Abstract
Background
The Bronx has the highest prevalence of asthma in the United States (US), and was also an early COVID-19 epicenter, making it a unique study location. Worldwide reports describe significant declines in pediatric emergency department (PED) visits during COVID-19. The ongoing impact of COVID-19 on all PED presentations, including asthma, at an early epicenter has not been studied beyond the pandemic peak and into the early phases of state re-opening.
Objectives
To compare PED health-seeking behaviors and clinical characteristics during the 2020 pandemic and subsequent initial New York State (NYS) phased re-opening to the same period in 2019.
Methods
Retrospective chart review of children <21 years utilizing the PED at a high-volume quaternary children's hospital in The Bronx, NY from March 15th 2020 – July 6th 2020 (pandemic cohort) and the same interval in 2019 (comparison cohort). Visits were assigned to pre-determined diagnostic categories. Demographic and clinical data were compared.
Results
19,981 visits were included. Visits declined by 66% during 2020. Proportions of asthma visits (2% vs. 7%, p < 0.0001) and minor medical problems (61% vs. 67%, p < 0.0001) had significant declines in the pandemic cohort, while major medical problems (13% vs. 8%, p < 0.0001), appendicitis (1% vs. 0.4%, p < 0.0001) and other surgical complaints (1% vs. 0.5%, p < 0.0001) had proportional increases in the pandemic cohort. No significant proportional changes were noted among psychosocial and trauma groups between the two cohorts.
Conclusion
The pandemic cohort experienced a substantial decrease in PED volume, but an increase in acuity and admission rates, which was sustained through the NYS phase-II re-opening. Despite being located in an asthma hub, the incidence of asthma-related PED visits declined appreciably in the pandemic cohort. Future studies examining the effects of indoor allergens in isolation on pediatric asthma are warranted.
Keywords: Pediatric emergency medicine, COVID-19, Epicenter, Asthma
Abbreviations: CDC, Centers for Disease Control and Prevention; ESI, Emergency Severity Index; IQR, Interquartile Ranges; MIS-C, Multisystem inflammatory syndrome in children; NYC, New York City; NYS, New York State; PED, Pediatric Emergency Department; US, United States; WHO, World Health Organization
1. Introduction
The novel coronavirus, SARS-CoV-2, and the disease it causes, COVID-19, were first reported in December 2019 in Wuhan, China [1] and declared a pandemic by the World Health Organization (WHO) in March 2020 [2]. Reports from sites affected early in the pandemic, mainly China and Europe, showed a relative sparing of children from severe morbidity and mortality associated with COVID-19 [[3], [4], [5], [6], [7]]. As US grew to have the highest number of confirmed cases, similar favorable pediatric prognosis patterns were observed [3]. Even after the US Centers for Disease Control and Prevention (CDC) released a May 2020 health advisory reporting a multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19, children continued to have a favorable prognosis consistent with previous reports [[8], [9], [10]].
Efforts to mitigate disease transmission, such as social-distancing measures, state lockdowns and school and recreational space closures also altered the pediatric medical landscape [11,12]. All aspects of pediatric medical care experienced a decrease in volume worldwide [13], including a significant reduction in PED visits [[14], [15], [16], [17], [18]]. At the same time, an increase in patient acuity was reported, [4,15,[17], [18], [19]]. While some studies have attributed this to a possible delay in seeking care due to intentional avoidance of health care facilities during the pandemic [16,19], Dean et al. found a large absolute decrease in PED critical care patients during the pandemic period, despite representing a high proportion of overall visits [20]. Recently, Chaiyachati et al. described the clinical profile of patients presenting to the PED at the Children's Hospital of Philadelphia before and during the pandemic peak. With the exception of increased ingestions, chief complaints remained similar when compared to the 3 years prior, despite a dramatic decrease in volume and increase in acuity [15].
