Abstract
Background:
Burnout and distress have a negative impact on nurses and the treatment they provide. Our aim was to measure the prevalence of burnout and distress among nurses in a cardiovascular centre at 2 quaternary referral hospitals in Canada, and compare these outcomes to those for nurses at academic health science centres (AHSCs) in the United States.
Methods:
We conducted a survey of nurses practising in a cardiovascular centre at 2 quaternary referral hospitals in Toronto, Ontario, between Nov. 27, 2018, and Jan. 31, 2019. The survey tool included the Well-Being Index (WBI), which measures fatigue, depression, burnout, anxiety or stress, mental and physical quality of life, work–life integration, meaning in work and distress; a score of 2 or higher on the WBI indicated high distress. We also evaluated nurses’ perception of the adequacy of staffing levels and of fair treatment in the workplace, and satisfaction with the electronic health record. We carried out standard univariate statistical comparisons using the χ2, Fisher exact or Kruskal–Wallis test as appropriate to perform univariate comparisons in the sample of respondents. We assessed the relation between a WBI score of 2 or higher and demographic characteristics. We compared univariate associations among WBI data for nurses at AHSCs in the US who completed the WBI to responses from our participants.
Results:
The response rate to the survey was 49.1% (242/493). Of the 242 respondents, 188 (77.7%) reported burnout in the previous month; 189 (78.1%) had a WBI score of 2 or higher, and 132 (54.5%) had a score of 4 or higher (indicative of severe distress). Ordinal multivariable analysis showed that lower WBI scores were associated with satisfaction with staffing levels (odds ratio [OR] 0.33, 95% confidence interval [CI] 0.16–0.69) and the perception of fair treatment in the workplace (OR 0.41, 95% CI 0.23–0.74). Higher proportions of our respondents than nurses at AHSCs in the US reported burnout (77.7% v. 60.5%, p < 0.001) and had a WBI score of 2 or higher (78.1% v. 57.0%) or 4 or higher (54.5% v. 32.0%) (both p < 0.001).
Interpretation:
Although levels of burnout and distress were high among nurses, their perceptions of adequate staffing and fair treatment were associated with lower distress. Addressing inadequate staffing and unfair treatment may decrease burnout and other dimensions of distress among nurses, and improve their work experience and patient outcomes.
Burnout is a work-related syndrome characterized by emotional exhaustion, a sense of reduced personal accomplishment and depersonalization that may manifest as negativity, cynicism, and the inability to express empathy or grief.1,2 Burnout negatively affects nurses’ physical and mental health,3 and the care they provide.4 It increases nursing turnover rates, and is associated with poor job performance, threats to patient safety,5,6 reduced patient satisfaction and worse patient outcomes.5,7,8 It is more prevalent in hospitals with a higher number of patients per nurse.7,9,10
More than 20% of nurses are at risk for posttraumatic stress disorder as a result of workplace mistreatment, and nearly half of all nurses experience burnout in some form, a rate more than twice that among professionals in other fields.11 In addition to burnout, clinically relevant dimensions of distress include meaning in work, severe fatigue, work–life integration, quality of life, and suicidal ideation.12 The Institute for Healthcare Improvement has stated that “if burnout in healthcare were described in clinical or public health terms, it might well be called an epidemic.”13
The aim of this research was to measure the prevalence of burnout and distress among nurses practising in a cardiovascular centre at 2 quaternary referral hospitals within a single-payer public health care system environment. We also compared the prevalence of burnout and distress between these nurses and nurses in practice in the United States at academic health science centres (AHSCs), defined as academic and learning hospitals that deliver basic and clinical research, education to health professionals and clinical care to patients.14
Methods
Design, setting and recruitment
We conducted a survey at the Peter Munk Cardiac Centre (PMCC), Toronto General Hospital and Toronto Western Hospital, University Health Network, Toronto, Ontario, Canada. The survey was open to all PMCC nurses and was conducted between Nov. 27, 2018, and Jan. 31, 2019. Posters describing the survey were placed in multiple areas across the 2 locations (Appendix 1, available at www.cmajopen.ca/content/9/1/E19/suppl/DC1). An independent third party (Canadian Viewpoint, https://canview.com/) sent an initial email invitation (Appendix 2, available at www.cmajopen.ca/content/9/1/E19/suppl/DC1) and subsequent reminders to complete the survey to all nurses practising in the PMCC. Neither University Health Network nor the study authors had access to individual responses to the survey, which were collected by Corporate Web Services (www.cws.net/).
Survey development
Multiple surveys can be used to assess burnout, well-being and other work-related dimensions of distress, including the Maslach Burnout Inventory – Human Services Survey for Medical Personnel,1,2,15 the Oldenburg Burnout Inventory, the single-item measure used in the Physician Worklife Study, the Copenhagen Burnout Inventory, the Stanford Professional Fulfillment Index, the Well-Being Index (WBI)12,16 and the Patient Health Questionnaire-9 of the self-report component of the Primary Care Evaluation of Mental Disorders inventory. The validity and reliability of these survey instruments, including consideration of the format, source of data, development and testing, links to outcomes or health system characteristics related to health care professionals, past or validated applications, and cost, have been reported.17
After reviewing these validated survey instruments, we chose to use the WBI because it has a core of only 9 questions, takes minutes to complete, provides instantaneous and confidential feedback to survey participants, and has been independently validated for use in a diverse group of health care professionals, including physicians, nurses and nonphysician employees.12,16,18 Use of the WBI also enabled comparison of our results to a large group of nurses in the US, in whom a WBI score of 2 or higher identified those with high levels of overall distress.18 We considered a WBI score of 4 or higher to be consistent with severe distress among nurses.18 The WBI can also identify nurses who are doing well (high overall quality of life, high degree of meaning in work, satisfied with work–life balance) and those whose degree of distress increases the risk of adverse professional consequences.18
Seven of the 9 WBI items are questions that are answered “Yes” or “No,” with 1 point assigned for each “Yes” response.
