Abstract
Aims
Biofilm formation is one of the primary reasons for the difficulty in treating implant-related infections (IRIs). Focused high-energy extracorporeal shockwave therapy (fhESWT), which is a treatment modality for fracture nonunions, has been shown to have a direct antibacterial effect on planktonic bacteria. The goal of the present study was to investigate the effect of fhESWT on Staphylococcus aureus biofilms in vitro in the presence and absence of antibiotic agents.
Methods
S. aureus biofilms were grown on titanium discs (13 mm × 4 mm) in a bioreactor for 48 hours. Shockwaves were applied with either 250, 500, or 1,000 impulses onto the discs surrounded by either phosphate-buffered saline or antibiotic (rifampin alone or in combination with nafcillin). The number of viable bacteria was determined by quantitative culture after sonication. Representative samples were taken for scanning electron microscopy.
Results
The application of fhESWT led to a ten-fold reduction in bacterial counts on the metal discs for all impulse numbers compared to the control (p < 0.001). Increasing the number of impulses did not further reduce bacterial counts in the absence of antibiotics (all p > 0.289). Antibiotics alone reduced the number of bacteria on the discs; however, the combined application of the fhESWT and antibiotic administration further reduced the bacterial count compared to the antibiotic treatment only (p = 0.032).
Conclusion
The use of fhESWT significantly reduced the colony-forming unit (CFU) count of a S. aureus biofilm in our model independently, and in combination with antibiotics. Therefore, the supplementary application of fhESWT could be a helpful tool in the treatment of IFIs in certain cases, including infected nonunions.
Cite this article: Bone Joint Res 2021;10(1):77–84.
Keywords: fhESWT, Extracorporeal shockwave, Biofilm, Antibiotic, Staphylococcus aureus, Nonunion
Article focus
Antibactericidal efficacy of focused high-energy extracorporeal shockwave therapy (fhESWT) on bacterial biofilm.
Effect of combining fhESWT with antibiotic treatment on bacterial biofilm.
Key messages
Reduction of Staphylococcus aureus biofilm by fhESWT regardless of number of impulses.
Additional decrease of colony-forming unit (CFU) count on S. aureus biofilm by fhESWT in combination with nafcillin and rifampin.
Strengths and limitations
First study evaluating the antibiofilm efficacy of fhESWT on orthopaedic implants, in combination with antibiotics.
The main limitations of the study are that the impact of combining antibiotic agents other than rifampicin and nafcillin with shockwave therapy remains unknown, and the effects on bacterial species other than S. aureus are not tested.
Introduction
Implant-related infection (IRI) is among the most feared complications in orthopaedic trauma surgery as it is associated with impaired outcome, longer hospitalization, and higher healthcare costs.1 Conventional surgical treatment in early IRI normally consists of debridement, irrigation, implant retention, and antibiotic therapy, but failure rates vary from 10% to 30%.2,3 Staphylococcal biofilms are known to form on foreign bodies and allow bacteria to evade host responses and antibiotics,4 and so biofilm-colonized implants must often be removed.5 Several prophylactic procedures to prevent biofilm formation such as antibiotic coating of orthopaedic implants have shown encouraging results.6 However, these implants are not yet available for every anatomical region or device and cannot prevent biofilm formation in every case.7 New treatment options are therefore needed to improve treatment quality, and ideally ones which facilitate implant retention. Recently, adjunctive therapies such as acetic acid or the bacteriophage-derived lysin PlySs2 showed promising in vitro and in vivo results in treating Staphylococcus aureus biofilm,8,9 but such innovative strategies have not yet reached the clinic.
Focused high-energy extracorporeal shockwave therapy (fhESWT) is a non-invasive alternative for the treatment of fracture or arthrodesis nonunions with healing rates of nonunions up to 70% to 90% after six months.10-12 This therapy uses longitudinal acoustic waves to emit energy at areas with impedance discontinuities, such as the soft tissue to implant interface. The mechanism is not yet fully understood, however osteo- and angioinductive effects appear to play an important role.13,14 The use of fhESWT gained interest as a non-surgical supplement for treating musculoskeletal infections, as in vitro studies demonstrated an energy-dependent decrease of viable bacteria after exposure.15-17 Also, initial in vivo studies demonstrated a synergistic effect of fhESWT in treating bone infections in combination with antibiotics.18-20 Specifically, Inanmaz et al18 could show superior bactericidal activity of fhESWT in combination with teicoplanin compared to teicoplanin alone in a rat model of implant-related osteomyelitis. The use of fhESWT alone, without antibiotics, did not lower the colony-forming unit (CFU) count. However, in that model the implant (Kirschner wire (K-wire)) was removed before shockwave application, which impairs the comparability with the clinical scenario since the implant, and the biofilm on it, are the key treatment targets.18 Qi et al20 demonstrated a synergistic bactericidal effect of fhESWT and gentamicin in a rat model with a retained femoral K-wire.20 In an in vivo study in rabbits, the greatest impact of fhESWT on reducing the bacterial load was found on the implant surface compared to the surrounding tissue and bone.19 Whether fhESWT has a specific action against biofilm, or this effect is due to the fact that the impedance discontinuity is highest on the soft tissue/implant interface, remains to be determined. Should fhESWT specifically target implant-related biofilm, and act to enhance antibiotic activity, it would suggest the clinical value may not only be due to improved treatment outcome, but may also allow more frequent retention of the implant.
