Abstract
Introduction
Real-world evidence has demonstrated improved glycemic control and insulin management following introduction of smart insulin pens in a Swedish type 1 diabetes (T1D) population. To understand the implications for healthcare costs and expected health outcomes, this analysis evaluated the long-term cost-effectiveness of introducing smart insulin pens to standard-of-care T1D treatment (standard care) from a Swedish societal perspective.
Methods
Clinical outcomes and healthcare costs (in 2018 Swedish krona, SEK) were projected over patients’ lifetimes using the IQVIA CORE Diabetes Model to estimate cost-effectiveness. Clinical data and baseline characteristics for the simulated cohort were informed by population data and a prospective, noninterventional study of a smart insulin pen in a Swedish T1D population. This analysis captured direct and indirect costs, mortality, and the impact of diabetes-related complications on quality of life.
Results
Over patients’ lifetimes, smart insulin pen use was associated with per-patient improvements in mean discounted life expectancy (+ 0.90 years) and quality-adjusted life expectancy (+ 1.15 quality-adjusted life-years), in addition to mean cost savings (direct, SEK 124,270; indirect, SEK 373,725), versus standard care. A lower frequency and delayed onset of complications drove projected improvements in quality-adjusted life expectancy and lower costs with smart insulin pens versus standard care. Overall, smart insulin pens were a dominant treatment option relative to standard care across all base-case and sensitivity analyses.
Conclusions
Use of smart insulin pens was projected to improve clinical outcomes at lower costs relative to standard care in a Swedish T1D population and represents a good use of healthcare resources in Sweden.
Supplementary Information
The online version contains supplementary material available at 10.1007/s13300-020-00980-1.
Keywords: Diabetes complications, Diabetes self-management, Diabetes technology, Digital health, eHealth, Health technology assessment, Healthcare economics, Hypoglycemia, Insulin therapy, Type 1 diabetes
Key Summary Points
| Why carry out this study? |
| Digital health solutions are becoming increasingly established for chronic disease management, particularly in the treatment of diabetes; however, there is a need for evidence to support healthcare payers in making value-based decisions on the new digital technologies |
| Smart insulin pens record the timing and dose of insulin injections, while their data can be integrated with continuous glucose monitoring to improve diabetes self-management and address an unmet need for patients to become more actively engaged with their diabetes care |
| The aim of the present modeling analysis—which was informed by clinical data from a Swedish prospective, noninterventional study—was to evaluate the long-term cost-effectiveness of introducing smart insulin pens to standard-of-care treatment for type 1 diabetes (standard care) from a Swedish societal perspective |
| What was learned from the study? |
| Projections showed that smart insulin pens were associated with lower healthcare costs and improved health outcomes (i.e., a dominant treatment option) versus standard care in the base-case analysis and across all of the sensitivity analyses conducted |
| Our findings suggest that smart insulin pens are likely to be a good use of healthcare resources in Sweden in this patient population with type 1 diabetes, and they add to a growing body of evidence that digital technologies can add value to the treatment of chronic diseases |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13296119.
Introduction
Diabetes, including type 1 diabetes (T1D), is associated with the development of microvascular and macrovascular complications [1, 2], which have significant negative effects on quality of life [3, 4], and morbidity and mortality [5], with substantial costs to healthcare systems across patients’ lifetimes [6]. The incidence of T1D is increasing worldwide [2]; new cases of T1D in Europe are rising at a rate of 3.4% annually, with projections showing that, if the current trend continues, incidence will double in the next 20 years [7]. In Sweden, the incidence of pediatric-onset T1D has doubled in the last 40 years to 43.9 per 100,000—the second highest incidence rate in the world [2, 8].
The development and implementation of new digital solutions are key to supporting the management of chronic diseases [9]. They offer potential innovative solutions to reduce the burden of chronic disease on patients and healthcare providers, address the lack of data to inform therapeutic decision-making, improve clinical outcomes, and reduce healthcare needs [10]. However, the cost of these digital solutions can be a barrier to their implementation [11], and healthcare payers need evidence to make value-based decisions on digital tools. Economic analyses are increasingly being used to support healthcare decision-making [12]. One such method is cost-effectiveness analysis, which provides evidence on health gains and resource implications of a certain intervention by comparing the costs of interventions with expected outcomes (most commonly measured in quality-adjusted life-years, QALYs) [13].
For people with diabetes, there are a growing number of digital technologies available that enable optimized monitoring of lifestyle and pharmaceutical interventions, and also capture accurate data that can aid healthcare professionals in decision-making [14]. Smart insulin pens are one such digital tool, able to record the timing and dose of insulin delivered, and they can be combined with intermittently scanned or real-time continuous glucose monitoring (CGM) data, for example. From a patient perspective, smart insulin pens have the added benefit over standard insulin pens of capturing data on insulin delivery. When smart insulin pens were introduced to a cohort of people with T1D already using CGM in Sweden, they resulted in improved glycemic control (greater time in range, TIR), reduced time in hypoglycemia, and fewer missed bolus insulin doses [15, 16]. As a result of these factors, smart insulin pen use led to a significant increase in the amount of bolus insulin being administered each day, with no change to basal insulin dosing [15].
In combination, smart insulin pens and CGM may lead to improved diabetes self-management, and address an unmet need for patients to become more actively engaged with their diabetes care in this population of people with T1D [15]. However, it is important to understand the implications for healthcare costs and expected health outcomes based on improvements in glycemic control, but also increased bolus insulin doses. The cost-effectiveness of this digital tool should therefore be investigated and, as such, the aim of the present analysis, informed by Swedish real-world evidence, was to evaluate the long-term cost-effectiveness of introducing smart insulin pens to standard-of-care treatment of T1D (standard care) from a societal perspective in Sweden.
