Abstract
Background: Resilience is a process that allows recovery from or adaptation to adversities. The aim of this study was to evaluate state resilience during the COVID-19 pandemic in psychiatric patients (PP), unaffected relatives (UR) and community controls (CC).
Methods: This study is part of the Barcelona ResIlience Survey for Mental Health COVID-19 (BRIS-MHC) project. Logistic regression models were performed to identify mental health outcomes associated with bad state resilience and predictors of good state resilience. The association between state resilience and specific affective temperaments as well as their influence on the association between depressive symptoms and state resilience were verified.
Results: The study recruited 898 participants that took part in the survey. The presence of depressive symptoms was a predictor of bad state resilience in PP (β=0.110, OR=1.117, p=0.028). No specific mental health outcome was associated with bad state resilience in UR and CC. Predictors of good state resilience in PP were having pursued hobbies/conducted home tasks (β=1.261, OR=3.528, p=0.044) and level of organization in the family (β=0.986, OR=2.682, p=0.008). Having a controlling family was inversely associated with good state resilience in CC (β=-1.004, OR=0.367, p=0.012). The association between bad state resilience and depressive symptoms was partially mediated by affective temperaments.
Limitations: Participants self-reported their psychiatric diagnoses, their relatives’ diagnoses or the absence of a psychiatric disorder, as well as their psychiatric symptoms.
Conclusions: Enhancing resilience and coping strategies in the face of the COVID-19 pandemic might have important implications in terms of mental health outcomes.
Keywords: COVID-19, resilience, mental health, coping strategies, affective temperaments
1. Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic caused by the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) virus is a global health threat (Wang et al., 2020). In order to overcome the contagion situation, the governments of different European countries imposed a lockdown. By March 18, 2020, it was applied to more than 250 million people in Europe (Henley, 2020).
Great concern exists about the psychological consequences of the pandemic, in terms of the short- and long-term impact on the mental health of both the general population and, particularly, of individuals already suffering from a psychiatric disease (Moreno et al., 2020; Vieta et al., 2020).
According to recent meta-analyses, the prevalence of stress, anxiety, and depression in the general population as a result of the pandemic in the general population is around 30% (Luo et al., 2020; Salari et al., 2020). A Spanish online survey (González-Sanguino et al., 2020) revealed that specific factors, such as being in the older age group and having economic stability were negatively related to symptoms of depression, anxiety and post-traumatic stress disorder (PTSD).
It has been proved that some individuals are more psychologically resilient to adversity than others and that patterns of vulnerability or resilience differ (Sominsky et al., 2020). Literature has consistently demonstrated an inverse relationship between psychological resilience and psychological distress, particularly in the case of natural disasters, such as the 2010 Haiti Earthquake (Blanc et al., 2016) or the 2005 Hurricane Katrina (Osofsky and Osofsky, 2013).
State resilience is a process that comprises: 1) Immunity, stable and undisturbed mental health in the presence of a prolonged period of adversity (Ayed et al., 2019); 2) Bouncing back, a trajectory of bouncing back from adversity, regaining the former mental stability after a stressful period or event (Amering, M., & Schmolke, 2009) and 3) Growth, when the person does not return to a previous level of functioning but is doing even better than before the adversity occurred (Ayed et al., 2019). Also, the individual could have personality traits such as motivation, hope, humour or talents, skills and interests that may protect from life difficulties. Resilience also relies on functional, supporting and meaningful social networks and positive bonds (Ayed et al., 2019).
Resilience is a dynamic process of adaptation to challenging life conditions encompassing several aspects of personal resources and is considered to be protective against mental disorders (Kim-Cohen, 2007).
Two U.S. national surveys evaluated trait resilience in the general population during the COVID-19 pandemic (Killgore et al., 2020; Liu et al., 2020). Since resilience is an active process, correlates of state resilience should be also evaluated in the face of the current pandemic, particularly in patients suffering from a psychiatric disorder.