The dosage (number of impulses and energy flux density) of fhESWT was evaluated in vitro on bacterial suspensions.15 However, to our knowledge there is no study investigating the dose-response effect of fhESWT in combination with retained implants on a bacterial biofilm.
Therefore, the goal of the present study was to further investigate the effect of fhESWT on S. aureus biofilm on titanium implants in an in vitro setting. To our knowledge, this is the first study evaluating the dose-dependent effect of fhESWT alone and in conjunction with antibiotics routinely used in the clinic on a S. aureus biofilm, in order to provide some insight into the efficacy of fhESWT in treating orthopaedic device related infections.
Methods
Bacterial suspension
The bacterial strain used in this study was a multi-sensitive S. aureus: JAR 060131, available at the Swiss culture Collection (Waedenswil, Switzerland; Accession number CCOS 890).21 The strain has an minimal inhibitory concentration (MIC) to nafcillin (Sagent Pharmaceuticals, Schaumburg, Illinois, USA) of 0.5 µg/ml, and to rifampin (Labatec Pharma, Geneva, Switzerland) of 0.012 µg/ml.
Routine cultures were prepared from a working frozen stock kept at -20°C. When required, cultures were streaked out on a tryptic soy agar (TSA) plate (Oxoid, Basingstoke, UK), and single colonies were then incubated in tryptic soy broth (TSB) (Oxoid) overnight at 37°C in a shaking water bath. A fresh subculture was prepared to generate a log phase bacterial suspension. Bacteria were washed three times by centrifugation (2,500 xg for five minutes) to remove residual TSB and were resuspended in PBS each time. A bacterial suspension of approximately 2 × 108 CFUs/ml was prepared for addition to the adhesion chamber.
Bacterial adhesion and biofilm bioreactor
A custom-built bacterial adhesion chamber was used as previously described,22 with a capacity of holding 27 titanium discs (13 mm × 4 mm). Volumes of 100 ml of the bacterial suspension and 10 ml of fresh frozen human plasma (FFP) were added to 890 ml TSB and added through the inlet pipe. The adhesion chamber was incubated for 48 hours at 37°C to allow bacterial adhesion and biofilm formation. Hereafter, the fluid was removed and simultaneously flushed with 5 litres of sterile PBS to remove planktonic bacteria while preventing multiple liquid-air transitions. The rods were retrieved from the bioreactor and the metal discs were transferred separately in a laminar flow hood to a sterile plastic bag (SteriBag; Bürkle, Bad Bellingen, Germany). The sterile plastic bags were filled either with 7 ml of sterile PBS, 200 μg/ml rifampin (Labatec Pharma, Geneva, Switzerland) or a combination of 200 μg/ml rifampin and 200 μg/ml nafcillin (Sagent Pharmaceuticals, Schaumburg, Illinois, USA).
Extracorporeal shockwave therapy application
The first evaluation compared the dose-dependent effect of fhESWT on bacterial biofilm. With the shockwave system (LithoSpace Ortho; Jena Med Tech, Jena, Germany; for pressure vs time plot, see Supplementary Figure a), either no shockwaves or 250, 500, or 1,000 impulses were applied to both sides of the discs, with the following settings: energy flux density 0.4 mJ/mm2; 23kV; and 4 Hz. Each group contained two discs in separate bags. Experiments were repeated three times.
The second comparison evaluated a potential synergistic effect of a combined treatment of shockwaves with antibiotics on the biofilm. Therefore, discs were transferred into a solution with rifampin at a high concentration (200 µg/ml) and received either no shockwaves or 500 impulses per side with the same energy settings. A combination of nafcillin 200 µg/ml (400 × MIC) and rifampin 200 µg/ml (17,000 × MIC) were also tested in the same manner. The dosage of the antibiotics was selected based on preliminary experiments to achieve some anti-biofilm effects. Experiments were repeated three times.
Quantitative microbiology
Discs receiving shockwaves only were transferred immediately after treatment into sterile PBS (5 ml) under a laminar flow hood. Discs receiving the combination of shockwaves and antibiotics were kept for 24 hours at room temperature for antibiotic exposure and were thereafter transferred to sterile PBS.
Viable bacteria were quantified in the surrounding liquid by plating 1 ml onto TSA plates using a spiral plater (Eddy Jet 2; I&L Biosystems, Königswinter, Germany). Viable bacteria retained on the discs were assessed via sonicating the discs for three minutes (Bandelin Sonorex, Berlin, Germany) and plating 1 ml of the sonicate fluid onto TSA plates.
