Abstract
Backgroud
Prevalence of skin lesions among diabetic patients is a major health concern. Therefore, this systematic review and meta-analysis study was conducted to determine the prevalence of skin lesions in diabetic patients.
Methods
To identify and select relevant articles, the SID, MagIran, IranMedex, IranDoc, Google Scholar, Cochrane, Embase, ScienceDirect, Scopus, PubMed, and Web of Science (WoS) databases were searched without a lower time limit and until April 2020. The random effects model was used to perform the analysis, and the heterogeneity of studies was assessed using the I2 index. Data were analyzed within the Comprehensive Meta-Analysis (Version 2) software.
Results
After evaluating the 22 final articles with a total sample size of 8406, the prevalence of skin lesions among diabetes patients were found as 70.3% (95% CI: 63–76.7%). Moreover, according to the meta-regression analysis, the effect of ‘sample size’ on th prevalence of skin lesions was significantly different in diabetes patients (p < 0.05).
Conclusion
The results of this study show that skin lesions are common in diabetes patients. Therefore, appropriate policies needs to be adopted to improve the situation and to monitor patients and outcomes at all levels.
Keywords: Skin lesions, Prevalence, Diabetes, Meta-analysis
Introduction
Diabetes Mellitus (DM) is the most common endocrine disorder worldwide. This chronic disease is due to hereditary insulin deficiency or insufficient production of insulin [1]. Its prevalance is estimated to reach 4.4% by 2030 (i.e. circa 366 million). It is also predicted that by 2025, 300 million people will be affected globally [2]. Other literature has also projected that DM will result in about 592 million diabetic patients by 2035. The International Diabetes Federation estimates that more than 70% of people with type 2 diabetes will be in developing countries by 2030 [3].
Diabetes affects most organs of the body. The skin is a very active member of the metabolic and endocrine functions. Insulin affects different parts of the skin and is required for the growth and differentiation of creatine cells in the culture medium and regulates the entry of glucose into the skin cells [4].
Insulin irregularities and the increase in blood glucose levels lead to metabolic, vascular, neurological and immune abnormalities. Skin which is affected by metabolic damage and chronic degenerative complications of diabetes, changes in lipid profile and glycosylation of proteins, and their deposition lead to skin manifestations in patients with diabetes. Thus skin manifestations can be the first symptoms of diabetes [5].
skin manifestations of diabetes can be divided into four categories: “with strong to weak association with DM”, Junta (viral or foreign), skin manifestations of diabetes complications (microangiopathy, ma croangiopathy and neuropathy), and skin complications as a result of diabetic treatment [6].
DM manifestations may be different based on duration of disease and blood glucose level. Eventually, all patients with DM show skin changes due to the long-term effects of blood glucose levels on blood circulation and skin collagen. Moreover, anti-diabetic drugs can have side effects on the skin. Furthermore, diabetes-related skin lesions may be an entry factor for possible microorganisms and secondary infections [7].
Over one-third of diabetic patients have some form of skin manifestations over their chronic disease. It is estimated thata total of 70% of diabetic patients experience skin changes during the disease [8].
Due to the high prevalence of skin lesions among diabetic patients, and due to the lack of comrehensive general statistics on the topic, we decided to conduct a systemtatic review and perform meta-anlysis on the reported results of the existing high-quality studies that had conducted researchon the prevalence of skin lesions in patients with diabetes.
Methods
As highlighted earlier, this study is a systematic review and meta-analysis. To identify related articles, the national and international databases of SID, MagIran, IranMedex, IranDoc, Google Scholar, Cochrane, Embase, ScienceDirect, Scopus, PubMed, and Web of Science (WoS) were searched without a lower time limit and until April 2020. Moreover, to enhance the comprehensiveness of the search processes, the lists of references used within the identified articles were also reviewed to access further relevant studies.