Another important aspect that could be associated with resilience and adaptation to the COVID-19 pandemic is represented by affective temperaments. Temperaments are conceived as early-appearing individual differences in emotional reactivity, with strong biological underpinnings and stability across the lifespan (Moccia et al., 2020). Since affective temperaments might mediate adaptive functioning, promoting better or worse coping mechanisms to environmental stressors (Akiskal and Akiskal, 2005), they might influence resilience or mediate its effects on the development of psychiatric symptomatology.
The present study was aimed at evaluating state resilience during the COVID-19 pandemic in psychiatric patients, unaffected relatives and community controls. We sought to identify mental health outcomes associated with bad state resilience and predictors of good state resilience in those three groups. We also assessed the association between state resilience and specific affective temperaments. Finally, we evaluated if the association between depressive symptoms and bad state resilience was mediated by affective temperaments in the different subgroups.
2. Methods
This study is part of the Barcelona ResIlience Survey for Mental Health COVID-19 (BRIS-MHC) project, whose aim was to assess whether the lockdown measures were more aversive for individuals with a previous psychiatric disorder (Solé et al., 2021).
It received ethics approval from the Hospital Clínic de Barcelona Ethics Committee and the authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
2.1. Design
The characteristics of the BRIS-MHC project have been described elsewhere (Solé et al., 2021). Briefly, Spanish citizens aged over 18 years were invited to complete the survey over a time period (14th May to 8th June 2020), during the lockdown due to the pandemic in Spain, with different levels of restrictions (stage 1 or 2) and after six months will be contacted for a follow-up online survey. Baseline findings on state resilience are reported in the present study.
Patients suffering from a psychiatric disorder, their unaffected relatives and the general population were invited to complete the survey. The survey was conducted using the online anonymous survey system of Hospital Clinic of Barcelona through a multiple step procedure: a) e-mail invitation to patients visited at the Mental Healthcare of the Hospital Clinic of Barcelona, b) dissemination of the link through social media and other advertisements c) involvement of national associations of stakeholders (e.g., associations of users/caregiver). The snowball sampling procedure gave us the opportunity to recruit a larger sample of the Spanish population.
Most of the psychiatric patients who participated in the BRIS-MHC belong to the Bipolar and Depressive and Schizophrenia Unit of the Hospital Clinic with the diagnoses verified by a medical professional, for the rest of the participants, the diagnoses were self-reported as interviews were not feasible at this time frame. The survey included one question asking whether participants had a psychiatric disorder (or a relative suffering from psychiatric disorders), and if so, which psychiatric disorder they had and when they were diagnosed. Patients with different long-lasting psychiatric disorders, such as major depressive disorder, anxiety disorders, bipolar disorder or schizophrenia were included in the survey as well as patients presenting a first episode of psychosis or mania in the last 5 years.
2.2. Participants
A total of 898 participants took part in the survey. Participants have been divided into three groups: psychiatric patients (PP), unaffected relatives (UR), and community controls (CC). Reasons for exclusion are reported in Supplementary Figure 2. The final sample consisted of 530 participants, 174 (32.8%) PP, 83 (15.7%) UR and 273 (51.5%) CC.
2.3. Measures
All relevant measures, socio-demographic data and information related to COVID-19 were fully described in the seminal article of the group (Solé et al., 2021). The entire survey took approximately 15-20 minutes to complete and covered nine broad topics: a) depression and anxiety, b) trauma experiences, c) psychotic-like experiences, d) resilience (state and trait), e) affective temperament, f) perceived family environment, g) cognition, h) cognitive reserve and i) physical aggressiveness. Measures are summarized in the Appendix A.
As for state resilience, which was the focus of the present BRIS-MHC study, it was evaluated on the basis of six yes/no items derived from the Brief Resilience Scale (BRS) (Smith, 2008). The BRS assesses the original and most basic meaning of the word resilience, namely the ability to bounce back or recover from stress. There are six-items, half of which are negatively focused and half positively focused. Inverted items were turned into positive answers. If the participants scored yes on zero to two items they were considered to have “bad state resilience”. If they scored yes on four to six items “good state resilience” was assumed. If the participants scored yes on three items, they were considered to have “neutral state resilience”.