Methods
Swedish Prospective, Noninterventional Study Design
The design and results of the Swedish noninterventional study have been published previously [15]. In brief, a one-arm, prospective, observational, proof-of-concept study evaluated the introduction of a near-field communication (NFC)-enabled smart insulin pen (NovoPen® 6; Novo Nordisk A/S, Bagsværd, Denmark) in 94 adults with T1D receiving basal–bolus insulin therapy and using CGM, from 12 diabetes clinics in Sweden [15]. Participants were included in the study at the discretion of their healthcare team and received a smart insulin pen for basal and/or bolus insulin injections. Downloadable long-term injection data were blinded to participants during the baseline period (baseline until visit 1), but CGM data could be viewed, and the dose of the last injection was displayed on the smart insulin pen [15]. At visit 1, the first set of injection data was downloaded at the participant’s diabetes clinic, and subsequent follow-up visits were scheduled according to standard clinical practice. Smart insulin pen and CGM data were downloaded at each visit (CGM data were also uploaded between visits), and discussed and acted upon by the participant and healthcare team [15].
Glycemic summary measures and the number of missed bolus dose injections were compared between the blinded baseline period and the follow-up period [15]. The follow-up period was defined as any point after the fifth visit, to allow for adequate discussion of available smart insulin pen data with the healthcare team [15]. All 94 participants were included in the TIR analysis, while the 81 participants who were using the smart insulin pen for bolus insulin dosing were included in the bolus dose analyses and missed bolus dose analysis [15]. TIR was defined as the time spent with sensor glucose within the acceptable range (3.9–10.0 mmol/L [70–180 mg/dL]) [17]. Time spent in hypoglycemia (divided into level 1, 3.0 to < 3.9 mmol/L [54 to < 70 mg/dL]) and level 2, < 3.0 mmol/L [< 54 mg/dL]) [17], total daily insulin dose, mean glucose level, and the coefficient of variation were additional outcomes [15].
Cost-Effectiveness Model Overview
A cost-effectiveness analysis was performed by projecting costs (2018 Swedish krona, SEK) and clinical outcomes over patients’ lifetimes following the introduction of a smart insulin pen in a Swedish T1D population. This approach aims to capture the development of diabetes-related complications and their impact on projected costs, life expectancy, and quality of life, in alignment with guidelines on the assessment of the cost-effectiveness of diabetes interventions [18]. The analysis was performed using the IQVIA CORE Diabetes Model (IQVIA, Durham, NC), a validated computer-simulation model of diabetes [19]. The model projected the development of diabetes-related complications, mortality, hypoglycemia over a 60-year time horizon (i.e., patients’ remaining lifetimes) based on risk factors such as glycated hemoglobin (HbA1c), blood pressure, lipids, and body mass index. First-order stochastic uncertainty was captured via a Monte Carlo approach. Modeled outcomes included direct medical costs, indirect costs, life expectancy, quality-adjusted life expectancy, and the cumulative incidence and time to onset of diabetes-related complications in each simulation arm. It was assumed that patients continued to receive their set intervention (smart insulin pen in addition to standard care versus standard care) for the duration of their lifetime. Future costs and clinical outcomes were discounted at a rate of 3% per annum, in alignment with guidelines for economic evaluations in Sweden [20]. This article does not contain any new studies with human participants or animals performed by any of the authors.
Clinical Data
Model inputs for clinical outcomes were informed by the Swedish prospective, noninterventional study [15]. In the study, smart insulin pens were associated with an additional 1.89 h per day TIR compared with the baseline measurement (without a smart insulin pen; 9.19 h, over a median follow-up of 7 months), and daily bolus insulin dose increased from 25.1 units [U] to 32.1 U from baseline to visit 5 [15]. There are currently no published risk equations allowing TIR to be directly linked to incidence of diabetes-related complications and, therefore, a conversion from TIR to HbA1c was made, based on a previously identified linear relationship between the two parameters [21]. A 10% change in TIR was considered equivalent to a change in HbA1c of 0.8% (9 mmol/mol) [21]. TIR as a percentage (baseline, 41.4%; end of trial, 49.9%; change in TIR, + 8.5%) was converted to HbA1c using the following regression equation (HbA1c = [TIR − 155.4]/− 12.762) [21]. This conversion allowed long-term outcomes to be modeled on the basis of published risk equations that use HbA1c as a risk factor for developing complications. These calculated HbA1c values at baseline (8.93%) and end of trial (8.27%) resulted in a HbA1c treatment effect of − 0.67% (− 7 mmol/mol), which was applied in the smart insulin pens arm, with no HbA1c treatment effect applied in the standard care arm. The HbA1c treatment effect was assumed to be constant in both arms of the analysis, with the difference maintained for the duration of the analysis. Hypoglycemic event rates were based on the study period of the Swedish prospective, noninterventional study for the smart insulin pens arm, and the baseline value for the standard care arm (3287.25 and 6574.50 events per 100 patient-years, respectively). For modeling purposes, hypoglycemia was defined as at least 15 min of below 54 mg/dL (< 3.0 mmol/L) in CGM data [22], and all hypoglycemic events were categorized as nonsevere. Mortality as a result of diabetes-related complications and background mortality based on Sweden-specific life tables [23] were applied.
Simulated Cohort
All baseline characteristics were taken from people with T1D enrolled in the Swedish National Diabetes Register [24], other than baseline HbA1c (calculated from baseline TIR from the Swedish prospective, noninterventional study) [15], number of cigarettes smoked per day, and mean weekly alcohol consumption (both assumed to be the same as the Swedish general population) [25, 26] (Table 1). The model simulated the lifetime progression of diabetes in a cohort of 1000 hypothetical patients and repeated the process 1000 times for each simulation arm. This simulation generated mean and standard deviation values of clinical effectiveness and costs.