TSA plates were incubated at 37°C for 24 hours. Then, the number of CFUs was counted semi-automatically (SCAN1200; Interscience, Saint-Nom-la-Bretèche, France). The bacteria were confirmed as S. aureus via Latex agglutination test (Staphaurex; Thermo Fisher Scientific, Waltham, Massachusetts, USA) on each positive sample.
Scanning electron microscopy
Scanning electron microscopy (SEM: Hitachi FESEM 4700; Hitachi, Tokyo, Japan) was performed on representative samples with a secondary electrons (SE) and yttrium aluminium garnet (YAG) backscattered electrons (BSE) detector (Hitachi) and analyzed with digital acquisition software Quartz PCI (Quartz Imaging Corporation, Vancouver, Canada). Before observation, the samples were sputter coated with 10 nm gold/palladium (80:20) using a BAL-TEC MED 020 (BAL-TEC AG, Pfaeffikon, Switzerland).
Statistical analysis
Results are presented as means of each group with standard error of the mean (SEM). Data were checked for normal distribution. Since all data in shockwave-only experiments were normally distributed, we performed a one-way analysis of variance (ANOVA), followed by Tukey’s range test. In the experiments combining antibiotics and shockwaves, an independent-samples t-test with Welch's correction for normal distributed data and a Mann-Whitney U test in cases of non-normal distributed data were performed. In all cases, significance was set at p < 0.05. Prism 7 software was used for all statistical tests (GraphPad Software, San Diego, California, USA).
Results
Dose-dependent effect of fhESWT on biofilm
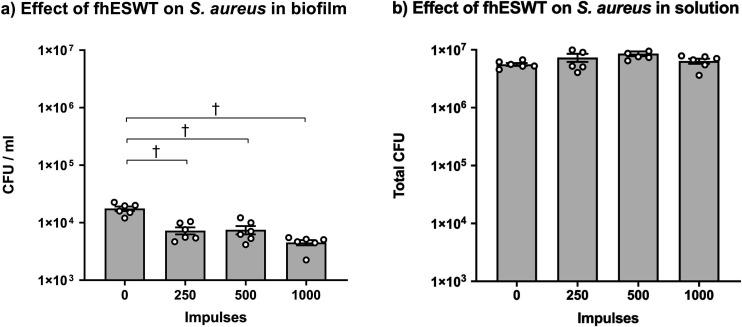
The use of fhESWT significantly decreased the bacterial load on the discs (Figure 1). This effect was seen regardless of number of impulses (mean: control group: 8.82 × 104 CFUs/ml (SEM 0.80 × 104); 250 impulses: 3.65 × 104 CFUs/ml (SEM 0.50 × 104); 500 impulses: 3.76 × 104 CFUs/ml (SEM 0.62 × 104); 1,000 impulses: 2.27 × 104 CFUs/ml (SEM 0.24 × 104); p < 0.001, ordinary one-way ANOVA followed by Tukey's range test). The highest number of impulses tested (1,000) displayed a non-significant decrease in bacteria compared to both the 250- and 500-impulse conditions (1,000 vs 500 impulses: p = 0.289; 1,000 vs 250 impulses: p = 0.353, both ordinary one-way ANOVA followed by Tukey's range test; Figure 1a). The bacterial count in the fluid, however, was approximately 100-fold higher than those remaining on the disc, and no significant differences were detected (Figure 1b).
Fig. 1.
Dose-dependent effect of focused high-energy extracorporeal shockwave therapy (fhESWT). a) Effect of different impulse numbers of fhESWT on Staphylococcus aureus colony-forming units (CFUs) in biofilm grown on titanium discs. b) Effect of different impulse numbers of fhESWT on S. aureus in the surrounding fluid of the plastic bag. N = 6 per group, significant difference compared to zero impulses (*p < 0.05; †p < 0.001, all ordinary one-way analysis of variance (ANOVA) followed by Tukey's range test), mean and standard error of the mean (SEM).
