Abstract
Purpose
Verruca Vulgaris is a common benign cutaneous lesion which only reported occasionally to have malignant potential. Our purpose is to report a rare case of verruca vulgaris involving the eyelid and subsequently transformed into the combination of squamous cell carcinoma and basal cell carcinoma.
Observations
We reported a case of a 97-year-old female with a chronic biopsy proven verruca vulgaris involving the left lateral canthus. She presented with pain and swelling 5 years after the biopsy. Physical examination showed a painful warty crushed growth mass surrounded by erythematous skin changes, sized 40 × 40mm. Excisional biopsy showed squamous cell carcinoma and a microscopic focus of basal cell carcinoma.
Conclusions and importance
Our case demonstrates the oncogenic potential of verruca vulgaris into the combination of squamous cell carcinoma and basal cell carcinoma within one lesion. Size, chronicity and UV radiation may increase the risk of malignancy. Early surgical excision should be considered in eyelid involving chronic verruca vulgaris.
Keywords: Verruca vulgaris, Common wart, Squamous cell carcinoma, Basal cell carcinoma, Human papillovirus, Eyelid
Abbreviations: BCC, Basal cell carcinoma; HPV, Human Papillovirus; PCR, Polymerase chain reaction; SCC, Squamous cell carcinoma
1. Introduction
Verruca vulgaris (common wart) is a common Human Papillovirus (HPV) induced benign cutaneous lesion frequently seen on the hands.1 The lesion usually presents as a dome-shaped papules with a keratotic and verrucous surface, sized 1–20mm2. Facial lesions may have a filiform appearance.3 It is caused by different HPV subtypes, and HPV1, HPV2 and HPV4 are implicated in verruca vulgaris.2 While certain oncogenic subtypes are associated with genital wart such as HPV6 and HPV 11,4 there are reported cases of malignant transformation of verruca vulgaris in immunosuppressed patients5 and patients with lymphedema.6 We describe one case of verruca vulgaris involving eyelid later transforming into squamous cell carcinoma(SCC) and microscopic focus of basal cell carcinoma(BCC).
2. Case report
A 86-year-old Chinese female first attended our oculoplastic clinic at Tung Wah Eastern Hospital in March 2013 for pain over her left lateral canthus mass. The mass was first noticed in 2011, and the size was static without pain until 2013. There was no history of trauma nor constitutional symptoms. The patient was a chronic smoker and required long term medications for diabetes mellitus, hypertension and cardiac arrhythmia. She had both laparoscopic cholecystectomy and right modified radical mastectomy performed 10 years ago for cholangitis and breast cancer respectively.
Physical examination showed a well demarcated warty surface mass with tenderness, sized 30 × 20mm2, involving the left lateral canthus (Image1). There was no blood nor discharge. Blood test revealed decreased absolute lymphocyte level of 0.61 × 10^9/L (reference level<1). The differential diagnosis included verruca vulgaris, molluscum contagiosum, seborrheic keratosis, lichen planus and squamous cell carcinoma etc. Incisional biopsy of the mass showed pathohistological features of verrucous acanthosis, marked hyperkeratosis and parakeratosis, and the overall picture was compatible with verruca vulgaris. There was no dysplasia nor malignancy. Immunostaining or polymerase chain reaction (PCR) for HPV was not performed.