Responses to the statement “The work I do is meaningful to me” were based on the Empowerment at Work Scale19 (7-point Likert scale where 1 = very strongly disagree and 7 = very strongly agree). Respondents who indicated 1 or 2 on the Likert scale had 1 point added to their score, and those who indicated 6 or 7 on the Likert scale had 1 point subtracted from their score.
Respondents indicated their level of agreement with the statement “My work schedule leaves me enough time for my personal/family life” on a 5-point Likert scale where 1 = strongly disagree and 5 = strongly agree. Respondents who indicated lower satisfaction with work–life integration (i.e., 1 or 2 on the Likert scale) had 1 point added to their score, and those who indicated higher satisfaction (i.e., 4 or 5 on the Likert scale) had 1 point subtracted from their score.
Accordingly, the total score for the WBI ranged from −2 to 9.
We also asked survey participants to supply demographic information and respond to 3 additional statements designed to assess work culture (“Please rate your satisfaction with your electronic health record,”20 “The staffing levels in this work setting are sufficient to handle the number of patients” and “I am treated fairly in the workplace”). Respondents indicated their level of agreement with the 3 statements on a 5-point Likert scale where 1 = strongly disagree and 5 = strongly agree. The full survey tool is presented in Appendix 3 (available at www.cmajopen.ca/content/9/1/E19/suppl/DC1).
Feedback
On completion of the survey, nurses received instantaneous feedback via email in the form of a dashboard from the survey administrator (Corporate Web Services) that quantified each dimension of distress. If a WBI score indicative of high distress (i.e., ≥ 218) was identified, the email response to individual study participants included the information required to access local, regional and provincial resources that provide assistance managing stress and resilience, fatigue, emotional concerns, suicidal thoughts, issues related to relationships and work–life balance, and alcohol or substance abuse.
Statistical analysis
Missing data were excluded from the analyses. We evaluated the relation between nurses’ responses to individual survey questions and their gender, years in practice, area of practice, satisfaction with the hospital’s electronic health record, perception of the adequacy of staffing levels and of being treated fairly in the workplace, work–life integration and meaning in work. We assessed demographic and environmental factors that predicted high WBI scores, and compared nurses’ responses to the survey to those of nurses in practice at AHSCs in the US.18 We also recorded the number of times respondents accessed contact information for local, regional or provincial resources after they received feedback.
We carried out standard univariate statistical comparisons using the χ2 test when expected counts were 5 or greater, the Fisher exact test when expected counts were less than 5, and the Kruskal–Wallis test for nonparametric continuous variables to perform univariate comparisons in the sample of respondents. We assessed the relation between selected demographic and work culture items and responses to elements of the survey both between and within groups. We also assessed the relation between a WBI score of 2 or higher and demographic characteristics, as well as responses to statements about work culture.
We used multivariable logistic regression to identify independent associations between demographic and workplace characteristics and a WBI score of 2 or higher, and calculated odds ratios (ORs) and 95% confidence intervals (CIs) for the association of each independent predictor of a WBI score of 2 or higher. We also carried out ordinal logistic regression (cumulative logit) analysis for WBI score categories that indicate low (−2 through 1), high (2 or 3) or severe (≥ 4) distress. Odds ratios reported are reflective of the odds of being in a lower category. Finally, we compared univariate associations among WBI data for nurses in practice at AHSCs in the US18 with responses from our respondents. We conducted all analyses using SAS version 9 (SAS Institute).
Ethics approval
The University Health Network Research Ethics Board provided a waiver for the requirement for research ethics approval for this study (waiver 18-0246).
Results
Of the 493 nurses who received a request to complete the survey, 242 (49.1%) responded. We report the respondents’ gender, years since graduation from nursing school, years working at University Health Network, primary practice location and employment status in Table 1.
Table 1:
Characteristics of nurses who responded to the Well-Being Index survey
| Characteristic | No. (%) of respondents n = 242 |
|---|---|
| Gender | |
| Male | 31 (12.8) |
| Female | 206 (85.1) |
| Gender diverse | 1 (0.4) |
| Missing | 4 (1.6) |
| Time since graduation from nursing school, yr | |
| < 2 | 14 (5.8) |
| 2–5 | 32 (13.2) |
| 6–10 | 39 (16.1) |
| 11–15 | 34 (14.0) |
| > 15 | 123 (50.8) |
| Time working at University Health Network, yr | |
| < 2 | 25 (10.3) |
| 2–5 | 47 (19.4) |
| 6–10 | 28 (11.6) |
| 11–15 | 49 (20.2) |
| > 15 | 93 (38.4) |
| Employment status | |
| Full-time, permanent | 197 (81.4) |
| Part-time, permanent | 36 (14.9) |
| Casual, temporary, other | 9 (3.7) |
| Work area | |
| Outpatient clinic | 13 (5.4) |
| Inpatient ward | 101 (41.7) |
| Critical care* | 100 (41.3) |
| Catheterization laboratory or interventional radiology | 19 (7.8) |
| Other | 9 (3.7) |
Coronary intensive care unit or cardiovascular intensive care unit.