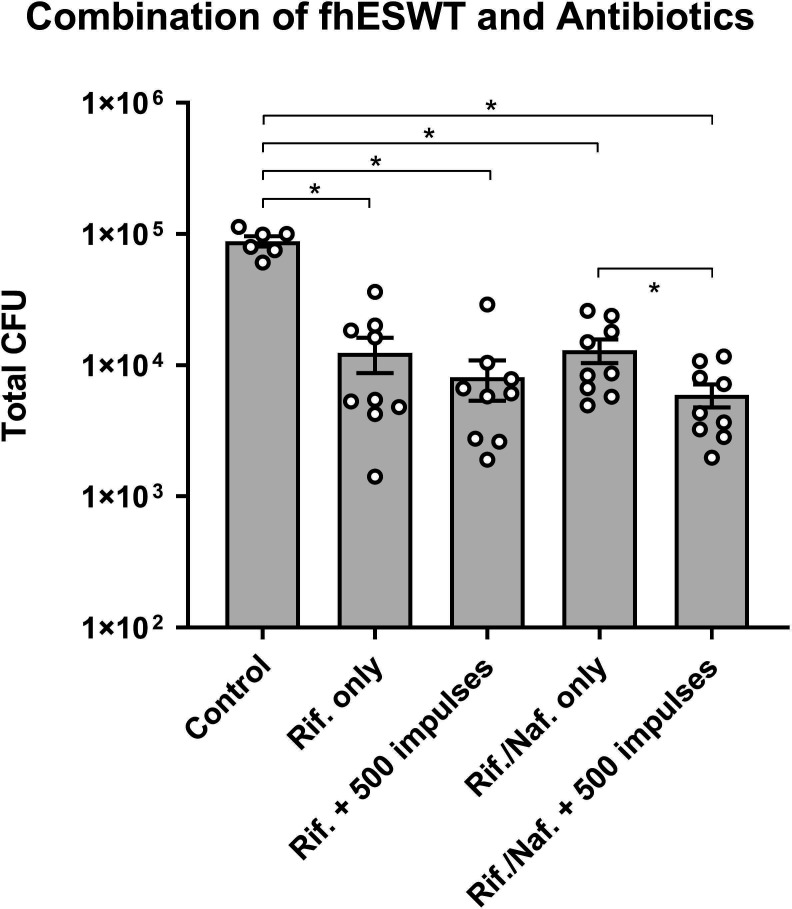
Combination of fhESWT and antibiotics on biofilm
Exposure of biofilm to rifampin and nafcillin, without any shockwave exposure, decreased the bacterial load on the discs in all four groups compared to the control group (mean: control: 8.82 × 104 CFUs/ml (SEM 1.95 × 104); rifampin alone: 1.25 × 104 CFUs/ml (SEM 1.13 × 104); rifampin and nafcillin: 1.30 × 104 CFUs/ml (SEM 0.80 × 104)) (Figure 2). No viable bacteria could be cultured from the surrounding fluids in all groups that contained antibiotics, in contrast to high CFU counts in controls that received no antibiotics and no shockwaves (Figure 1b).
Fig. 2.
Bacterial count on titanium discs with 24 hours of either 200 μg/ml of rifampin or a combination of 200 μg/ml of rifampin and 200 μg/ml of nafcillin. In the third and fifth columns, 500 impulses of focused high-energy extracorporeal shockwave therapy (fhESWT) were performed additionally. N = 9 for all groups, significant difference compared to no impulses (*p < 0.05), mean and standard error of the mean (SEM). Rif, rifampin; Naf, nafcillin.
The combination of rifampin and shockwaves tended to decrease the CFU count on the discs more than rifampin alone but did not reach statistical significance (mean 1.25 × 104 (SEM 0.38 × 104) vs 0.81 × 104 (SEM 0.28 × 104); p = 0.730, Mann-Whitney U test) (Figure 2). However, when shockwaves were applied on discs in a solution containing both rifampin and nafcillin, this lowered the bacterial load on the discs (mean 1.30 × 104 (SEM 0.27 × 104) vs 0.60 × 104 (SEM 0.12 × 104); p = 0.032, Mann-Whitney U test) significantly compared to the antibiotics alone (Figure 2).
Scanning electron micrographs were taken in the control group and after exposure to shockwaves (500 impulses) and antibiotics (rifampin), alone or in combination, to visually compare cellular morphology post-exposure. In the control group, we observed a regular biofilm formation (Figures 3a and 3c). In contrast, fhESWT exposure resulted in multiple fields of scattered debris in approximate oval-to-circular pattern of 6 μm diameter, leaving only very few intact bacteria on the disc (see Figures 3d and 3f). After rifampin exposure, the colonies displayed a regular morphology with coccoid bacteria and no, or minimal, lysis or cellular debris observed (Figures 3g and 3i). In contrast, the combined treatment of rifampin and fhESWT showed, equivalent to the shockwave-only group, multiple fields of scattered debris and few, if any, intact bacteria (see Figures 3j and 3l).
Fig. 3.