Patients visiting the Mental Healthcare facilities of the Hospital Clinic of Barcelona were also asked about the duration of their psychiatric condition, about their need for an urgent visit to the community mental health service during the quarantine, and about whether they decided to stop taking psychiatric medications during the lockdown. Furthermore, the participants were asked about their family history of psychiatric disorders (first and second degree) and if they live together with someone suffering from any psychiatric condition. Lastly, all participants were asked if they needed any visits to the psychiatric emergency room, had been admitted to the psychiatric ward, or had attempted suicide during the lockdown.
2.4. Statistical analyses
The three subgroups (PP, UR and CC) were described in terms of percentages of good or bad state resilience.
Independent variables were divided in two groups, those indicating mental health outcomes (depressive, anxiety or psychotic-like experiences) and those representing predictors of good resilience, such as coping strategies and family environment.
Within each subgroup (PP, UR and CC), differences in these variables were examined between those with bad or good state resilience. Chi-square test (X2) or Fisher's exact test (F) were used for dichotomous or ordinal variables. The strength of the association was measured by Phi and Cramer's V. For continuous variable, normality of distribution was assessed. Unpaired t-tests (t) were used for comparisons. Effect sizes were calculated for continuous variables as Hedges' g value (Hedges, 1981; Hedges and Olkin, 1985).
Two multiple logistic regression models were performed for each subgroup. The first one included significant mental health outcomes (independent variables) in the bivariate analyses associated with bad state resilience (dependent variable). Variables related to COVID-19 were entered as covariates in the model (if significant) in order to control for stressors related to COVID-19. The second model involved significant predictors (independent variables) of good state resilience (dependent variable). A final hierarchical logistic regression model was built to identify, controlling for being part of the three subgroups, which psychiatric symptoms were associated with bad state resilience. All tolerance values in the logistic regression analyses were > 0.2 and all variance inflation factors were < 2, thereby indicating that multicollinearity was not a source of bias (Yoo et al., 2014) .
The association between state resilience (dependent variable) and affective temperaments (independent variables) was explored in a hierarchical logistic regression model, controlling for the type of subgroup.
The mediation of affective temperaments on the association between depressive symptoms and bad state resilience was also assessed through mediation analyses (Baron and Kenny, 1986). In the first instance, the dependent variable (depressive symptoms) was regressed onto the independent variable (state resilience) (path c). In the second equation, the mediator variables (temperaments) were regressed onto the independent variable (state resilience) (path a). Finally, the dependent variable was regressed onto the independent variable, adjusted for the mediator (path b and c’) (Supplementary Figure 1). Hence, if the independent variable is no longer significant when the mediator is controlled, the finding supports full mediation. If the independent variable is still significant, the finding supports partial mediation.
All p-values were two-tailed and statistical significance was set at p<0.05. Statistical analyses were performed using the Statistical Package for Social Sciences (SPSS, 23.0 version for Windows).
3. Results
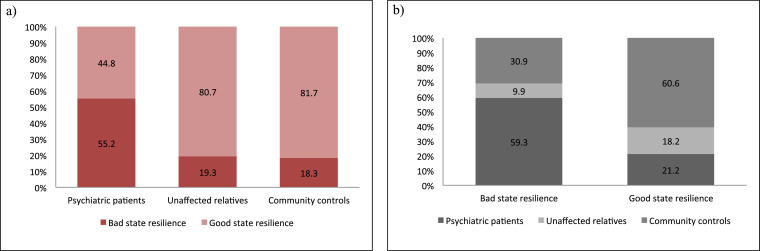
The three subgroups (PP n=174, 32.8%, UR n=83 (15.7%), and CC n=273, 51.5%) were significantly different in terms of state resilience (X2=85.510, p<0.001, phi=0.389) (Figure 1 ). PP significantly differed from both UR (X2=28.006, p<0.001, phi=0.338) and CC (X2=63.972, p<0.001, phi=0.383). There were no differences between UR and CC in relation to state resilience (X2=0.001, p=0.971, phi=-0.010).
