Abstract
Sexism has been an issue in bleeding disorders for centuries. Women with bleeding disorders have been underrecognized and underdiagnosed. Those who are diagnosed often experience delays in diagnosis and feel that their symptoms are dismissed or minimized. Several factors contribute to this sexism. Historically, the clinical and research focus within the bleeding disorder community has been on men and hemophilia. Von Willebrand disease, a disease that has long been recognized as affecting women, is much more common than hemophilia, yet has significantly fewer resources devoted to it. The lack of knowledge and comfort that patients and health care providers have regarding menstruation compounds the issue, as heavy menstrual bleeding is one of the most common symptoms seen in women with bleeding disorders. Stemming from the universal stigmatization of periods, this lack of comfort and knowledge results in fewer women seeking care, fewer health care providers addressing the issue, and fewer women getting the care they deserve. Progress has been made, with many organizations dedicating resources to improving the care of these women. The road is long, and much more work is needed to ensure that women with bleeding disorders receive the care they deserve.
Keywords: hemophilia A, menstruation, sexism, von Willebrand disease, women
Essentials.
Sexism is a long‐standing issue in bleeding disorders (BDs), leading to inequity for affected women.
Clinical and research focus within bleeding disorders has been on men and hemophilia.
Stigmatization of menstruation leads to decreased awareness and inadequate care.
Women with BDs are underrecognized, underdiagnosed, and undertreated.
Sexism has been an issue in bleeding disorders for centuries, leading to inequity for affected women (see Figure 1). The first description of the genetic basis of hemophilia came in 1820, with Nasse’s law—“hemophilia is transmitted entirely by unaffected females to their sons” 1 —conveniently without mention of how that transmission continued from those sons to their daughters. This sentiment was echoed in this statement published in the Lancet in 1886: “It may be almost said that the females hand down the disease while the males are the victims of it.” 2 Placing the responsibility solely on females is even more striking given that male sons of carriers have a 50% chance of being affected versus 100% of the daughters of affected men. The earliest case in the literature of a woman with hemophilia was in 1923 and describes a woman diagnosed in middle age. At the age of 10, she was found unconscious following a tooth extraction and required a 3‐week hospitalization and had multiple subsequent hemorrhagic episodes. Despite this impressive bleeding history, the authors remark that her case fell into the category of “an abnormal tendency to bleed in female members of admitted haemophiliac families, such tendency being slight or atypical as compared with well‐marked hemophilia.” 3 It would be another 25 years before another case was described.
Figure 1.
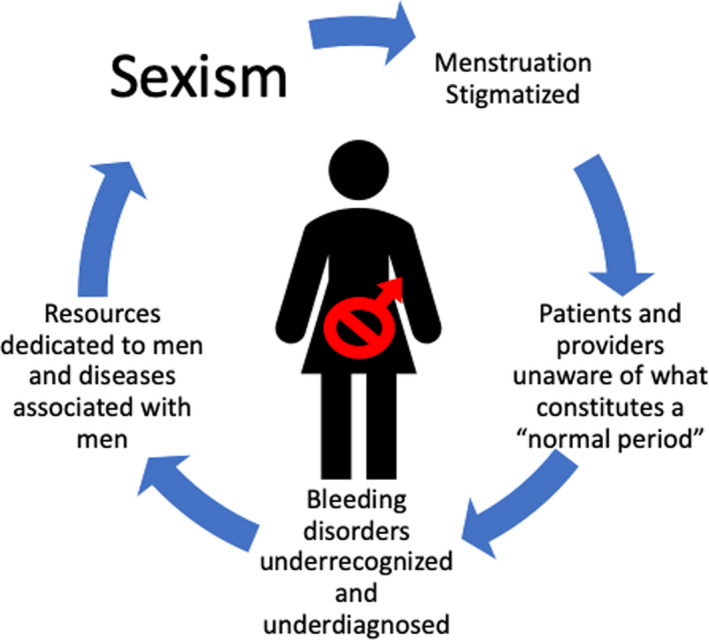
Cycle of sexism in the management of bleeding disorders.