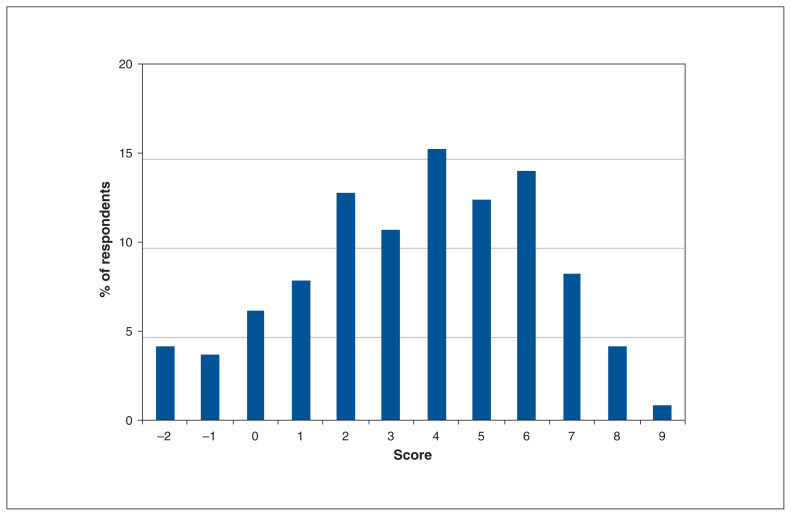
The mean WBI score was 3.6 (standard deviation [SD] 2.61). The distribution of WBI scores is shown in Figure 1.
Figure 1:
Distribution of Well-Being Index scores among 242 nurses in the Peter Munk Cardiac Centre.
Of the 242 respondents, 188 (77.7%) reported that, in the previous month, they felt burned out from their work, 191 (78.9%) indicated they had been bothered by emotional problems, and 179 (74.0%) reported that work was hardening them emotionally. Just over one-third (87 [36.0%]) agreed or strongly agreed that their work schedule left them enough time for their personal life, and 172 (71.1%) agreed or strongly agreed that the work they did was meaningful to them. Responses to the remaining survey questions appear in Appendix 4 (available at www.cmajopen.ca/content/9/1/E19/suppl/DC1).
Thirty-six (15.6%) of 230 respondents agreed or strongly agreed that staffing levels were adequate. Compared to those respondents, the 194 nurses (84.3%) who were neutral or somewhat or strongly disagreed that staffing levels were adequate were more likely to report feeling burned out from their work (159 [82.0%] v. 20 [55.6%], p < 0.001), to worry that work was hardening them emotionally (152 [78.4%] v. 19 [52.8%], p = 0.001), to feel down, depressed or hopeless (114 [58.8%] v. 13 [36.1%], p = 0.01), to feel that things were piling up so high they could not overcome them (98 [50.5%] v. 11 [30.6%], p = 0.03), to be bothered by emotional problems (159 [82.0%] v. 22 [61.1%], p = 0.005) and to disagree that their work schedule left them enough time for their personal life (96 [49.5%] v. 9 [25.0%], p = 0.001).
Just over half of respondents (118/230 [51.3%]) agreed or strongly agreed they were treated fairly in the workplace. Compared to those respondents, the 112 nurses (48.7%) who were neutral or somewhat or strongly disagreed that they were treated fairly in the workplace were more likely to report feeling burned out from their work (99 [88.4%] v. 80 [67.8%], p < 0.001), to worry that work was hardening them emotionally (94 [83.9%] v. 77 [65.2%], p = 0.001), to feel down, depressed or hopeless (74 [66.1%] v. 53 [44.9%], p = 0.001), to feel that things were piling up so high they could not overcome them (67 [59.8%] v. 42 [35.6%], p < 0.001) and to disagree that their work schedule left them enough time for their personal life (62 [55.4%] v. 43/118 [36.4%], p = 0.008).
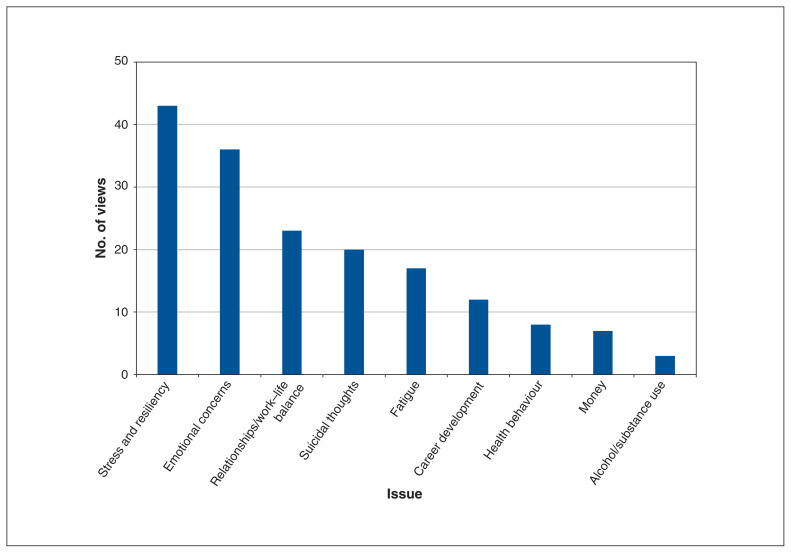
One hundred (43.5%) of 230 respondents agreed or strongly agreed that they were satisfied with the electronic health record. The 130 nurses (56.5%) who were neutral or disagreed or strongly disagreed that they were satisfied with the electronic health record were more likely than those respondents to report being bothered by emotional problems (111 [85.4%] v. 70 [70.0%], p = 0.005]. Overall, respondents who had graduated more recently from nursing school were more likely than those who had graduated in earlier years to report that they had fallen asleep while sitting inactive in a public place (p = 0.01). The number of times nurses accessed contact information for local, regional or provincial resources that help manage each element of distress is presented in Figure 2.