Figure 1.
Differences in bad and good state resilience among subgroups a) Differences within subgroups b) Differences within state resilience
Socio-demographic, lockdown and COVID-19 related variables are reported for the three subgroups in the Supplementary Table 1. The three groups did not show significant differences in terms of bad or good state resilience regarding socio-demographic, lockdown and COVID-19 related variables. Only the PP group displayed a significant difference in bad versus good state resilience between those who experienced unpleasant events during lockdown and those who did not (p=0.020, phi=-0.192).
3.1. Mental health outcomes of bad state resilience
Results for mental health outcomes are reported in Table 1 . Particularly, differences in anxious symptoms were only present in CC (p=0.042, g=0.325). Differences in depressive symptoms were present in the three groups, with a larger effect size for UR (PP: p=<0.001, g=0.749; UR: p=<0.001, g=0.973; CC: p=<0.001, g=0.815). As for positive psychotic-like experiences, differences were reported for the three subgroups, with a larger effect size for CC (PP: p=0.020, g=0.349; UR: p=0.038, g=0.588; CC: p=0.003, g=0.734). Differences in negative psychotic-like experiences were reported only for PP and CC, with a larger effect size for CC (PP: p<0.001, g=0.592; CC: p<0.001, g=0.820).
Table 1.
Association between bad state resilience and mental health outcomes
| Psychiatric patients | Unaffected relatives | Community controls | |||||||
|---|---|---|---|---|---|---|---|---|---|
| State resilience | Bad (n=96) | Good (n=78) | Bad (n=16) | Good (n=62) | Bad (n=50) | Good (n=223) | |||
| Psychiatric variables | n (%) | n (%) | X2 or F, p | n (%) | n (%) | X2 or F, p | n (%) | n (%) | X2 or F, p |
| Sleep routine changes | 9.177, 0.011 | 1.276, 0.619 | 16.168, < 0.001 | ||||||
| With difficulties in sleeping | 66 (68.8) | 36 (46.2) | 10 (62.5) | 31 (46.3) | 38 (76) | 101 (45.3) | |||
| No difficulties in sleeping | 16 (16.7) | 21 (26.9) | 2 (12.5) | 15 (22.4) | 5 (10) | 46 (20.6) | |||
| No changes | 14 (14.6) | 21 (26.9) | 4 (25) | 21 (31.3) | 7 (14) | 76 (34.1) | |||
| Sleep-onset insomnia | 23 (24) | 13 (14.7) | 0.985, 0.321 | 6 (37.5) | 8 (11.9) | 6.017, 0.024 | 16 (32) | 40 (17.9) | 4.129, 0.042 |
| Sleep-maintenance insomnia | 33 (34.4) | 16 (20.5) | 3.431, 0.064 | 5 (31.25) | 20 (29.9) | 0.012, 1.000 | 18 (36) | 43 (19.3) | 5.650, 0.017 |
| Early morning wakening insomnia | 12 (12.5) | 10 (12.8) | 0.000, 1.000 | 2 (12.5) | 7 (10.5) | 0.056, 1.000 | 10 (20) | 23 (10.3) | 2.752, 0.097 |
| Going to bed later than usual | 36 (37.5) | 17 (21.8) | 4.297, 0.038 | 5 (31.25) | 15 (22.4) | 0.555, 0.519 | 12 (24) | 40 (17.9) | 0.620, 0.431 |
| Waking-up tired | 36 (37.5) | 13 (16.7) | 8.232, 0.004 | 3 (18.75) | 10 (14.9) | 0.143, 0.708 | 10 (20) | 22 (9.9) | 3.134, 0.077 |
| Physical aggressiveness (yes) | 6 (6.3) | 4 (5.1) | 0.111, 1.000 | 1 (6.3) | 2 (3) | 0.395, 0.479 | 2 (4.1) | 4 (1.8) | 0.964, 0.297 |
