Abstract
Background: Psychiatrically vulnerable adolescents may be at heightened risk for suicide during the COVID-19 pandemic. This study characterizes suicidal ideation (SI) and suicide attempts (SA) in a sample of adolescents psychiatrically hospitalized during COVID-19. Rates of SI and SA are compared to a historical hospital sample from a matched period in the year prior. Associations between specific stressors and COVID-related SI are also explored. Methods: This cross-sectional chart review utilizes hospital intake data, including self-reports of SA, SI (general and COVID-related), and COVID-specific stressors. Results: SA and SI ratings were higher in the COVID-19 sample compared to the historical sample. Stressors related to missing special events, financial problems, in-home conflict, and changes in living circumstances were associated with COVID-related SI. Among first-time admissions, several interpersonal stressors were linked to COVID-related SI. Limitations: Analyses were cross-sectional, limiting our ability to draw conclusions about causality. Conclusions: This study offers preliminary evidence that COVID-19 may be contributing to suicidal thoughts and behaviors in high-risk adolescents.
Keywords: COVID-19, Coronavirus, Adolescents, Suicidal ideation, Suicide attempts
1. Introduction
The coronavirus disease-2019 (COVID-19) pandemic has disrupted daily life for individuals across the lifespan. While limiting social interactions is essential for minimizing COVID-19 spread, the resultant adverse effects may be acutely felt by adolescents who are in a developmental period when social relationships are especially salient. Disruptions from the pandemic cut across many intersecting domains, including academic, interpersonal, financial, and health. For instance, schools transitioning from in-person to remote may have affected meal access, academic instruction, social interaction, and mental health services (Golberstein et al., 2020; Guessoum et al., 2020). Indeed, the impact of COVID-related stress has been observed in adolescents who exhibit elevated internalizing symptoms during the pandemic compared to the three months prior (Chahal et al., 2020) and compared to younger youth (Tang et al., 2020).
Increases in suicide rates have been documented during epidemic events (Chan et al., 2006; Wasserman, 1992). However, there is a dearth of research on correlates of adolescent suicidality during epidemics (Guessoum et al., 2020). Recent literature has linked COVID-19 stressors to past-month suicidal ideation (SI) and suicide attempts (SA) in adults (Ammerman et al., 2020), but no published research has looked at these rates in adolescents during the COVID-19 pandemic.
This study explores SI and recent SA in a sample of psychiatrically-hospitalized adolescents. Using historical chart data from the same hospital, SI and SA rates are compared across matched four-month periods in 2019 and 2020 to explore differences in suicidal thoughts and behaviors. Additionally, associations between specific stressors and COVID-related SI are explored.
2. Methods
2.1. Procedure
Data were gathered during standard intake procedures for an adolescent psychiatric inpatient unit, which includes a self-report battery of mental health questionnaires. Psychology staff monitor and assist adolescents with survey completion (e.g., clarifying instructions, reading surveys aloud if needed). Most admitted adolescents agree to complete the intake battery, however, some refuse or are unable to complete the surveys due to psychiatric acuity. The Institutional Review Board approved and waived informed consent for this retrospective chart review study.
2.2. Participants
This sample included adolescents (11–18 years old) hospitalized during the COVID-19 pandemic (April 13, 2020 to September 14, 2020). Notably, school closings began March 13, 2020; data collection began one month into statewide pandemic-related closings (see Fig. 1 for study timeline detailing key COVID-19 milestones).
Fig. 1.