Table 1.
Simulated cohorts
| Characteristic | Parameter | Unit | Source |
|---|---|---|---|
| Age | 41.6 | Years | SWE-NDR [24] |
| Duration of diabetes | 26.1 | Years | SWE-NDR [24] |
| Male | 0.545 | Proportion | SWE-NDR [24] |
| HbA1ca | |||
| Smart pens arm | 8.27/66.9 | Percentage/mmol/mol | Adolfsson et al. 2020 [15] |
| Standard care arm | 8.93/74.1 | Percentage/mmol/mol | Adolfsson et al. 2020 [15] |
| NSHE | |||
| Smart pens arm | 3287.25 | Events per 100 patient-years of observation | |
| Standard care arm | 6574.50 | ||
| Blood pressure | |||
| Systolic | 128.7 | mmHg | SWE-NDR [24] |
| Diastolic | 73.6 | mmHg | SWE-NDR [24] |
| Cholesterol | |||
| Total | 146.2 | mg/dL | SWE-NDR [24] |
| HDL | 62.6 | mg/dL | SWE-NDR [24] |
| LDL | 103.2 | mg/dL | SWE-NDR [24] |
| Triglycerides | 95.6 | mg/dL | SWE-NDR [24] |
| BMI | 25.3 | kg/m2 | SWE-NDR [24] |
| Smokers | 0.122 | Proportion | SWE-NDR [24] |
| Cigarettesb | 14 | Number per day | Population data [25] |
| Alcohol consumption | 5.98/177 | Fluid ounces per week/mL per week | Population data [26] |
| Ethnicity | |||
| Whitec | 1.000 | Proportion | Assumed |
Data are mean, unless otherwise stated
BMI body mass index, HbA1c glycated hemoglobin, HDL high-density lipoprotein, LDL low-density lipoprotein, NSHE nonsevere hypoglycemic events, SWE-NDR Swedish National Diabetes Register
aHbA1c data were derived from time in range and converted using a published regression equation [21]; the HbA1c value for the smart pens arm was calculated as 8.933–0.666 [derived treatment effect from the regression equation] = 8.267%, with all figures rounded to 2 decimal places
bOnly applies to the smokers
cThese data were not collected in the prospective, noninterventional Swedish study, so were assumed to be 100% white for simplicity in this analysis
Quality-of-Life Utilities
Quality-adjusted life expectancy was assessed using the CORE Default Method, which involves taking the lowest state utility associated with existing complications and adding event utilities for any events that occur in that year (Supplementary Table S1), to create annual utility scores for each simulated patient. Utilities associated with diabetes and disease-related complications were extracted from published sources (Supplementary Table S1).
Costs
Costs were estimated from a Swedish societal perspective to capture all direct medical costs (pharmacy costs, costs associated with diabetes-related complications, and concomitant patient management costs) and indirect costs as a result of lost productivity. Insulin doses applied in this model were based on the baseline values of patients enrolled in the Swedish prospective, noninterventional study for the standard care arm, and based on end-of-trial data for the smart insulin pens arm (daily bolus dose increased from 25.1 U at baseline to 32.1 U at visit 5) [15]. Resource use and costs relating to insulin delivery were based on prices in Sweden, and are shown in Supplementary Table S2. Smart insulin pens and conventional durable insulin pens (without smart technology) have the same cost in Sweden (SEK 536.05) [27]; these costs were excluded from the analysis for simplicity owing to the relatively low costs and the durability (up to 5 years) of the insulin pens (Supplementary Table S2). Resource use relating to patient management was assumed to be the same as the general population of people with T1D in Sweden and is detailed along with patient management costs in Supplementary Table S3.
The cost of diabetes-related complications in the year of the event and for annual follow-ups (applied in each year of the simulation subsequent to the event) were identified through a literature review, and costs were inflated to 2018 values (Supplementary Table S4). Indirect costs of diabetes-related complications were considered in both arms of the analysis. Working age was considered to be from 20 to 65 years of age, with an average annual salary of SEK 438,000 for men and SEK 391,200 for women [28], and the working year considered to be 250 days. Days off work estimates were taken from an analysis of Danish registry data [29] or a study on the annual cost of hypoglycemia in Sweden [30], or a conservative assumption was used when no estimates could be identified (Supplementary Table S5). Cost results are presented in SEK, with a conversion to euros (EUR) in the Supplementary Appendix using a SEK 0.091 exchange rate, correct as of 27 March 2020.
Sensitivity Analyses
As the extrapolation of clinical results by modeling long-term outcomes is associated with a level of uncertainty, sensitivity analyses were performed to assess the robustness of the findings and identify key drivers of modeled outcomes. Sensitivity analyses were performed by varying model parameters. The influence of time horizon on the outcomes projected by the model was investigated by running analyses over 3, 5, and 10 years. The base-case analysis used the baseline HbA1c from the Swedish prospective, noninterventional study, and sensitivity analyses were performed with variation in this input parameter. The calculated change in HbA1c (with the smart insulin pen relative to standard care) was varied to investigate uncertainty around the impact of smart insulin pens on glycemic control and the relationship between TIR and HbA1c. Further sensitivity analyses were conducted removing treatment effects in terms of HbA1c and hypoglycemic event rates, and with treatment switching from standard care to the smart insulin pen.