Due to the insensitivity of the Persian databases to the AND, OR and NOT search operators, searches on these databases were performed only using the equivalent Persian keyword of epidemiology, prevalence, diabetes, skin, lesions. Searches in International databases was conducted using the Medical Subject Headings (MeSH) keywords that included prevalence, skin, cutaneous, manifestations, lesions, derm, diabetes and appropriate combinations of these search terms. All epidemiological studies that examined the prevalence of skin lesions among diabetic patients were reviewed, irrespective of their language. The inclusion criteria were as follows: Original research articles investigating the prevalence of skin lesions in diabetic patients. Exclusion criteria included: Non-random sample size, lack of subject relevance, inadequate data such as lack of reporting skin lesions, review articles, case reports, letters to the editor, and intervention studies.
Study selection
Following the search, all relevant articles were collected, and a list of abstracts was prepared. After anonymizing the articles by hiding journal titles and authors’ names, the full texts of the articles were provided to the reviewers. Each article was independently examined by two reviewers, and if an article was rejected, the reason for its rejection was mentioned. In case of a disagreement between the two reviewers, the article was then reviewed by a third reviewers. Considering the above process, as a result of the initial search, a total of 1800 articles related to the subject were identified. Two reviewers independently examined the articles’ title and abstract. If a title or an abstract was likely to be relevant to the fous of the study, the full text of the article was then reviewed. Finally, after reviewing the full text of several studies, 22 articles entered the quality evaluation phase.
Qualitative evaluation of studies
To assess the quality of the selected cross-sectional studies, the STROBE checklist was used. This checklist consists of 22 sections, of which 18 sections/items are general and applicable to all observational studies i.e. cohort, case-control, and cross-sectional studies. Articles that fulfilled 6 or 7 criteria were considered as high-quality articles. Articles satisfying more than 2, but less than 6, and articles fulfilling 2 criteria were respectively considered the medium and low-quality articles.
Data extraction
Data of from all the final studies were extracted using a different pre-prepared checklist. Items on the checklist included: article title, first author’s name, year of publication, study location, female sample size, male sample size, mean age, and skin lesions in diabetic patients.
Statistical analysis
Since the prevalence as a rate has a binomial distribution, prevalence variance was calculated using a binomial distribution variance formula and a weighted mean was used to amalgamate the reported prevalence rates in different studies. The I2 index test was used to evaluate the heterogeneity of the selected studies. Meta-regression analysis was also used to evaluate the prevalence of skin lesions in diabetic patients with the two variables of ‘year of study’ and ‘sample size.’ The Egger’s test at the significance level of 0.05 was used to investigate potential publication bias, and the corresponding Funnel plots were drawn.. Data were analyzed using the Comprehensive Meta-Analysis (Version 2) software.
Results
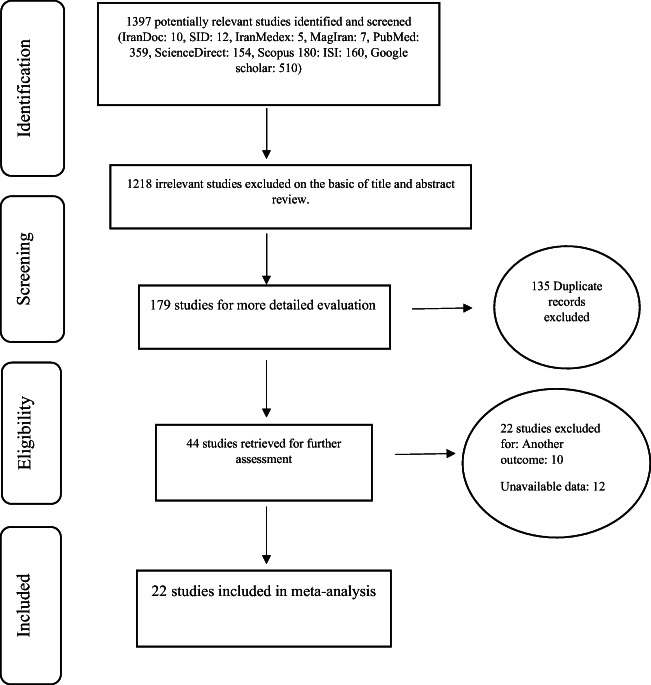
In this study, all studies with a focus on the prevalence of skin lesions in diabetic patients were systematically reviewed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. In the initial search, 1397 articles were identified. Subsequently, 1218 irrelevant articles, 135 duplicate articles, and 22 articles with a low quality or an inaccessible text were excluded. Finally, 22 studies were finally selected and included for the review and meta-analysis (Fig. 1, and Table 1). The specifications of the studies entered into the meta-analysis are provided in Table 1. Poential publication bias was evaluated using and the Egger’s test, and the corresponding funnel plot (Fig. 2), at significance level of 0.05. The result of the test indicated that there is no publication bias in the present study (p = 0.052).