Given its X‐linked inheritance, historically it has been taught that hemophilia is a disease that affects males, with females being asymptomatic carriers. However, there are multiple ways for women to be affected. In females carrying a single mutation, expression of factor is dependent on cellular mosaicism, based on the phenomenon of X inactivation (Lyonization). 4 If a predominance of cells expresses the mutated X chromosome, factor levels will be proportionately low. Severe and moderate hemophilia can be seen in women secondary to homozygosity, compound heterozygosity, extreme Lyonization, or aberrations in the X chromosome. 4 More commonly, women demonstrate mild deficiencies secondary to slight skewing toward the mutated chromosome. An important complicating factor is that the bleeding tendency in hemophilia carriers does not correlate well with factor level, and abnormal bleeding has been documented in carriers with normal levels. 5 Despite these data, many carriers feel that their symptoms are dismissed and that this language enables neglect. 6 The first formal recognition that women could in fact carry a diagnosis of hemophilia came in 2012 when the World Federation of Hemophilia updated its definitions, stating that hemophilia occurs in males and females. 7 This was followed in 2018 by the International Society on Thrombosis and Haemostasis (ISTH) guidelines stating that if a female carrier had factor VIII levels < 40, they should be considered as having hemophilia. 8 Unfortunately, that same year, in a special issue focused on women, this statement was found: “Bleeding disorders are typically sex specific: some, such as classical hemophilia, occur only in men.” 9 To this day, the Centers for Disease Control and Prevention website states that “a female who is a carrier sometimes can have symptoms of hemophilia. In fact, some doctors describe these women as having mild hemophilia.” 10 The specific terminology used is important, as many women feel that the carrier label is dismissive and invalidates their symptoms and experience. 11
Given this, it is not surprising that hemophilia in women is underrecognized and underdiagnosed. For every man with hemophilia, there are ~ 1.5 female somatic carriers, and approximately one‐third of these will have low factor levels. As such, women should make up approximately 30% of patients with hemophilia, yet the latest report from the World Federation of Hemophilia included only 3.5% women. 9 In addition to underdiagnosis, there are also significant delays in diagnosis even in those most severely affected. Women with moderate and severe hemophilia have delays in diagnosis of 6.5 months and 39 months, respectively, compared to men, despite similar symptoms and age at first bleed. 12
Sexism is similarly seen in the treatment of von Willebrand disease (VWD). Menses and postpartum bleeding render more females symptomatic with VWD, yet they also suffer from underrecognition and delayed diagnosis. While 76% of males with VWD are diagnosed by 10 years of age, 50% of females are not diagnosed by 12 years of age. 13 This is particularly problematic, as heavy menstrual bleeding is the most common symptom seen in females with VWD, and a delayed diagnosis does not allow for anticipatory guidance around menarche and normal menses. On average, women with VWD experience a 16‐year delay between symptom onset and diagnosis and report six bleeding symptoms before diagnosis. 13
The primary clinical and research focus in the bleeding disorders community has also historically been on males and hemophilia. VWD and rare bleeding disorders, which historically have been recognized as affecting women, have lagged significantly behind. A search for VWD, which is at least 10 times more common than hemophilia A (HA) and hemophilia B (HB) combined, returns 12 652 PubMed indexed citations, compared to 22 499 for HA and 5280 for HB. This discrepancy is similarly reflected in the number of open and completed trials listed on clinicaltrials.gov (27 and 33 for VWD, 173 and 357 for HA, 67 and 148 for HB) and the number of currently approved products in the United States (4 for VWD, 17 for HA, and 8 for HB).