| Trauma experiences | |||||||||
| Re-experience† | 3.83 (3.041) | 2.83 (2.552) | 1.004, 0.321 | 1 (1.732) | 2.40 (1.713) | -1.239, 0.241 | 3.18 (4.143) | 1.59 (1.998) | 1.223, 0.245 |
| Dissociative symptoms (yes) | 3 (10) | 0 | 1.292, 0.545 | 0 | 0 | - | 2 (18.2) | 1 (3.1) | 2.860, 0.156 |
| Psychotic-like experiences | |||||||||
| Positive psychotic-like experiences† | 1.78 (2.095) | 1.13 (1.532) | 2.340, 0.020 | 1.69 (1.662) | 0.97 (1.101) | 2.106, 0.038 | 1.65 (2.067) | 0.71 (1.529) | 3.111, 0.003 |
| Negative psychotic-like experiences† | 1.97 (1.888) | 1 (1.269) | 4.016, <0.001 | 1.31 (1.352) | 0.87 (1.057) | 1.436, 0.154 | 1.70 (1.529) | 0.75 (1.058) | 4.173, <0.001 |
| Depressive symptoms† | 8.71 (5.895) | 4.92 (3.850) | 4.972, <0.001 | 7.63 (4.884) | 4.29 (2.993) | 3.478, <0.001 | 6.47 (3.906) | 3.81 (3.095) | 5.139, <0.001 |
| Anxious symptoms† | 5.58 (2.237) | 5.10 (1.885) | 1.455, 0.148 | 5.56 (1.825) | 5.23 (1.669) | 0.691, 0.492 | 5.33 (1.853) | 4.74 (1.804) | 2.039, 0.042 |
| Visit to psychiatric emergency rooms (yes) | 1 (1.1) | 3 (3.9) | 1.514, 0.326 | 0 | 4 (6.1) | 1.019, 0.581 | 0 | 4 (1.8) | 0.754, 1.000 |
| Need a first visit with psychiatrist or psychologist (yes) | - | - | - | 3 (18.8) | 6 (10) | 0.840, 0.359 | 3 (7.9) | 16 (7.4) | 0.013, 1.000 |
| Psychiatric admission (yes) | 1 (1.1) | 2 (2.6) | 0.592, 0.587 | 0 | 1 (1.5) | 0.245, 1.000 | 0 | 1 (0.5) | 0.185, 1.000 |
| Suicide attempt (yes) | 1 (1.1) | 0 | 0.815, 1.000 | 0 | 1 (1.5) | 0.245, 1.000 | 0 | 1 (0.4) | 0.187, 1.000 |
† continuous variable, M (mean) and SD (standard deviation) reported with t- and p-values.
Differences in sleep routine changes between those with bad versus good state resilience were reported by both PP (p=0.011, phi=0.229) and CC (p< 0.001, phi=0.238). As for the PP subgroup, differences were reported mainly in the sleep patterns characterized by going to bed later than usual (p=0.038, phi=-0.170) and waking-up tired (p=0.004, phi=-0.230), with a bigger effect size for the latter. Sleep-onset (p=0.042, phi=-0.135) and sleep-maintenance (p=0.017, phi=-0.155) insomnia presented a bigger effect size in the CC subgroup. Sleep-onset insomnia was also reported by UR (p=0.024, phi=-0.269).
No differences existed among participants with bad or good state resilience in the three different subgroups in terms of changes in sexual activity or drug consumption (tobacco, alcohol or cannabis).
In the PP group, but not in the UR (X2=0.747, p=0.772) and CC groups (X2=1.599, p=0.450), there were differences among participants in their expectations about the future (X2=10.903, p=0.004, phi=0.245), with more patients with bad state resilience having the sensation that things will take a long time to recover (bad state resilience n=18, 19.1% versus good state resilience 4, 5.2%) whilst those with good state resilience had a more optimistic attitude (bad state resilience n=8, 8.5% versus good state resilience 15, 19.5%).
