Abstract
Breath-hold divers (BHD) enduring apnea for more than 4 min are characterized by resistance to release of reactive oxygen species, reduced sensitivity to hypoxia, and low mitochondrial oxygen consumption in their skeletal muscles similar to northern elephant seals. The muscles and myocardium of harbor seals also exhibit metabolic adaptations including increased cardiac lactate-dehydrogenase-activity, exceeding their hypoxic limit. We hypothesized that the myocardium of BHD possesses similar adaptive mechanisms. During maximum apnea 15O-H2O-PET/CT (n = 6) revealed no myocardial perfusion deficits but increased myocardial blood flow (MBF). Cardiac MRI determined blood oxygen level dependence oxygenation (n = 8) after 4 min of apnea was unaltered compared to rest, whereas cine-MRI demonstrated increased left ventricular wall thickness (LVWT). Arterial blood gases were collected after warm-up and maximum apnea in a pool. At the end of the maximum pool apnea (5 min), arterial saturation decreased to 52%, and lactate decreased 20%. Our findings contrast with previous MR studies of BHD, that reported elevated cardiac troponins and decreased myocardial perfusion after 4 min of apnea. In conclusion, we demonstrated for the first time with 15O-H2O-PET/CT and MRI in elite BHD during maximum apnea, that MBF and LVWT increases while lactate decreases, indicating anaerobic/fat-based cardiac-metabolism similar to diving mammals.
Subject terms: Cardiovascular biology, Cardiovascular biology
Introduction
The physiological adaptions in breath hold divers (BHD) to apnea, includes significant diving responses, attenuated post-apnea acidosis, reduced sensitivity to oxidative stress and, probably critical to their performances, reduced sensitivity to hypoxia1–6. It has also been demonstrated that similar to adaptions in the northern elephant seal, which can endure apnea for more than 120 min, BHD have a non-coupled maximum respiratory state in their skeletal muscles ~ 22–23% lower than matched aerobic athletes7. Hence, the skeletal muscles of BHD possess an oxygen conserving adaptation, and this might—at least partly—explain, the extreme performances of BHD holding their breath for more than 11 min and swimming as far as 300 m, or diving beyond 200 m in depth, all on a single breath of air (http://www.freedive-earth.com/aida-freediving-world-records). Similarly, samples of the skeletal muscles and the heart from adult harbor seals (Phoca Vitulina) shows up to sixfold higher β-hydroxyacyl-CoA dehydrogenase activities normalized to tissue-specific resting metabolic rate, and the heart of the seals possess the highest lactate dehydrogenase activity, compared to dog and rat, suggesting both a reliance on anaerobic metabolism during dives exceeding the animal's aerobic limit, but also a high aerobic capacity for lipid metabolism within the heart8. It could be hypothesized, that the hearts of BHD would possess similar adaptions. However, two cardiac magnetic resonance imaging (CMR) studies of BHD reported that after only 4 min of dry apnea concomitant with a reduction in arterial oxygen saturation ~ 23%, cardiac troponins increase, and CMR epicardial perfusion decreases about 60%9,10. We have reported of elite BHD enduring a reduced arterial oxygen saturation of more than ~ 33%4, and after competitions with pool static apneas of ~ 5 min (and subsequent 88 ± 21 m underwater swim), where cardiac troponins remains unchanged normal11. The explanation might be, that BHD who can endure apnea for more than 4 min have a lesser increase in ischemia-modified albumin (IMA), a marker of the release of reactive oxygen species (ROS) and a measure of resistance to hypoxemia, than compared to BHD who can endure less than 4 min of apnea12. This is in accordance with studies of adult seals are demonstrated to have a higher relative capacity for mitochondrial respiration than pups and juvenile seals13, and adult diving mammals also have resistance to release of ROS during dives to tolerate ischemia14,15, indicating that the hypoxic capacity is an adaption.
Hence, it is hypothesized that similar adaptive mechanisms to hypoxia as observed in the hearts of adult diving mammals could be observed in the hearts of human elite BHD, who can endure apnea for more than 4 min. This study aimed to demonstrate this hypothesized adaptation in BHD. As myocardial ischemia is dependent on both blood oxygen levels, perfusion and the need of oxygen based on cardiac contraction, these parameters were quantified using arterial samples, cine CMR and 15O-H2O-PET/CT and the resulting myocardial oxygenation as a sign of ischemia measured using BOLD CMR at rest and during a maximal voluntary apnea in elite BHD with a self-reported maximum static apnea of more than 5 min.
Methods
This study included eight Danish healthy male non-smoking subjects and was approved by the Regional Ethics Committee of Copenhagen (H-1-2013-060). All clinical investigations were conducted according to the principles expressed in the Declaration of Helsinki. Informed consent, written and oral, were obtained from the participants.
All subjects were elite BHD (age 42 ± 8 years) able to hold their breath for more than 5 min and ranked among the national top 10. Three ranked among the World top 10, one was a 2016 outdoor free-diving World champion, one reached third place at the same championship (no limit depth competition), and one was a World record holder.
VO2 max measurement and dual-energy X-ray absorptiometry scan
Subjects completed a standardized warm-up followed by an incremental cycling test starting at a workload of 150 W and increasing 25 W every minute until voluntary exhaustion. Pulmonary O2 and CO2 concentrations in the expired gas were continuously measured breath-by-breath (Quark, Cosmed, Rome, Italy) during the test. The highest recorded 30 s average oxygen uptake (VO2) during the test was defined as VO2max. For recognition of true VO2max three of five criteria had to be met: individual perception of exhaustion, respiratory exchange ratio > 1.15, plateau of VO2 curve, heart rate approaching age-predicted maximum and inability to maintain a pedaling frequency above 70 rpm. A dual-energy X-ray absorptiometry scan (Lunar iDXA; Lunar, Madison, WI, USA) was performed to assess body composition.
Cardiac magnetic resonance imaging (CMR)
Image acquisition
For one day prior to the study, the subjects refrained from physical exercise and consumption of alcohol or caffeine. Imaging was performed in a 1.5 T MR imaging system (Achieva, Philips Medical System, The Netherlands) after a warm-up of three consecutive apnea to maximize the diving response4. Cine images were acquired at (1) rest during a short (< 20 s) apnea at end-expiration with open pharynx, (2) end of a apnea with max expiration and (3) the end of dry static apnea after glossopharyngeal insufflation (GPI)16. Images were collected shortly before end of apnea before breathing, and subjects were instructed to stay as calm as possible during imaging to avoid imaging artefacts. Cardiac chamber volumes and function were collected in the transversal and double-oblique short axis stacks with 8 mm thick slices and 25% gap. Cine imaging were performed with retrospectively ECG-gated steady-state free precession sequences (SSFP) reconstructed to 25 phases covering the entire cardiac cycle using the following settings: TR/TE 3.3/1.6 ms, flip angle 60°; and spatial resolution 1.3 × 1.3 × 8 mm3. For blood oxygen level dependence (BOLD) imaging a fast gradient-echo multi-echo black blood T2* sequence was used in the short axis plane17,18. The BOLD sequences were acquired at rest and after 240 s of apnea, to ensure image collection on all subjects, as the duration of this could be up to 20 s. BOLD had the following settings: TR 25.8 ms with effective repetition time 1600 ms and collecting 14 images with TE from 3.2 to 24.1 ms, flip angle 20°; and spatial resolution 1 × 2 × 1.2 × 8 mm3.
