Key Points
Question
Are there differences in functional outcomes between early and late intervention for intubation-related laryngeal injury?
Findings
In this cohort study of 29 patients with laryngeal injury resulting from endotracheal intubation, early intervention for acute laryngeal injury after intubation was associated with fewer surgical procedures, a shorter duration of tracheostomy dependence, and restored laryngeal function without requiring open reconstruction compared with patients treated with late intervention.
Meaning
Early intervention in laryngeal injury after intubation may disrupt the natural course of this disease, minimize fibrotic scar formation, and limit long-term physiological impairment.
Abstract
Importance
Patients with laryngeal injury after endotracheal intubation often present long after initial injury with mature fibrosis compromising cricoarytenoid joint mobility and glottic function.
Objective
To compare functional outcomes between early and late intervention for intubation-related laryngeal injury.
Design, Setting, and Participants
This retrospective cohort study involved 29 patients with laryngeal injury resulting from endotracheal intubation who were evaluated at a tertiary care center between May 1, 2014, and June 1, 2018. Ten patients with intubation injury to the posterior glottis who received early treatment were compared with 19 patients presenting with posterior glottic stenosis who received late treatment. Statistical analysis was performed from May 1 to July 1, 2019.
Exposures
Early intervention, defined as a procedure performed 45 days or less after intubation, and late treatment, defined as an intervention performed greater than 45 days after intubation.
Main Outcomes and Measures
Patient-specific and intervention-specific covariates were compared between the 2 groups, absolute differences with 95% CIs were calculated, and time to tracheostomy decannulation was compared using log-rank testing.
Results
The 2 groups had similar demographic characteristics and a similar burden of comorbid disease. Ten patients who received early intervention (7 women [70%]; median age, 59.7 years [range, 31-72 years]; median, 34.7 days to presentation [IQR, 1.5-44.8 days]) were compared with 19 patients who received late intervention (11 women [58%]; median age, 53.8 years [range, 34-73 years]; median, 341.9 days to presentation [IQR, 132.7-376.3 days]). Nine of 10 patients (90%) who received early intervention and 11 of 19 patients (58%) who received late interventions were decannulated at last follow-up (absolute difference, 32%; 95% CI, −3% to 68%). Patients who received early treatment required fewer total interventions than patients with mature lesions (mean, 2.2 vs 11.5; absolute difference, 9.3; 95% CI, 6.4-12.1). In addition, none of the patients who received early treatment required an open procedure, whereas 17 patients (90%) with mature lesions required open procedures to pursue decannulation.
Conclusions and Relevance
This study suggests that early intervention for patients with postintubation laryngeal injury was associated with a decreased duration of tracheostomy dependence, a higher rate of decannulation, and fewer surgical procedures compared with late intervention. Patients who underwent early intervention also avoided open reconstruction. These findings may bear relevance to the management of patients requiring extended durations of endotracheal intubation during recovery for critical illness related to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
This cohort study compares functional outcomes between early and late intervention for patients with intubation-related laryngeal injury.
Introduction
Worldwide, 13 million to 20 million patients are intubated in intensive care units each year.1 Prior studies have shown that up to 57% of patients intubated for more than 12 hours show evidence of acute laryngeal injury after extubation.1,2,3 Acute laryngeal injury is associated with worse patient-reported breathing and vocal symptoms as compared with patients without acute laryngeal injury. Although past studies have centered on defining the prevalence of acute laryngeal injuries after prolonged intubation,4,5,6 to our knowledge, little work has focused on early treatment strategies to mitigate the long-term complications of acute laryngeal injuries.