The lack of knowledge and comfort that patients and physicians have discussing menstruation is a major contributor to these problems. Periods have been stigmatized across cultures for centuries. In ancient Rome, it was said that “if the menstrual discharge coincides with an eclipse of the moon or sun, the evils resulting from it are irremediable; and no less so, when it happens while the moon is in conjunction with the sun; the congress with a woman at such a period being noxious, and attended with fatal effects to the man. 14 ” In ancient Greece, missed menses were thought to lead to blood accumulation around the heart and a wandering uterus, leading to erratic behavior or hysteria (the Greek word for uterus). 15 Major religions refer to menstruating women as unclean and suggest segregation during menses. 16 And little progress has been made in fighting this stigma. An online international survey in 2017 of >10 000 men and women between the ages of 13 and 50 revealed that 37% had never seen periods depicted in popular culture, 49% felt that there was stigma attached to periods, and 56% would rather be bullied than talk about periods. 17 Further, 41% of parents with daughters had never had a discussion about menstruation. 18
Given this universal stigma, it is not surprising that only 4 of 10 women experiencing heavy menstrual bleeding will seek care for it. 19 Patients and clinicians alike may be unaware of what constitutes normal menstrual cycles. 20 Physicians often fail to elicit detailed information on menses, with <10% of pediatricians and family medicine physicians documenting a full menstrual history during well adolescent female visits. 17 Adolescents most commonly learn about menstruation from their mothers so this problem is compounded in families with VWD where very abnormal bleeding patterns may in fact be normalized. Research is lacking, with a PubMed search for “menstruation” revealing < 4000 publications per decade over the past 3 decades, compared to almost 15 000 over the past decade for “semen.” 21 Untreated heavy menstrual bleeding frequently leads to iron deficiency and anemia, as well as decreased quality of life.
Despite continued sexism in the diagnosis and treatment of bleeding disorders, there are reasons to be hopeful for the future. Organizations like the National Hemophilia Foundation, HemAware, Hemophilia Ontario, Hemophilia Federation of America, and many others now have dedicated programming focused on women with bleeding disorders. The Foundation for Women and Girls With Blood Disorders was started in 2010, started a dedicated grant program in 2016, and had their inaugural conference this year. LetsTalkPeriod.ca was created in 2016 and aims to increase awareness around the signs and symptoms of bleeding disorders and includes a self‐administered bleeding assessment tool to help guide patients to the help they need. In 2018, The Hemophilia Foundation of Michigan hosted the inaugural National Conference for Women With Hemophilia, aptly named “Being Visible: Hear Our Voices.” That same year, the gynecologic health and disease branch of the National Institute of Child Health and Human Development convened a meeting to “identify gaps and opportunities in menstruation science and to raise awareness of the need for more research in this field.” 21 And on International Women’s Day in 2019, United Nations experts put out a call to break the taboo around menstrual health. Looking ahead, there is much more work to be done. There is a critical need for increasing education and awareness, of health care providers as well as patients, dedicated research funding to further our currently limited understanding, and significant resource investment to improve the care of these women. They deserve no less.
RELATIONSHIP DISCLOSURE
The authors have no conflicts of interest to disclose.
AUTHOR CONTRIBUTIONS
ACW and PDJ conceived of the original idea for the manuscript, ACW conducted a literature review and wrote the initial draft, and PDJ made substantial edits and revisions.
Weyand AC, James PD. Sexism in the management of bleeding disorders. Res Pract Thromb Haemost.2021;5:51–54. 10.1002/rth2.12468
Handling Editor: Dr Cihan Ay.
Contributor Information
Angela C. Weyand, Email: acweyand@med.umich.edu, @acweyand.
Paula D. James, @james_paulad.