Image analysis
Left and right ventricular (LV and RV) and atrial (LA and RA) volumes were determined in end-diastole (ED) and end-systole (ES) and used to determine the influence of apnea on cardiac volumes, function, filling and individual chamber outflow. Data were analyzed by one experienced level three CMR reader and one level one CMR cardiologist using dedicated software (Segment version 2.1) carefully avoiding image artefacts and imaging especially during involuntary breathing movements19. LV wall thickness (LVWT) was determined from a midventricular short-axis slice from the epicardial and endocardial borders delineations of the left ventricle at end-diastole. Stroke volume (SV) was computed as the difference between end diastolic volume (EDV) and end systolic volume (ESV). Ejection fractions were computed as SV divided by EDV. T2* was determined from the BOLD images using a LV septal midwall region of interest carefully avoiding image artefacts and using a fitting algorithm in the Segment software as previously described20.
Arterial blood gases and hemodynamic data
On a separate day, after a warm-up of three consecutive apneas to maximize the diving response4, all subjects performed a maximum static pool apnea to simulate apnea during natural circumstances; (1) before, (2) after 4 min of apnea, and (3) just before end of maximum apnea, arterial blood samples were obtained through a catheter (1.1 mm, 20 gauge) in the radial artery of the non-dominant arm with connection to a transducer for continuous flow of saline (Baxter, Uden, the Netherlands). Blood gas analyses were performed immediately after sampling, using an automated self-calibrating blood gas machine (ABL 725, Radiometer, Copenhagen, Denmark) and evaluated for pH, bicarbonate, lactate, PaCO2, and the arterial oxygen tension (PaO2).
Arterial blood pressures and heart rates were recorded concomitantly using a Lifepack ® 20 monitor.
Lipids
Blood samples for lipid analysis were collected following 8 h of fasting from the radial artery as described above for arterial blood gas collection, and before the pool dive. Total Cholesterol, High-density lipoprotein, Low-density lipoprotein and Triglycerides were measured with an automated analyzer (Roche Integra 400, Roche Diagnostics, Switzerland) using commercially available kits.
15O-H2O-PET/CT perfusion determined myocardial metabolism
Imaging protocol and image reconstruction
The six subjects with the longest pool maximum apneas, were recruited for an additional 15O-H2O-PET/CT study. The participants in the 15O-H2O-PET/CT sub-study were required to be able to hold their breath for 5 min while lying in the PET/CT scanner in the supine position with arms raised above the head. They were instructed to refrain from intake of chocolate, to refrain from strenuous physical exercise for one day and to be fasting for at least 6 h before the study.
15O-H2O-PET/CT data were obtained in list mode on a GE Discovery MI Digital Ready PET/CT system (GE, Milwaukee, WI, USA). The participants underwent three image acquisitions: (1) at rest, (2) during hyperemia induced by a dry static apnea after GPI16 and after a warm-up of three consecutive apneas to maximize the diving response4, and (3) third in the recovery phase 4 min after the apnea (Fig. 1). For each acquisition, 400 MBq 15H2O was administered intravenously in an antecubital vein as a single bolus using an automated injection system (Medrad Stellant, Bayer, Leverkusen, Germany). For the stress acquisition, 15H2O was infused after 2 min (n = 3) or 4 min (n = 3) after initiation of the apnea with acquisition of data for at least an additional 2 min (Fig. 1). Average apnea duration was 378 ± 77 s. For each PET scan, an attenuation CT was performed at time points allowing for correct co-registration of the PET and CT images. The resting and recovery attenuation correction CT’s were thus performed immediately prior to and after the PET scans, whereas the apnea attenuation correction CT was performed during warm-up mimicking maximal apnea.
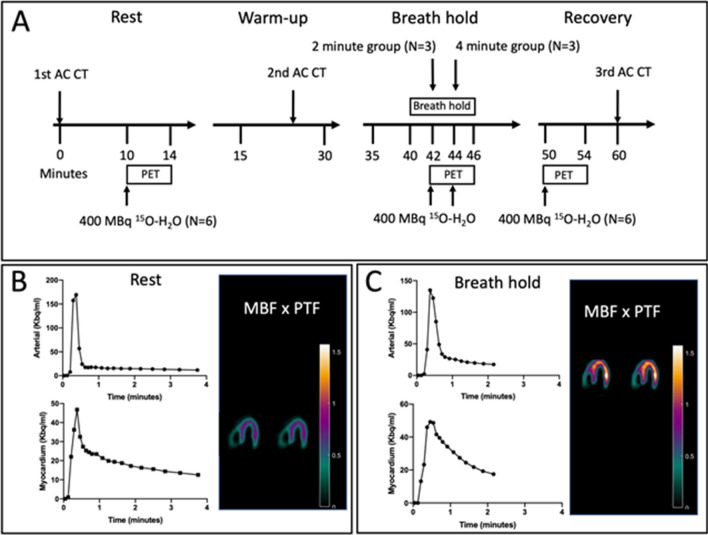
Figure 1.
(A) 15O-H2O-PET/CT study day flowchart. The resting and recovery perfusion 15O-H2O-PET/CT scans were performed in all participants, whereas the apnea perfusion 15O-H2O-PET/CT was performed with participants divided into two groups with radiotracer bolus injected at 2- and 4-min after initiation of apnea. The average breath hold of all participants were 378 ± 77 s. (B) Example of input function (arterial radioactivity, upper row) and myocardial time-activity curves (lower row) in a representative participant. As seen, the entire time-activity curve of the participant has been captured allowing for precise calculation of MBF and PTF. In the right column, horizontal long axis slices with calculation of MBF × PTF allows for parametric visualization of radiotracer uptake in the left ventricle. (C) Input function and myocardial time-activity curve for the same subject during apnea. Due to cessation of apnea approximately 2-min after injection of radiotracer (the participant was in the 4-min group), the entire myocardial time-activity curve was not recorded. However, the inflow of tracer was accurately recorded allowing for accurate determination of MBF × PTF, evident from the correct delineation of the left ventricle on the horizontal long axis slices (right side column).
Image analysis
Myocardial blood flow (MBF) was quantified by 15O-H2O-PET/CT on a GE Discovery MI Digital Ready PET/CT system (GE, Milwaukee, WI, USA) at time points as specified above. The 4-min dynamic images were reconstructed in a 3.27 × 3.27 × 3.27 mm matrix utilizing all normal corrections (attenuation, scatter, dead time and randoms) and the VPFX-S reconstruction algorithm. For subsequent analysis, the dynamic scan was divided into 21 frames (1 × 10, 8 × 5, 4 × 10, 2 × 15, 3 × 20 and 2 × 30 s). Kinetic analyses were performed using aQuant software (MedTrace Pharma, Lyngby, Denmark) and a validated 1-tissue compartment model with image derived input from cluster analysis, corrections for spillover and automatic estimation of MBF and perfusable tissue fraction (PTF)21. In healthy subjects, PTF primarily reflects the incomplete estimation of true tissue radiotracer uptake (the partial volume effect), which is a particular challenge in subjects with diaphragmatic movements and therefore reported. This parameter is derived from the tracer inflow, whereas MBF is derived from the outflow curve (see Fig. 1B for examples).