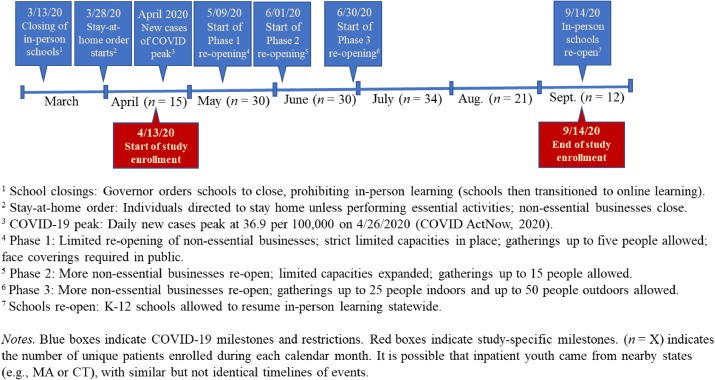
Timeline of COVID-19 milestones and restrictions in the state of Rhode Island during the study period.
A historical sample from the year prior (April 13, 2019 to September 14, 2019) was used for comparison. This sample included all adolescents who completed the self-report battery during this timeframe. Intake procedures were the same for both samples, except the COVID-19 survey was added in 2020. From the historical dataset, demographic, SA and SI data were used in analyses.
Within both samples, the most common reasons for admission were safety concerns (i.e., behaviors indicating imminent danger to themselves or others). All patients who completed the self-report battery were included, regardless of reason for admission.
2.3. Measures
Demographics. At intake, adolescents self-reported age, gender, ethnicity, and race.
Suicidal ideation. Adolescents completed the Suicidal Ideation Questionnaire-Junior (SIQ-Jr; Reynolds, 1987), a valid and reliable 15-item questionnaire assessing SI frequency among youth. Items are rated on a seven-point scale: 0 (never) to 6 (almost daily). Clinically, scores greater than 30 indicate high risk. Summed scores (0-90) were used in analyses. Internal consistency was excellent (α = 0.96 in both the 2019 and 2020 samples).
Suicide attempts. Adolescents were asked two yes/no questions, “Have you made any suicide attempts in the [30 or 7] days before you came to the hospital?”
Hospitalization history. Adolescents were asked whether they had been previously hospitalized for emotional or behavioral concerns, including outside of the current hospital, as a proxy for psychiatric vulnerability. For adolescents who denied past hospitalization(s), electronic medical records were cross-referenced within the healthcare system (the largest in the state, serving the majority of the state's acute psychiatric adolescent population). Identified discrepancies were coded “yes” for prior hospitalization if records indicated that the adolescent had been admitted in the past for psychiatric concerns. Reports of past hospitalizations were not validated through chart review, as hospitalizations outside of the system cannot be verified.
COVID-SI. Adolescents were asked about SI explicitly linked to COVID-19: “To what extent have you felt suicidal in relation to COVID-19?” Responses ranged from 0 (not much/not at all) to 4 (a lot). COVID-SI was dichotomized (yes[1]/no[0]), with responses greater than “0” considered endorsements.
COVID-related stressors. Adolescents were asked “To what degree did you experience any of the following stressors as a result of COVID-19?”, followed by a series of specific stressors (see Table 1 ). Answers ranged from 0 (not at all) to 4 (extremely).
Table 1.
Differences in stressor ratings between COVID-related suicidality groups.