A widely accepted pathophysiological mechanism7 supported by case reports photodocumenting the development of posterior glottic stenosis after intubation injury8 proposes that intubation injuries in the larynx occur when the endotracheal tube is forced against the posterior glottis by the vector force of the tongue base.8,9 Direct pressure to the abutting laryngeal mucosa leads to ulceration with associated formation of hypertrophic granulation tissue.2 Animal models demonstrate that the laryngeal injury undergoes a rapid infiltration of inflammatory cells, followed by neovascularized granulation tissue, and subsequently progresses to mature fibrosis.2,8,9,10,11 Left untreated, acute laryngeal injury can result in posterior glottic stenosis with restricted glottic mobility and impaired ventilation. The development of posterior glottic stenosis often requires tracheostomy and extensive long-term surgical management.12 Both posterior glottic stenosis and its treatment can significantly affect quality of life.10,13
Postintubation laryngeal injury is a clinical challenge in part because patients commonly present to the otolaryngologist late in the disease course. Subjective dyspnea or an inability to tolerate decannulation commonly occurs 8 to 12 weeks after the inciting intubation event as the acute tissue injury progresses to mature fibrosis.14 Occasionally, however, patients may be referred while still in the acute phase of disease, when there is evolving mucosal ulceration or granulation tissue that may be amenable to endoscopic interventions to minimize the full progression of disease. Prior work by Nouraei et al14,15 demonstrated that early endoscopic management of postintubation tracheal stenosis (involving intralesional corticosteroid injection, removal of granulation tissue, and balloon dilation) decreased the number of interventions and increased the number of intervention-free intervals. In this study, we investigated whether a similar benefit could be obtained when applying the principles from the tracheal work by Nouraei et al14,15 to laryngeal injuries arising after endotracheal intubation. We prospectively compared functional outcomes between early (≤45 days from the inciting injury) and late intervention (>45 days from the inciting injury) for intubation-related laryngeal injury.
Methods
Study Design and Comparator Groups
This retrospective cohort study involved 29 adult patients who sustained injury to the posterior laryngeal mucosa after endotracheal intubation. This study was performed in accordance with the Declaration of Helsinki16 and Good Clinical Practice and was approved by the Vanderbilt University Medical Center Institutional Review Board, who waived the requirement for written or oral consent given the minimal risk and nature of the deidentified data collected. Given the data from animal models and clinical observation that postintubation injuries to the posterior glottic mucosa frequently require 90 days to progress to mature fibrosis, we defined early intervention as a procedure 45 days or less after intubation and late treatment as an intervention greater than 45 days after initial injury.
Study Population Data
Ten patients with acute injuries to the posterior laryngeal mucosa and 19 patients with mature posterior glottic stenosis were evaluated between May 1, 2014, and June 1, 2018. Within our institution, patients with suspected acute laryngeal injury are identified via symptoms assessed by the critical care team (dysphonia and stridor) or evidence on physical examination of acute laryngeal injury visualized on endoscopic assessment (obtained in routine care as part of postextubation swallowing assessment). Patients with mature scarring were referred as outpatient consultations to our center for complex airway reconstruction. Prior to referral, no patients received other airway interventions apart from tracheostomies. Demographic information and medical comorbidities were recorded for each patient. Data collected on medical comorbidities were used to calculate the Charlson Comorbidity Index.17
Surgical Technique
Early Intervention
Patients’ airways were comanaged by the anesthesia and the surgical teams during induction of anesthesia using an oral mask. Patients received intravenous anesthesia consisting of propofol combined with a muscle relaxant. After glottic exposure was achieved with a laryngoscope, intermittent supraglottic jet ventilation was used to maintain oxygen saturation.
Interventions for acute lesions followed 3 broad principles: (1) fresh granulation tissue, if left in situ, may form a mature fibrotic scar; (2) necrotic posterior glottic mucosa serves as a nidus for chronic sustained inflammation (similar to burn eschar) and should be removed; and (3) a local corticosteroid injection may help arrest the active inflammatory infiltrate. These 3 principles were applied via gentle debridement of exophytic granulation tissue; devitalized mucosa (commonly encountered as white eschar) was trimmed back to bleeding, viable tissue using an operating microscope and microlaryngeal instrumentation; and the mucosa adjacent to the cricoarytenoid joint capsule was injected bilaterally with corticosteroids (triamcinolone acetonide) using a microlaryngeal injector (Xomed Ltd). These intralesional injections were performed primarily at the base of the lesions in a submucosal plane. The CRE Pulmonary Balloon Dilator (Boston Scientific) was used in an attempt to facilitate submucosal drug diffusion. Great care was taken to preserve healthy mucosa and avoid iatrogenic trauma to the true vocal fold mucosal cover.
Late Intervention
Patients with mature lesions of the larynx initially underwent operative diagnostic endoscopy to facilitate anatomical staging of their airway disease. Assessments followed modified criteria from the European Laryngological Society consensus statement.18 Patients with posterior glottic stenosis were then initially treated with incision of the posterior cicatrix with a sickle knife combined with a corticosteroid injection adjacent to the cricoarytenoid joint capsule followed by balloon dilation using the CRE Pulmonary Balloon Dilator to promote submucosal drug diffusion and cicatricial release.