As for the PP subgroup, a hierarchical logistic regression model was built and the variable of having suffered unpleasant events during lockdown was entered at Step 1 in order to control for stressors related to COVID-19. After including mental health outcomes at Step 2 (X2 (df=6)=29.283, p<0.001), the strongest predictor of bad state resilience in PP was represented by depressive symptoms (OR=1.117, β=0.110, p=0.028). Direct logistic regression models were built for both UR (X2 (df=3)=12.299, p=0.006) and CC (X2 (df=6)=33.965, p<0.001). No statistically significant predictor of bad state resilience in UR or CC emerged.
The final hierarchical logistic regression model built to assess specific psychiatric symptoms associated with bad state resilience, controlling for being a member of one of the three subgroups (PP, UR, CC) (X2 (df=7)=125.595, p<0.001), revealed that depressive (β=0.176, OR=1.193, p<0.001) and negative psychotic-like experiences (β=0.213, OR=1.238, p=0.028) were significantly associated with bad state resilience.
3.2. Predictors of good state resilience
A positive family environment in comparison with a negative or a neutral family environment seemed to correlate with good state resilience both in PP (X2=10.437, p=0.006, phi=0.249) and CC (X2=8.407, p=0.015, phi=0.191) but not in UR (X2=0.250, p=0.924), with a bigger effect size for PP than for CC (Table 2 ).
Table 2.
Family environmental styles and coping strategies during lock/down associated with good state resilience
| Psychiatric patients | Unaffected relatives | Community controls | |||||||
|---|---|---|---|---|---|---|---|---|---|
| State resilience | Bad (n=96) | Good (n=78) | Bad (n=16) | Good (n=62) | Bad (n=50) | Good (n=223) | |||
| Variables (yes) | n (%) | n (%) | X2 or F, p | n (%) | n (%) | X2 or F, p | n (%) | n (%) | X2 or F, p |
| Family environmental styles | |||||||||
| Cohesion (C) | 75 (85.2) | 70 (95.9) | 3.948, 0.047 | 13 (81.3) | 61 (95.3) | 3.649, 0.091 | 43 (93.5) | 206 (96.3) | 0.724, 0.417 |
| Expressivity (EX) | 70 (80.5) | 63 (87.5) | 0.959, 0.327 | 14 (87.5) | 60 (92.3) | 0.376, 0.620 | 36 (78.3) | 199 (93.4) | 10.350, 0.003 |
| Conflicts (CON) | 28 (32.9) | 17 (24.3) | 1.007, 0.316 | 6 (37.5) | 11 (18) | 2.792, 0.172 | 15 (31.9) | 50 (23.9) | 0.906, 0.341 |
| Independence (IND) | 54 (64.3) | 46 (70.8) | 0.435, 0.510 | 11 (78.6) | 51 (81) | 0.041, 1.000 | 29 (63) | 177 (86.3) | 12.321, <0.001 |
| Achievement Orientation (AO) | 68 (80) | 61 (87.1) | 0.938, 0.333 | 14 (87.5) | 59 (90.8) | 0.154, 0.654 | 42 (93.3) | 204 (97.6) | 2.218, 0.152 |
| Intellectual-Cultural Orientation (ICO) | 59 (66.3) | 53 (74.6) | 0.945, 0.331 | 12 (75) | 54 (81.8) | 0.391, 0.503 | 32 (71.1) | 183 (84.3) | 3.573, 0.059 |
| Active-Recreational Orientation (ARO) | 28 (32.2) | 33 (48.5) | 3.615, 0.057 | 9 (64.3) | 42 (64.6) | 0.001, 1.000 | 31 (72.1) | 143 (68.1) | 0.112, 0.738 |
| Moral-Religious Emphasis (MRE) | 70 (81.4) | 63 (90) | 1.640, 0.200 | 15 (93.8) | 57 (89.1) | 0.313, 1.000 | 33 (73.3) | 178 (86) | 3.467, 0.063 |
| Organization (ORG) | 28 (32.9) | 37 (56.1) | 7.184, 0.007 | 7 (43.8) | 30 (47.6) | 0.001, 1.000 | 15 (33.3) | 96 (48) | 2.625, 0.105 |