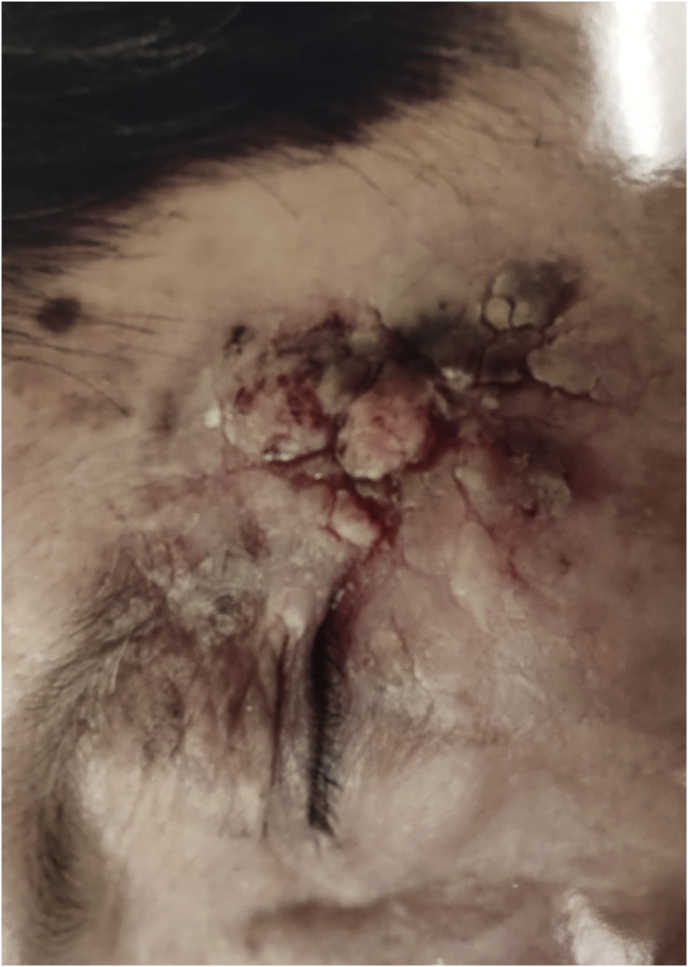
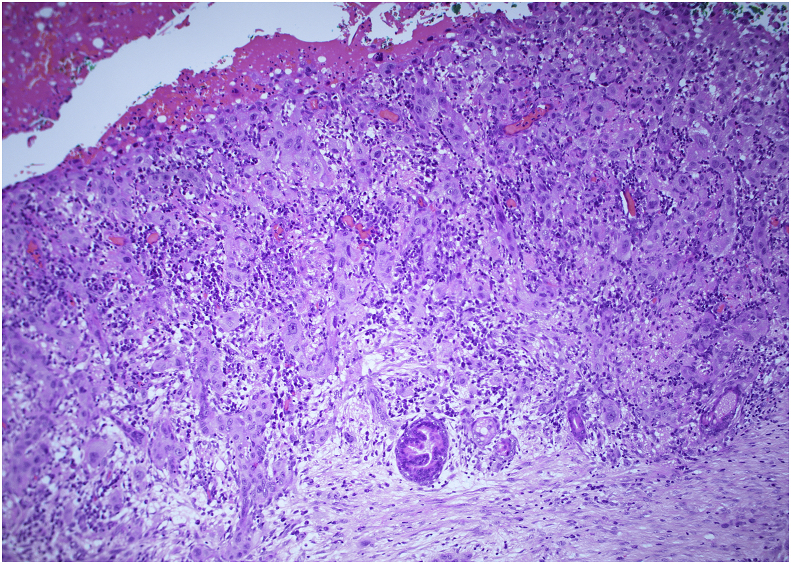
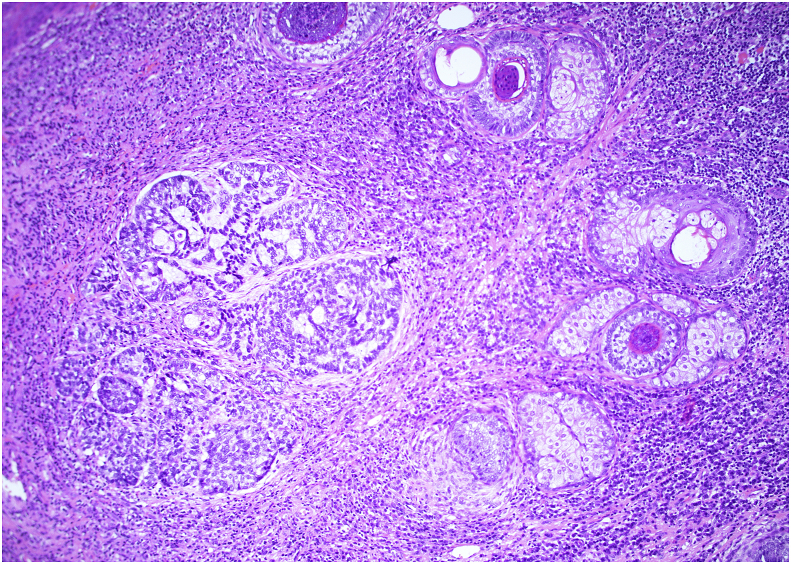
Pain subsided with topical Neomycin and Clotrimazole cream for 2 weeks. Mass remained static in size without pain for 5 years. This patient attended our oculoplastic clinic for the second time in March 2019. She complained of dull pain over the verruca vulgaris lesion. Physical examination revealed an enlarged painful mass over the lateral canthus, sized 40 × 40 mm2, with warty crushed growth surrounded by erythematous skin changes (Image2). Blood test showed decreased absolute lymphocyte level of 0.84 × 10^9/L(reference level <1). Pain persisted with a course of oral augmentin and topical chloramphenicol ointment for 1 week. Excisional biopsy of the mass and left eyelid reconstruction was performed. Cryotherapy was applied to the wound base, and all bleeding vessels were cauterized. Rotational flap from the left supra-brow skin and the skin graft from the supraclavicular region were used for the wound closure in view of the high skin tension (Image3). Pathohistological examination of the mass showed squamous cell carcinoma with invasion of 1.5mm in depth (Image4: Microscopic power 40x) and a microscopic focus of basal cell carcinoma (Image5: Microscopic power 100x) with a clear margin of less than 1mm. Both the circumferential and deep margins were clear of dysplasia and malignancy. Immunostaining and PCR for HPV were negative. The postoperative course was uneventful, and the wound healed healthily without complication for 12 months follow up.