Statistical analysis
To test for imbalances in the variables in our study with a limited number of subjects, we performed a power calculation: A P-value < 0.05 was considered statistically significant. Given this level of significance, our sample size of 6 subjects in the 15O-H2O-PET/CT sub study resulted in a power of 80% to detect an expected increase in MBF of at least 1 ml/g/min with a standard deviation of 0.422.
Variables are presented as mean ± standard error of the mean (SEM). Data were analyzed by Sigma-Plot ® using one-way repeated measures ANOVA. Kruskal–Wallis with Tukey’s methods posthoc respectively were used to evaluate differences between the collected data during rest, apnea, and recovery. Time-related changes in MBF, PTF and MBF × PTF interaction in the 2- and 4-min groups were analyzed using a mixed model repeated measures ANOVA.
Results
VO2 max and dual-energy X-ray absorptiometry scan
The morphometric variables age, height, body mass, whole-body aerobic capacity (VO2max) and lipids, are displayed in Table 1.
Table 1.
Subject characteristics.
| Parameter | Result |
|---|---|
| No. subjects | 8 male BHD |
| Static personal best (seconds) | 395 ± 48 |
| Dynamic pool personal best (meters) | 171 ± 38 |
| Dynamic pool no fins personal best (meters) | 143 ± 38 |
| Age (years) | 43 ± 8 |
| Height (cm) | 186 ± 8 |
| Weight (kg) | 80 ± 6 |
| Body surface area | 2.0 ± 0.1 |
| Body Mass Index | 23.1 ± 1.9 |
| Fat mass % | 19.0 ± 3.4 |
| Bone mineral content (kg) | 3.2 ± 0.3 |
| Fat (kg) | 15.2 ± 3.7 |
| Fat free mass (kg) | 62.1 ± 4.2 |
| Bone mineral density (kg/m2) | 1.3 ± 0.1 |
| T/Z-score (+ 1 to − 1) | 0.8 ± 1.0 |
| Maximal oxygen uptake (ml O2/min) | 3672 ± 672 |
| Capillary Hemoglobin (g/dl) | 15.2 ± 0.8 |
| Venous Hemoglobin (calculated66, g/dl) | 14.6 ± 0.7 |
| Cholesterol mmol/l | 4.8 ± 0.9 |
| HDL mmol/l | 1.3 ± 0.4 |
| LDL mmol/l | 3.1 ± 1.2 |
| Triglycerid | 1.1 ± 0.3 |
| Creatinine mmol/l | 81 ± 14 |
Basic morphometric data. Values are mean ± Standard Error of Means.
BHD breath hold divers, HDL High density lipoprotein, LDL low density lipoprotein.
Pool apnea
After GPI and 326 ± 19 s of static apnea in a pool, heart rate (HR) decreased from 86 ± 5 bpm to 50 ± 13 beats/min (P < 0.001, Tables 2, 3), while Mean Arterial Blood pressure (MAP) increased from 103 ± 4 mmHg to 148 ± 15 mmHg (P < 0.001), and PaCO2 rose from 5.2 ± 0.2 kPa to 7.0 ± 0.2 kPa (P < 0.001) concomitant with a decrease in PaO2 from 12.2 ± 0.5 kPa to 4.3 ± 0.4 kPa (P < 0.001), and a decrease in pH from 7.42 ± 0.029 to 7.35 ± 0.01 (P < 0.001) and a decrease in lactate from 1.70 ± 0.13 to 1.36 ± 0.18 (P = 0.013).
Table 2.
Hemodynamic parameters and blood gas results at rest, after 4 min apnea and at end of apnea (326 ± 19 s).
| Rest | 4 min apnea | Max apnea | After apnea | |
|---|---|---|---|---|
| MAP/mmHg | 81 ± 5 | 87 ± 7 | 58 ± 4 * | P < 0.001 |
| HR/beats min−1 | 117 ± 4 | 113 ± 10 | 60 ± 3 * | P < 0.001 |
| SaO2/ % | 7.4 ± 0.4 | 7.3 ± 0.6 | 4.9 ± 0.4 * | P < 0.001 |
| Neck saturation/% | 59 ± 1 | 56 ± 1 | 51 ± 2 * | P = 0.003 |
| pH | 207 ± 8 | 202 ± 16 | 128 ± 7 * | P < 0.001 |
| PaCO2/kPa | 93 ± 6 | 93 ± 6 | 73 ± 5 * | P < 0.001 |
| PaO2/kPa | 114 ± 4 | 109 ± 10 | 56 ± 3 * | P < 0.001 |
| SBE | 55 ± 1 | 53 ± 1 | 44 ± 1 * | P < 0.001 |
| Bicarbonate | 35 ± 3 | 37 ± 8 | 24 ± 2 * | P = 0.013 |
| Lactate | 79 ± 5 | 102 ± 6 * | 46 ± 5 * | P < 0.042 |
Values are means ± Standard Error of Means. *P < 0.05 vs. rest and ***P < 0.001.
MAP mean arterial pressure, HR heart rate, SBE standard base excess, SaO2 arterial oxygen saturation. PaCO2 partial pressure of carbondioxide, PaO2 Partial pressure of oxygen.
Table 3.
Cardiovascular variables and organ volumes as evaluated with Cardiac Magnetic Resonance imaging at rest, at end of apnea with maximal expiration and at end of 240 s of apnea with glossopharyngeal insufflation (GPI) in 8 elite breath-hold divers.
| Parameter | Rest | End of apnea with max expiration | End of apnea with GPI | P-value: GPI compared to rest |
|---|---|---|---|---|
| LV EDV, ml | 198 ± 8 | 199 ± 16 | 119 ± 6 * | P < 0.001 |
| LV ESV, ml | 81 ± 5 | 87 ± 7 | 58 ± 4 * | P < 0.001 |
| LV SV, ml | 117 ± 4 | 113 ± 10 | 60 ± 3 * | P < 0.001 |
| LV CO, l/min | 7.4 ± 0.4 | 7.3 ± 0.6 | 4.9 ± 0.4 * | P < 0.001 |
| LV EF, % | 59 ± 1 | 56 ± 1 | 51 ± 2 * | P = 0.003 |
| RV EDV, ml | 207 ± 8 | 202 ± 16 | 128 ± 7 * | P < 0.001 |
| RV ESV, ml | 93 ± 6 | 93 ± 6 | 73 ± 5 * | P < 0.001 |
| RV SV, ml | 114 ± 4 | 109 ± 10 | 56 ± 3 * | P < 0.001 |
| RV EF, % | 55 ± 1 | 53 ± 1 | 44 ± 1 * | P < 0.001 |
| LA EDV, ml | 35 ± 3 | 37 ± 8 | 24 ± 2 * | P = 0.013 |
| LA ESV, ml | 79 ± 5 | 102 ± 6 * | 46 ± 5 * | P < 0.042 |
| RA EDV, ml | 56 ± 9 | 59 ± 10 | 29 ± 4 * | P = 0.009 |
| RA ESV, ml | 104 ± 12 | 131 ± 10 | 40 ± 4 * | P < 0.001 |
| BOLD, ms | 33.7 ± 2.8 | NA | 32.6 ± 1.9 | P = 0.453 |
| LVWT, mm | 7.5 ± 0.44 | NA | 9.8 ± 0.51 | P < 0.005 |
Values are means ± Standard Error of Means. *P < 0.05 vs. rest.