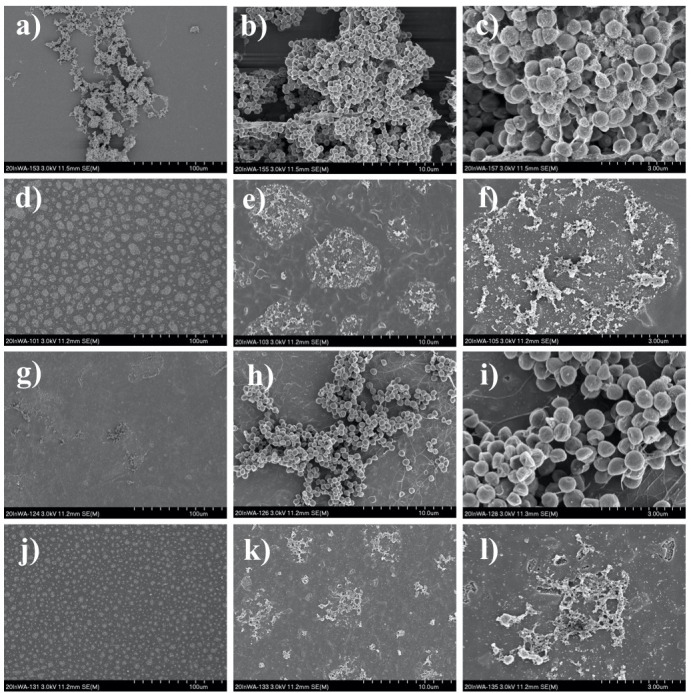
Representative scanning electron microscopy (SEM) images of biofilm on titanium discs in different magnifications (a, d, g, j: 500×; b, e, h, k: 5,000×; c, f, i, l: 15,000×). a) to c) Control group. d) to f) 500 impulses of focused high-energy extracorporeal shockwave therapy (fhESWT) without antibiotics. g) to i) Rifampin 200 μg/ml without fhESWT. j) to l) 500 impulses of fhESWT + rifampin 200 μg/ml.
Discussion
The formation of implant-related bacterial biofilm is one of the main reasons for treatment failure of IRI. New antibiofilm approaches remain a major goal in orthopaedic research. The effect of fhESWT on bacterial biofilms on orthopaedic devices has not been investigated before, although there are data showing it has an effect against planktonic bacteria.15,16 In a first in vivo investigation, we observed that fhESWT reduced bacterial burden on the implants, although it was not clear if this was a direct effect against biofilm or an indirect effect such as increased local perfusion, and thus improved antibiotic penetration into infected tissue.19 In this study, we evaluated the dose-dependent effect of fhESWT on S. aureus biofilms in vitro to determine if fhESWT has a direct antibiofilm effect, synergistic effects in combination with antibiotics, and whether this effect depends on the number of impulses.
We evaluated the dose response effect of fhESWT and found a statistically significant reduction with 250 impulses, but no further statistically significant reduction at 500 and 1,000 impulses. Earlier results by Gerdesmeyer et al15 found a clear dose-dependent effect, whereby at least 1,000 impulses were required for antibacterial activity and 4,000 impulses were needed for almost complete eradication. The impulses in that study were created with a different shockwave generator, but with similar energy levels (0.59 mJ/mm2 vs 0.40 mJ/mm2 in our study).15 In the clinical context of a fracture nonunion, where fhESWT is used to stimulate bone healing, patients typically receive 3,000 impulses in total, which may be 1,000 impulses in three distinct sites.23 In the in vitro setting, where there is no soft tissue or skin hindering application of shockwaves, it may be that the effect is greater than an equivalent number of impulses in vivo. However, we also performed up to 1,000 impulses per side of the disc, imitating the clinical regimen. The fact that the biofilm is impacted by relatively few impulses and does not require a high number of impulses for the antibiofilm effect suggests that the clinical regimen of 3,000 impulses may be quite appropriate.
The exact mechanisms of antibiofilm activity of shockwaves remain to be fully elucidated. Our SEM images revealed a mechanical disruptive effect of fhESWT on bacteria that is distinct from the effect seen after antibiotic treatment alone. The application of fhESWT seems to have a direct effect on bacterial biofilm based on the widespread deposition of oval-shaped deposits across the surface of the metal, presumptively remnants of biofilm and bacteria. To our knowledge, this phenomenon has not been previously described. A single previous study investigated the effect of fhESWT on biofilm on metal implants via SEM,20 whereby a reduction in CFU count of S. aureus was visible in SEM pictures with fhESWT alone and an even stronger reduction with fhESWT and gentamicin.20 However, there were no signs of any impact of fhESWT on the bacterial structure in the published images. In any case, those biofilms were not cultured in the presence of plasma, in which case the biofilm matrix is less representative of the clinical situation and less comparable to our data.20 Horn et al17 investigated the effect of fhESWT on bacterial cell walls via Sytox Green fluorescence staining and revealed that the effect on a S. aureus suspension was not primarily due to a change of the cell wall integrity, as they observed a discrepancy between the strong bactericidal effect of fhESWT and only a low intracellular Sytox green uptake.17 Furthermore, no morphological differences were observed on SEM images between the control group and the high-dose group of 0.96 mJ/mm2 and 4,000 impulses.17 However, in line with our results, there is evidence for fhESWT to have a direct disruptive and bactericidal effect on bacterial biofilms, although these data have not been of direct relevance to orthopaedic implants, but rather to urinary catheters and periodontitis.24,25
There is also evidence that the effect of fhESWT is not specific for S. aureus, but rather general to different bacterial species, both Gram-negative and Gram-positive. Gollwitzer et al16 evaluated the effect of fhESWT with a high-energy flux density of 0.96 mJ/mm2 on planktonic bacterial suspensions of different bacterial species (multisensitive S. aureus, multiresistant S. aureus, Staphylococcus epidermidis, Pseudomonas aeruginosa, Enterococcus faecium).16 The shockwaves lead to a statistically significant 99% eradication on all five species, with the highest effect on multisensitive S. aureus and S. epidermidis, both of which are the main culprits for musculoskeletal infections.16 Further studies are warranted to elucidate if the antibiofilm effect results from mechanical destruction, shedding of bacteria from the metal (analogous to sonication), or another mechanism, and how this effect translates across different bacterial species.