If the initial endoscopic procedure failed to restore glottic mobility, subsequent surgical operations were classified as cordotomy or total arytenoidectomy, extended cricotracheal resection (with concomitant posterior costal cartilage graft), tracheoplasty, or laryngotracheal reconstruction. Laryngotracheal reconstructions were further categorized as open posterior costal cartilage graft or endoscopic posterior costal cartilage graft. According to guiding principles beyond the scope of this discussion, the type of airway reconstruction was matched with the patient’s pathologic characteristics to maximize airway improvement while minimizing surgical morbidity.19,20,21
Outcome Measures
We compared the time to decannulation and the rate of decannulation among patients with early vs late intervention for intubation-related posterior glottic injury. In addition, we recorded the total number of endoscopic and open reconstructive procedures that patients underwent during the study period.
Statistical Analysis
Statistical analysis was performed from May 1 to July 1, 2019. Data were presented as mean (SE) values or percentages. Absolute differences (ADs) with 95% CIs were calculated for each patient characteristic or exposure. Statistical analyses were conducted using Stata, version 16.1 (StataCorp LLC). Time to decannulation was illustrated using the Kaplan-Meier method and compared using log-rank statistics.
Results
Ten patients who received early intervention (median, 34.7 days to presentation; IQR, 1.5-44.8 days) were compared with 19 patients who received late intervention (median, 341.9 days to presentation; IQR, 132.7-376.3 days). A total of 7 patients (70%) who received early intervention were female vs 11 patients (58%) who received late intervention (AD, 12%; 95% CI, −25% to 49%) (Table). The median ages of patients were similar in both groups (early, 59.7 years [range, 31-72 years] vs late, 53.8 years [range, 34-73 years]; AD, 6%; 95% CI, −32% to 44%). The patients also had a similar burden of comorbid medical illness (Charlson Comorbidity Index: early, 1.4 vs late, 1.7; AD; 0.3; 95% CI, −1.5 to 0.7). The grading of the severity of the postintubation laryngeal injury for patients who received early treatment is presented in the eTable in the Supplement. Given the nature of outside hospital referral for patients presenting with mature glottic lesions, we were unable to document the grade of their initial postintubation injury severity.
Table. Patient, Injury, and Treatment Characteristics.
| Characteristic | Early (n = 10) | Late (n = 19) | Absolute difference (95% CI) |
|---|---|---|---|
| Demographic characteristics | |||
| Age, median (range), y | 59.7 (31-72) | 53.8 (34-73) | 5.9 (−32.1 to 43.9) |
| Female, No (%) | 7 (70) | 11 (58) | 12 (−25 to 49) |
| Charlson Comorbidity Index | 1.38 | 1.68 | 0.30 (−1.48 to 0.71) |
| Injury characteristics | |||
| Posterior glottic stenosis, No. (%) | 10 (100) | 19 (100) | NA |
| Tracheostomy prior to surgery, No. (%)a | 7 (70) | 16 (84) | 14 (−45 to 17) |
| Intervention characteristics | |||
| Interventions, mean (SD), No. | 2.2 (1.6) | 11.5 (5.9) | 9.3 (6.4 to 12.1) |
| Open procedures, No. (%) | 0 | 17 (90) | NA |
| Time to decannulation, mean (SD), d | 54.1 (26) | 154.9 (64.5) | 100.8 (47.8 to 153.8) |
| Time to first intervention, d | 34.7 | 341.9 | 307.2 (124.4 to 523.3) |
| Length of follow-up, d | 121.4 | 179.4 | 53.4 (−48.4 to 155.3) |
Abbreviation: NA, not applicable.
Prior to surgical intervention for posterior glottic stenosis.
The most prevalent indication for intubation and mechanical ventilation for patients who received early treatment (7 [70%]) and for those who received late treatment (8 [42%]) was trauma (motor vehicle accidents and burns). In addition, the proportion of patients who received tracheostomies prior to surgical interventions was not different between the early and late treatment cohorts (7 [70%] vs 16 [84%]; AD, 14%; 95% CI, −45% to 17%). Nine of 10 patients in the early treatment group and all 19 patients treated late required a tracheostomy at some point during their disease course.