Figure 2:
Number of views of online resources by respondents, by issue.
Predictors of high Well-Being Index scores
Of the 242 respondents, 189 (78.1%) had a WBI score of 2 or higher, and 132 (54.5%) had a score of 4 or higher. Respondents were more likely to have a WBI score of 2 or higher if they were neutral or somewhat or strongly disagreed than if they agreed or strongly agreed that staffing levels were sufficient (161/194 [83.0%] v. 19/36 [52.8%], p < 0.001), if they were neutral or somewhat or strongly disagreed than if they agreed or strongly agreed that they were treated fairly in the workplace (97/112 [86.6%] v. 83/118 [70.3%], p < 0.001), and if they were neutral or somewhat or very unsatisfied than if they were satisfied or very satisfied with the electronic health record (109/130 [83.8%] v. 71/100 [71.0%], p < 0.003) (Table 2). We did not identify a relation between the proportion of respondents with a WBI score of 2 or higher and gender, years since graduation, years working at University Health Network, employment status or area of practice (Table 2).
Table 2:
Predictors of Well-Being Index score indicating high distress (≥ 2)
| Variable | No. (%*) of respondents | p value | |
|---|---|---|---|
| WBI score ≥ 2 n = 189 |
WBI score < 2 n = 53 |
||
| Gender | 0.9 | ||
| Male | 24 (77.4) | 7 (22.6) | |
| Female | 160 (77.7) | 46 (22.3) | |
| Gender diverse | 1 (100.0) | 0 (0.0) | |
| Missing | 4 (100.0) | 0 (0.0) | |
| Time since graduation from nursing school, yr | 0.4 | ||
| < 2 | 12 (85.7) | 2 (14.3) | |
| 2–5 | 28 (87.5) | 4 (12.5) | |
| 6–10 | 31 (79.5) | 8 (20.5) | |
| 11–15 | 28 (82.4) | 6 (17.6) | |
| > 15 | 90 (73.2) | 33 (26.8) | |
| Time working at University Health Network, yr | 0.8 | ||
| < 2 | 21 (84.0) | 4 (16.0) | |
| 2–5 | 35 (74.5) | 12 (25.5) | |
| 6–10 | 23 (82.1) | 5 (17.9) | |
| 11–15 | 39 (79.6) | 10 (20.4) | |
| > 15 | 71 (76.3) | 22 (23.7) | |
| Employment status | 0.7 | ||
| Full-time permanent | 154 (78.2) | 43 (21.8) | |
| Part-time permanent | 27 (75.0) | 9 (25.0) | |
| Casual, temporary, other | 8 (88.9) | 1 (11.1) | |
| Work area | 0.6 | ||
| Outpatient clinic | 9 (69.2) | 4 (30.8) | |
| Inpatient ward | 84 (83.2) | 17 (16.8) | |
| Critical care† | 75 (75.0) | 25 (25.0) | |
| Catheterization laboratory or interventional radiology | 14 (73.7) | 5 (26.3) | |
| Other | 7 (77.8) | 2 (22.2) | |
| Satisfaction with electronic health record | 0.003 | ||
| Very unsatisfied | 33 (94.3) | 2 (5.7) | |
| Somewhat unsatisfied | 41 (77.4) | 12 (22.6) | |
| Neutral | 35 (83.3) | 7 (16.7) | |
| Somewhat satisfied | 58 (77.3) | 17 (22.7) | |
| Very satisfied | 13 (52.0) | 12 (48.0) | |
| Missing | 9 (75.0) | 3 (25.0) | |
| Somewhat/very satisfied with electronic health record (v. neutral/unsatisfied) | 0.003 | ||
| Yes | 71 (71.0) | 29 (29.0) | |
| No | 109 (83.8) | 21 (16.2) | |
| Missing | 9 (75.0) | 3 (25.0) | |
| Staffing levels in work setting are sufficient | < 0.001 | ||
| Disagree strongly | 103 (90.4) | 11 (9.6) | |
| Disagree somewhat | 44 (69.8) | 19 (30.2) | |
| Neutral | 14 (82.4) | 3 (17.6) | |
| Agree somewhat | 16 (51.6) | 15 (48.4) | |
| Agree strongly | 3 (60.0) | 2 (40.0) | |
| Missing | 9 (75.0) | 3 (25.0) | |
| Somewhat/strongly agree staffing levels in work setting are sufficient (v. neutral/disagree) | < 0.001 | ||
| Yes | 19 (38.8) | 17 (61.2) | |
| No | 161 (83.0) | 33 (17.0) | |
| Missing | 9 (75.0) | 3 (25.0) | |
| Treated fairly in workplace | < 0.001 | ||
| Disagree strongly | 37 (90.2) | 4 (9.8) | |
| Disagree somewhat | 35 (92.1) | 3 (7.9) | |
| Neutral | 25 (75.8) | 8 (24.2) | |
| Agree somewhat | 66 (84.6) | 12 (15.4) | |
| Agree strongly | 17 (42.5) | 23 (57.5) | |
| Missing | 9 (75.0) | 3 (25.0) | |
| Somewhat/strongly agree treated fairly in workplace (v. neutral/disagree)† | |||
| Yes | 83 (70.3) | 35 (29.7) | |
| No | 97 (86.6) | 15 (13.4) | |
| Missing | 9 (75.0) | 3 (25.0) | |
Note: WBI = Well-Being Index.