| Stressor item | COVID-related suicidality group (n = 67) Mean; SD | No COVID-related suicidality group (n = 75) Mean; SD | t-statistic, p-value | Hedges’ g |
|---|---|---|---|---|
| Access to basic needs (food, medication) | M = 1.58; | M = 1.39; | t = -1.31; | 0.22 |
| SD = 1.03 | SD = 0.70 | p = .194 | ||
| Money problems | M = 1.94; | M = 1.60; | t = -1.93; | 0.32 |
| SD = 1.13 | SD = 0.97 | p = .055 | ||
| Fighting/arguing/conflict at home | M = 2.70; | M = 2.28; | t = -1.93; | 0.32 |
| SD = 1.39 | SD = 1.21 | p = .056 | ||
| Being cutoff from contact with others | M = 2.67; | M = 2.35; | t = -1.38; | 0.23 |
| SD = 1.49 | SD = 1.29 | p = .170 | ||
| Not being able to go out/leave the home when I want to | M = 2.97; | M = 2.71; | t = -1.19; | 0.20 |
| SD =1.31 | SD = 1.32 | p = .237 | ||
| Not being able to attend special events | M = 2.78; | M = 2.19; | t = -2.57; | 0.43 |
| SD = 1.38 | SD = 1.35 | p = .011 | ||
| Having to change who I'm living with | M = 1.76; | M = 1.40; | t = -1.98; | 0.34 |
| SD = 1.21 | SD = 0.93 | p = .050 | ||
| Not being able to see people I care about in person | M = 2.97; | M = 2.64; | t = -1.38; | 0.23 |
| SD = 1.46 | SD =1.39 | p = .170 | ||
| Someone I care about got sick | M = 1.69; | M = 1.69; | t = 0.34; | 0.00 |
| SD = 1.13 | SD = 1.23 | p = .973 | ||
| Worried about getting COVID-19 myself | M = 2.18; | M = 1.87; | t = -1.46; | 0.24 |
| SD = 1.35 | SD = 1.19 | p = .147 | ||
| Worries about someone I care about getting COVID-19 | M = 2.94; | M = 2.69; | t = -1.02; | 0.17 |
| SD = 1.42 | SD = 1.45 | p = .309 |
Note: Boldindicates statistically significant differences (p < .05) across groups; Italic indicates trend-level (.10 > p > .05) differences across groups.
3. Results
During the 2020 (COVID-19) study enrollment period, 189 unique adolescents were admitted to the psychiatric inpatient unit and 142 adolescents (75.1%) completed the self-report battery. The sample was 45.8% female, 40.1% male, 7.0% gender-queer/non-conforming/fluid, 4.9% transgender male, and 2.1% did not identify with any of the listed categories or declined to answer. Fifty-one youth (35.9%) were Hispanic/Latinx. The sample was 54.9% white, 15.5% Black, 13.4% other race, and 16.2% multiracial.
The 2019 sample included 196 adolescents. The 2020 sample was significantly older (m = 15.06, SD = 1.72 vs. m = 14.53, SD = 2.03; t(327.76) = -2.58, p = .010; Hedges’ g = 0.28). Age was not related to (a) SA or SI within or across samples, or (b) COVID-related stressors. There were no differences in rates of Hispanic/Latinx youth, gender identities, or racial identities across samples.
The rate of past-week SA was significantly greater in 2020 (n = 35) compared to 2019 (n = 31), with a small effect (phi = 0.11): 24.6% versus 15.8%; Χ2 = 4.09, p = .043. The rate of past-month SA was also significantly higher in 2020 (n = 44) compared to 2019 (n = 38), with a small effect (phi = 0.13): 31.0% versus 19.4%; Χ2 = 6.03, p = .014. SIQ-Jr scores were significantly greater in 2020 (m = 36.08, SD = 27.66) compared to 2019 (m = 30.05, SD = 26.23; t(336) = −2.04, p = .042), demonstrating a small effect (Hedges’ g = 0.22).
Within the 2020 sample, 67 adolescents (47.2%) agreed that to some extent, they felt suicidal in relation to COVID-19 (m = 2.57, SD = 1.16). Seventy-five adolescents (52.8%) denied COVID-SI. There were no differences in past-week or past-month SA rates across those who did and did not endorse COVID-SI. SIQ-Jr scores were significantly greater among those who endorsed COVID-SI (m = 46.99, SD = 24.22) versus those who did not (m = 26.35, SD = 27.05; t(140) = -4.77, p < .001), demonstrating a large effect (Hedges’ g = 0.80).
T-tests compared mean stressor ratings across adolescents who did and did not endorse COVID-SI (Table 1). Ratings for being unable to attend special events were significantly higher (indicating more severe impact) among youth who endorsed COVID-SI. There were trends toward higher ratings for financial problems, in-home conflict, and having to change living circumstances among youth who endorsed COVID-SI.