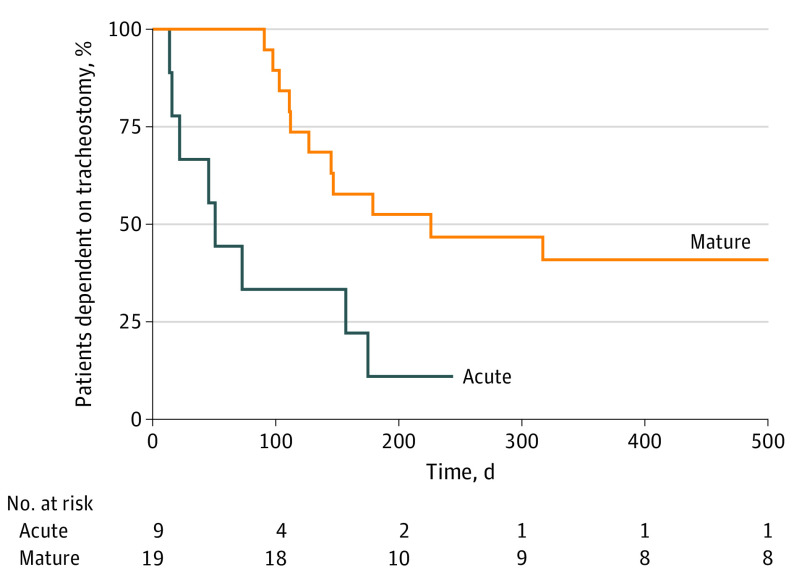
The mean (SD) time from initial intervention to tracheostomy decannulation was significantly shorter for patients who received early treatment (54.1 [26] vs 154.9 [64.5] days; AD, 101 days; 95% CI, 48-154) (Figure; Table). Nine patients (90%) who received early intervention and 11 patients (58%) who received late interventions were decannulated at last follow-up (AD, 32%; 95% CI, −3% to 68%).
Figure. Kaplan-Meier Analysis of the Time From First Intervention to Tracheostomy Decannulation Between the Early (Acute) and Late (Mature) Intervention Groups.
Kaplan-Meier analysis of the time from first intervention to tracheostomy decannulation between the acute and mature intervention groups. Time measured from first intervention to treat posterior glottic injury. Log-rank test comparing mature vs acute Intervention (hazard ratio, 3.15; 95% CI, 0.91-10.82).
Patients who received early treatment required fewer total interventions than patients with mature lesions (mean [SD], 2.2 [1.6] vs 11.5 [5.9]; AD, 9.3; 95% CI, 6.4-12.1). In addition, none of the patients who received early treatment required an open procedure, whereas 17 patients (90%) with mature lesions required open procedures to pursue decannulation.
Discussion
Early endoscopic intervention for acute laryngeal injury after intubation was associated with fewer surgical interventions, a shorter duration of tracheostomy dependence, and restored laryngeal function without requiring open reconstruction compared with late intervention. Acute laryngeal injury after intubation is characterized by mucosal ulceration and perichondritis, which then proceeds to the development of granulation tissue. Mature laryngeal stenosis occurs when the granulation tissue is replaced by fibrotic scar tissue, leading to contracture of the initial injury and narrowing of the airway lumen.22,23 Our results suggest that early intervention in laryngeal injury may disrupt the natural course of this disease, minimize fibrotic scar formation, and limit long-term physiological impairment. These findings are consistent with those of Nouraei et al,14,15 who found that acute tracheal injury secondary to prolonged endotracheal intubation was more successfully treated when interventions occurred early in the disease course.
The management of mucosal injury after endotracheal intubation has assumed heightened importance with the recent coronavirus disease 2019 (COVID-19) pandemic owing to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).24 Early clinical reports suggest that the length of intensive care unit stay for patients with COVID-19 appears to be long, with many patients remaining intubated for 7 to 14 days.25 Emerging data will be necessary to guide decisions about the timing and safety of interventions after critical illness related to COVID-19.
Taken together with the findings of Nouraei et al,14,15 our results suggest that more focus should be placed on timely diagnosis and intervention of acute airway injuries after intubation. A prospective cohort study demonstrated that most patients who were intubated for more than 12 hours experienced some form of acute laryngeal injury.3 These injuries are associated with a higher prevalence of respiratory and vocal complications compared with their uninjured counterparts. Early endoscopic interventions may seek to address these injuries when they are identified in a timely manner. Future studies should explore the utility of formalized screening protocols for high-risk patients with significant comorbid illness, prolonged intubation, or extended dyspnea after extubation.