The Bronx, New York was one of the earliest epicenters for the COVID-19 pandemic and as of November 2020, is the county in the US with the 5th most COVID-19 related deaths [21]. The prevalence and morbidity of pediatric asthma in the Bronx are the highest in the nation, [22] including the highest rates of asthma-related hospitalizations and deaths in New York City (NYC) [23,24]. Prior studies have shown that genetic and environmental factors play important roles in the pathogenesis of pediatric asthma. Among the environmental factors, allergens within the home environment, as well as those associated with inner-city living, have been shown to contribute towards an asthma diagnosis. Exposures to cockroaches, mice and mold are well-described asthma risk factors, along with increased early-in-life tobacco smoke exposure, decreased breast-feeding exposure and diet [25]. Poor air quality associated with inner-city living has attributed to the higher incidence of asthma among inner city children [22]. As COVID-19 is a respiratory pathogen, there were heightened concerns that children with asthma in the Bronx would be more susceptible to COVID-19.
To date, most data reported has focused on PED trends before and during the pandemic peak [14,15,18,26] and a recent study looking beyond the height of the pandemic was limited to critically ill children [27]. Unique to our study, are the reported initial effects of a state phased re-opening on all PED trends in a known COVID-19 epicenter. Additionally, though Kenyon et al recently described the effects of COVID-19 on PED asthma visits [28], this study attempts to describe these effects beyond the pandemic peak, at a known asthma and COVID-19 epicenter.
The objectives of this study were to (1) determine the impact of COVID-19 on PED health-seeking behaviors, volume, acuity and common presenting ailments, including asthma, at an epicenter, compared to the same interval 1 year prior; and (2) to determine if any noted trends correlated with the NYS stay-at-home executive orders and initial state phased re-opening dates.
2. Methods
2.1. Study design
This was a retrospective chart review at a large urban quaternary academic children's hospital in the Bronx, New York during the following time periods: March 15th 2020 – July 6th 2020 (pandemic cohort) and the same interval in 2019 (comparison cohort). The dates selected aimed to capture trends from 1 week before the NYC “shelter-in-place” order (March 22nd 2020) until the end of NYS phase II re-opening (July 6th 2020) to show the immediate pre-and post- state mandate PED trends. This study was reviewed and approved as exempt by the Albert Einstein College of Medicine Institutional Review Board.
2.2. Study population
Inclusion criteria were age < 21 years and having been evaluated in the PED during the specified time frame. Exclusion criterion was a disposition of “left without being seen.”
2.3. Data collection
Demographic data, Emergency Severity Index (ESI) level based acuity, disposition (admission, discharge, left against medical advice, eloped after medical assessment or transferred to another medical center), and clinical diagnosis were collected through electronic chart review (EPIC® VX.X) with a query for arrival at the CHAM Emergency Department, age < 21 during the aforementioned times, assigned diagnosis and no LWBS disposition. Definitions for eight broad diagnostic categories were created prior to data collection by the authors (RL, DF, JJ, HK). Categories included: Asthma, COVID-19 related illness, Minor Medical Problems, Major Medical Problems, Psychosocial, Surgical, Appendicitis and Trauma (Table 1 ).
Table 1.
Diagnostic category classifications and definitions.
| Diagnostic category | Definition |
|---|---|
| Asthma-related Illness |
|
| COVID-19-related Illness |
|
| Major Medical Problems |
|
| Minor Medical Problems |
|
| Psychiatric/Psychosocial |
|
| Surgical, excluding Appendicitis |
|
| Trauma |
|
| Appendicitis |
|
To maintain a high inter-rater agreement when assigning diagnoses into eight categories, two investigators (RL and JJ) independently reviewed the same 2 days of data outside of the study date range, using the predetermined guide. An inter-rater agreement of 98.5% (279/283 sample charts) was reached between the two investigators for the two sample days. The same two investigators (RR, JJ) then independently assigned diagnostic categories to each visit in the study dataset based on the chief complaint and admission/discharge diagnoses. The investigators alternated between days to avoid additional bias.
2.4. Statistical analyses
Frequency distributions for demographics and patient disposition were examined. Patients assigned ESI level 1 or 2 were considered high acuity and ESI levels 3–5 were low acuity. Categorical data (e.g. disposition, ESI, and diagnosis classification) were summarized as proportions and compared by time period (2020 vs. 2019) using Pearson's chi-square test. Age was reported as medians with interquartile ranges (IQR) and age between both years was compared using the nonparametric Mann-Whitney U test.