Proportion of row total.
Coronary intensive care unit or cardiovascular intensive care unit.
Binary logistic multivariable analysis showed that respondents who graduated within the previous 15 years were 2.7-fold more likely than those who graduated in earlier years to have a WBI score of 2 or higher (OR 2.69, 95% CI 1.08–6.71) (Table 3). Respondents who thought staffing levels were adequate were less likely than those who did not to have a WBI score of 2 or higher (OR 0.27, 95% CI 0.12–0.64).
Table 3:
Multivariable model for factors associated with Well-Being Index score indicating high distress (≥ 2)
| Effect (reference) | OR (95% CI) |
|---|---|
| Male gender (v. female gender) | 1.17 (0.42–3.30) |
| ≤ 15 yr since graduation (v. ≥ 16 yr) | 2.69 (1.08–6.71) |
| ≤ 5 yr working at University Health Network (v. ≥ 6 yr) | 0.64 (0.24–1.66) |
| Not full-time, permanent (v. full-time, permanent) | 0.87 (0.35–2.18) |
| Work area | |
| Inpatient ward (v. all others) | 0.89 (0.31–2.54) |
| Critical care* (v. all others) | 0.50 (0.19–1.34) |
| Satisfied with electronic health record (v. not) | 0.63 (0.32–1.27) |
| Treated fairly in workplace (v. not) | 0.53 (0.25–1.13) |
| Staffing levels sufficient (v. not) | 0.27 (0.12–0.64) |
Note: CI = confidence interval, OR = odds ratio.
Coronary intensive care unit or cardiovascular intensive care unit.
Ordinal multivariable analysis also showed that satisfaction with staffing levels was associated with lower WBI scores (OR 0.33, 95% CI 0.16–0.69) (Table 4). In addition, there was a significant association between the perception of fair treatment and ranking in a lower WBI score category (OR 0.41, 95% CI 0.23–0.74). Ordinal multivariable analysis did not identify an association between time since graduation and lower WBI score category.
Table 4:
Ordinal multivariable analysis for factors associated with Well-Being Index score indicating low (≤ 2), high (2 or 3) or severe (≥ 4) distress
| Effect (reference) | OR (95% CI) |
|---|---|
| Female gender (v. male gender) | 1.00 (0.46–2.30) |
| ≤ 15 yr since graduation (v. ≥ 16 yr) | 1.40 (0.75–2.70) |
| ≤ 5 yr at University Health Network (v. ≥ 6 yr) | 1.40 (0.68–2.80) |
| Not full-time, permanent (v. full-time, permanent) | 1.30 (0.63–2.60) |
| Work area | |
| Inpatient ward (v. all others) | 0.80 (0.36–1.80) |
| Critical care* (v. all others) | 0.60 (0.28–1.30) |
| Satisfied with electronic health record (v. not) | 0.78 (0.45–1.30) |
| Staffing levels sufficient (v. not) | 0.33 (0.16–0.69) |
| Treated fairly in workplace (v. not) | 0.41 (0.23–0.74) |
Note: CI = confidence interval, OR = odds ratio.
Coronary intensive care unit or cardiovascular intensive care unit.
Comparison with nurses in the United States
Compared to 3627 nurses in practice at AHSCs in the US,18 our respondents had a higher mean WBI score (3.6 [SD 2.61] v. 2.1 [SD 2.58]), and were more likely to report being bothered by emotional problems (78.9% v. 64.1%), feeling burned out from work (77.7% v. 60.5%), being worried that work was hardening them emotionally (74.0% v. 46.6%), feeling down, depressed or hopeless (55.8% v. 41.3%), feeling that things were piling up so high they could not overcome them (47.5% v. 41.0%), feeling that their physical health interfered with their ability to do their daily work (44.6% v. 24.6%) and that they had fallen asleep while sitting inactive in a public place (38.4% v. 12.1%) (all p < 0.001) (Table 5). They were less likely to agree or strongly agree that their work schedule left them enough time for their personal life (mean rating on 5-point Likert scale 2.9 [SD 1.23] v. 3.3 [SD 1.16], p < 0.001). In addition, a greater proportion of our respondents than US nurses had a WBI score of 2 or higher (78.1% v. 57.0%) or 4 or higher (54.5% v. 32.0%) (both p < 0.001).