Results
Base-Case Analysis
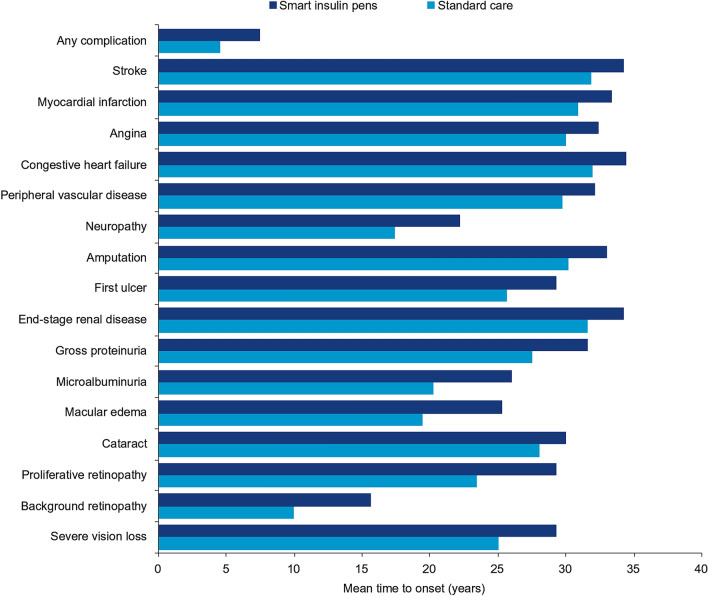
Projections showed that smart insulin pens were associated with improvements in mean discounted life expectancy of 0.90 years per patient and mean discounted quality-adjusted life expectancy of 1.15 QALYs per patient, compared with standard care (Table 2). Clinical benefits resulted from a reduced incidence of all diabetes-related complications, with a single exception (cataract) in the smart insulin pens arm compared with standard care over the 60-year time horizon of the analysis (Table 2). Treatment with smart insulin pens was also associated with a delayed mean time to onset of any diabetes-related complication (+ 2.9 years) versus standard care (Fig. 1).
Table 2.
Results of the base-case analysis
| Smart insulin pen | Standard care | Difference | |
|---|---|---|---|
| Outcomes, mean (SD) | |||
| Discounted direct costs (SEK) | 635,599 (19,290) | 759,869 (21,883) | − 124,270 |
| Discounted combined costs (SEK) | 1,541,648 (55,546) | 2,039,643 (61,753) | − 497,995 |
| Discounted life expectancy (years) | 20.20 (0.19) | 19.31 (0.20) | + 0.90 |
| Discounted quality-adjusted life expectancy (QALYs) | 14.74 (0.14) | 13.59 (0.14) | + 1.15 |
| Cumulative incidence of complications, % | |||
| Cardiovascular disease | |||
| Myocardial infarction | 15.04 | 16.20 | − 1.16 |
| Angina | 12.22 | 13.09 | − 0.87 |
| Stroke | 3.22 | 3.41 | − 0.19 |
| Congestive heart failure | 3.83 | 4.07 | − 0.24 |
| Peripheral vascular disease | 16.45 | 16.79 | − 0.34 |
| Renal disease | |||
| Microalbuminuria | 41.91 | 58.50 | − 16.59 |
| Gross proteinuria | 21.71 | 33.28 | − 11.57 |
| End-stage renal disease | 8.30 | 12.74 | − 4.44 |
| Death following end-stage renal disease | 6.12 | 9.67 | − 3.55 |
| Eye disease | |||
| Background diabetic retinopathy | 76.61 | 88.25 | − 11.64 |
| Proliferative diabetic retinopathy | 22.26 | 38.95 | − 16.69 |
| Macular edema | 42.79 | 58.87 | − 16.08 |
| Severe vision loss | 32.27 | 42.80 | − 10.53 |
| Cataract | 21.81 | 20.64 | + 1.17 |
| Neuropathic complications | |||
| Neuropathy | 63.51 | 75.26 | − 11.75 |
| Diabetic foot complications | |||
| Foot ulcer | 47.23 | 57.48 | − 10.25 |
| Amputation | 17.70 | 21.78 | − 4.08 |
QALY quality-adjusted life-year, SEK 2018 Swedish krona
Fig. 1.
Projected mean time to onset of complications. Base-case analysis, treatment effects were maintained for patient lifetimes
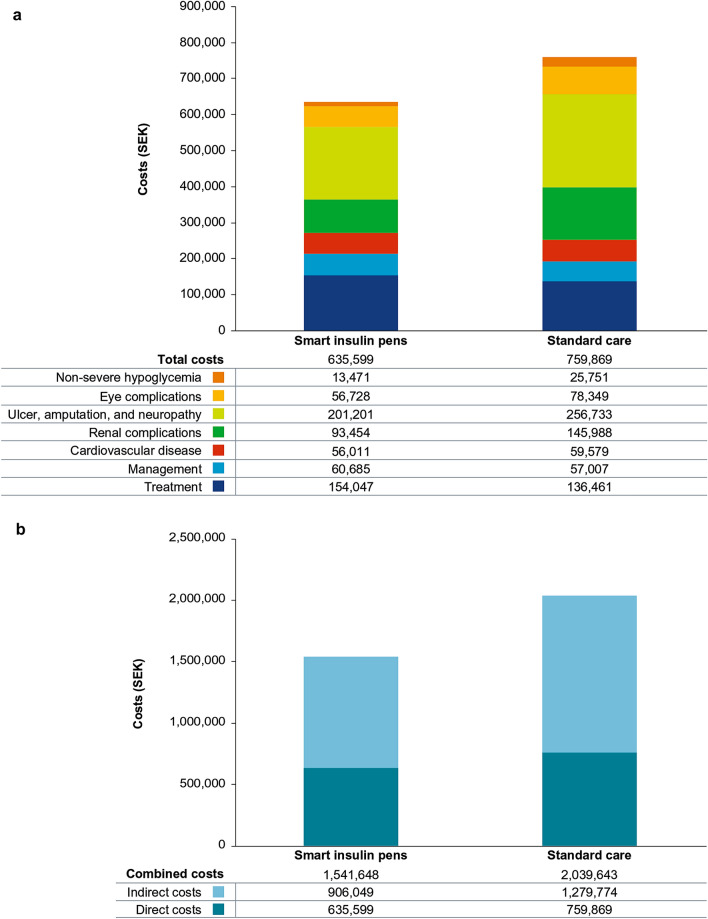
For direct medical costs, projections indicated that the mean cost per patient was SEK 124,270 (EUR 11,309) lower in the smart insulin pens arm compared with standard care, over a patient’s lifetime (Fig. 2a; Supplementary Table S6). Higher treatment costs in the smart insulin pens arm (SEK 154,047 [EUR 14,018]) compared with the standard care arm (SEK 136,461 [EUR 12,418]) (Fig. 2a; Supplementary Table S7) were a result of a higher bolus insulin dose and increased survival, which led to further treatment over the long term. However, this higher treatment cost in the smart insulin pens arm was offset by cost savings arising from the reduced incidence of diabetes-related complications (Fig. 2a). For indirect costs, a mean saving of SEK 373,725 (EUR 34,009) per patient was projected for the smart insulin pens arm versus the standard care arm (SEK 906,049 [EUR 82,450] versus SEK 1,279,774 [EUR 116,459]) (Fig. 2b; Supplementary Table S7). When direct and indirect costs were combined, cost savings of SEK 497,995 [EUR 45,318] per patient with smart insulin pens were projected versus standard care (smart insulin pens, SEK 1,541,648 [EUR 140,290]; standard care, SEK 2,039,643 [EUR 185,607]) (Fig. 2b; Supplementary Table S7).