GPI glossopharyngeal, insufflation; LV left ventricular; RV right ventricular; EDV end-diastolic volume; ESV end-systolic volume; SV stroke volume; CO cardiac output; EF ejection fraction; LA left atrial volume; RA right atrial volume; BOLD blood oxygen level dependent, LVWT left ventricular wall thickness.
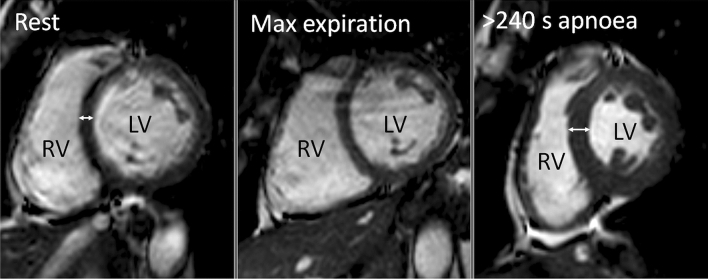
CMR
CMR after 240 s of apnea with GPI, revealed that ventricular volumes decreased, both right (~ 38%, P < 0.001, Table 3) and left (~ 40%, P = 0.001). Atrial volumes decreased as well, both right (~ 48%, P < 0.01) and left (~ 31%, P < 0.05), Right and left stroke volumes decreased (right ~ 51%, P < 0.001, left ~ 49%, P < 0.001) as did left ventricular cardiac output (~ 34%, P = 0.001). At the end of 240 s of apnea with GPI a decrease was observed in right and left ventricular ejection fraction (RVEF rest 53 ± 1% vs. BH 44 ± 1%, P < 0.001 and LVEF rest 59 ± 1% vs. apnea 51 ± 2%, P = 0.003), concomitant with an increase in LV wall thickness (~ 31%, P < 0.005, Fig. 2).
Figure 2.
Example of Cardiac MR imaging of one subject, displaying a midventricular short axis view at papillary muscle level at end-diastole. Compared to rest (left panel), the left ventricle (LV) and right ventricle (RV) are similar in size at end of apnea with maximum expiration (center panel). In contrast, at the end of > 240 s of apnea with glossopharyngeal insufflation (right panel) there is a decrease in LV and RV size and thickening of the ventricular wall (double-headed arrows) compared to rest.
T2* BOLD did not change.
Results at end of apnea with max expiration did not change compared to rest, except for LA ESV (Table 3).
Myocardial perfusion imaging (15O-H2O-PET/CT)
MBF increased after 4 min of apnea from 0.97 ± 0.15 ml/min/g at rest to 2.15 ± 0.39 ml/min/g during apnea (378 ± 77 s) induced stress (P = 0.001; Table 4), whereas PTF decreased from 0.67 ± 0.09 at rest to 0.58 ± 0.1 during apnea (P = 0.03, Table 4).
Table 4.
Myocardial blood flow (MBF) as evaluated with 15O-H2O-PET/CT at rest, during apnea of 378 ± 77 s and at recovery in 6 elite breath-hold divers.
| Rest (n = 5) | 2 min apnea (n = 3) | 4 min apnea (n = 3) | Recovery (n = 5) | P-value * | |
|---|---|---|---|---|---|
| MBF (ml/g/min) | 0.97 ± 0.15 | 0.82 ± 0.24 | 2.15 ± 0.39 | 1.02 ± 0.20 | 0.002 |
| PTF | 0.67 ± 0.09 | 0.71 ± 0.09 | 0.58 ± 0.10 | 0.68 ± 0.09 | 0.03 |
| MBF × PTF (ml/g/min) | 0.65 ± 0.17 | 0.58 ± 0.13 | 1.24 ± 0.23 | 0.70 ± 0.18 | 0.001 |
Values are means ± Standard deviations. *Mixed model repeated measures ANOVA. Rest compared to apnea.
MBF myocardial blood flow, PTF perfusable tissue fraction.
Discussion
The main and novel findings of our study are: After a warm-up of three consecutive apneas and 1) during 4 min of apnea, the hearts of BHD in this study were without signs of concomitant T2* BOLD assessed myocardial ischemia on CMR, 2) after 4 min of apnea 15O-H2O-PET/CT revealed increased myocardial blood flow to levels approaching theoretical maximum hyperemia23–26 without signs of regional myocardial perfusion deficits, and 3) at end of max pool apnea, systemic oxygenation decreased to 4.3 kPa ± 0.4 and pH decreases concomitant with a decrease in lactate in BHD. This has to our knowledge not previously been described. Hence, we demonstrated for the first time that BHD, similar to adult diving mammals, possess cardiac hypoxic resistance and increased myocardial blood flow with CMR and 15O-H2O-PET/CT during apnea ~ 6 min, and also lactate metabolization during max pool apnea. Our study also demonstrated that at end of max apnea with GPI, mean arterial blood pressure increased, and HR, biventricular EDV, CO and EF decreased, concomitant with an increase in LV wall diameter and an increase in PaCO2.
Guensch et al. demonstrated, that when PaCO2 is increased, myocardial perfusion and oxygenation remains preserved or even increased during apnea episodes of 60 s in anaesthetised animals and during voluntary apnea of up to 117 s in healthy humans27,28: Longer apneas causes higher increases in BOLD-signal intensity and a decline in capillary PO2 is compensated through a CO2-mediated increase in MBF as a countermeasure for desaturation and prevention of compromised myocardial oxygenation during long effective apneas28. During repetitive apnea in BHD combined with 100 W exercise, it has been demonstrated that PaO2 decreases to 7.3 kPa and PaCO2 increases to 8.2 kPa4 concomitant with a decrease in pH to 7.35. In this study, PaO2 decreased to 4.3 ± 0.4 kPa while PaCO2 increased to 7.0 ± 0.2 kPa and pH decreased to 7.35 during max apnea (326 ± 19 s). In part, this adaption to hypoxia and hypercapnia may explain the findings of sustained myocardial oxygenation and the increased MBF during apnea in our study, and the latter is comparable to increases in MBF during max exercise in endurance trained athletes29.