Table 5:
Comparison of Well-Being Index scores between nurses in practice at the Peter Munk Cardiac Centre and at academic health science centres in the United States16
| Item | No. (%) of respondents* | p value | |
|---|---|---|---|
| PMCC nurses n = 242 |
US nurses n = 3627 |
||
| Gender | 0.004§ | ||
| Male | 31 (12.8) | 281 (7.7) | |
| Female | 206 (85.1) | 3340 (92.1) | |
| Gender diverse | 1 (0.4) | 3 (0.1) | |
| Missing | 4 (1.6) | 3 (0.1) | |
| Have you felt burned out from your work? | < 0.001§ | ||
| Yes | 188 (77.7) | 2196 (60.5) | |
| No | 54 (22.3) | 1431 (39.4) | |
| Have you worried that work is hardening you emotionally? | < 0.001§ | ||
| Yes | 179 (74.0) | 1689 (46.6) | |
| No | 63 (26.0) | 1938 (53.4) | |
| Have you often felt bothered by feeling down, depressed, or hopeless? | < 0.001§ | ||
| Yes | 135 (55.8) | 1497 (41.3) | |
| No | 107 (44.2) | 2130 (58.7) | |
| Have you fallen asleep while sitting inactive in a public place? | < 0.001§ | ||
| Yes | 93 (38.4) | 438 (12.1) | |
| No | 149 (61.6) | 3189 (87.9) | |
| Have you felt that all things you had to do were piling up so high that you could not overcome them? | 0.047§ | ||
| Yes | 115 (47.5) | 1488 (41.0) | |
| No | 127 (52.5) | 2139 (59.0) | |
| Have you been bothered by emotional problems? | < 0.001§ | ||
| Yes | 191 (78.9) | 2326 (64.1) | |
| No | 51 (21.1) | 1301 (35.9) | |
| Has your physical health interfered with your ability to do your daily work at home and/or away from home? | < 0.001§ | ||
| Yes | 108 (44.6) | 894 (24.6) | |
| No | 134 (55.4) | 2733 (75.4) | |
| The work I do is meaningful to me† | 0.07¶ | ||
| Mean rating ± SD | 5.9 ± 1.14 | 5.7 ± 1.31 | |
| Median rating (range) | 6 (1.0 to 7.0) | 6 (1.0 to 7.0) | |
| The work I do is meaningful to me, rating | 0.1§ | ||
| 1–2 | 3 (1.2) | 115 (3.2) | |
| 3–5 | 67 (27.7) | 1130 (31.2) | |
| 6–7 | 172 (71.1) | 2382 (65.7) | |
| My work schedule leaves me enough time for my personal/family life‡ | < 0.001¶ | ||
| Mean rating ± SD | 2.9 ± 1.23 | 3.3 ± 1.16 | |
| Median rating (range) | 3 (1.0 to 5.0) | 3 (1.0 to 5.0) | |
| My work schedule leaves me enough time for my personal/family life, rating | < 0.001§ | ||
| 1–2 | 110 (45.4) | 1055 (29.1) | |
| 3 | 45 (18.6) | 908 (25.0) | |
| 4–5 | 87 (36.0) | 1664 (45.9) | |
| Well-Being Index score | < 0.001¶ | ||
| Mean ± SD | 3.6 ± 2.61 | 2.1 ± 2.58 | |
| Median (range) | 4 (−2.0 to 9.0) | 2 (−2.0 to 9.0) | |
| Well-Being Index score ≥ 2 | < 0.001¶ | ||
| Yes | 189 (78.1) | 2069 (57.0) | |
| No | 53 (21.9) | 1558 (43.0) | |
| Well-Being Index score ≥ 4 | < 0.001¶ | ||
| Yes | 132 (54.5) | 1160 (32.0) | |
| No | 110 (45.4) | 2467 (68.0) | |
Note: SD = standard deviation.
Except where noted otherwise.
Rated on a 7-point Likert scale where 1 = very strongly disagree and 7 = very strongly agree.
Rated on a 5-point Likert scale where 1 = strongly disagree and 5 = strongly agree.
χ2 test.
Kruskal–Wallis test.
Interpretation
In this survey, 78% of PMCC nurses had a WBI score of 2 or higher (high distress), and 54% had a score of 4 or higher (severe distress). The perception of adequate staffing levels and of being treated fairly in the workplace independently predicted low distress among PMCC nurses. Negative views of staffing levels and a perception of being treated unfairly in the nursing workplace were associated with an increased prevalence of burnout, feeling hardened emotionally, feeling down, depressed or hopeless, and believing that things were piling up so high that one could not overcome them.
A WBI score of 2 or higher identified respondents with high levels of overall distress because, among nurses in practice at AHSCs in the US,18 such scores were associated with a 4.4-fold higher likelihood of burnout, 2.4-fold higher likelihood of poor overall quality of life and intent to leave their current position (for reasons other than retirement) in the next 24 months, 2.3-fold higher likelihood of severe fatigue and twofold higher likelihood of reporting a recent patient care error. We interpreted a WBI score of 4 or higher as indicating severe distress because such scores were associated with an 8.1-fold higher likelihood of burnout, 4.6-fold higher likelihood of low quality of life and intent for nurses to leave their current position in the next 24 months, 3.6-fold higher likelihood of recent suicidal ideation, 3.5-fold higher likelihood of extreme fatigue and 2.7-fold higher likelihood of reporting a recent patient care error.18 The observation that the well-being of nurses is directly related to the safety and quality of care that nurses provide and the rate of hospital-acquired infections, as well as nurses’ career satisfaction and turnover,18,21–23 emphasizes the importance of these findings. The prevalence of distress scores above the threshold at which nurses are at risk for mental health issues and for providing suboptimal patient care underscores the need to direct effort and resources toward intervention strategies that have been shown to decrease burnout and distress among nurses.24,25 The level of burnout and distress identified in the present study can be used as a baseline to evaluate the efficacy of future interventions that are designed to decrease burnout and distress among nurses in the PMCC.
Although binary multivariable analysis identified graduation from nursing school within the previous 15 years as an independent predictor of high distress, ordinal multivariable analysis failed to identify a relation between time since graduation and lower WBI score category. Other studies have shown high levels of burnout and distress among nurses in the early phase of their career7,10,26 and that nurses are two-to threefold more likely to leave their job in their first 5 years of practice.27 The relation between years since graduation from nursing school and distress among nurses in the PMCC requires further study.
System-level policy factors may play a role in the development of nurse burnout and other dimensions of distress. Our interest in understanding the similarities, differences and drivers of distress among nurses between Canada and the US stems in part from the fact that the 2 countries have very different health care systems. We found that, compared to nurses in practice at AHSCs in the US,18 PMCC nurses reported a significantly higher prevalence of burnout and emotional problems and had higher overall WBI scores, and higher proportions had a WBI score indicative of high or severe distress.