Fig. 2.
Mean a direct costs and b combined (direct and indirect) costs over patients’ lifetimes. Base-case analysis, treatment effects were maintained for patient lifetimes. SEK, 2018 Swedish krona
Estimation of long-term cost-effectiveness outcomes indicated that both life expectancy and quality-adjusted life expectancy were improved with smart insulin pens compared with standard care, at a decreased cost from a healthcare payer and a societal perspective. Therefore, treatment with smart insulin pens was considered dominant over standard care from both a healthcare payer and a societal perspective.
Sensitivity Analyses
Overall, results of the sensitivity analyses indicated that the result of the base-case analysis was robust to changes in the input parameters and assumptions used, with smart insulin pens found to be dominant relative to standard care in all sensitivity analyses (Table 3; in EUR in Supplementary Table S6). Shortening the time horizon led to smaller clinical benefits and cost savings with smart insulin pens compared with standard care; however, smart insulin pens remained dominant over standard care for even the shortest time horizon of 3 years (Table 3). The HbA1c improvement with smart insulin pens was a key driver of outcomes, as demonstrated through abolishing the treatment effect in HbA1c and hypoglycemic events in turn. When the HbA1c difference between arms was not applied, the clinical benefit fell from 1.15 QALYs (base-case analysis) to 0.24 QALYs, with smart insulin pens remaining dominant over standard care (Table 3). When hypoglycemic event rates were assumed equal in both arms, the clinical benefit fell from 1.15 QALYs (base-case analysis) to 0.90 QALYs (Table 3). Compared with the base-case analysis (treatments maintained for the full 60-year time horizon), switching patients in the standard care arm to smart insulin pens after 3–10 years of the simulation yielded smaller differences in costs and clinical benefits between the simulation arms, as the treatment effects in HbA1c, hypoglycemia, and treatment costs were abolished during the analysis, rather than being maintained for the entire time horizon as in the base case.
Table 3.
Results of the sensitivity analyses
| Analysis | Discounted direct costs (SEK) | Discounted combined costs (SEK) | Discounted quality-adjusted life expectancy (QALYs) | ICER (SEK per QALY)a | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Smart insulin pen | Standard care | Difference | Smart insulin pen | Standard care | Difference | Smart insulin pen | Standard care | Difference | ||
| Base case | 635,599 | 759,869 | − 124,270 | 1,541,648 | 2,039,643 | − 497,995 | 14.74 | 13.59 | + 1.15 | Smart insulin pens dominant |
| 3-year time horizon | 39,204 | 42,490 | − 3286 | 95,520 | 141,403 | − 45,884 | 2.21 | 2.17 | + 0.04 | Smart insulin pens dominant |
| 5-year time horizon | 68,034 | 76,006 | − 7972 | 171,264 | 251,522 | − 80,258 | 3.55 | 3.47 | + 0.08 | Smart insulin pens dominant |
| 10-year time horizon | 147,293 | 172,482 | − 25,190 | 403,989 | 579,865 | − 175,876 | 6.45 | 6.26 | + 0.19 | Smart insulin pens dominant |
| Baseline HbA1c of 7.96% (64 mmol/mol) | 503,716 | 590,549 | − 86,833 | 1,232,903 | 1,630,768 | − 397,865 | 15.80 | 14.86 | + 0.94 | Smart insulin pens dominant |
| Baseline HbA1c of 7.1% (54 mmol/mol) | 425,384 | 483,414 | − 58,030 | 1,046,641 | 1,383,286 | − 336,645 | 16.52 | 15.74 | + 0.78 | Smart insulin pens dominant |
| HbA1c reduction of 0.4% (4 mmol/mol)b | 684,446 | 759,869 | − 75,422 | 1,656,833 | 2,039,643 | − 382,810 | 14.38 | 13.59 | + 0.80 | Smart insulin pens dominant |
| HbA1c reduction of 0.8% (9 mmol/mol)b | 615,900 | 759,869 | − 143,969 | 1,489,429 | 2,039,643 | − 550,214 | 14.91 | 13.59 | + 1.33 | Smart insulin pens dominant |
| HbA1c treatment effect not applied | 758,052 | 759,869 | − 1817 | 1,840,469 | 2,039,643 | − 199,173 | 13.83 | 13.59 | + 0.24 | Smart insulin pens dominant |
| Hypoglycemia difference not applied | 649,065 | 759,869 | − 110,803 | 1,755,774 | 2,039,643 | − 283,869 | 14.48 | 13.59 | + 0.90 | Smart insulin pens dominant |
| Treatment switched after 3 yearsc | 635,598 | 663,626 | − 28,028 | 1,541,634 | 1,648,193 | − 106,559 | 14.74 | 14.48 | + 0.25 | Smart insulin pens dominant |
| Treatment switched after 5 yearsc | 635,598 | 680,623 | − 45,025 | 1,541,635 | 1,718,398 | − 176,763 | 14.74 | 14.33 | + 0.40 | Smart insulin pens dominant |
| Treatment switched after 10 yearsc | 635,598 | 707,083 | − 71,485 | 1,541,635 | 1,848,503 | − 306,868 | 14.74 | 14.04 | + 0.70 | Smart insulin pens dominant |
HbA1c glycated hemoglobin, ICER incremental cost-effectiveness ratio, QALY quality-adjusted life-year, SEK 2018 Swedish krona
aICER is reported for both direct and combined costs and, in all sensitivity analysis simulations, the outcome of dominance was the same when either direct or combined costs were considered
bFor the smart insulin pen relative to standard care
cIn the standard care simulation arm to smart insulin pen use, performed by removing differences in HbA1c, hypoglycemic event rates, and treatment costs from the time of switch until the end of the time horizon
Discussion