REFERENCES
- 1. Nasse CF. Von einer erblichen Neigung zu tödlichen Blutungen [From a hereditary propensity to fatal bleeding]. Arch Med Erfahrungen. 1820;C:385–434. [Google Scholar]
- 2. Treves F. London hospital: a case of haemophilia: a pedigree through five generations. Lancet. 1886;128:533–4. [Google Scholar]
- 3. Warde M. Haemophilia in the female. Br Med J. 1923;6(2):599–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. d'Oiron R, O'Brien S, James AH. Women and girls with haemophilia: lessons learned. Haemophilia. 2020. [DOI] [PubMed] [Google Scholar]
- 5. Paroskie A, Gailani D, DeBaun MR, Sidonio RF Jr. A cross‐sectional study of bleeding phenotype in haemophilia A carriers. Br J Haematol. 2015;170(2):223–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arya S, Wilton P, Page D, Boma‐Fischer L, Floros G, Winikoff R, et al. "Everything was blood when it comes to me": understanding the lived experiences of women with inherited bleeding disorders. J Thromb Haemost. 2020. 10.1111/jth.15102. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 7. Srivastava A, Brewer AK, Mauser‐Bunschoten EP, Key NS, Kitchen S, Llinas A, et al. Treatment Guidelines Working Group on Behalf of The World Federation Of Hemophilia. Guidelines for the management of hemophilia. Haemophilia. 2013;19(1):e1‐47 10.1111/j.1365-2516.2012.02909.x [DOI] [PubMed] [Google Scholar]
- 8. Makris M, Oldenburg J, Mauser‐Bunschoten EP, Peerlinck K, Castaman G, Fijnvandraat K, et al. Subcommittee on Factor VIII, Factor IX and Rare Bleeding Disorders. The definition, diagnosis and management of mild hemophilia A: communication from the SSC of the ISTH. J Thromb Haemost. 2018;16(12):2530‐2533. 10.1111/jth.14315 [DOI] [PubMed] [Google Scholar]
- 9. Rosendaal FR, Reitsma PH. Lots and lots of women. J Thromb Haemost. 2018;16(5):817 10.1111/jth.14019 [DOI] [PubMed] [Google Scholar]
- 10. Information on Hemophilia for Women. https://www.cdc.gov/ncbddd/hemophilia/women.html (Accessed October 9, 2020).
- 11. World Federation of Hemophilia Global Annual Survey, 2017.
- 12. Di Michele DM, Gibb C, Lefkowitz JM, Ni Q, Gerber LM, Ganguly A. Severe and moderate haemophilia A and B in US females. Haemophilia. 2014;20(2):e136–e143. [DOI] [PubMed] [Google Scholar]
- 13. Data and Statistics on von Willebrand Disease. https://www.cdc.gov/ncbddd/vwd/data.html (Accessed October 9, 2020).
- 14. Pliny the Elder's Natural History . The Empire in the Encyclopedia. Oxford: Oxford University Press; 2004. [Google Scholar]
- 15. Gilman S. Hysteria Beyond Freud. Berkeley: University of California Press; 1993; 18–20. [Google Scholar]
- 16. Bhartiya A. Menstruation, religion and society. Int J Social Sci Humanity. 2013;3:523–7. [Google Scholar]
- 17. Essity Femcare Hero II Brand Campaign Survey, 2017.
- 18. Kadir RA, Edlund M, Von Mackensen S. The impact of menstrual disorders on quality of life in women with inherited bleeding disorders. Haemophilia. 2010;16:832–9. [DOI] [PubMed] [Google Scholar]
- 19. American Academy of Pediatrics Committee on Adolescence , American College of Obstetricians and Gynecologists Committee on Adolescent Health Care , Diaz A, Laufer MR, Breech LL. Menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Pediatrics. 2006;118(5):2245‐50. 10.1542/peds.2006-2481 [DOI] [PubMed] [Google Scholar]
- 20. McShane M, Perucho J, Olsakowski M, Gaughan JP, Brown RT, Feldman‐Winter L. Menstrual history‐taking at annual well visits for adolescent girls. J Pediatr Adolesc Gynecol. 2018;31(6):566–70. [DOI] [PubMed] [Google Scholar]
- 21. Critchley HOD, Babayev E, Bulun SE, Clark S, Garcia‐Grau I, Gregersen PK, et al. Menstruation: science and society. Am J Obstet Gynecol. 2020;223(5):624–64. [DOI] [PMC free article] [PubMed] [Google Scholar]