3. Discussion
Verruca vulgaris is a common benign cutaneous lesion caused by HPV frequently found on hands.1 Despite different treatment modalities, recurrences are commonly seen.8 Two-thirds of warts disappear spontaneously within 24 months. Conservative approach or topical medications can be applied for solitary small size lesion.7 Large and chronic lesion may require surgical excision.8 Riad et al.14 reported the use of mitomycin C in recurrent eyelid margin verruca vulgaris without sign of recurrence for 8-months follow-up. We performed surgical excision for our patient because it was a chronic and large lesion with signs of inflammation. Clinical features, patient preferences and cost of treatment should all be taken into consideration for the treatment plan.
The usual size of verruca vulgaris is around 1–20 mm, and enlarged size suggests chronicity. The characteristic histopathologic features may lose with time, and HPV may not be detected in lesions of long duration.8 Routine HPV subtyping is not indicated in verruca vulgaris. We attempted to perform PCR for HPV from the first tissue biopsy 5 years ago, unfortunately the DNA quality was inadequate for PCR.
Cases reported on malignant transformation of Verruca Vulgaris were scarce, Goette et al.9 reported a case of carcinoma in situ in common wart and supported the oncogenic potential of the papovavirus. Another case reported by Noel et al.5 suggested that classic common warts may progress into high grade lesions in immunosuppressed patient, and HPV1 was identified in both tissue samples from common wart and SCC. Shelley et al.6 reported a patient with lymphedema and experienced common wart transformation into SCC. Both chronicity and large lesion as well as sun exposing area may contribute to the malignant transformation in our immunocompetent patient.
Basosquamous carcinoma is defined histologically as a tumor containing areas of both BCC and SCC with a transition zone between them.12 In comparison to our second tissue biopsy, it showed microscopic focus of basal cell carcinoma, 0.7 mm, in the dermis underneath the dysplastic epidermis focally without evidence of transition zone from SCC. Therefore, the presence of both SCC and BCC could be purely coincidental, or defined as collision tumor, which was described as the merging of 2 originally separate, adjacent, and often well-demarcated neoplasms within close proximity of each other.10
Retrospective review by Boyd and Rapini et al.11 of 40,000 cutaneous biopsies showed that 69 were collision tumors and none of them showed combination of SCC and BCC.
The combination of different tumors may be pure coincidence. BCC and melanocytic nevus were most reported combination in skin tumors.11 Several hypotheses proposed regarding the causes of the combination of different tumors. The field cancerization theory suggested that within an area with recurrent skin damage, such as UV radiation, the risk for development of 2 neoplasms within one lesion was increased.13 Our patient showed both SCC and BCC within one lesion, and both conditions occur in sun exposed area such as head and neck region. We proposed that long lasting or giant verruca vulgaris as well as UV radiation can contribute to the development for neoplastic transformation.Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5
Fig. 1.
Well-demarcated warty surface mass over the left lateral canthus.
Fig. 2.
Enlarged painful warty mass surrounded by erythematous skin changes over the lateral canthus.
Fig. 3.
Rotational flap from the left supra-brow skin and the skin graft from the supraclavicular region were used for the wound closure.
Fig. 4.
Histological features of squamous cell carcinoma with invasion of 1.5mm in depth.
Fig. 5.
Microscopic focus of basal cell carcinoma (Microsopic power 100x).