Fig. 1.
PRISMA flow diagram for the study selection
Table 1.
Characteristic of the included studies
| Author,year, Reference | Age | City | Sample size | Prevalence % |
|---|---|---|---|---|
| Abas dorjani,2002 [9] | 15–66 | Rasht | 354 | 70.1 |
| Nighat Majeed,2004 [10] | – | Lahore | 200 | 58 |
| Sandeep Khuraiya,2019 [11] | 10–80 | India | 300 | 63 |
| Sivaram Avula,2014 [12] | 13–83 | India | 200 | 62 |
| Sameer kH,2011 [13] | 20–85 | Saudi Arabia | 558 | 96.1 |
| Deepika,2016 [14] | 7–90 | Ludhiana | 500 | 76.8 |
| Siddagangaiah Vathsala,2019 [15] | 10–88 | India | 500 | 82.8 |
| Kiran Fatima,2018 [16] | 28–80 | Islamabad | 100 | 64 |
| Florencia Galdeano,2009 [17] | 16–85 | Luis lagomaggiore | 125 | 90.4 |
| Saira Furqan,2014 [18] | 18–70 | Karachi, Pakistan | 100 | 84 |
| S. KIPRONO, E,2015 [19] | 2–90 | Moshi, Tanzania | 544 | 43.9 |
| SafaaSalih Alwaash,2017 [20] | 10–80 | IRAQ | 1002 | 37.8 |
| S Sasmaz,2004 [21] | 33–76 | Kahramanmaras Sutcu Imam | 151 | 85.4 |
| mahbobeh hossaeni,2007 [22] | 54 | Tehran | 1135 | 64 |
| Khurshid Ahmed,2009 [23] | 54 | Pakistan | 350 | 76.6 |
| Abhyudaya Verma,2019 [24] | 18–70 | India | 300 | 60.33 |
| AdepuSumitra Devi,2016 [25] | 35–75 | Warangal, Telangan | 100 | 64 |
| MashkoorAhmed Wani,2009 [26] | 18–83 | Srinagar | 200 | 68 |
| Nighat Majeed,2004 [27] | 32 | Lahore | 200 | 58 |
| Rocsana yaghmaei,2003 [28] | 14–79 | Sanandaj | 134 | 64.2 |
| Tariq Mahmood,2002 [29] | 2–75 | Sargodha | 162 | 81.5 |
| Mariaviagulam Vinnarasan2017 [30] | 40–70 | Thanjavur | 1200 | 40 |
Fig. 2.
Funnel plot results for the prevalence of skin lesions among diabetic patients
Considering the I2 rest results (I2 = 97.7), and due to the heterogeneity of the selected studies, the random-effects model was used to combine the reported results of the selected research works. The total sample size was equal to 8406 people aged between 7 to 90 years; the selected articles are listed in Table 1. The lowest and the highest prevalence rates of skin lesions in diabetes patients were related to the work of Safaa Salih Alwaash et al. 2017 in Iraq [20] with 37.8% (95% CI: 34.9–40.9%) and the study of Sameer et al. [13]. in 2011 in Saudi Arabia with 96.1% (95% CI: 94.1–97.4) respectively. Considering the meta-analysis results, the overall prevalence of skin lesions among diabetic patients is found to be70.3% (95% CI: 63–76.7%). Figure 3 represents this prevalence based on the random effect model; in this figure, the centre of each square denotes the reported prevalence for its corresponding study, and the width of the square shows the confidence interval of 95%. The diamond represents the overall prevalence of skin lesions among diabetes patients for the all studies combined. (Fig. 3).