The reasons for these unexpected results are not clear but may relate to differences between the Canadian and US health care systems. For example, nursing income is lower in Canada than in the US (US$55 260 v. US$70 610) (2018 data),28 and the percent occupancy of acute care beds is consistently higher in Canada than in the US (91% v. 64% in 2000, 92% v. 63% in 2015).29 Therefore, personal financial pressures and crowded hospital environments may have contributed to the observed differences in burnout and WBI scores between our respondents and US nurses.
Another possible explanation for the high WBI scores in the present study is that the work environment in the PMCC is more challenging than in other AHSCs in our region. However, this is not supported by annual nursing turnover data: a lower proportion of nurses voluntarily left their position in the PMCC (3.9%) than across all of University Health Network (which includes the Toronto General Hospital, the Toronto Western Hospital, Princess Margaret Hospital and the Toronto Rehabilitation Institute) (4.4%) or all 17 AHSCs in Ontario (6.5%) in fiscal year 2017/18 (Aimi Ly, Human Resources, University Health Network: personal communication, 2019). All of these nursing turnover rates appear lower than those in the rest of Canada (19.9%10) and the US (18.6% in hospitals with > 500 beds in 201827).
In addition to nurses, we also evaluated the prevalence of burnout and distress among physicians and allied health care staff in the PMCC. Similar to the results we observed for nurses, physicians reported a higher prevalence of burnout and a higher proportion of WBI scores indicative of high or severe distress than physicians in practice at AHSCs in the US who completed the WBI.30 Although allied health staff had higher average WBI scores, reported a higher prevalence of burnout and were more worried that work was hardening them emotionally than nonphysician employees in the US who completed the WBI, the proportions of PMCC allied health care staff and nonphysician employees in the US who had WBI scores consistent with high or severe distress were similar.31
Limitations
The relatively modest number of respondents may limit study validity and make type 2 statistical errors more likely, and the low response rate (49%) may have introduced response bias. The fact that this was a 2-institution study may limit the generalizability of our results. The supplemental survey questions related to perception of the adequacy of staffing levels and of fair treatment in the workplace, and satisfaction with the electronic health record were not subject to pilot evaluation in this study. Although we cannot exclude the possibility that nurses experiencing burnout may be less likely to complete a survey that could be viewed as additional work, most nurses (230/242) participating in the survey answered all survey questions. Comparison of the prevalence of burnout and high WBI scores between our respondents and nurses in practice at AHSCs in the US may have a gender bias, because the proportion of male respondents was relatively higher in the PMCC cohort than in the US cohort. Importantly, our respondents included only nurses practising in the area of cardiovascular medicine and surgery, which may limit the ability to directly compare the prevalence of burnout and distress between our respondents and US nurses, who practised across the full spectrum of specialties.
Conclusion
Although levels of burnout and distress were high among nurses in the PMCC, the perception of adequate staffing levels and of fair treatment in the workplace independently predicted lower levels of distress. Initiatives that focus on addressing inadequate staffing and unfair treatment may lower distress levels among PMCC nurses and improve their work experience and patient outcomes.
Supplementary Material
Acknowledgements
The authors thank Liselotte Dyrbye, Professor of Medical Education and Professor of Medicine, Division of Community Internal Medicine, Department of Internal Medicine, Mayo Clinic and Danielle Martin, Executive Vice President and Chief Medical Executive, Women’s College Hospital for very helpful discussions.
See related research articles at www.cmajopen.ca/lookup/doi/10.9778/cmajo.20200057 and www.cmajopen.ca/lookup/doi/10.9778/cmajo.20200059
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Barry Rubin, Rebecca Goldfarb and Leanna Graham designed the study. Barry Rubin drafted the manuscript. Daniel Satele carried out the statistical analysis. All of the authors contributed to the study conception, analyzed and interpreted the data, revised the manuscript critically for important intellectual content, approved the version to be published and agreed to be accountable for all aspects of the work.
Funding: This work was supported by a grant from the Peter Munk Cardiac Centre Innovation Fund.
Data sharing: All data presented in this manuscript are available to other investigators on request from the corresponding author.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/9/1/E19/suppl/DC1.
Disclaimer: The funding group had no role in the design, conduct or implementation of the study or manuscript, or the decision to submit, preparation of and editing of the manuscript.