Kyhl et al. reported that myocardial perfusion index decreased 60% after ~ 4 min of apnea10, and Eichhorn et al. reported that 4–5 h after a similar period of apnea and a decrease in PaO2, ~ 23% in BHD, cardiac troponins elevate9. This study could not confirm these observations in elite BHD with personal records of static apnea of more than 5 min, and after a similar decrease in PaO2, after 4 min of apnea and at end of max apnea. Our observations are also consistent with animal models demonstrating that after the onset of myocardial ischemia, cell death is not immediate but takes a finite period to develop: it has been reported that the level of cardiac troponins I (cTnI) starts to increase by 30 min with a peak value at 3 h after cardiac arrest in adult pigs30 and 4 h of hypoxia in rats has no effect on coronary flow rate or cardiac troponin T31. cTNI (and Pro-atrial natriuretic peptide) also remain unaffected in competitive BHD 3 h after two consecutive maximum apneas (static apnea ~ 5 min and subsequent ~ 88 m underwater swim) (Kjeld T. et al. 2014). The question is, why the otherwise highly adapted BHD, possessing extreme tolerance for hypoxia1–5,7 including a mitochondrial adaption to hypoxia in their skeletal muscles similar to the northern elephant seal7, should display or suffer from cardiac injury after only 4 min of apnea9,10? However, high altitude permanent residents, chronically exposed to hypoxia, suffer more often from acute coronary syndromes than comparable low altitude populations, probably due to hyperlipidemia32 and hence arteriosclerotic coronary disease, and it may be, that the BHD studied by Kyhl et al. and by Eichhorn et al., were not as cardiac healthy as the subjects with normal lipids33 and low resting MBF34 in our study (Tables 1 and 4) or as well adapted as discussed below12.
Diving seals are exposed to repetitive cycles of ischemia and following reperfusion. Similarly sleeping seals experience sleep apnea, but do not increase production of ROS nor suffer systemic or local oxidative damage15 in contrast to terrestrial animals with sleep apnea. Joulia et al. demonstrated in BHD that ischemia-modified albumin (IMA), a marker of the release of ROS during hypoxemia, increases less in the BHD who endured apnea for more than 4 min, than compared to those who endure less than 4 min of apnea12. Our study included only BHD who endured apnea for more than 5 min, and our results indicated that they have a similar resistance to cardiac hypoxia as observed in adult diving mammals8. Our results included increased myocardial perfusion and are in contrast to the studies by Eichhorn et al. and Kyhl et al. of BHD enduring apneas of 4 min or less and reporting signs of myocardial injury and reduced myocardial perfusion9,10. However, studies of restrained and sedated seals demonstrate severely reduced myocardial perfusion during static apnea35, but sedation depresses the cardiovascular system including the myocardial regional oxygen supply36, and cannot be compared to the foraging animal with an increased metabolic demand during their dives. Compared to the lung tissue and skeletal muscles, seal hearts have the lowest levels of Hypoxia-Inducible Factor-1alpha, an adaptive protein to protect against hypoxia37,38. This indicates, that the hearts of seals, also sensitive to localized ischemia39, do not have decreased myocardial perfusion during their dives, as it would cause myocardial damage. Elite BHD performing maximum apnea, also go through a struggling phase, with muscular tensions, hence also an increased metabolic demand, which in part may explain the increased myocardial perfusion at end of apnea in our study.
Fatty acids are the major energy source for healthy myocardium, but lactate and ketone bodies, can be the energy substrate under certain circumstances40. Gormsen et al. demonstrated that ketone bodies increased myocardial blood flow 75% without affecting myocardial fatty acid transport or oxidative capacity in the myocardium of healthy subjects41. A novel study demonstrated that ketone bodies can even increase CO and LVEF in patients with heart failure without impairing myocardial external energy efficiency42. These observations are in line with our results of elite BHD, demonstrating that after a warm-up and during a consecutive maximum apnea, myocardial perfusion increases, concomitant with a decrease in pH and also a decrease in lactate. A decrease in lactate may be the consequence of decreased production, a higher metabolic rate or both, whereas hypercapnia-induced respiratory acidosis during exercise promote a decrease in blood pH43, but a respiratory acidosis have negligible effects on the lactate response44. We interpretate the concomitant decrease in pH as a consequence of the increase in PaCO245 during decreasing lactate in this study, the latter may indicate lactate metabolization, as discussed below. Similarly, the hearts of harbor seals have a heightened lactate dehydrogenase activity indicating an adaptation for the anaerobic production of adenosine triphosphate (ATP) on dives beyond the animal's aerobic dive limit8. Lactate is cumulated during aerobic exercise, and can be metabolized after exercise by skeletal muscle, heart, liver, kidneys, brain, adipose tissue and lungs46. However, Kaijser et al. demonstrated that lactate is the primary substrate for oxidation of the heart muscle cells during short-term normoxic heavy exercise in normal young subjects at sea level47, and similarly the subjects in our study performed maximum apnea with increases in MBF comparable to the increases in MBF in endurance trained athletes during maximum exercise29. Sherpas living in high altitude with chronic hypoxic exposure have also been demonstrated to decrease lactate levels during maximum exercise suggestive of lactate metabolization48,49. Hence, we suggest, that the elite BHD in our study have an adaption to metabolize lactate during hypoxia similar to these high-altitude Sherpas and the harbour seal cardiac mitochondria8.
Mitochondria are central to synthesis of ATP and ROS, and hence also important to myocyte death50,51. Exposing the myocardium to acute ischemia and reperfusion causes initially mitochondrial dysfunction and subsequent excessive production of ROS by the electron transport chain50. The deleterious effects of ROS include damage to the mitochondria52, resulting in depolarization and apoptosis53. These processes may ultimately lead to a compromised cardiac function: Chronic ischemic hearts in animal models also possess a decreased capacity for oxidative phosphorylation54–57, whereas hypoxia in a hypobaric environment may trigger increased cardiac carbohydrate metabolism and enhanced mitochondrial respiratory capacity, even with preserved contractile function58. Stride et al. demonstrated that chronic ischemic human hearts possess a decreased intrinsic mitochondrial respiration59, which ultimately may lead to failure of the left ventricle60. In this study of elite BHD during hypoxia, no signs of myocardial ischemia could be demonstrated by CMR or myocardial perfusion deficits by 15O-H2O-PET/CT, despite a decline in ejection fraction, and hence declined myocardial contractile function concomitant with bradycardia at end of apnea. We suggest that the resistance to even more extreme cardiac hypoxia in our study, than found in previous similar studies9,10, at least in part confirms our hypothesis, of elite BHD possessing a cardiac adaptive resistance to hypoxia.
Swine LV volume in a CMR closed-chest model have been demonstrated to decrease ~ 53% during 25 min of untreated ventricular fibrillation, while the mean interventricular width or LV wall thickness markedly increases61. At the end of apnea in our study, LVEDV decreased by ~ 49%, concomitantly with an ~ 31% increase in LV wall thickness and a ~ 49% decrease in LVCO which is consistent with the findings in similar studies of BHD9,10. Our findings are also comparable to observations in diving adult harbor seals in which thermodilution measured stroke volumes at surface are almost twice the volumes compared to when submerged62.
In conclusion, our study demonstrated for the first time cardiac hypoxic resistance and increased MBF in the hearts of elite BHD, during apnea of more than 5 min concomitant with systemic hypoxia below 4.3 kPa ± 0.4 and decreasing lactate. Our results indicate an increased ability for anaerobic and fat-based metabolism in the hearts of elite BHD during hypoxia similar to the harbor seal during routine diving. In elite BHD, biventricular EF and SV decreases at end of maximum apnea concomitant with bradycardia, similar to CMR of hypoxic diving mammals during apnea. Hence, the results of our study confirm, that the hearts of elite BHD have similar adaptions to hypoxia as air breathing diving mammals.