4. Conclusion
This is the first case in our knowledge to demonstrate the oncogenic potential of verruca vulgaris into the combination of squamous cell carcinoma and basal cell carcinoma within one lesion. Size, chronicity and UV radiation may increase the risk of malignancy. Early surgical excision should be considered in chronic verruca vulgaris involving eyelids.
Patient consent
Written consent for the publication of this case was obtained from patient's legal guardian.
Funding
No funding or grant support
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship:
Declaration of competing interest
The following authors have nothing to disclosure: KKH Lai, HL Li, STC Ko, E Chan.
Acknowledgements
None.
References
- 1.Grayson W. Infectious diseases of the skin. In: Calonje E., Brenn T., Lazar A., Mckee P., editors. Mckee's Skin Pathology with Clinical Correlations. fourth ed. Elsevier; Toronto: 2012. pp. 760–895. [Google Scholar]
- 2.Cardoso J.C., Calonje E. Cutaneous manifestations of human papillomaviruses: a review. Acta Dermatovenerol Alpina Pannonica Adriatica. 2011 Sep;20(3):145–154. [PubMed] [Google Scholar]
- 3.Grayson W. Infectious diseases of the skin. In: Calonje E., Brenn T., Lazar A., Mckee P., editors. Mckee's Skin Pathology with Clinical Correlations. fourth ed. Elsevier; Toronto: 2012. pp. 760–895. [Google Scholar]
- 4.Daugherty M., Byler T. Genital wart and human papillomavirus prevalence in men in the United States from penile swabs: results from national health and nutrition examination surveys. Sex Transm Dis. 2018;45(6):412–416. doi: 10.1097/OLQ.0000000000000761. [DOI] [PubMed] [Google Scholar]
- 5.Noel J.C., Detremmerie O., Peny M.O. Transformation of common warts into squamous cell carcinoma on sun-exposed areas in an immunosuppressed patient. Dermatology. 1994;189(3):308–311. doi: 10.1159/000246869. [DOI] [PubMed] [Google Scholar]
- 6.Shelley W.B., Wood M.G. Transformation of the common wart into squamous cell carcinoma in a patient with primary lymphedema. Cancer. 1981;48(3):820–824. doi: 10.1002/1097-0142(19810801)48:3<820::aid-cncr2820480325>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 7.Al Aboud A.M., Nigam P.K. StatPearls Publishing; Treasure Island (FL): 2019. Wart (Plantar, Verruca Vulgaris, Verrucae) May 13. StatPearls [Internet] [Google Scholar]
- 8.Ergün S.S., Su O., Büyükbabaný N. Giant verruca vulgaris. Dermatol Surg. 2004;30(3):459–462. [PubMed] [Google Scholar]
- 9.Goette D.K. Carcinoma in situ in verruca vulgaris. Int J Dermatol. 1980;19(2):98–101. doi: 10.1111/j.1365-4362.1980.tb00263.x. [DOI] [PubMed] [Google Scholar]
- 10.Satter E.K., Metcalf J., Lountzis N. Tumors composed of malignant epithelial and melanocytic populations: a case series and review of the literature. J Cutan Pathol. 2009;36:211–219. doi: 10.1111/j.1600-0560.2008.01000.x. [DOI] [PubMed] [Google Scholar]
- 11.Boyd A.S., Rapini R.P. Cutaneous collision tumors. An analysis of 69 cases and review of the literature. Am J Dermatopathol. 1994;16(3):253–257. [PubMed] [Google Scholar]
- 12.Tan C.Z., Rieger K.E., Sarin K.Y. Basosquamous carcinoma: controversy, advances, and future directions. Dermatol Surg. 2017;43(1):23–31. doi: 10.1097/DSS.0000000000000815. [DOI] [PubMed] [Google Scholar]
- 13.Ahlgrimm-Siess V., Hofmann-Wellenhof R., Zalaudek I. Collision of malignant melanoma (lentigo maligna type) with squamous cell carcinoma in solar-damaged skin of the face. Dermatol Surg. 2007;33:122–124. doi: 10.1111/j.1524-4725.2007.33023.x. [DOI] [PubMed] [Google Scholar]
- 14.Ma'luf R.N. Treatment of recurrent eyelid margin verruca vulgaris with mitomycin C. Ophthalmic Plast Reconstr Surg. 2010;26(3):214–215. doi: 10.1097/IOP.0b013e3181b9e73e. [DOI] [PubMed] [Google Scholar]