3. Results
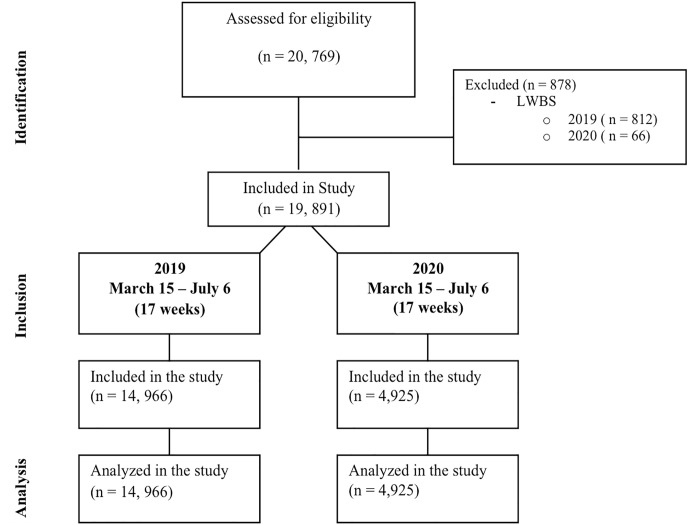
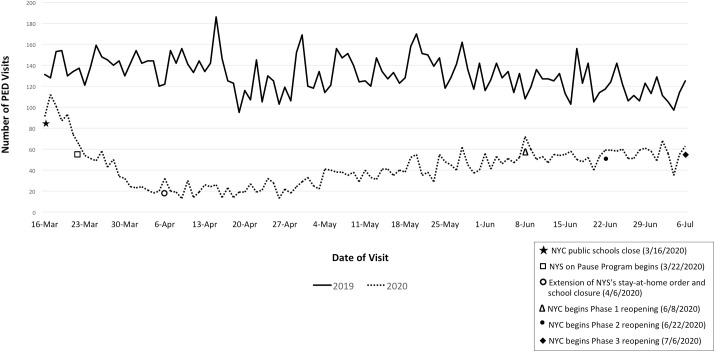
A total of 19,981 visits were included and analyzed: 14,996 PED visits from the 17-week period in 2019 and 4925 visits from the corresponding 17-week period in 2020 (Fig. 1 ). The 2020 pandemic cohort was significantly older than the 2019 cohort, (median ages = 7 yr. vs. 6 yr., p < 0.0001) and there was no difference in the gender distribution between the two cohorts. Pandemic PED visits were more likely to be categorized as having high acuity (24% vs. 17%, p < 0.0001) and had higher admission rates (17% vs. 11%, p < 0.0001) (Table 2 ). There was an overall decline of 66% in the total number of PED visits in the pandemic cohort compared to the 2019 comparison cohort. This decrease was most pronounced on April 6th, 2020, where the lowest daily census in the pandemic cohort corresponded with the extension of the NYS stay-at-home and school closure order (Fig. 2 ). The overall volume decrease continued throughout the pandemic and was sustained through the early stages of NYS phased re-openings, with the daily census during the phase I and II re-opening dates remaining nearly half of what it was at the same time the year prior (Fig. 2).
Fig. 1.
Flow diagram of patient chart inclusion.
Table 2.
Comparison of patient characteristics between pandemic and comparison cohort.
| 2019 Cohort n = 14,966 | 2020 Cohort n = 4925 | p-Value | |
|---|---|---|---|
| Age, median (IQR) years | 6 (2−13) | 7 (2–16) | <0.0001 |
| Gender, Female n (%) | 7280 (49) | 2459 (50) | 0.082 |
| High Acuity (ESI 1 & 2) n (%) | 2577 (17) | 1175 (24) | <0.0001 |
| PED Disposition Admission n (%) | 1673 (11) | 832 (17) | <0.0001 |
The bold p-values represent those of statistical significance
Fig. 2.
PED daily census in the pandemic vs. comparison cohorts.