Perspectives
Future studies may reveal myocardial oxygen extraction at end of apnea in elite BHD, and may confirm presumed hyperdynamic LVEF due to lactate metabolization after apnea in elite BHD.
Furthermore, it is speculated that understanding of these mechanisms may help in the development of new treatments of severe clinical conditions caused by extreme hypoxia, e.g. cardiac surgery, organ transplantation and in the post-resuscitation care setting.
Limitations
The number of subjects was low because the inclusion criteria required the BHD to have very long apnea, and this may give problems with statistical power. A correlation analysis would be of interest to find a possible graded difference in diving response between subjects, but this would need to have a larger number of subjects with larger differences in levels of apnea. However, the findings were for most analyses statistically significant because of the pronounced physiological effects and each subject being its own control. BOLD on the other hand was not different during apnea compared to baseline and thus this finding should be viewed with some caution due to few subjects. The length of the apneas were different for MR, 15O-H2O-PET/CT and blood gases in the pool: BOLD-MR and blood gases were both collected at 4 min of breath-hold to be able to compare the results. 15O-H2O/PET-CT for absolute perfusion cannot be done at one time point but is collected over several minutes. Therefore, we collected data from 2 to more than 8 min of breath-hold. Subjects insisted on drinking coffee on the day for apneas before 15O-H2O-PET/CT, and therefore MBF may be impaired compared to fasting from caffein63,64. In one subject, resting and recovery 15O-H2O-PET/CT scans were lost due to technical difficulties.
Apnea during exercise with facial immersion have been demonstrated to increase the cardiovascular responses compared to apnea and exercise without facial immersion65. However, data collected in our study were both dry and wet static apnea, and a difference may be observed in the cardiovascular responses, if all data could be collected during wet apnea65.
Acknowledgements
We thank the volunteers for their enthusiasm in their participation in this study, and Niels Jensen from Stryker for lending equipment, and the Emergency Medical Service, Copenhagen, Denmark for the availability of monitor equipment. (LIFEPAK® 15 monitor & defibrillator). Also, we thank Katrine Linnet for collecting arterial blood gases, and Anders Reuss, Maria Birna Arnardottir, Brian Møllgren and Mogens Fenger for the biochemical analyses and Jacob Bejder & Nikolai Nordsborg for physical fitness testing. Jeppe Madsen and Lone Winkler Møller are thanked for their help performing the 15O-H2O-PET-CT studies. We thank Professor Hans-Erik Bøtker and Lars Thorbjørn Jensen for inspiration.
Author contributions
T.K. conceived the study and was in charge of the overall direction and planning of the presented idea and developed the hypothesis. All authors provided feedback, assisted in the analysis, critically revised the manuscript, and approved the final revised version. J.M., H.T., E.H., B.Z., L.G. and H.A. contributed to the design of the study. K.F., J.M., T.K., E.H., B.Z., L.G., A.B. and H.A. carried out the experiments. K.F., J.M., T.K., E.H., A.B., L.G. and H.A. contributed to sample preparation. All authors contributed to the interpretation and analysis of the results according to their specific specialized areas: CMR by M.C., E.O., H.T., J.M., K.F. and T.K., 15O-H2O-PET/CT by L.G. and T.K. VO2 max and dual-energy X-ray absorptiometry scan by B.Z. and A.B. Pool arterial blood gases, collection of lipid blood samples and non-invasive hemodynamic data by H.A., E.H., A.B., J.H. and T.K.
Funding
This study was supported by public funding from the Departments of Radiology and Anesthesiology, Herlev Hospital, University of Copenhagen, Denmark.
Data availability
Data collected in this study are all saved encrypted at hospital servers.
Competing interests
Thomas Kjeld is a voluntary (unpaid) board member of the Danish National Diving Federation. The other authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
3/11/2021
A Correction to this paper has been published: 10.1038/s41598-021-85418-9
References
- 1.Schagatay E, Van KM, Emanuelsson S, Holm B. Effects of physical and apnea training on apneic time and the diving response in humans. Eur. J. Appl. Physiol. 2000;82:161–169. doi: 10.1007/s004210050668. [DOI] [PubMed] [Google Scholar]
- 2.Foster GE, Sheel AW. The human diving response, its function, and its control. Scand. J. Med. Sci. Sports. 2005;15:3–12. doi: 10.1111/j.1600-0838.2005.00440.x. [DOI] [PubMed] [Google Scholar]
- 3.Lindholm P. Loss of motor control and/or loss of consciousness during breath-hold competitions. Int. J. Sports Med. 2007;28:295–299. doi: 10.1055/s-2006-924361. [DOI] [PubMed] [Google Scholar]
- 4.Kjeld T, Pott FC, Secher NH. Facial immersion in cold water enhances cerebral blood velocity during breathhold exercise in humans. J. Appl. Physiol. 2009;106:1243–1248. doi: 10.1152/japplphysiol.90370.2008. [DOI] [PubMed] [Google Scholar]
- 5.Kjeld T, Rasmussen MR, Jattu T, Nielsen HB, Secher NH. Ischemic preconditioning of one forearm enhances static and dynamic apnea. Med. Sci. Sports Exerc. 2014;46:151–155. doi: 10.1249/MSS.0b013e3182a4090a. [DOI] [PubMed] [Google Scholar]
- 6.Costalat G, Pichon A, Coquart J, Bauer F, Lemaitre F. Cardio-ventilatory responses to poikilocapnic hypoxia and hypercapnia in trained breath-hold divers. Respir. Physiol. Neurobiol. 2014;192:48–54. doi: 10.1016/j.resp.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Kjeld T, et al. Oxygen conserving mitochondrial adaptations in the skeletal muscles of breath hold divers. PLoS ONE. 2018;13:e0201401. doi: 10.1371/journal.pone.0201401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fuson AL, Cowan DF, Kanatous SB, Polasek LK, Davis RW. Adaptations to diving hypoxia in the heart, kidneys and splanchnic organs of harbor seals (Phoca vitulina) J. Exp. Biol. 2003;206:4139–4154. doi: 10.1242/jeb.00654. [DOI] [PubMed] [Google Scholar]
- 9.Eichhorn L, et al. Cardiovascular magnetic resonance assessment of acute cardiovascular effects of voluntary apnoea in elite divers. J. Cardiovasc. Magn Reson. 2018;20:40. doi: 10.1186/s12968-018-0455-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kyhl K, et al. Organ perfusion during voluntary pulmonary hyperinflation; A magnetic resonance imaging study. Am. J. Physiol. Heart Circ. Physiol. 2016;310:H444–H451. doi: 10.1152/ajpheart.00739.2015. [DOI] [PubMed] [Google Scholar]