| Control (CTL) | 22 (25) | 10 (14.1) | 2.273, 0.132 | 5 (33.3) | 21 (33.3) | 0.001, 1.000 | 19 (39.6) | 31 (14.8) | 13.859, <0.001 |
| Coping strategies during lock-down | |||||||||
| Follow a routine | 63 (66.3) | 60 (77.9) | 2.271, 0.126 | 12 (75) | 56 (83.6) | 0.642, 0.474 | 43 (86) | 194 (88.2) | 0.035, 0.852 |
| Talk to relatives/friends | 90 (53.9) | 77 (98.7) | 1.335, 0.379 | 16 (100) | 67 (100) | - | 49 (98) | 221 (100) | 4.436, 0.185 |
| Physical exercise | 63 (67) | 56 (73.7) | 0.599, 0.439 | 13 (81.3) | 60 (89.6) | 0.840, 0.397 | 44 (91.7) | 176 (80.4) | 2.731, 0.098 |
| Healthy/balanced diet | 70 (76.1) | 68 (88.3) | 3.406, 0.065 | 13 (81.3) | 56 (89.4) | 0.798, 0.401 | 43 (91.5) | 184 (84.8) | 0.936, 0.333 |
| Drink water to hydrate | 86 (91.5) | 72 (92.3) | 0.000, 1.000 | 12 (75) | 57 (85.1) | 0.935, 0.456 | 45 (90) | 195 (88.2) | 0.012, 0.914 |
| Being updated about COVID-19 with media exposure | 62 (66.7) | 44 (56.4) | 1.484, 0.223 | 8 (53.3) | 42 (63.6) | 0.549, 0.559 | 26 (54.2) | 145 (65.6) | 1.763, 0.184 |
| Pursue hobbies or conduct home tasks | 67 (71.3) | 69 (88.5) | 6.604, 0.010 | 11 (68.8) | 52 (77.6) | 0.555, 0.519 | 38 (77.6) | 183 (83.2) | 0.525, 0.469 |
| Do relaxing activities | 68 (73.9) | 68 (87.2) | 3.851, 0.050 | 13 (81.3) | 51 (78.5) | 0.060, 1.000 | 38 (79.2) | 171 (78.1) | 0.000, 1.000 |
F=Fisher's exact test
Specifically, in the PP subgroup, cohesion (C) (X2=3.948, p=0.047, phi=0.177) and organization (ORG) (X2=7.184, p=0.007, phi=0.232) in the family correlated with good state resilience. As for CC, a family environment characterized by expressivity (EX) (X2=10.350, p=0.003, phi=0.200) and independence (IND) (X2=12.321, p<0.001, phi=0.235) correlated with good state resilience. Inversely, a family environment perceived by the individual as controlling (control – CTL) (X2=13.859, p<0.001, phi=-0.244) was more reported by CC as correlating with bad state resilience. No differences in perceived family environment were found between good and bad state resilience in UR.
As for coping strategies during the lock-down, those PP with good state resilience reported having pursued hobbies or conducted home tasks (X2=6.604, p=0.010, phi=0.210), or having participated in relaxing activities (X2=3.851, p=0.050, phi=0.165), more than those with bad state resilience, with a bigger effect size for the former coping strategy. No specific coping strategy was found to be associated with differences between participants with good or bad state resilience in CC and UF.
In the hierarchical logistic regression model built for the PP subgroup (X2 (df=5)=25.319, p<0.001), the strongest predictor of good state resilience in PP was having pursued hobbies or conducted home tasks (β=1.261, OR=3.528, p=0.044), followed by organization in the family environment (β=0.986, OR=2.682, p=0.008). On the contrary, having suffered unpleasant events during lockdown was inversely associated with good state resilience (β=-1,038, OR=0.354, p=0.030). As for CC (X2 (df=3)=19.918, p<0.001), having a controlling family (CTL) was inversely associated with good state resilience in CC (β=-1.004, OR=0.367, p=0.012).