The proportion of major medical problems (13% vs. 8%, p < 0.0001), appendicitis (1% vs. 0.4%, p < 0.0001) and other surgical complaints (1% vs. 0.5%, p < 0.0001), were higher in 2020, while declines were observed in minor medical problems (61% vs. 67%, p < 0.0001) and asthma (2% vs. 7%, p < 0.0001) presentations (Table 3 ). No significant proportional changes were noted among psychosocial and trauma groups (Table 3). There were no differences in gender or acuity level between the 2 years in patients who presented with asthma; however, the asthma group from the pandemic cohort was significantly older (7 vs. 5, p < 0.008) and more likely to be admitted (18% vs. 12%, p < 0.002) (Table 4 ). PED COVID-19 related visits represented 4% (196/4925) of the total patients seen in 2020 cohort. Of that group, 30% were admitted to the hospital (58/196) and 12% were admitted directly to the Intensive Care Unit from the ED (7/58).
Table 3.
Comparison of visit numbers and percentages per diagnostic category between pandemic and comparison cohort.
| Diagnostic category | 2019 |
2020 |
p-Value |
|---|---|---|---|
| n = 14,966 | n = 4925 | ||
| Asthma-related Illness n (%) | 987 (7%) | 119 (2%) | <0.0001 |
| COVID-19-related Illness n (%) | 0 (0%) | 199 (4%) | <0.0001 |
| Major Medical Problems n (%) | 1258 (8%) | 641 (13%) | <0.0001 |
| Minor Medical Problems n (%) | 9980 (68%) | 2984 (61%) | <0.0001 |
| Psychiatric/Psychosocial n (%) | 607 (4%) | 197(4%) | 0.863 |
| Surgical, excluding Appendicitis n (%) | 68 (0.5%) | 46 (1%) | <0.0001 |
| Trauma n (%) | 2000 (13%) | 671 (14%) | 0.642 |
| Appendicitis n (%) | 66 (0.4%) | 68 (1%) | <0.0001 |
The bold p-values represent those of statistical significance
Table 4.
Comparison of PED asthma presentations between pandemic and comparison cohort.
| 2019 Cohort: Asthma |
2020 Cohort: Asthma |
p-Value | |
|---|---|---|---|
| n = 987 | n = 119 | ||
| Age, median (IQR) years | 5 (3−10) | 7 (3–15) | <0.008 |
| Gender, Female n (%) | 392 (40) | 55 (46) | 0.172 |
| High Acuity (ESI 1 & 2) n (%) | 465 (47) | 48 (49) | 0.752 |
| PED Disposition Admission n (%) | 122 (12) | 27 (18) | <0.002 |
The bold p-values represent those of statistical significance
4. Discussion
Consistent with national [[14], [15], [16],18] and international reports [29], we observed a substantial decrease in the total volume of pediatric patients seeking emergency care during the 2020 pandemic period. This decrease was observed from the start of the COVID-19 pandemic in the Bronx and continued through the NYS phase II re-opening, despite an eventual decrease in city and state COVID-19 related illness and deaths. Although we cannot fully explain the trend that we observed locally, or that reported worldwide, it is likely multifactorial. Firstly, the SARS-CoV-2 virus has a relatively predictable pattern in children, with minimal to no symptoms [3]. Even with more severe presentations, children continue to have a favorable prognosis [9] and were relatively spared from significant morbidity and mortality during this pandemic. Second, “shelter-in-place” orders and school closures greatly reduce exposure risk and common seasonal virus spread. Spread of all infectious agents, including COVID-19, was likely reduced even further with the emphasis placed on simple self-protective measures, such as mask wearing, frequent hand washing and social distancing.
Despite the decrease in volume, there were significant increases in patient acuity and admission rates during the 2020 pandemic. Congruent with this was a significant increase in the proportion of visits in the major medical problem diagnostic category (13% vs. 8%, p < 0.0001), which other studies have reported as well [15,18,26]. Although firm conclusions regarding these trends cannot be established at this time, we think that they likely reflect a multifactorial change in healthcare seeking behavior among pediatric patients and their caregivers during the pandemic. It is possible that intentional avoidance of the PED may have lead to a delay in seeking care, thereby increasing overall morbidity [19,29]. Likewise, the lack of contact with primary care physicians and pediatric subspecialty office closures may have increased acuity. In contrast, the relative proportional increase in acuity may in fact be due to a significant absolute decline among lower acuity patients [27], possibly resulting from an increase in self-management of non-emergent minor medical complaints at home.