Fig. 3.
Prevalence of skin lesions in diabetic patients based on the randomized model
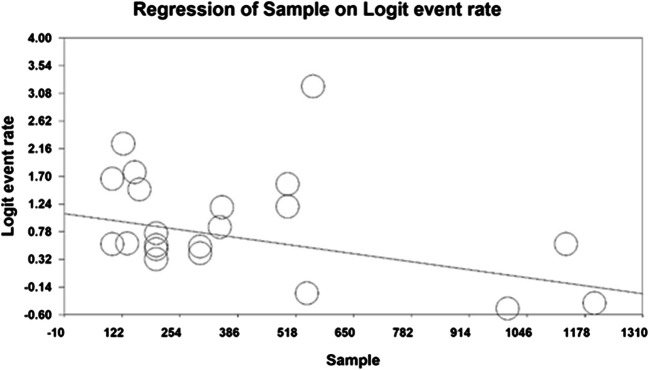
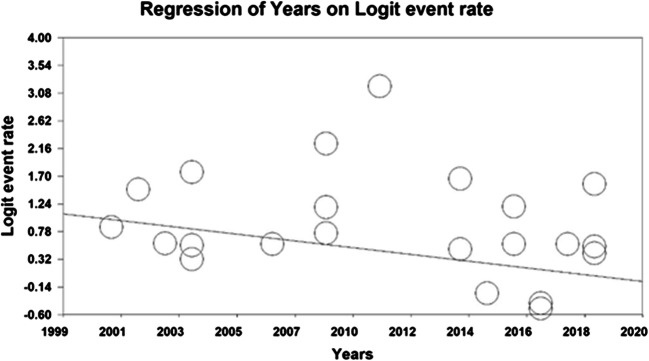
The associations between the two variables of ‘year of study’ and ‘sample size’ with the prevalence of skin lesions among diabetic patients were investigated using the meta-regression analysis. Accordingly, the prevalence of skin lesions in diabetic patients decreased by increasing ‘sample size’, and this was statistically significant(P < 0.05) (Fig. 4). Furthermore, the prevalence of skin lesions in diabetic patients decreased, by increasing ‘year of study’, and this was also statistically significant (P < 0.05) (Fig. 5).
Fig. 4.
Meta-regression association between sample size and prevalence of skin lesions among diabetic patients
Fig. 5.
Meta-regression of association between year of study and prevalence of skin lesions among diabetic patients
Discussion
Diabetes is a chronic clinical syndrome that is caused by an absolute or relative insulin deficiency. It is also known as hyperglycemia. The disease is classified into two types: type 1 or insulin-dependent diabetes mellitus (IDDM), and type 2 or insulin-dependent diabetes mellitus (NIDDM). Most skin disorders are associated with diabetes complications such as neuropathy, microangiopathy, immune dysfunction, insulin resistance, protein glycosylation, and abnormal lipid metabolism [31].
Diabetes is a modern epidemic that affects about 8.3% of the world’s population, and 46% of cases are still undiagnosed [32]. Skin manifestations have become more widespread with the increase of diabetes prevalence [33]. The overall incidence of skin disorders in DM varies from 51.1% to 97% in different regions of the world [34].
The present research work is the first systematic review and meta-analysis study on the prevalence of skin lesions among diabetic patients. This piece of research has been formulated using the most optimal secondary analysis methods on a total of 22 eligible primary studies. The selected articles used in this work were published between 2002 and 2019. The entire combined sample was 8406people aged 7 to 90 years old. According to our meta-analysis, the overall prevalence of skin lesions in diabetic patients is found to be 70.3% (95% confidence interval: 63–76.7%). In a different study which was conducted to examine the pattern of mild disease in diabetic patients, the athors’ reported that out of 500 cases of diabetes, 384 cases (equivalent to 76.8%) had skin lesions, 34.1% had fungal infections, 17.4% had bacterial infections, and 6% of casewere examined to have viral infections [6].
Comparison of the results of this study with other studies show that the prevalence found in our work is lower than that of Sameer et al. [13] in Jeddah (70.3% vs. 96.1%), yet is higher than the prevalence reported in the work of Vinnarasan et al. (2017) in Thanjavur (70.3% vs. 40%) [22].