The second aspect under investigation was the potential synergistic interaction between shockwaves and antibiotic therapy. Biofilm formation decreases susceptibility to antibiotics and also enhances resistance to host immune defenses compared to planktonic cultures of the same strain.26-28
As the exact mechanism of fhESWT on biofilms remains unknown, the application of fhESWT may either disrupt the biofilm structure and facilitate exposure of bacteria to antibiotic agents or kill bacteria directly or indirectly. To analyze the additional effect of fhESWT in combination with conventional antibiotic treatment, we evaluated two different antibiotic regimens in combination with fhESWT. We chose rifampin since it is commonly used in clinics to treat IRIs and is known to have anti-staphylococcal biofilm activity.29 Rifampin alone lowered the bacterial load on the discs, but the additional application of the shockwaves could not statistically significantly lower the CFU count any further. A reason for this might be the very quick development of resistance of S. aureus to rifampin when used alone.5,30 Therefore, we also trialled the combination of rifampin with another antibiotic (nafcillin) as it is advisable in the clinical scenario. Rifampin is also known to be more effective when partnered with a second antibiotic agent.29,31 Nafcillin is a bactericidal antibiotic that works via inhibiting bacterial cell wall synthesis, but also has no described activity against extracellular polymeric substance (EPS). The combination of rifampin and nafcillin, which is a common combination in clinics, lowered the CFU count on the discs alone, but adjunctive fhESWT resulted in a further statistically significant reduction. This suggests that fhESWT might not only mechanically disrupt the extracellular matrix (ECM) structure, but might facilitate antibiotic penetration into bacteria.
To our knowledge, no other studies have investigated the combined effect of focused high-energy ESWT and antibiotics in vitro on to an orthopaedic device related bacterial biofilm. Wanner et al32 evaluated the effect of low-energy ESWT on a 72-hour S. aureus or S. epidermidis biofilm in vitro. In that study, ESWT itself did not lead to a statistically significant reduction of the bacterial load for both species. However, the combination of ESWT and rifampin or cefuroxime eradicated the biofilm and no viable cells were found. The lack of coupling agents in the development of a S. aureus biofilm in their model, such as fibronectin and other plasma proteins, made their biofilm less clinically relevant than the biofilm in our study, leading to a possible increased susceptibility of the biofilm to the antibiotics and fhESWT.32 Inclusion of matrix proteins present in plasma increases the complexity and clinical relevance of the biofilm studied here. Furthermore, S. aureus was shown to be 3.8 times more adhesive to an orthopaedic device in the presence of human plasma compared to controls without human plasma.22 In comparison to the study of Wanner et al,32 we assessed a 48-hour biofilm. In a prior study with the same bioreactor, we could show a robust biofilm already after 2.5 hours.32 A possible explanation for the non-bactericidal effect of the low dose ESWT itself in the Wanner study32 could be the lower energy, although to date there have been no comparative studies between low dose or focused high-energy shockwave therapy. Equivalent to the findings of our study, Gnanadhas et al24 and Datey et al25 could show an enhanced susceptibility of bacterial biofilms toward antibiotic treatment after shockwave treatment in cases of urinary catheter infection and periodontitis.24,25
Our experimental model attempted to simulate IRI with biofilm formation and treatment with clinically relevant antibiotics and fhESWT. Obviously, there are certain limitations of that model. For example, the application of fhESWT on metal discs that are surrounded by fluid does not recapitulate soft tissue and implant attachment to a solid body such as bone. The energy of fhESWT is reduced behind structures with high impedance (e.g. bone, metal implants), shown by preliminary experiments on fine plaster blocks (Supplementary Figure b). In any case, fhESWT is not meant to be a standalone treatment, but rather an adjunctive treatment option in combination with standard treatment comprising debridement, irrigation, and systemic antibiotics.
In conclusion, fhESWT reduces S. aureus biofilm in vitro on metal discs. SEM images suggest a combination of mechanical removal from the surface and destruction of bacterial cells. Additionally, fhESWT in our model synergistically increased the efficacy of antibiotics in reducing viable bacteria in biofilm. Because of this and the known osteo- and angioinductive effects, the application of fhESWT in human medicine could be helpful for improving the treatment quality in certain cases of orthopaedic device related infections.