There was no significant difference in rate of COVID-SI between individuals with prior psychiatric hospitalizations (n = 75) and those whose first hospitalization was during COVID-19 (n = 67). Parallel series of t-tests were run within each of these groups to compare stressor ratings across those who did and did not endorse COVID-SI. Among adolescents experiencing their first hospitalization, those who endorsed COVID-SI (n = 28/67) had higher ratings for the following stressors, with medium effects: being cutoff from contact with others (t(65) = -2.16, p = .034; Hedges’ g = 0.53), being unable to leave home (t(65) = -2.34, p = .022; Hedges’ g = 0.58), missing events (t(65) = -2.57, p = .013; Hedges’ g = 0.63), and not being able to see people they care about (t(65) = −2.14, p = .036; Hedges’ g = 0.52). Among adolescents with a history of hospitalization, those who endorsed COVID-SI (n = 39/75) had higher rates of worry about themselves contracting COVID-19 (t(71.33) = -2.22, p = .030), demonstrating a medium effect (Hedges’ g = 0.51).
4. Discussion
Despite the clear impact of COVID-19 on adolescents’ daily lives, little is known about how the pandemic has influenced suicidal thoughts and behaviors among vulnerable youth. Our findings suggest that SI and SA were elevated among psychiatrically hospitalized adolescents during the pandemic, compared to data from the same hospital unit during the year prior. These findings are consistent with public health warnings and recent evidence from the U.S. Center for Disease Control and Prevention indicating that SI has increased among U.S. young adults during the pandemic (Czeisler et al., 2020; Sher, 2020).
Nearly half of the 2020 sample reported feeling suicidal specifically in relation to COVID-19, indicating the potentially detrimental impact of the pandemic on youth mental health. There are likely many reasons why COVID-19 may contribute to increased suicidality among youth. Providing potential insight into these reasons, we found that adolescents who endorsed COVID-SI, compared to those who did not, reported experiencing significantly more stress related to missing special events (small-medium effect), and some elevated stress related to money problems, in-home conflict, and changing who they are living with (small effects). Notably, while prior work has emphasized the pandemic's effects on adolescents’ loneliness and peer socialization (Ellis et al., 2020; Loades et al., 2020), our findings suggest that COVID-related stressors occur across multiple domains (e.g., finance, home-life stability) that are associated with SI. This has important implications for suicide prevention and intervention efforts during the pandemic. Specifically, these findings highlight the importance of familial and financial support, in addition to social integration, to enhance feelings of security and well-being among youth. High risk populations, including psychiatrically vulnerable, system-involved, or gender or sexual minority youth, are likely particularly vulnerable to COVID-related stressors (Cohen and Bosk, 2020).
Patterns of associations between specific stressors and COVID-SI differed based on whether or not adolescents had a history of psychiatric hospitalization. For previously-hospitalized adolescents, worry about contracting COVID-19 was the only stressor significantly associated with COVID-related suicidality (medium effect). A large proportion of adolescents experiencing their first hospitalization endorsed COVID-SI, and interpersonal stressors (i.e., limited contact with others, unable to leave home, missing events) appear to be linked, with medium effects, to feeling suicidal in this subgroup. These findings are consistent with studies of previously healthy children and adolescents that found social isolation and loneliness were associated with increased depression risk (see Loades et al., 2020 for review). Given evidence that loneliness duration (vs. intensity) may be more strongly linked to mental health (Loades et al., 2020), the extended and uncertain nature of COVID-related social isolation is particularly concerning for adolescents. Implementing social support initiatives may be crucial to reduce loneliness and isolation, possibly mitigating the negative impact of COVID-19 on adolescent mental health.
4.1. Limitations
Analyses were cross-sectional, limiting our ability to draw conclusions about causality or directionality. The timeframe for the 2020 sample spanned a period during which COVID-19 restrictions varied (Fig. 1). There may be nuances in the associations between stressors and SI depending on pandemic phase. The relatively modest sample size limits our ability to examine these intricacies. At the time of study initiation, there were no reliable and valid measures of COVID-related stressors and SI. Our measure has high face validity but has not been psychometrically examined.