Limitations
This study has some limitations. The chief limitations relate to the observational nature of our data and the differing time to presentation between the 2 patient cohorts. In addition, our project did not explore data on deglutitive function after laryngeal injury for endotracheal intubation. Future studies examining the association of intubation with long-term laryngeal function will require assessment of dysphagia (either via validated patient-reported outcome measures or instrumental examinations) to provide a comprehensive portrait of the survivorship experiences after critical illness. In addition, the nature of regional referral from outside our institution also precluded a direct comparison of the characteristics of the inciting intubations (eg, the size of endotracheal tube and the duration of intubation). These factors affected our ability to compare the severity of laryngeal injury between the 2 groups. Because patients in the late treatment group present much later in their course of disease, the severity of their initial injuries is impossible to ascertain. The superior results in the early treatment group may reflect a less severe grade of disease. In a similar vein, patients with mature injury may have other confounding variables secondary to long-term tracheostomy, which can complicate the decannulation process compared with the early group.
Although well-documented case reports illustrate the potential for acute injuries to develop into chronic fibrotic stenosis in the posterior glottis,8 it remains theoretically possible that some injuries may resolve regardless of intervention. However, a recent prospective observational study of a large cohort of critically ill patients after intubation demonstrated that acute laryngeal injury occurs in more than half of patients who receive mechanical ventilation and is associated with significantly worse breathing 10 weeks after extubation.3 These results support the idea that many acute injuries do not completely resolve and instead significantly affect functional recovery from critical illness.
Despite these limitations, our results show excellent long-term functional outcomes with low perioperative risk with early intervention. Traditionally, mature laryngeal fibrosis (posterior glottic stenosis) has proved to be a recalcitrant clinical entity, with all treatment options requiring imperfect compromises between voicing, breathing, and swallowing.13 Although our work does not provide definitive proof of the superior effectiveness of early intervention, it does offer evidence supporting future multi-institutional efforts to rigorously address this question.
Conclusions
Early intervention in postintubation laryngeal injury was associated with a decreased duration of tracheostomy dependence, higher rate of decannulation, and required fewer surgical procedures compared with patients treated with late intervention. Patients who underwent early intervention also avoided open reconstruction. These findings may bear relevance to the management of patients requiring an extended duration of endotracheal intubation during recovery for critical illness related to SARS-CoV-2 infection.
eTable. Grading Assessment of Injury Severity in Patients With Acute Injury
References
- 1.Brodsky MB, Levy MJ, Jedlanek E, et al. Laryngeal and upper airway symptoms and injury following endotracheal intubation: a systematic review. Am J Respir Crit Care Med. 2017:195:A1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Colton House J, Noordzij JP, Murgia B, Langmore S. Laryngeal injury from prolonged intubation: a prospective analysis of contributing factors. Laryngoscope. 2011;121(3):596-600. doi: 10.1002/lary.21403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shinn JR, Kimura KS, Campbell BR, et al. Incidence and outcomes of acute laryngeal injury after prolonged mechanical ventilation. Crit Care Med. 2019;47(12):1699-1706. doi: 10.1097/CCM.0000000000004015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pandharipande PP, Girard TD, Jackson JC, et al. ; BRAIN-ICU Study Investigators . Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306-1316. doi: 10.1056/NEJMoa1301372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bulic D, Bennett M, Rodgers H, et al. Delirium after mechanical ventilation in intensive care units: the Cognitive and Psychosocial Assessment (CAPA) Study protocol. JMIR Res Protoc. 2017;6(2):e31. doi: 10.2196/resprot.6660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whited RE. Posterior commissure stenosis post long-term intubation. Laryngoscope. 1983;93(10):1314-1318. doi: 10.1002/lary.1983.93.10.1314 [DOI] [PubMed] [Google Scholar]