Studies have shown that skin infections are commonly caused by cutaneous lesions or by fungal causes [10–12, 14, 16]. Uncontrolled diabetes leads to infections. Such infections are generally resistant to treatment [35]. Prevalence studies have shown that fungal infections are more common than bacterial infections [21]. Khuraiya et al. (2019) performed a study of skin lesions in 300 diabetic patients. They reported the prevalence of skin lesions as 62%, the prevalence of fungal infection 35.3%, prevalence of bacterial infection 20%, and and the incidence of viral infection was reported 7.33% [11]. The increased prevalence of infection among these patients can be due to peripheral vascular disease, diabetes neuropathy, abnormal circulation, hypohidrosis, and decreased phagocytosis [5].
Skin manifestations are associated with blood glucose level control [10]. In the study of Khuraiya et al. (2019) which was conducted on 300 diabetic patients, 63% of the patients had skin lesions. Among the diabetes patients, 86 patients (28.7%) had a good control of diabetes with HbA1c levels in the range of 6.6%–6.7%, while 132 patients (44%) had a poor control of their diabetes with HbA1c levels greater than 8. Cutaneous manifestations are more common in patients with a poor control over blood glucose level, which is in turn reflected by high levels of HbA1c. Uncontrolled diabetes increases the risk of microangiopathy and its associated complications, and makes the skin susceptible to various infections [11]. In the study of Majeed et al. (2004), HbA1c was used as a parameter to control blood glucose levels over a three month period. Patients with high HbA1c were found to have significant occurance of skin disorders [10]. Verma et al. (2019) reported that hyperglycemia plays an important role in the development of skin lesions since, 64.64% of patients had an HbA1 over 7 [24].
Diabetes foot lesion causes diabetic foot ulcer and gangrene. Also, 20% of diabetic patients are hospitalized only because of diabetes mellitus [36]. In the study of Majeed et al. (2004) diabetic foot ulcer was seen in 2 patients (1%), and 2 other patients (1%) had amputations of the toes [10]. In the study of Khuraiya et al. (2019), 9 patients had diabetes foot ulcers [11]. Mahajan et al. (2003), Rao and Pai (1997)and Al-Mutairi et al. (2006) reported diabetic foot ulcers in 2, 1, and 8 cases respectively [37–39].
The relative increase in the incidence of physiological changes in aging skin in patients also with diabetes may be attributed to a decrease in body resistance, as well as to the longer duration of diabetes in these patients. In the study of Khuraiya et al. (2019), men were more exposed to cutaneous manifestations than women [11]. Rao and Pai (1997), Goyal et al. (2010), and Chatterjee et al. (2014) reported that the prevalence of cutaneous manifestations is more among diabetic men [37, 40, 41]. However, in the study by Mahajan et al. (2003) and Nigam et al. (2003) the prevalence was found to be higher in women [38, 42]. In the research work of Avula et al. (2014), most cases were related to cutaneous manifestations in patients in their fifth and fourth decade of life (33% and 27%, respectively) [12]. Mahajan et al. (2003) reported that the most common age group with cutaneous lesions is 50–41 years with33% [38].
Prevalence of cutaneous lesions is common among diabetic patients and some skin infections are more prevalent than others. Therefore, skincare and continuous skin examination are very important measures in these patients. Moreover, it is necessary to remind and familiarize doctors and medical staff with the skin related symptoms of diabetes. It is vital to conduct comprehensive skin examinations at regular intervals, and to train and inform diabetes patients and their families with common cutaneous conditions, and in particular their infectious causes.
Conclusion
Skin diseases are an important aspect of diabetes. Cutaneous infection is the most common skin lesion, and skin manifestations are associated with blood glucose levels. Cutaneous manifestations are more common among patients with a poor control of blood glucose level. This is reflected by the high amount of HbA1c. Careful control of diabetes is essential to minimize the incidence of these complications. Proper skincare reduces the risk of skin lesions; Therefore, dermatologists can play an important role in reducing skin complications and improving the quality of life in these patients.