The Bronx borough of NYC has the highest asthma prevalence and morbidity in the country [30], with pediatric asthma in the Bronx being nearly twice the national average [22]. Given that COVID-19 is a respiratory pathogen, we anticipated an increase in asthma exacerbations and new presentations. However, instead, we observed an impressive decline in the relative proportion of PED asthma presentations, similar to the recent findings reported by Kenyon et al [28] in other regions of the country. While we cannot conclude if patients self-treated at home or did not have exacerbations at all, we suspect that the same aforementioned factors influencing volume decline played a role in reducing asthma presentations. School closures and social distancing measures decreased exposures to common pathogens that cause pediatric illness [2] and trigger asthma exacerbations. Improved air quality, in part due to reduced road and air traffic, may have positively impacted asthmatics. Furthermore, “shelter-in-place” orders during high pollen season, likely reduced external allergen exposure in the early spring, possibly reducing allergy induced reactive airway disease. Home aeroallergens such as cockroaches, mice and mold have long been described as known triggers for asthma exacerbation [22]. Given the dramatic increase in time spent indoors due to the pandemic, there was concern that this may negatively impact asthmatics; yet, our data reflects the opposite. Like that suggested by Kenyon et al., we suspect that indoor aeroallergens may have less of an impact on asthma exacerbations than previously thought [28]. Overall, our findings support the significant role environmental factors contribute towards asthma pathogenesis, as even in a well-known asthma hub, we report a dramatic decline in asthma PED visits that occurred simultaneously with drastic behavioral and environmental modifications as public health initiatives.
Given the pandemic's high mortality and morbidity and the associated anxiety this yields, health care providers anticipated the need for increased mental health services; yet, our data did not show a significant difference in the proportions of patients presenting with psychiatric/psychosocial complaints between the two cohorts. This may be explained by the fact that significant portions of pediatric mental health evaluations come from school referrals with school-related stress [31,32]. Studies have demonstrated a direct correlation between mental health visits to the PED and school attendance [[32], [33], [34]], though pandemic related stress, which will continue to be part of our new normal, may have different referral patterns. Our study period is likely not long enough to reflect any long term changes in patterns of utilization of mental health services. The proportion of patients utilizing the PED for surgical conditions was significantly higher in 2020, including appendicitis presentations. Other NYC Children's Hospitals reported similar findings [35], possibly demonstrating that COVID-19 may have had less of a collateral effect on surgical diagnoses, juxtaposed to asthma. The Bronx experienced a significant increase in ill adults due to COVID-19 [21], to the point that our Children's Hospital was converted to care for adults [36]; however, the pediatric volume of those seeking care due to COVID-19 remained comparatively low. Nonetheless, similar to previous reports, those presenting with COVID-19 related complaints had high overall admission rate, including direct ICU admissions from the ED [37,38]. This suggests that although typically mild, COVID-19 and resultant complications such as MIS-C, should not be taken lightly in those sick enough to be brought to the PED for evaluation.
Since the onset of this pandemic, the PED volume has dropped precipitously with the most pronounced drop occurring during the peak of the pandemic in NYC in early April 2020 (Fig. 3.) As of July 2020, NYC appears to be slowly recovering, with many New Yorkers returning to work and the resumption of non-essential services; yet, the PED visit volume remains low compared to the year prior. The emphasis placed on self-protection with face coverings, frequent hand washing and social distancing are likely to extend beyond the pandemic and may reduce subsequent viral exposure [39], having a lasting effect on the wellbeing of children.
5. Limitations
Our study had several limitations: First, as is the nature with all chart review retrospective studies, our data is limited by incomplete and inaccurate data; however, limiting the cohort to charts with complete electronic records mitigated this. Secondly, this was a chart review at a single academic center; however, recently published data from other single institutions reflects similar pediatric emergency department utilization patterns [15] suggesting our results may be generalizable to other institutions.
6. Conclusion
Our data showed a substantial decrease in overall PED volume, but increased acuity and admission rates that persisted throughout the NYS phase II re-opening, which helps describe the effects of school closures, “shelter-in-place” orders and initial state phased re-openings in a COVID-19 epicenter on pediatric illness patterns. Efforts at all levels of the healthcare system directed at educating patients and caregivers of the need for appropriate health seeking behavior should be addressed. The observed significant reduction of emergency care utilization among pediatric asthmatics in the Bronx, where asthma prevalence is three times the national average, not only highlights the complex interactive nature of various allergens on asthma exacerbations, but also provides an optimistic outlook on the modifiable external factors that play significant roles in the wellbeing of children with asthma. Future studies examining the effects of indoor allergens in isolation on pediatric asthma are warranted.