Results indicated that more SI and SA were endorsed during COVID-19 compared to the year prior. It is possible that this is a reflection of the acuity of adolescents admitted during the pandemic (i.e., those with symptoms severe enough to come to an environment of congregate living during a time when social distancing was strongly promoted), rather than a reflection of increased suicidality per se. Nonetheless, this finding indicates that the hospital was serving a more psychiatrically acute, high-risk population during the pandemic.
5. Conclusions
Through historical chart review, this study offers preliminary evidence that the COVID-19 pandemic may be contributing to greater suicidal thoughts and behaviors in high-risk adolescents. Overall, missing special events appears to be a stressor moderately associated with COVID-related SI in this sample of psychiatrically hospitalized youth. Financial stressors and conflict or changes in the home were also associated with COVID-SI, with small effects. For adolescents admitted to a psychiatric hospital for the first time during the pandemic, interpersonal COVID-related stressors may be particularly difficult to cope with, as these stressors were moderately associated with SI. These findings underscore the need for prevention efforts aimed at mitigating the effects of social isolation and loneliness in this age group.
Funding
Drs. Thompson and Burke were supported by the National Institutes of Mental Health [K23 MH119211 and T32 MH019927, respectively]. Dr. Thomas was supported in part by Institutional Development Award Number U54GM115677 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds Advance Clin- ical and Translational Research (Advance-CTR). The funding agencies had no role in the design and conduct of the study; collection, manage- ment, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. The content is solely the responsibility of the authors.
Declaration of Competing Interest
The authors have no conflicts of interest to disclose.
References
- Ammerman B., Burke T., Jacobucci R., McClure K. Preliminary investigation of the association between COVID-19 and suicidal thoughts and behaviors in the U.S. J. Psychiatr. Res. 2020;134:32–38. doi: 10.31234/osf.io/68djp. [DOI] [PubMed] [Google Scholar]
- Chahal R., Kirshenbaum J.S., Miller J.G. Higher executive control network coherence buffers against puberty-related increases in internalizing symptoms during the COVID-19 pandemic. Biol Psychiatry Cogn Neurosci Neuroimaging. 2020;6(1):79–88. doi: 10.1016/j.bpsc.2020.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan S.M.S., Chiu F.K.H., Lam C.W.L. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int. J. Geriatr. Psychiatry. 2006;21(2):113–118. doi: 10.1002/gps.1432. [DOI] [PubMed] [Google Scholar]
- Cohen R.I., Bosk E.A. Vulnerable youth and the COVID-19 pandemic. Pediatrics. 2020;146(1) doi: 10.1542/peds.2020-1306. [DOI] [PubMed] [Google Scholar]
- COVID ActNow, 2020. Rhode Island. https://.covidactnow.org/us/rhode_island-ri/?s=1508461
- Czeisler M.É., Lane R.I., Petrosky E. 2020. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States; p. 69. MMWR. Morbidity and Mortality Weekly Report. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis W.E., Dumas T.M., Forbes L.M. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can. J. Behav. Sci. 2020;52(3):177. [Google Scholar]
- Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174(9):819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades M.E., Chatburn E., Higson-Sweeney N. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry. 2020;59(11):1218–1239. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds W.M. Psychological Assessment Resources; Odessa, FL: 1987. Suicidal Ideation Questionnaire- Junior. [Google Scholar]
- Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113(10):707–712. doi: 10.1093/qjmed/hcaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang S., Xiang M., Cheung T., Xiang Y.T. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J. Affect. Disord. 2020;279:353–360. doi: 10.1016/j.jad.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman I.M. The impact of epidemic, war, prohibition and media on suicide: United States, 1910-1920. Suicide Life Threat Behav. 1992;22:240–254. [PubMed] [Google Scholar]