Acknowledgements
The authors would like to thank the faculty members of the Faculty of Nursing and Midwifery, Kermanshah University of Medical Sciences for their support with this research.
Authors’contributions
SHR and NS and SHR contributed to the design, MM and RJ statistical analysis, participated in most of the study steps. SHSH and AHF and AVR and SHR and MHF and HK prepared the manuscript. NS and MM and SHR assisted in designing the study, and contributed to the interpretation of the study. All authors have read and approved the content of the manuscript.
Abbreviations
- DM
Diabetes mellitus
- STROBE
Strengthening the Reporting of Observational Studies in Epidemiology for cross- sectional Study
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analysis.
Data availability
Datasets are available through the corresponding author upon reasonable request.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nader Salari, Email: n_s_514@yahoo.com.
Amin Hosseinian-Far, Email: amin.hosseinian-far@northampton.ac.uk.
Melika Hosseinian-Far, Email: mel.hosseinian@gmail.com.
Hossein Kavoussi, Email: hkawosi@kums.ac.
Rostam Jalali, Email: ks_jalali@yahoo.com.
Aliakbar Vaisi-Raygani, Email: visi_akbar@yahoo.com.
Shabnam Rasoulpoor, Email: Sh.rasoulpour@gmail.com.
Shna Rasoulpoor, Email: Shna.rasolpour@gmail.com.
Masoud Mohammadi, Email: masoud.mohammadi1989@yahoo.com.
Shervin Shabani, Email: Sherwin.shabani@gmail.com.
References
- 1.Mukherjee PK, Maiti K, Mukherjee K, Houghton PJ. Leads from Indian medicinal plants with hypoglycemic potentials. J Ethnopharmacol. 2006;106(1):1–28. doi: 10.1016/j.jep.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 2.Wild SH, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030: response to Rathman and Giani. Diabetes care. 2004;27(10):2569. doi: 10.2337/diacare.27.10.2569-a. [DOI] [PubMed] [Google Scholar]
- 3.Echouffo-Tcheugui JB, Dagogo-Jack S. Preventing diabetes mellitus in developing countries. Nat Rev Endocrinol. 2012;8(9):557–562. doi: 10.1038/nrendo.2012.46. [DOI] [PubMed] [Google Scholar]
- 4.Ferinkel R, Freinkel N. Cutaneous manifestations of endocrine diseases. u: Fitzpatrick TB i dr.[ur.]. Dermatology in general medicine, New York, itd: McGraw-Hill. 1993:2113–31.
- 5.Sibbald RG, Schachter RK. The skin and diabetes mellitus. Int J Dermatol. 1984;23(9):567–584. doi: 10.1111/j.1365-4362.1984.tb05694.x. [DOI] [PubMed] [Google Scholar]
- 6.Perez MI, Kohn SR. Cutaneous manifestations of diabetes mellitus. J Am Acad Dermatol. 1994;30(4):519–531. doi: 10.1016/S0190-9622(94)70058-3. [DOI] [PubMed] [Google Scholar]
- 7.Ragunatha S, Anitha B, Inamadar AC, Palit A, Devarmani SS. Cutaneous disorders in 500 diabetic patients attending diabetic clinic. Indian journal of dermatology. 2011;56(2):160–164. doi: 10.4103/0019-5154.80409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wohlrab J, Wohlrab D, Meiss F. Skin diseases in diabetes mellitus. Journal der Deutschen Dermatologischen Gesellschaft = Journal of the German Society of Dermatology : JDDG. 2007;5(1):37–53. doi: 10.1111/j.1610-0387.2007.06073.x. [DOI] [PubMed] [Google Scholar]
- 9.Darjani A. Attar khataie A, Farrokhian K, Sobhani A. Kalantari S Prevalence of Skin Lesions in Diabetic Patients jour guilan uni med sci. 2002;11(43):60–66. [Google Scholar]
- 10.Majeed M, Iqbal F, Mehboob A. Frequency and association of cutaneous manifestations of diabetes mellitus with HbA1c. Proc Shaikh Zayed Postgrad Med Inst. 2004;18:85–89. [Google Scholar]