References
- 1.Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. Palo Alto (CA): Consulting Psychologists Press; 1996. [Google Scholar]
- 2.Dzau VJ, Kirch DG, Nasca TJ. To care is human — collectively confronting the clinician-burnout crisis. N Engl J Med. 2018;378:312–4. doi: 10.1056/NEJMp1715127. [DOI] [PubMed] [Google Scholar]
- 3.Melnyk BM, Kelly SA, Stephens J, et al. Interventions to improve mental health, well-being, physical health, and lifestyle behaviors in physicians and nurses: a systematic review. Am J Health Promot. 2020 Nov;34:929–41. doi: 10.1177/0890117120920451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gunawan J, Aungsuroch Y, Fisher ML, et al. Factors related to the clinical competence of registered nurses: systematic review and meta-analysis. J Nurs Scholarsh. 2020;52:623–33. doi: 10.1111/jnu.12594. [DOI] [PubMed] [Google Scholar]
- 5.Hall LH, Johnson J, Watt I, et al. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS One. 2016;11:e0159015. doi: 10.1371/journal.pone.0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Welp A, Meier LL, Manser T. Emotional exhaustion and workload predict clinician-rated and objective patient safety. Front Psychol. 2015;5:1573. doi: 10.3389/fpsyg.2014.01573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bakhamis L, Paul DP, 3rd, Smith H, et al. Still an epidemic: the burnout syndrome in hospital registered nurses. Health Care Manag (Frederick) 2019;38:3–10. doi: 10.1097/HCM.0000000000000243. [DOI] [PubMed] [Google Scholar]
- 8.Dall’Ora C, Ball J, Reinius M, Griffiths P. Burnout in nursing: a theoretical review. Hum Resour Health. 2020 Jun 5;18:41. doi: 10.1186/s12960-020-00469-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Darban F, Balouchi A, Narouipour A, et al. Effect of communication skills training on the burnout of nurses: a cross-sectional study. J Clin Diagn Res. 2016;10:IC01–4. doi: 10.7860/JCDR/2016/19312.7667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Brien-Pallas L, Murphy GT, Shamian J, et al. Impact and determinants of nurse turnover: a pan-Canadian study. J Nurs Manag. 2010;18:1073–86. doi: 10.1111/j.1365-2834.2010.01167.x. [DOI] [PubMed] [Google Scholar]
- 11.Dyrbye LN, West CP, Johnson PO, et al. Burnout and satisfaction with work–life integration among nurses. J Occup Environ Med. 2019;61:689–98. doi: 10.1097/JOM.0000000000001637. [DOI] [PubMed] [Google Scholar]
- 12.Dyrbye LN, Satele D, Shanafelt T. Ability of a 9-item well-being index to identify distress and stratify quality of life in US workers. J Occup Environ Med. 2016;58:810–7. doi: 10.1097/JOM.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 13.Perlo J, Balik B, Swensen S, et al. IHI White Paper. Cambridge (MA): Institute for Healthcare Improvement; 2017. IHI framework for improving joy in work. [Google Scholar]
- 14.French CE, Ferlie E, Fulop NJ. The international spread of Academic Health Science Centres: a scoping review and the case of policy transfer to England. Health Policy. 2014;117:382–91. doi: 10.1016/j.healthpol.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 16.Dyrbye LN, Satele D, Sloan J, et al. Utility of a brief screening tool to identify physicians in distress. J Gen Intern Med. 2013;28:421–7. doi: 10.1007/s11606-012-2252-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Valid and reliable survey instruments to measure burnout, well-being, and other work-related dimensions. Washington (DC): National Academy of Medicine; [accessed 2019 Feb 7]. Available https://nam.edu/valid-reliable-survey-instruments-measure-burnout-well-work-related-dimensions. [Google Scholar]
- 18.Dyrbye LN, Johnson PO, Johnson LM, et al. Efficacy of the Well-Being Index to identify distress and well-being in U.S. nurses. Nurs Res. 2018;67:447–55. doi: 10.1097/NNR.0000000000000313. [DOI] [PubMed] [Google Scholar]
- 19.Spreitzer GM. Psychological empowerment in the workplace: dimensions, measurement, and validation. Acad Manage J. 1995;38:1442–65. [Google Scholar]
- 20.Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91:836–48. doi: 10.1016/j.mayocp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 21.Dyrbye LN, Shanafelt TD, Sinsky CA, et al. Burnout among health care professionals: a call to explore and address this underrecognized threat to safe, high-quality care [discussion paper] Washington: National Academy of Medicine; 2017. [Google Scholar]
- 22.McHugh MD, Kutney-Lee A, Cimiotti JP, et al. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Aff (Millwood) 2011;30:202–10. doi: 10.1377/hlthaff.2010.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cimiotti JP, Aiken LH, Sloane DM, et al. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012;40:486–90. doi: 10.1016/j.ajic.2012.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barrientos-Trigo S, Vega-Vazquez L, De Diego-Cordero R, et al. Interventions to improve working conditions of nursing staff in acute care hospitals: scoping review. J Nurs Manag. 2018;26:94–107. doi: 10.1111/jonm.12538. [DOI] [PubMed] [Google Scholar]
- 25.de Oliveira SM, de Alcantara Sousa LV, do Socorro Vieira Gadelha M, et al. Prevention actions of burnout syndrome in nurses: an integrating literature review. Clin Pract Epidemiol Ment Health. 2019;15:64–73. doi: 10.2174/1745017901915010064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spence Laschinger HK, Wong C, Read E, et al. Predictors of new graduate nurses’ health over the first 4 years of practice. Nurs Open. 2018;6:245–59. doi: 10.1002/nop2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.2019 national health care retention & RN staffing report. East Petersburg (PA): NSI Nursing Solutions; 2019. [Google Scholar]
- 28.Martin D, Miller AP, Quesnel-Vallée A, et al. Canada’s universal health-care system: achieving its potential. Lancet. 2018;391:1718–35. doi: 10.1016/S0140-6736(18)30181-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Health at a glance 2017: OECD indicators. Paris: Organisation for Economic Co-operation and Development; 2017. Occupancy rate of curative (acute) care beds, 2000 and 2015 (or nearest year) [Google Scholar]
- 30.Rubin B, Goldfarb R, Satale D, et al. Burnout and distress among physicians in a cardiovascular centre of a quaternary hospital network: a cross-sectional survey. CMAJ Open. 2021;9:10–8. doi: 10.9778/cmajo.20200057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rubin B, Goldfarb R, Satale D, et al. Burnout and distress among allied health care professionals in a cardiovascular centre of a quaternary hospital network: a cross-sectional survey. CMAJ Open. 2021;9:29–37. doi: 10.9778/cmajo.20200059. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.