- 11.Kjeld T, et al. Release of erythropoietin and neuron-specific enolase after breath holding in competing free divers. Scand. J. Med. Sci. Sports. 2015;25:e253–e257. doi: 10.1111/sms.12309. [DOI] [PubMed] [Google Scholar]
- 12.Joulia F, et al. Ischaemia-modified albumin during experimental apnoea. Can. J. Physiol. Pharmacol. 2015;93:421–426. doi: 10.1139/cjpp-2014-0538. [DOI] [PubMed] [Google Scholar]
- 13.Chicco AJ, et al. High fatty acid oxidation capacity and phosphorylation control despite elevated leak and reduced respiratory capacity in northern elephant seal muscle mitochondria. J. Exp. Biol. 2014;217:2947–2955. doi: 10.1242/jeb.105916. [DOI] [PubMed] [Google Scholar]
- 14.Vazquez-Medina JP, Zenteno-Savin T, Elsner R. Antioxidant enzymes in ringed seal tissues: Potential protection against dive-associated ischemia/reperfusion. Comp. Biochem. Physiol. C. 2006;142:198–204. doi: 10.1016/j.cbpc.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Vazquez-Medina JP, Zenteno-Savin T, Elsner R, Ortiz RM. Coping with physiological oxidative stress: a review of antioxidant strategies in seals. J. Comp. Physiol. B. 2012;182:741–750. doi: 10.1007/s00360-012-0652-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seccombe LM, et al. Features of glossopharyngeal breathing in breath-hold divers. J. Appl. Physiol. 2006;101:799–801. doi: 10.1152/japplphysiol.00075.2006. [DOI] [PubMed] [Google Scholar]
- 17.Vohringer M, et al. Oxygenation-sensitive CMR for assessing vasodilator-induced changes of myocardial oxygenation. J. Cardiovasc. Magn Reson. 2010;12:20. doi: 10.1186/1532-429X-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dharmakumar R, Qi X, Hong J, Wright GA. Detecting microcirculatory changes in blood oxygen state with steady-state free precession imaging. Magn. Reson. Med. 2006;55:1372–1380. doi: 10.1002/mrm.20911. [DOI] [PubMed] [Google Scholar]
- 19.Heiberg E, et al. Design and validation of Segment–freely available software for cardiovascular image analysis. BMC. Med. Imaging. 2010;10:1. doi: 10.1186/1471-2342-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bidhult S, et al. Validation of a new T2* algorithm and its uncertainty value for cardiac and liver iron load determination from MRI magnitude images. Magn. Reson. Med. 2016;75:1717–1729. doi: 10.1002/mrm.25767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harms HJ, et al. Automatic generation of absolute myocardial blood flow images using [15O]H2O and a clinical PET/CT scanner. Eur. J. Nucl. Med. Mol. Imaging. 2011;38:930–939. doi: 10.1007/s00259-011-1730-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Danad I, et al. Quantitative assessment of myocardial perfusion in the detection of significant coronary artery disease: Cutoff values and diagnostic accuracy of quantitative [(15)O]H2O PET imaging. J. Am. Coll. Cardiol. 2014;64:1464–1475. doi: 10.1016/j.jacc.2014.05.069. [DOI] [PubMed] [Google Scholar]
- 23.Nesterov SV, et al. Myocardial perfusion quantitation with 15O-labelled water PET: High reproducibility of the new cardiac analysis software (Carimas) Eur. J. Nucl. Med. Mol. Imaging. 2009;36:1594–1602. doi: 10.1007/s00259-009-1143-8. [DOI] [PubMed] [Google Scholar]
- 24.Nakazato R, Heo R, Leipsic J, Min JK. CFR and FFR assessment with PET and CTA: Strengths and limitations. Curr. Cardiol. Rep. 2014;16:484. doi: 10.1007/s11886-014-0484-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Uren NG, et al. Effect of aging on myocardial perfusion reserve. J. Nucl. Med. 1995;36:2032–2036. [PubMed] [Google Scholar]
- 26.Heinonen I, et al. Myocardial blood flow and adenosine A2A receptor density in endurance athletes and untrained men. J. Physiol. 2008;586:5193–5202. doi: 10.1113/jphysiol.2008.158113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guensch DP, Fischer K, Flewitt JA, Friedrich MG. Myocardial oxygenation is maintained during hypoxia when combined with apnea: A cardiovascular MR study. Physiol Rep. 2013;1:e00098. doi: 10.1002/phy2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guensch DP, et al. Breathing manoeuvre-dependent changes in myocardial oxygenation in healthy humans. Eur. Heart J. Cardiovasc. Imaging. 2014;15:409–414. doi: 10.1093/ehjci/jet171. [DOI] [PubMed] [Google Scholar]
- 29.Heinonen I, et al. Myocardial blood flow and its transit time, oxygen utilization, and efficiency of highly endurance-trained human heart. Basic Res. Cardiol. 2014;109:413. doi: 10.1007/s00395-014-0413-1. [DOI] [PubMed] [Google Scholar]
- 30.Bertsch T, et al. Cardiac troponin I and cardiac troponin T increases in pigs during ischemia-reperfusion damage. Exp. Toxicol. Pathol. 2000;52:157–159. doi: 10.1016/S0940-2993(00)80111-6. [DOI] [PubMed] [Google Scholar]
- 31.Asayama J, et al. Release kinetics of cardiac troponin T in coronary effluent from isolated rat hearts during hypoxia and reoxygenation. Basic Res. Cardiol. 1992;87:428–436. doi: 10.1007/BF00795055. [DOI] [PubMed] [Google Scholar]
- 32.Al-Huthi MA, Rajaa YA, Al-Noami M, Abdul Rahman AR. Prevalence of coronary risk factors, clinical presentation, and complications in acute coronary syndrome patients living at high vs low altitudes in Yemen. MedGenMed. 2006;8:28. [PMC free article] [PubMed] [Google Scholar]
- 33.Colantonio LD, et al. Association of serum lipids and coronary heart disease in contemporary observational studies. Circulation. 2016;133:256–264. doi: 10.1161/CIRCULATIONAHA.115.011646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guerraty MA, et al. The role of resting myocardial blood flow and myocardial blood flow reserve as a predictor of major adverse cardiovascular outcomes. PLoS ONE. 2020;15:e0228931. doi: 10.1371/journal.pone.0228931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kjekshus JK, Blix AS, Elsner R, Hol R, Amundsen E. Myocardial blood flow and metabolism in the diving seal. Am. J. Physiol. 1982;242:R97–104. doi: 10.1152/ajpregu.1982.242.1.R97. [DOI] [PubMed] [Google Scholar]
- 36.Kanto JH. Propofol, the newest induction agent of anesthesia. Int. J. Clin. Pharmacol. Ther. Toxicol. 1988;26:41–57. [PubMed] [Google Scholar]
- 37.Johnson P, Elsner R, Zenteno-Savin T. Hypoxia-inducible factor 1 proteomics and diving adaptations in ringed seal. Free Radic. Biol. Med. 2005;39:205–212. doi: 10.1016/j.freeradbiomed.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 38.Johnson P, Elsner R, Zenteno-Savin T. Hypoxia-Inducible Factor in ringed seal (Phoca hispida) tissues. Free Radic. Res. 2004;38:847–854. doi: 10.1080/10715760410001725526. [DOI] [PubMed] [Google Scholar]