- 11.Khuraiya S, Lal N, Naseerudin VJ, Kachhawa D. A cross sectional study of cutaneous manifestations in 300 patients of diabetes mellitus. International Journal of Advances in Medicine. 2019;6(1):150. doi: 10.18203/2349-3933.ijam20190122. [DOI] [Google Scholar]
- 12.Avula S, Masthansahib D, Latha MM. Cutaneous manifestations of diabetes mellitus: a cross-sectional study in a tertiary care hospital. Indian Journal of Mednodent and Allied Sciences. 2014;2(3):261–266. doi: 10.5958/2347-6206.2014.00025.9. [DOI] [Google Scholar]
- 13.Zimmo SK. Prevalence of skin manifestations in diabetes mellitus at King Abdulaziz University hospital. Saudi Journal of Internal Medicine. 2012;2(1):19–22. doi: 10.32790/sjim.2012.2.1.4. [DOI] [Google Scholar]
- 14.Gupta SK, Singh P. Pattern of dermatological diseases in patients of diabetes mellitus. Journal of Pakistan Association of Dermatology. 2017;26(3):214–218. [Google Scholar]
- 15.Vathsala S, Murthy SC, Shashibhushan J. Cutaneous manifestations in diabetes mellitus: a study among 500 patients in a tertiary care center in South India. IP Indian Journal of Clinical and Experimental Dermatology. 2019;5(2):141–145. doi: 10.18231/j.ijced.2019.031. [DOI] [Google Scholar]
- 16.Fatima K. Skin manifestations of diabetes mellitus. Journal of Rawalpindi Medical College. 2018:252–5.
- 17.Galdeano F, Zaccaria S, Parra V, Giannini ME, Salomón S. Cutaneous manifestations of diabetes mellitus: clinical meaning. Dermatología Argentina. 2013;16(2010):117–121. [Google Scholar]
- 18.Furqan S, Kamani L, Jabbar A. Skin manifestations in diabetes mellitus. Journal of Ayub Medical College Abbottabad. 2014;26(1):46–48. [PubMed] [Google Scholar]
- 19.Kiprono S, Minde E, Mavura D, Masenga J. Prevalence of cutaneous manifestations of diabetes mellitus: a hospital-based cross-sectional study in northern Tanzania. East Afr Med J. 2015;92(5):221–225. [Google Scholar]
- 20.Alwaash SS, Al-Shibly K. Dermatological manifestations of diabetes mellitus in Hilla City. Medical Journal of Babylon. 2017;14(3):495–500. [Google Scholar]
- 21.Sasmaz S, Buyukbese M, Cetinkaya A, Celik M, Arican O. The prevalence of skin disorders in type-2 diabetic patients. Int J Dermatol. 2005;3(1):1–4. [Google Scholar]
- 22.Hossaini MS, Ehsani AH, Hossainpanah F, Azizi F. Frequency of skin lesions among 1135 diabetic patients and their association with microvascular complications. Pejouhesh dar Pezeshki (Research in Medicine) 2006;30(3):193–199. [Google Scholar]
- 23.Ahmed K, Muhammad Z, Qayum I. Prevalence of cutaneous manifestations of diabetes mellitus. J Ayub Med Coll Abbottabad. 2009;21(2):76–79. [PubMed] [Google Scholar]
- 24.Verma A, Pandya P, Sharma D. Skin manifestations in patients with type-II diabetes mellitus. International Journal of Research and Review. 2019;6(9):59–65. [Google Scholar]
- 25.Devi AS, Lal BM. Skin manifestations in type 2 Dianetes mellitus. J Evid Based Med Healthc. 2016;3(61):3292–3294. doi: 10.18410/jebmh/2016/712. [DOI] [Google Scholar]
- 26.Ahmed Wani M, Hassan I, Hayat Bhat M, Masood AQ. Cutaneous manifestations of diabetes mellitus: a hospital based study in Kashmir. India Egyptian Dermatology Online Journal. 2009;5(2):1–6. [Google Scholar]
- 27.Majeed M, Iqbal F, Mehboob A. Cutaneous manifestations in type-1 and type-2 diabetes mellitus (a study profile of 200 patients) Proc Shaikh Zayed Postgrad Med Inst. 2004;18:63–68. [Google Scholar]