In this analysis, clinical outcomes and healthcare costs were modeled following the introduction of a smart insulin pen versus standard of care for adults in Sweden with T1D to determine cost-effectiveness. Direct cost savings with the smart insulin pen were projected to be SEK 124,270 (EUR 11,309) per patient and combined cost (direct and indirect costs) savings to be SEK 497,995 (EUR 45,318) per patient. Use of smart insulin pens was associated with increases in both mean discounted life expectancy of 0.90 years per patient and mean quality-adjusted life expectancy of 1.15 QALYs per patient, compared with standard care.
There is a growing market for digital health solutions in chronic disease management [9] and they are becoming increasingly established in the management of diabetes [14]. Smart insulin pens are one such innovation that have the ability to integrate refillable insulin cartridges, wireless communication, and insulin delivery tracking, and display information to the user [31]. Our analysis, modeled on the efficacy of a smart insulin pen in the Swedish prospective, noninterventional study [15], provides important information on long-term cost-effectiveness. Ultimately, it is the cost and payer coverage that will determine uptake of smart insulin pens, but this is likely to increase on the basis of demonstrable cost-effectiveness [31].
Improvements in life expectancy with a smart insulin pen occurred as a result of a reduced frequency and increased time to onset of almost all diabetes-related complications over the 60-year time horizon, owing to a reduction in HbA1c with smart insulin pens (converted from TIR). Cataract was the only diabetes-related complication that had a higher projected cumulative incidence rate in the smart insulin pens arm versus standard care, likely to be as a result of increased survival. As such, it is important to note that the cumulative incidence of all other diabetes-related complications was lower than in the standard care arm despite the longer survival. Results of the sensitivity analyses confirmed that the reduction in HbA1c, as determined by TIR in the Swedish prospective, noninterventional study [15], associated with smart insulin pen use was a key driver of improved outcomes. However, even when the HbA1c treatment effect was abolished, smart insulin pens remained dominant versus standard care.
In the Swedish one-arm, prospective, observational, proof-of-concept study, the introduction of smart insulin pens was associated with significantly fewer missed bolus insulin doses than at baseline, most likely as a result of patients evaluating their past dosing data with their healthcare team, assisting with remembering to deliver mealtime insulin, improving insulin dose timing relative to meals, and adjusting insulin appropriately [15, 16]. This improved insulin management following the introduction of the smart insulin pen is likely to have contributed to the increased TIR, through more consistent and stable glucose levels [15, 16]. Following the publication of the Swedish prospective, noninterventional study findings, healthcare payers may have had financial concerns regarding overall cost-effectiveness, due to the higher bolus insulin use with smart insulin pens over standard care. Accordingly, in the present analysis, it was projected that smart insulin pens were associated with higher treatment costs than standard care (SEK 17,586 [EUR 1600] per patient), driven by higher bolus insulin use, as well as increased patient survival and, therefore, a longer duration of treatment over patients’ lifetimes. However, the cost of optimized insulin management with the smart insulin pen was offset by savings from a reduced incidence of diabetes-related complications in comparison with standard care from a lifetime perspective. Furthermore, the durability of smart insulin pens, with a life-span of up to 5 years [32], should alleviate concerns from payers regarding their upfront cost. Over patients’ lifetimes, projected cost savings to the Swedish public healthcare payer with smart insulin pens (versus standard care) might free up some of the limited healthcare budget allocated to T1D (refer to simulated cost distribution in Fig. 2a), and this could be directed towards other aspects of the care and management of people with T1D, for instance diabetes education and the prevention of complications.
Combined (direct and indirect) cost savings of almost SEK 500,000 [EUR 45,500] per patient were projected over a lifetime time horizon, with greater workplace productivity in the smart insulin pens arm than in the standard care arm. Smart insulin pens are designed to improve insulin administration and record data to facilitate discussion and action by patients and healthcare professionals [31], but from a global perspective are not yet widely funded. Smart insulin pens were dominant from both a public healthcare payer perspective (direct costs only) and a societal perspective (combined costs), with increased life expectancy and cost savings compared with standard care. While the base-case analysis was performed over a 60-year time horizon, with a 3% annual discount rate applied to projected outcomes, additional sensitivity analyses confirmed cost-effectiveness over time horizons as short as 3 years. Therefore, the findings of the present analysis add to a growing body of evidence that digital technologies can add value to the treatment of chronic diseases. To the best of the authors’ knowledge, this is the first economic evaluation of a smart insulin pen.