Declaration of competing interest
The authors have none to disclose.
Acknowledgments
Acknowledgements
The Pediatric Emergency Department and The Pediatric Scholarly Oversight Committee at the Children's Hospital at Montefiore.
Funding/Support
No funding was secured for this study.
Contributors' statement
Dr. Levene conceptualized and designed the study; acquired and organized the data from the EMR, coded data, assisted with data analysis, designed figures and tables, drafted the initial manuscript and reviewed and revised the manuscript.
Dr. Fein conceptualized and designed the study, acquired and organized the data from the EMR, drafted the initial manuscript and reviewed and revised the manuscript.
Dr. Silver carried out the data analysis and reviewed and revised the manuscript.
Dr. Joels organized, coded data, designed figures and reviewed and revised the manuscript.
Dr. Khine conceptualized and designed the study, drafted the initial manuscript and critically reviewed and revised the manuscript.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
- 1.Control, C.f.D. and Prevention . 2020. Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19) 2020. [Google Scholar]
- 2.World Health Organization Rolling updates on coronavirus disease (COVID-19) 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen [cited 2020 June 1]; Available from:
- 3.Ludvigsson J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dong Y., et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020 doi: 10.1542/peds.2020-0702. [DOI] [Google Scholar]
- 5.Tagarro A., et al. Screening and severity of coronavirus disease 2019 (COVID-19) in children in Madrid, Spain. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thornton J. Covid-19: A&E visits in England fall by 25% in week after lockdown. Br Med J Publish Group. 2020 doi: 10.1136/bmj.m1401. [DOI] [PubMed] [Google Scholar]
- 7.Parri N., et al. COVID-19 in 17 Italian pediatric emergency departments. Pediatrics. 2020 doi: 10.1542/peds.2020-1235. [DOI] [PubMed] [Google Scholar]
- 8.Hoang A., et al. COVID-19 in 7780 pediatric patients: a systematic review. EClinicalMedicine. 2020:100433. doi: 10.1016/j.eclinm.2020.100433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castagnoli R., et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. April 22, 2020;174(9) doi: 10.1001/jamapediatrics.2020.1467. [published online ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Jamal N., et al. Biphasic variation over time in presenting features of patients with COVID-19. Pediatrics. 2020;146(5) doi: 10.1542/peds.2020-014902. [DOI] [PubMed] [Google Scholar]
- 11.Cluver L., et al. Parenting in a time of COVID-19. Lancet. 2020;395(10231) doi: 10.1016/S0140-6736(20)30736-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheridan G.A., et al. Pediatric trauma and the COVID-19 pandemic: a 12-year comparison in a level-1 trauma center. HSS J. 2020:1–5. doi: 10.1007/s11420-020-09807-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Santoli J.M. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration—United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6919e2. [DOI] [PubMed] [Google Scholar]
- 14.Hartnett K.P., et al. Impact of the COVID-19 pandemic on emergency department visits – United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaiyachati B.H., et al. Trends in pediatric emergency department utilization after institution of COVID-19 mandatory social distancing. J Pediatr. 2020;226 doi: 10.1016/j.jpeds.2020.07.048. 10.1016/j.jpeds.2020.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Isba R., et al. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch Dis Child. 2020;105(7) doi: 10.1136/archdischild-2020-319385. PMID: 32376695. [DOI] [PubMed] [Google Scholar]
- 17.Jeffery M.M., et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180(10):1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Even L., et al. Pediatric emergency department volumes and throughput during the COVID-19 pandemic. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.09.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lazzerini M., et al. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4(5):e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dean P., Zhang Y., Frey M., et al. The impact of public health interventions on critical illness in the pediatric emergency department during the SARS-CoV-2 pandemic [published online ahead of print, 2020 Aug 10] J Am Coll Emerg Phys Open. 2020 doi: 10.1002/emp2.12220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.JHU John's Hopkins University: COVID-19 United States cases by county. 2020. https://coronavirus.jhu.edu/us-map [cited 2020 9/4]; Available from:
- 22.Warman K., Silver E.J., Wood P.R. Modifiable risk factors for asthma morbidity in Bronx versus other inner-city children. J Asthma. 2009;46(10):995–1000. doi: 10.3109/02770900903350481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garg R., et al. New York City Department of Health and Mental Hygiene: New York City Childhood Asthma Initiative; 2003. Asthma facts.http://www.nyc.gov/html/doh/downloads/pdf/asthma/facts.pdf [Google Scholar]
- 24.Talib H.J., Lax Y., Reznik M. The impact of a clinical asthma pathway on resident education. Biomed Res Int. 2018 doi: 10.1155/2018/5472876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Whu R., et al. Risk factors for pediatric asthma in the South Bronx. J Asthma. 2007;44(10):855–859. doi: 10.1080/02770900701752516. [DOI] [PubMed] [Google Scholar]
- 26.Dann L., et al. Disappearing act: COVID-19 and paediatric emergency department attendances. Arch Dis Child. 2020;105(8):810–811. doi: 10.1136/archdischild-2020-319654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dean P., et al. The impact of public health interventions on critical illness in the pediatric emergency department during the SARS-CoV-2 pandemic. J Am Coll Emerg Phys Open. 2020 doi: 10.1002/emp2.12220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kenyon C.C., et al. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract. 2020;8(8) doi: 10.1016/j.jaip.2020.05.045. p. 2774–2776.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scaramuzza A., et al. Changing admission patterns in paediatric emergency departments during the COVID-19 pandemic. Arch Dis Child. 2020;105(7):704–706. doi: 10.1136/archdischild-2020-319397. [DOI] [PubMed] [Google Scholar]
- 30.Witonsky J., et al. The association of environmental, meteorological, and pollen count variables with asthma-related emergency department visits and hospitalizations in the Bronx. J Asthma. 2019;56(9):927–937. doi: 10.1080/02770903.2018.1514627. [DOI] [PubMed] [Google Scholar]
- 31.Benarous X., et al. Changes in the use of emergency care for the youth with mental health problems over decades: a repeated cross sectional study. Front Psych. 2019;10:26. doi: 10.3389/fpsyt.2019.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goldstein A.B., et al. Mental health visits in a pediatric emergency department and their relationship to the school calendar. Pediatr Emerg Care. 2005;21(10):653–657. doi: 10.1097/01.pec.0000181420.56729.4f. [DOI] [PubMed] [Google Scholar]
- 33.Hoffmann J.A., et al. Trends in visits and costs for mental health emergencies in a pediatric emergency department, 2010–2016. Acad Pediatr. 2019;19(4):386–393. doi: 10.1016/j.acap.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 34.Lueck C., et al. Do emergency pediatric psychiatric visits for danger to self or others correspond to times of school attendance? Am J Emerg Med. 2015;33(5):682–684. doi: 10.1016/j.ajem.2015.02.055. [DOI] [PubMed] [Google Scholar]
- 35.Kvasnovsky C.L., et al. Limiting operations for acute appendicitis in children: lessons learned from the US epicenter of the COVID-19 pandemic. J Pediatr Surg. 2020 doi: 10.1016/j.jpedsurg.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Philips K., et al. Rapid implementation of an adult coronavirus disease 2019 unit in a children’s hospital. J Pediatr. 2020;222:22–27. doi: 10.1016/j.jpeds.2020.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaushik S., et al. Multisystem inflammatory syndrome in children associated with severe acute respiratory syndrome coronavirus 2 infection (MIS-C): a multi-institutional Study from New York City. J Pediatr. 2020;224:24–29. doi: 10.1016/j.jpeds.2020.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chao J.Y., et al. Clinical characteristics and outcomes of hospitalized and critically ill children and adolescents with coronavirus disease 2019 at a Tertiary Care Medical Center in New York City. J Pediatr. 2020;223 doi: 10.1016/j.jpeds.2020.05.006. p. 14–19.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yeoh D.K., et al. The impact of COVID-19 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1475. [DOI] [PMC free article] [PubMed] [Google Scholar]