Author contributions
A. Milstrey: Acquired and analyzed the data. Created the figures, Wrote the manuscript.
S. Rosslenbroich: Performed the statistical analysis. Revised the manuscript.
J. Everding: Designed the study, Interpreted the data, Revised and edited the manuscript.
M. J. Raschke: Designed the study, Interpreted the data, Revised and edited the manuscript.
R. G. Richards: Designed the study, Interpreted the data, Revised and edited the manuscript.
T. F. Moriarty: Designed the study, Interpreted the data, Revised and edited the manuscript.
J. Puetzler: Designed the study, Interpreted the data, Created the figures, Wrote, revised, and edited the manuscript.
T. F. Moriarty and J. Puetzler are joint senior authors.
Funding statement
The authors report a study-related grant and support for travel to meetings from AO Trauma, as part of the Clinical Priority Program Bone Infection (AO Trauma Research Grant). No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
We thank Jena Medtech (now Storz Medical), especially Dr. Werner Schwarze, for providing us with the LithoSpace Ortho. Iris Keller, Pamela Furlong, and Willemijn Boot, all from AO Research Institute Davos, are acknowledged for their expert assistance in the design, performance, and discussion of the presented work.
Ethical review statement
As this was an in vitro experiment, no ethical approval was required.
Supplementary material
Figures showing a pressure versus time plot of focused high-energy extracorporeal shockwave therapy (fhESWT) application, and the effect of fhESWT on fine plaster blocks.
© 2021 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- 1.Thakore RV, Greenberg SE, Shi H, et al. . Surgical site infection in orthopedic trauma: a case-control study evaluating risk factors and cost. J Clin Orthop Trauma. 2015;6(4):220–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berkes M, Obremskey WT, Scannell B, et al. . Maintenance of hardware after early postoperative infection following fracture internal fixation. J Bone Joint Surg Am. 2010;92-A(4):823–828. [DOI] [PubMed] [Google Scholar]
- 3.Tschudin-Sutter S, Frei R, Dangel M, et al. . Validation of a treatment algorithm for orthopaedic implant-related infections with device-retention-results from a prospective observational cohort study. Clin Microbiol Infect. 2016;22(5):457.e1–45457. [DOI] [PubMed] [Google Scholar]
- 4.Zimmerli W, Waldvogel FA, Vaudaux P, Nydegger UE. Pathogenesis of foreign body infection: description and characteristics of an animal model. J Infect Dis. 1982;146(4):487–497. [DOI] [PubMed] [Google Scholar]
- 5.Raad I, Hanna H, Jiang Y, et al. . Comparative activities of daptomycin, linezolid, and tigecycline against catheter-related methicillin-resistant Staphylococcus bacteremic isolates embedded in biofilm. Antimicrob Agents Chemother. 2007;51(5):1656–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fuchs T, Stange R, Schmidmaier G, Raschke MJ. The use of gentamicin-coated nails in the tibia: preliminary results of a prospective study. Arch Orthop Trauma Surg. 2011;131(10):1419–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidmaier G, Lucke M, Wildemann B, Haas NP, Raschke M. Prophylaxis and treatment of implant-related infections by antibiotic-coated implants: a review. Injury. 2006;37 Suppl 2(2):S105–S112. [DOI] [PubMed] [Google Scholar]
- 8.Tsang STJ, Gwynne PJ, Gallagher MP, Simpson AHRW. The biofilm eradication activity of acetic acid in the management of periprosthetic joint infection. Bone Joint Res. 2018;7(8):517–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sosa BR, Niu Y, Turajane K, et al. . 2020 John Charnley Award: the antimicrobial potential of bacteriophage-derived lysin in a murine debridement, antibiotics, and implant retention model of prosthetic joint infection. Bone Joint J. 2020;102-B(7_Supple_B):3–10. [DOI] [PubMed] [Google Scholar]
- 10.Cacchio A, Giordano L, Colafarina O, et al. . Extracorporeal shock-wave therapy compared with surgery for hypertrophic long-bone nonunions. J Bone Joint Surg Am. 2009;91-A(11):2589–2597. [DOI] [PubMed] [Google Scholar]
- 11.Furia JP, Juliano PJ, Wade AM, Schaden W, Mittermayr R. Shock wave therapy compared with intramedullary screw fixation for nonunion of proximal fifth metatarsal metaphyseal-diaphyseal fractures. J Bone Joint Surg Am. 2010;92-A(4):846–854. [DOI] [PubMed] [Google Scholar]