Limitations
Some limitations of this analysis should be acknowledged. Only TIR data were available from the Swedish prospective, noninterventional study [15] and, therefore, change in TIR was converted to change in HbA1c using a published regression equation [21], as there are no published risk equations allowing TIR to be directly linked to incidence of diabetes-related complications. While there is some uncertainty when making this conversion, sensitivity analyses were performed for various HbA1c levels to check the robustness of this conversion and the cost-effectiveness result, which all demonstrated that smart insulin pens were dominant versus standard care. Also noteworthy is that TIR has been associated with the risk of microvascular complications, and is an acceptable outcome measure for clinical trials [33]. A limitation of the Swedish prospective, noninterventional study, and therefore of the present analysis it informed, is the small study population and single-arm design [15]. Accordingly, baseline data were extrapolated for a hypothetical cohort who continued their previous regimen without a smart insulin pen, to make the comparison with the smart insulin pen simulation arm. In common with other health-economic analyses of diabetes interventions, the projections reported herein were reliant on relatively short-term clinical data. However, in the absence of long-term clinical data, modeled projections represent the best available alternative, while a long-term perspective is recommended by guidelines for cost-effectiveness analyses of diabetes interventions. Attempts were made to mitigate some of the inherent uncertainly around long-term projections through the use of a previously published and extensively validated model, as well as through conducting numerous sensitivity analyses to explore uncertainty in input parameters [34]. Our simulations were informed by clinical data from adults with T1D in Sweden and, hence, the findings may not be generalizable to wider populations. Future studies comparing smart insulin pens with standard care both in combination with CGMs are required to further validate that changes in glycemic control are a result of smart insulin pen use.
Conclusion
Our projections suggest that the introduction of smart insulin pens and their continued use over patients’ lifetimes was likely to improve clinical outcomes at lower costs relative to standard of care without smart insulin pens in a Swedish T1D population. Use of smart insulin pens in this adult patient population is, therefore, likely to be a good use of healthcare resources in Sweden.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank the participants of the Swedish prospective, noninterventional study, the study investigators and coordinators. The authors thank Ann-Charlotte Mårdby (Novo Nordisk A/S, Sweden) and João Diogo Da Rocha Fernandes (Novo Nordisk A/S, Denmark) for their review of and input to the manuscript.
Funding
Sponsorship for this analysis and the Rapid Service Fee were funded by Novo Nordisk A/S.
Medical Writing and/or Editorial Assistance
Medical writing support was provided by Zoe Schafer and editorial assistance provided by Helen Marshall, of Watermeadow Medical, an Ashfield company, part of UDG Healthcare plc, funded by Novo Nordisk A/S.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. J.J. is the guarantor of this work and, as such, had full access to all the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation
Some parts of this study were previously presented as a poster presentation at the 56th annual meeting of the European Association for the Study of Diabetes (EASD), 21–25 September 2020.
Disclosures
Johan H. Jendle has acted as an advisory panel member, board member or consultant for Abbott, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Medtronic, Novo Nordisk, and Sanofi, and has received research support and speaker honoraria from Abbott, AstraZeneca, Boehringer Ingelheim, Dexcom, Medtronic, and Novo Nordisk. William J. Valentine and Barnaby Hunt are full-time employees of Ossian, which received consultancy fees from Novo Nordisk to conduct the analyses. Åsa Ericsson, Jens Gundgaard, and Jonas Bech Møller are employees of and hold shares/stock in Novo Nordisk.
Compliance with Ethics Guidelines
This article does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.DiMeglio LA, Evans-Molina C, Oram RA. Type 1 diabetes. Lancet. 2018;391:2449–2462. doi: 10.1016/S0140-6736(18)31320-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.International Diabetes Federation . IDF Diabetes Atlas. 9. Brussels: International Diabetes Federation; 2019. [PubMed] [Google Scholar]
- 3.Alva M, Gray A, Mihaylova B, Clarke P. The effect of diabetes complications on health-related quality of life: the importance of longitudinal data to address patient heterogeneity. Health Econ. 2014;23:487–500. doi: 10.1002/hec.2930. [DOI] [PubMed] [Google Scholar]
- 4.Ahola AJ, Saraheimo M, Forsblom C, Hietala K, Sintonen H, Groop PH. Health-related quality of life in patients with type 1 diabetes-association with diabetic complications (the FinnDiane Study) Nephrol Dial Transplant. 2010;25:1903–1908. doi: 10.1093/ndt/gfp709. [DOI] [PubMed] [Google Scholar]
- 5.Lind M, Svensson AM, Kosiborod M, et al. Glycemic control and excess mortality in type 1 diabetes. N Engl J Med. 2014;371:1972–1982. doi: 10.1056/NEJMoa1408214. [DOI] [PubMed] [Google Scholar]
- 6.Bruno G, Pagano E, Rossi E, et al. Incidence, prevalence, costs and quality of care of type 1 diabetes in Italy, age 0–29 years: the population-based CINECA-SID ARNO Observatory, 2002–2012. Nutr Metab Cardiovasc Dis. 2016;26:1104–1111. doi: 10.1016/j.numecd.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Patterson CC, Harjutsalo V, Rosenbauer J, et al. Trends and cyclical variation in the incidence of childhood type 1 diabetes in 26 European centres in the 25 year period 1989–2013: a multicentre prospective registration study. Diabetologia. 2019;62:408–417. doi: 10.1007/s00125-018-4763-3. [DOI] [PubMed] [Google Scholar]