- 28.Yaghmaei R, Rahimi E. A study on frequency of skin complications in diabetec patiences referring to tohid hospital in Sanandaj (Iran) in 2000. Scientific Journal of Kurdistan University of Medical Sciences. 2004;9(1):43–47. [Google Scholar]
- 29.Mahmood T. Ul Bari a, agha H. cutaneous manifestations of diabetes mellitus. Journal of Pakistan Association of Dermatology. 2016;15(3):227–232. [Google Scholar]
- 30.Vinnarasan M, Sindhuja R, Vinothiney K, Balaji G. Cutaneous manifestations of diabetes mellitus. Journal of Evolution of Medical and Dental Sciences-JEMDS. 2017;6(83):5815–5819. doi: 10.14260/jemds/2017/1262. [DOI] [Google Scholar]
- 31.Kalus AA, Chien AJ, Olerud JE. Diabetes mellitus and other endocrine diseases. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ Fitzpatrick’s Dermatology in General Medicine 7th edn New York: McGraw Hill. 2008:1461–84.
- 32.Mendes AL, Miot HA, Haddad VJ. Diabetes mellitus and the skin. An Bras Dermatol. 2017;92(1):8–20. doi: 10.1590/abd1806-4841.20175514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Duff M, Demidova O, Blackburn S, Shubrook J. Cutaneous manifestations of diabetes mellitus. Clinical diabetes : a publication of the American Diabetes Association. 2015;33(1):40–48. doi: 10.2337/diaclin.33.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Macedo GM, Nunes S, Barreto T. Skin disorders in diabetes mellitus: an epidemiology and physiopathology review. Diabetology & metabolic syndrome. 2016;8(1):63–70. doi: 10.1186/s13098-016-0176-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Romano G, Moretti G, Di Benedetto A, Giofre C, Di Cesare E, Russo G, et al. Skin lesions in diabetes mellitus: prevalence and clinical correlations. Diabetes Res Clin Pract. 1998;39(2):101–106. doi: 10.1016/S0168-8227(97)00119-8. [DOI] [PubMed] [Google Scholar]
- 36.Vella J. Cutaneous markers of systemic disease in the lower extremity. Clin Podiatr Med Surg. 2016;33(3):423–440. doi: 10.1016/j.cpm.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 37.Rao GS, Pai GS. Cutaneous manifestations of diabetes mellitus. Indian journal of dermatology, venereology and leprology. 1997;63(4):232–234. [PubMed] [Google Scholar]
- 38.Mahajan S, Koranne R, Sharma S. Cutaneous manifestation of diabetes melitus. Indian Journal of Dermatology, Venereology, and Leprology. 2003;69(2):105. [PubMed] [Google Scholar]
- 39.Al-Mutairi N, Zaki A, Sharma AK, Al-Sheltawi M. Cutaneous manifestations of diabetes mellitus. Study from Farwaniya hospital, Kuwait. Medical principles and practice : international journal of the Kuwait University, Health Science Centre. 2006;15(6):427–430. doi: 10.1159/000095488. [DOI] [PubMed] [Google Scholar]
- 40.Goyal A, Raina S, Kaushal SS, Mahajan V, Sharma NL. Pattern of cutaneous manifestations in diabetes mellitus. Indian journal of dermatology. 2010;55(1):39–41. doi: 10.4103/0019-5154.60349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chatterjee N, Chattopadhyay C, Sengupta N, Das C, Sarma N, Pal SK. An observational study of cutaneous manifestations in diabetes mellitus in a tertiary care Hospital of Eastern India. Indian journal of endocrinology and metabolism. 2014;18(2):217–220. doi: 10.4103/2230-8210.129115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nigam P, Pande S. Pattern of dermatoses in diabetics. Indian Journal of Dermatology, Venereology, and Leprology. 2003;69(2):83. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Datasets are available through the corresponding author upon reasonable request.