- 12.Nicholson JA, Tsang STJ, MacGillivray TJ, Perks F, Simpson AHRW. What is the role of ultrasound in fracture management?: diagnosis and therapeutic potential for fractures, delayed unions, and fracture-related infection. Bone Joint Res. 2019;8(7):304–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lama A, Santoro A, Corrado B, et al. . Extracorporeal shock waves alone or combined with raloxifene promote bone formation and suppress resorption in ovariectomized rats. PLoS One. 2017;12(2):e0171276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang C-J, Wang F-S, Yang KD, et al. . Shock wave therapy induces neovascularization at the tendon–bone junction. A study in rabbits. J. Orthop. Res.. 2003;21(6):984–989. [DOI] [PubMed] [Google Scholar]
- 15.Gerdesmeyer L, von Eiff C, Horn C, et al. . Antibacterial effects of extracorporeal shock waves. Ultrasound Med Biol. 2005;31(1):115–119. [DOI] [PubMed] [Google Scholar]
- 16.Gollwitzer H, Horn C, Eiff CV, Henne M, Gerdesmeyer L. [Antibacterial effectiveness of high-energetic extracorporeal shock waves: an in vitro verification]. Z Orthop Ihre Grenzgeb. 2004;142(4):462–466. (Article in German) [DOI] [PubMed] [Google Scholar]
- 17.Horn C, Mengele K, Gerdesmeyer L, Gradinger R, Gollwitzer H. The effect of antibacterial acting extracorporeal shockwaves on bacterial cell integrity. Med Sci Monit. 2009;15(12):BR364–369. [PubMed] [Google Scholar]
- 18.Inanmaz ME, Uslu M, Isik C, Kaya E, Tas T, Bayram R. Extracorporeal shockwave increases the effectiveness of systemic antibiotic treatment in implant-related chronic osteomyelitis: experimental study in a rat model. J Orthop Res. 2014;32(6):752–756. [DOI] [PubMed] [Google Scholar]
- 19.Puetzler J, Milstrey A, Everding J, et al. . Focused high-energy extracorporeal shockwaves as supplemental treatment in a rabbit model of fracture related infection. J Orthop Res. 2020;38(6):1351–1358. [DOI] [PubMed] [Google Scholar]
- 20.Qi X, Zhao Y, Zhang J, et al. . Increased Effects of Extracorporeal Shock Waves Combined with Gentamicin against Staphylococcus aureus Biofilms In Vitro and In Vivo. Ultrasound Med Biol. 2016;42(9):2245–2252. [DOI] [PubMed] [Google Scholar]
- 21.Campoccia D, Montanaro L, Moriarty TF, Richards RG, Ravaioli S, Arciola CR. The selection of appropriate bacterial strains in preclinical evaluation of infection-resistant biomaterials. Int J Artif Organs. 2008;31(9):841–847. [DOI] [PubMed] [Google Scholar]
- 22.Rochford ETJ, Poulsson AHC, Salavarrieta Varela J, Lezuo P, Richards RG, Moriarty TF. Bacterial adhesion to orthopaedic implant materials and a novel oxygen plasma modified peek surface. Colloids Surf B Biointerfaces. 2014;113:213–222. [DOI] [PubMed] [Google Scholar]
- 23.Everding J, Freistühler M, Stolberg-Stolberg J, Raschke MJ, Garcia P. [Extracorporal shock wave therapy for the treatment of pseudarthrosis : New experiences with an old technology]. Unfallchirurg. 2017;120(11):969–978. (Article in German) [DOI] [PubMed] [Google Scholar]
- 24.Gnanadhas DP, Elango M, Janardhanraj S, et al. . Successful treatment of biofilm infections using shock waves combined with antibiotic therapy. Sci Rep. 2015;5(1):17440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Datey A, Thaha CSA, Patil SR, Gopalan J, Chakravortty D. Shockwave therapy efficiently cures multispecies chronic periodontitis in a humanized rat model. Front Bioeng Biotechnol. 2019;7:382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roy R, Tiwari M, Donelli G, Tiwari V. Strategies for combating bacterial biofilms: a focus on Anti-Biofilm agents and their mechanisms of action. Virulence. 2017;9(1):522–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stewart PS, Costerton JW. Antibiotic resistance of bacteria in biofilms. Lancet. 2001;358(9276):135–138. [DOI] [PubMed] [Google Scholar]
- 28.Gristina AG. Biomaterial-centered infection: microbial adhesion versus tissue integration. Science. 1987;237(4822):1588–1595. [DOI] [PubMed] [Google Scholar]
- 29.Zimmerli W, Sendi P. Role of Rifampin against Staphylococcal Biofilm Infections In Vitro, in Animal Models, and in Orthopedic-Device-Related Infections. Antimicrob Agents Chemother. 2018;63(2):e01746–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perlroth J, Kuo M, Tan J, Bayer AS, Miller LG. Adjunctive use of rifampin for the treatment of Staphylococcus aureus infections: a systematic review of the literature. Arch Intern Med. 2008;168(8):805–819. [DOI] [PubMed] [Google Scholar]
- 31.Yu K, Song L, Kang HP, Kwon H-K, Back J, Lee FY. Recalcitrant methicillin-resistant Staphylococcus aureus infection of bone cells: Intracellular penetration and control strategies. Bone Joint Res. 2020;9(2):49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wanner S, Gstöttner M, Meirer R, Hausdorfer J, Fille M, Stöckl B. Low-energy shock waves enhance the susceptibility of staphylococcal biofilms to antimicrobial agents in vitro. J Bone Joint Surg Br. 2011;93-B(6):824–827. [DOI] [PubMed] [Google Scholar]