014;16(4):565-575. 10.1007/s10903-013-9966-6 10.1007/s10903-013-9966-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang JX, Huang ES, Drum ML, et al. Insurance status and quality of diabetes care in community health centers. Am J Public Health. 2009;99(4):742-747. 10.2105/AJPH.2007.125534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang JX, Bhaumik D, Huang ES, Meltzer DO. Change in insurance status and cost-related medication non-adherence among older US adults with diabetes from 2010 to 2014. J Health Med Econ. 2018;4(2):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med. 2016;176(10):1501-1509. 10.1001/jamainternmed.2016.4419 [DOI] [PubMed] [Google Scholar]
- 11.Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. JAMA. 2015;314(4):366-374. 10.1001/jama.2015.8421 [DOI] [PubMed] [Google Scholar]
- 12.Sommers BD, Musco T, Finegold K, Gunja MZ, Burke A, McDowell AM. Health reform and changes in health insurance coverage in 2014. N Engl J Med. 2014;371(9):867-874. 10.1056/NEJMsr1406753 [DOI] [PubMed] [Google Scholar]
- 13.McDonough JE, Rosman B, Butt M, Tucker L, Howe LK. Massachusetts health reform implementation: major progress and future challenges. Health Aff (Millwood). 2008;27(4)(suppl 1):w285-w297. 10.1377/hlthaff.27.4.w285 10.1377/hlthaff.27.4.w285 [DOI] [PubMed] [Google Scholar]
- 14.Burant C. Medical Management of Type 2 Diabetes. Arlington, VA: American Diabetes Association; 2012. [Google Scholar]
- 15.National Committee for Quality Assurance [cited 2019 January 2]; Last accessed October 25, 2020 from https://www.ncqa.org/hedis/measures/comprehensive-diabetes-care/.
- 16.Ku L, Matani S. Left out: immigrants’ access to health care and insurance. Health Aff (Millwood). 2001;20(1):247-256. 10.1377/hlthaff.20.1.247 [DOI] [PubMed] [Google Scholar]
- 17.National Center for Health Statistics, National Health Interview Survey Health insurance supplements, 1984-2016. 2017. Last accessed October 25, 2020 from https://www.cdc.gov/nchs/data/hus/2017/105.pdf.
- 18.Sommers BD, Kronick R. The Affordable Care Act and insurance coverage for young adults. JAMA. 2012;307(9):913-914. 10.1001/jama.307.9.913 [DOI] [PubMed] [Google Scholar]
- 19.Buchmueller TC, Levinson ZM, Levy HG, Wolfe BL. Effect of the Affordable Care Act on racial and ethnic disparities in health insurance coverage. Am J Public Health. 2016;106(8):1416-1421. 10.2105/AJPH.2016.303155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCormick D, Hanchate AD, Lasser KE, et al. Effect of Massachusetts healthcare reform on racial and ethnic disparities in admissions to hospital for ambulatory care sensitive conditions: retrospective analysis of hospital episode statistics. BMJ. 2015;350(mar30 9):h1480. 10.1136/bmj.h1480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barnett ML, Song Z, Rose S, Bitton A, Chernew ME, Landon BE. Insurance transitions and changes in physician and emergency department utilization: an observational study. J Gen Intern Med. 2017;32(10):1146-1155. 10.1007/s11606-017-4072-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roberts ET, Pollack CE. Does churning in Medicaid affect health care use? Med Care. 2016;54(5):483-489. 10.1097/MLR.0000000000000509 10.1097/MLR.0000000000000509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saudek CD, Brick JC. The Clinical Use of Hemoglobin A1c. Thousand Oaks, CA: SAGE Publications; 2009. 10.1177/193229680900300402 [DOI] [Google Scholar]
- 24.Brown AF, Gregg EW, Stevens MR, et al. Race, ethnicity, socioeconomic position, and quality of care for adults with diabetes enrolled in managed care: the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care. 2005;28(12):2864-2870. 10.2337/diacare.28.12.2864 [DOI] [PubMed] [Google Scholar]
- 25.Heidemann DL, Joseph NA, Kuchipudi A, Perkins DW, Drake S. Racial and economic disparities in diabetes in a large primary care patient population. Ethn Dis. 2016;26(1):85-90. 10.18865/ed.26.1.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pincus T, Esther R, DeWalt DA, Callahan LF. Social conditions and self-management are more powerful determinants of health than access to care. Ann Intern Med. 1998;129(5):406-411. 10.7326/0003-4819-129-5-199809010-00011 10.7326/0003-4819-129-5-199809010-00011 [DOI] [PubMed] [Google Scholar]
- 27.Gottlieb LM, Tirozzi KJ, Manchanda R, Burns AR, Sandel MT. Moving electronic medical records upstream: incorporating social determinants of health. Am J Prev Med. 2015;48(2):215-218. 10.1016/j.amepre.2014.07.009 [DOI] [PubMed] [Google Scholar]
- 28.Gottlieb L, Hessler D, Long D, Amaya A, Adler N. A randomized trial on screening for social determinants of health: the iScreen study. Pediatrics. 2014;134(6):e1611-e1618. 10.1542/peds.2014-1439 [DOI] [PubMed] [Google Scholar]
- 29.Pinto AD, Glattstein-Young G, Mohamed A, Bloch G, Leung FH, Glazier RH. Building a foundation to reduce health inequities: routine collection of sociodemographic data in primary care. J Am Board Fam Med. 2016;29(3):348-355. 10.3122/jabfm.2016.03.150280 10.3122/jabfm.2016.03.150280 [DOI] [PubMed] [Google Scholar]