- 8.Berhan Y, Waernbaum I, Lind T, Möllsten A, Dahlquist G. Thirty years of prospective nationwide incidence of childhood type 1 diabetes: the accelerating increase by time tends to level off in Sweden. Diabetes. 2011;60:577–581. doi: 10.2337/db10-0813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petersen CL, Weeks WB, Norin O, Weinstein JN. Development and implementation of a person-centered, technology-enhanced care model for managing chronic conditions: cohort study. JMIR Mhealth Uhealth. 2019;7:e11082. doi: 10.2196/11082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iyengar V, Wolf A, Brown A, Close K. Challenges in diabetes care: can digital health help address them? Clin Diabetes. 2016;34:133–141. doi: 10.2337/diaclin.34.3.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah VN, Garg SK. Managing diabetes in the digital age. Clin Diabetes Endocrinol. 2015;1:16. doi: 10.1186/s40842-015-0016-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rabarison KM, Bish CL, Massoudi MS, Giles WH. Economic evaluation enhances public health decision making. Front Public Health. 2015;3:164. doi: 10.3389/fpubh.2015.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robinson R. Cost-utility analysis. BMJ. 1993;307:859–862. doi: 10.1136/bmj.307.6908.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fagherazzi G, Ravaud P. Digital diabetes: perspectives for diabetes prevention, management and research. Diabetes Metab. 2019;45:322–329. doi: 10.1016/j.diabet.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 15.Adolfsson P, Hartvig NV, Kaas A, Moller JB, Hellman J. Increased time in range and fewer missed bolus injections after introduction of a smart connected insulin pen. Diabetes Technol Ther. 2020 doi: 10.1089/dia.2019.0411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jendle JH, Hartvig NV, Kaas A, Moller J, Mårdby A-CM, Catrina S-B. 975-P: Effect of late bolus injections on glycemic variability studied by connected pens. Diabetes. 2020;69:975-P.
- 17.Battelino T, Danne T, Bergenstal RM, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019;42:1593–1603. doi: 10.2337/dci19-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Diabetes Association Consensus Panel. Guidelines for computer modeling of diabetes and its complications. Diabetes Care. 2004;27:2262–5. [DOI] [PubMed]
- 19.Palmer AJ, Roze S, Valentine WJ, et al. The CORE Diabetes Model: projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin. 2004;20(Suppl 1):S5–26. doi: 10.1185/030079904X1980. [DOI] [PubMed] [Google Scholar]
- 20.The Pharmaceutical Benefits Board. General guidelines for economic evaluations from the Pharmaceutical Benefits Board (LFNAR 2003:2). https://www.tlv.se/download/18.2e53241415e842ce95514e9/1510316396792/Guidelines-for-economic-evaluations-LFNAR-2003-2.pdf. Accessed Dec 2020.
- 21.Vigersky RA, McMahon C. The relationship of hemoglobin A1C to time-in-range in patients with diabetes. Diabetes Technol Ther. 2019;21:81–85. doi: 10.1089/dia.2018.0310. [DOI] [PubMed] [Google Scholar]
- 22.Danne T, Nimri R, Battelino T, et al. International consensus on use of continuous glucose monitoring. Diabetes Care. 2017;40:1631–1640. doi: 10.2337/dc17-1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. Global Health Observatory data repository: life tables by country (Sweden). 2018. https://apps.who.int/gho/data/view.main.61600?lang=en. Accessed Dec 2020.
- 24.Eeg-Olofsson K, Cederholm J, Nilsson PM, et al. Glycemic control and cardiovascular disease in 7,454 patients with type 1 diabetes: an observational study from the Swedish National Diabetes Register (NDR) Diabetes Care. 2010;33:1640–1646. doi: 10.2337/dc10-0398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eriksen M, Mackay J, Ross H. Tobacco Atlas (4th edition). Atlanta: American Cancer Society; 2013.
- 26.World Health Organization. Global alcohol report—Sweden. 2014. https://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/swe.pdf. Accessed Dec 2020.
- 27.Tandvårds- och läkemedelsförmånsverket (TLV) [Dental and pharmaceutical benefits board]. Databas för beslut [Database for decisions]. Stockholm, Sweden. https://www.tlv.se/beslut/sok-i-databasen.html. Accessed Dec 2020.
- 28.Statistics Sweden. Average monthly salary by sector 1992–2018. https://www.scb.se/en/finding-statistics/statistics-by-subject-area/labour-market/wages-salaries-and-labour-costs/salary-structures-whole-economy/pong/tables-and-graphs/average-monthly-salary-by-sector/. Accessed Mar 2020.
- 29.Sørensen J, Ploug U. The cost of diabetes-related complications: registry-based analysis of days absent from work. Econ Res Int. 2013:618039.
- 30.Jönsson L, Bolinder B, Lundkvist J. Cost of hypoglycemia in patients with type 2 diabetes in Sweden. Value Health. 2006;9:193–198. doi: 10.1111/j.1524-4733.2006.00100.x. [DOI] [PubMed] [Google Scholar]
- 31.Sangave NA, Aungst TD, Patel DK. Smart connected insulin pens, caps, and attachments: a review of the future of diabetes technology. Diabetes Spectr. 2019;32:378–384. doi: 10.2337/ds18-0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Novo Nordisk. Introducing NovoPen® 5. 2019. https://www.novonordisk.com/patients/diabetes-care/pens--needles-and-injection-support/NovoPen5.html. Accessed Aug 2020.
- 33.Beck RW, Bergenstal RM, Riddlesworth TD, et al. Validation of time in range as an outcome measure for diabetes clinical trials. Diabetes Care. 2019;42:400–405. doi: 10.2337/dc18-1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McEwan P, Foos V, Palmer JL, Lamotte M, Lloyd A, Grant D. Validation of the IMS CORE diabetes model. Value Health. 2014;17:714–724. doi: 10.1016/j.jval.2014.07.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.