- 39.Elsner R, et al. Coronary blood flow and myocardial segment dimensions during simulated dives in seals. Am. J. Physiol. 1985;249:H1119–H1126. doi: 10.1152/ajpheart.1985.249.6.H1119. [DOI] [PubMed] [Google Scholar]
- 40.Kodde IF, van der Stok J, Smolenski RT, de Jong JW. Metabolic and genetic regulation of cardiac energy substrate preference. Comp Biochem. Physiol. A. 2007;146:26–39. doi: 10.1016/j.cbpa.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 41.Gormsen LC, et al. Ketone body infusion with 3-hydroxybutyrate reduces myocardial glucose uptake and increases blood flow in humans: A positron emission tomography study. J. Am. Heart Assoc. 2017;6:e005066. doi: 10.1161/JAHA.116.005066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nielsen R, et al. Cardiovascular effects of treatment with the ketone body 3-hydroxybutyrate in chronic heart failure patients. Circulation. 2019;139:2129–2141. doi: 10.1161/CIRCULATIONAHA.118.036459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kato T, Tsukanaka A, Harada T, Kosaka M, Matsui N. Effect of hypercapnia on changes in blood pH, plasma lactate and ammonia due to exercise. Eur. J. Appl. Physiol. 2005;95:400–408. doi: 10.1007/s00421-005-0046-z. [DOI] [PubMed] [Google Scholar]
- 44.McLellan TM. The influence of a respiratory acidosis on the exercise blood lactate response. Eur. J. Appl. Physiol. Occup. Physiol. 1991;63:6–11. doi: 10.1007/BF00760793. [DOI] [PubMed] [Google Scholar]
- 45.Wasserman K. The anaerobic threshold: definition, physiological significance and identification. Adv. Cardiol. 1986;35:1–23. [PubMed] [Google Scholar]
- 46.Van HG. Lactate kinetics in human tissues at rest and during exercise. Acta Physiol. 2010;199:499–508. doi: 10.1111/j.1748-1716.2010.02122.x. [DOI] [PubMed] [Google Scholar]
- 47.Kaijser L, Berglund B. Myocardial lactate extraction and release at rest and during heavy exercise in healthy men. Acta Physiol. Scand. 1992;144:39–45. doi: 10.1111/j.1748-1716.1992.tb09265.x. [DOI] [PubMed] [Google Scholar]
- 48.Hochachka PW, et al. The lactate paradox in human high-altitude physiological performance. News Physiol. Sci. 2002;17:122–126. doi: 10.1152/nips.01382.2001. [DOI] [PubMed] [Google Scholar]
- 49.Ge RL, et al. Higher exercise performance and lower VO2max in Tibetan than Han residents at 4,700 m altitude. J. Appl. Physiol. 1994;77:684–691. doi: 10.1152/jappl.1994.77.2.684. [DOI] [PubMed] [Google Scholar]
- 50.Murphy E, Steenbergen C. Mechanisms underlying acute protection from cardiac ischemia-reperfusion injury. Physiol. Rev. 2008;88:581–609. doi: 10.1152/physrev.00024.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Murphy MP. How mitochondria produce reactive oxygen species. Biochem. J. 2009;417:1–13. doi: 10.1042/BJ20081386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Perrelli MG, Pagliaro P, Penna C. Ischemia/reperfusion injury and cardioprotective mechanisms: Role of mitochondria and reactive oxygen species. World J. Cardiol. 2011;3:186–200. doi: 10.4330/wjc.v3.i6.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Di LF, Bernardi P. Mitochondria and ischemia-reperfusion injury of the heart: Fixing a hole. Cardiovasc. Res. 2006;70:191–199. doi: 10.1016/j.cardiores.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 54.Boudina S, et al. Alteration of mitochondrial function in a model of chronic ischemia in vivo in rat heart. Am. J. Physiol. Heart Circ. Physiol. 2002;282:H821–H831. doi: 10.1152/ajpheart.00471.2001. [DOI] [PubMed] [Google Scholar]
- 55.Dos SP, Laclau MN, Boudina S, Garlid KD. Alterations of the bioenergetics systems of the cell in acute and chronic myocardial ischemia. Mol. Cell Biochem. 2004;256–257:157–166. doi: 10.1023/b:mcbi.0000009866.75225.e2. [DOI] [PubMed] [Google Scholar]
- 56.Hu Q, et al. Reductions in mitochondrial O(2) consumption and preservation of high-energy phosphate levels after simulated ischemia in chronic hibernating myocardium. Am. J. Physiol. Heart Circ. Physiol. 2009;297:H223–H232. doi: 10.1152/ajpheart.00992.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kelly RF, et al. Continued depression of maximal oxygen consumption and mitochondrial proteomic expression despite successful coronary artery bypass grafting in a swine model of hibernation. J. Thorac. Cardiovasc. Surg. 2011;141:261–268. doi: 10.1016/j.jtcvs.2010.08.061. [DOI] [PubMed] [Google Scholar]
- 58.Essop MF. Cardiac metabolic adaptations in response to chronic hypoxia. J. Physiol. 2007;584:715–726. doi: 10.1113/jphysiol.2007.143511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stride N, et al. Impaired mitochondrial function in chronically ischemic human heart. Am. J. Physiol. Heart Circ. Physiol. 2013;304:H1407–H1414. doi: 10.1152/ajpheart.00991.2012. [DOI] [PubMed] [Google Scholar]
- 60.Stride N, et al. Decreased mitochondrial oxidative phosphorylation capacity in the human heart with left ventricular systolic dysfunction. Eur. J. Heart Fail. 2013;15:150–157. doi: 10.1093/eurjhf/hfs172. [DOI] [PubMed] [Google Scholar]
- 61.Berg RA, et al. Magnetic resonance imaging during untreated ventricular fibrillation reveals prompt right ventricular overdistention without left ventricular volume loss. Circulation. 2005;111:1136–1140. doi: 10.1161/01.CIR.0000157147.26869.31. [DOI] [PubMed] [Google Scholar]
- 62.Ponganis PJ, Kooyman GL, Zornow MH, Castellini MA, Croll DA. Cardiac output and stroke volume in swimming harbor seals. J. Comp. Physiol. B. 1990;160:473–482. doi: 10.1007/BF00258974. [DOI] [PubMed] [Google Scholar]
- 63.Higgins JP, Babu KM. Caffeine reduces myocardial blood flow during exercise. Am. J. Med. 2013;126:730–738. doi: 10.1016/j.amjmed.2012.12.023. [DOI] [PubMed] [Google Scholar]
- 64.Carlsson M, et al. Submaximal adenosine-induced coronary hyperaemia with 12 h caffeine abstinence: Implications for clinical adenosine perfusion imaging tests. Clin. Physiol Funct. Imaging. 2015;35:49–56. doi: 10.1111/cpf.12125. [DOI] [PubMed] [Google Scholar]
- 65.Andersson JP, Liner MH, Runow E, Schagatay EK. Diving response and arterial oxygen saturation during apnea and exercise in breath-hold divers. J. Appl. Physiol. 2002;93:882–886. doi: 10.1152/japplphysiol.00863.2001. [DOI] [PubMed] [Google Scholar]
- 66.Schumacher YO, et al. Haemoglobin mass in cyclists during stage racing. Int. J. Sports Med. 2008;29:372–378. doi: 10.1055/s-2007-965335. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data collected in this study are all saved encrypted at hospital servers.