- 7.Gaynor EB, Greenberg SB. Untoward sequelae of prolonged intubation. Laryngoscope. 1985;95(12):1461-1467. doi: 10.1288/00005537-198512000-00005 [DOI] [PubMed] [Google Scholar]
- 8.Howard NS, Shiba TL, Pesce JE, Chhetri DK. Photodocumentation of the development of type I posterior glottic stenosis after intubation injury. Case Rep Surg. 2015;2015:504791. doi: 10.1155/2015/504791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Courey MS, Bryant GL Jr, Ossoff RH. Posterior glottic stenosis: a canine model. Ann Otol Rhinol Laryngol. 1998;107(10, pt 1):839-846. doi: 10.1177/000348949810701005 [DOI] [PubMed] [Google Scholar]
- 10.Lano CF Jr, Duncavage JA, Reinisch L, Ossoff RH, Courey MS, Netterville JL. Laryngotracheal reconstruction in the adult: a ten year experience. Ann Otol Rhinol Laryngol. 1998;107(2):92-97. doi: 10.1177/000348949810700202 [DOI] [PubMed] [Google Scholar]
- 11.Sinha R, Correia R, Gardner D, et al. Mucosal injury following short-term tracheal intubation: a novel animal model and composite tracheal injury score. Laryngoscope Investig Otolaryngol. 2018;3(4):257-262. doi: 10.1002/lio2.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nouraei SAR, Heathcote KJ. A patient-centred multidomain instrument for improving the clarity of outcomes reporting and documentation in complex airway surgery. Clin Otolaryngol. 2018;43(6):1634-1639. doi: 10.1111/coa.13114 [DOI] [PubMed] [Google Scholar]
- 13.Hillel AT, Karatayli-Ozgursoy S, Samad I, et al. ; North American Airway Collaborative (NoAAC) . Predictors of posterior glottic stenosis: a multi-institutional case-control study. Ann Otol Rhinol Laryngol. 2016;125(3):257-263. doi: 10.1177/0003489415608867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nouraei SAR, Singh A, Patel A, Ferguson C, Howard DJ, Sandhu GS. Early endoscopic treatment of acute inflammatory airway lesions improves the outcome of postintubation airway stenosis. Laryngoscope. 2006;116(8):1417-1421. doi: 10.1097/01.mlg.0000225377.33945.14 [DOI] [PubMed] [Google Scholar]
- 15.Nouraei SAR, Ghufoor K, Patel A, Ferguson T, Howard DJ, Sandhu GS. Outcome of endoscopic treatment of adult postintubation tracheal stenosis. Laryngoscope. 2007;117(6):1073-1079. doi: 10.1097/MLG.0b013e318050ca12 [DOI] [PubMed] [Google Scholar]
- 16.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 17.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 18.Monnier P, Dikkers FG, Eckel H, et al. Preoperative assessment and classification of benign laryngotracheal stenosis: a consensus paper of the European Laryngological Society. Eur Arch Otorhinolaryngol. 2015;272(10):2885-2896. doi: 10.1007/s00405-015-3635-4 [DOI] [PubMed] [Google Scholar]
- 19.Hartley BEJ, Cotton RT. Paediatric airway stenosis: laryngotracheal reconstruction or cricotracheal resection? Clin Otolaryngol Allied Sci. 2000;25(5):342-349. doi: 10.1046/j.1365-2273.2000.00399.x [DOI] [PubMed] [Google Scholar]
- 20.Inglis AF Jr, Perkins JA, Manning SC, Mouzakes J. Endoscopic posterior cricoid split and rib grafting in 10 children. Laryngoscope. 2003;113(11):2004-2009. doi: 10.1097/00005537-200311000-00028 [DOI] [PubMed] [Google Scholar]
- 21.Boardman SJ, Albert DM. Single-stage and multistage pediatric laryngotracheal reconstruction. Otolaryngol Clin North Am. 2008;41(5):947-958, ix. doi: 10.1016/j.otc.2008.04.002 [DOI] [PubMed] [Google Scholar]
- 22.Gelbard A, Francis DO, Sandulache VC, Simmons JC, Donovan DT, Ongkasuwan J. Causes and consequences of adult laryngotracheal stenosis. Laryngoscope. 2015;125(5):1137-1143. doi: 10.1002/lary.24956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stauffer JL, Olson DE, Petty TL. Complications and consequences of endotracheal intubation and tracheotomy: a prospective study of 150 critically ill adult patients. Am J Med. 1981;70(1):65-76. doi: 10.1016/0002-9343(81)90413-7 [DOI] [PubMed] [Google Scholar]
- 24.Guan WJ, Ni ZY, Hu Y, et al. ; China Medical Treatment Expert Group for Covid-19 . Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. doi: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grasselli G, Zangrillo A, Zanella A, et al. ; COVID-19 Lombardy ICU Network . Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574-1581. doi: 10.1001/jama.2020.5394 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Grading Assessment of Injury Severity in Patients With Acute Injury