3.3. Affective temperaments and state resilience
As for the association between state resilience and affective temperaments (X2 (df=7, n=475)=113.848, p<0.001), after controlling for being a member of the three subgroups, the anxious (β=0.714, OR=2.043, p=0.017) and cyclothymic (β=0.898, OR=2.455, p=0.003) temperaments were significantly associated with bad state resilience. On the other hand, the hyperthymic temperament (β=-0.663, OR=0.515, p=0.007) was associated with good state resilience.
Mediation of affective temperaments on the association between bad state resilience and depressive symptoms
For the PP subgroup, resilience was partially mediated by all the temperaments (Table 3 , analysis 3). The temperament that exerted the strongest effect was the dysthymic temperament. The hyperthymic temperament was negatively associated with depressive symptoms. For CC, resilience was also partially mediated by all the temperaments, with the strongest effect exerted by the cyclothymic and the irritable temperaments. For UR, resilience was partially mediated by the cyclothymic and the dysthymic temperaments, with a stronger effect exerted by the latter.
Table 3.
Mediation of affective temperaments on the association between bad state resilience and depressive symptoms
| Psychiatric patients | Unaffected relatives | Community controls | |||||||
|---|---|---|---|---|---|---|---|---|---|
| aR2 | ß | p | aR2 | ß | p | aR2 | ß | p | |
| Analysis 1 (path c) | |||||||||
| Predictor: State Resilience Outcome: Depressive symptoms | 0.118 | 0.351 | <0.001 | 0.122 | 0.364 | 0.001 | 0.090 | 0.306 | <0.001 |
| Analysis 2 (path a) | |||||||||
| Predictor: State Resilience | |||||||||
| Outcome: Cyclothymic | 0.130 | 0.368 | <0.001 | 0.072 | 0.288 | 0.009 | 0.029 | 0.182 | 0.003 |
| Outcome: Dysthymic | 0.152 | 0.396 | <0.001 | 0.080 | 0.303 | 0.007 | 0.045 | 0.220 | <0.001 |
| Outcome: Irritable | 0.076 | 0.285 | <0.001 | 0.017 | 0.130 | 0.240 | 0.040 | 0.208 | 0.001 |
| Outcome: Hyperthymic | 0.086 | -0.302 | <0.001 | 0.007 | -0.140 | 0.221 | 0.013 | -0.130 | 0.036 |
| Outcome: Anxious | 0.087 | 0.303 | <0.001 | 0.011 | 0.153 | 0.172 | 0.014 | 0.135 | 0.027 |
| Analysis 3 (path b and c’) | |||||||||
| Predictor: State Resilience | |||||||||
| Mediator: Cyclothymic | 0.262 | 0.413 | <0.001 | 0.272 | 0.013 | 0.203 | 0.346 | <0.001 | |
| Outcome: Depressive symptoms | 0.199 | 0.006 | 0.180 | 0.286 | 0.009 | 0.243 | <0.001 | ||
| Mediator: Dysthymic | 0.319 | 0.492 | <0.001 | 0.325 | 0.003 | 0.185 | 0.321 | <0.001 | |
| Outcome: Depressive symptoms | 0.156 | 0.028 | 0.208 | 0.266 | 0.015 | 0.235 | <0.001 | ||
| Mediator: Irritable | 0.323 | 0.476 | <0.001 | NA | 0.202 | 0.346 | <0.001 | ||
| Outcome: Depressive symptoms | 0.216 | 0.002 | 0.234 | <0.001 | |||||
| Mediator: Hyperthymic | 0.136 | -0.160 | 0.040 | NA | 0.101 | -0.123 | 0.046 | ||
| Outcome: Depressive symptoms | 0.303 | <0.001 | 0.290 | <0.001 | |||||
| Mediator: Anxious | 0.334 | <0.001 | NA | 0.153 | 0.260 | <0.001 | |||
| Outcome: Depressive symptoms | 0.215 | 0.250 | 0.001 | 0.271 | <0.001 | ||||
β=standardized values, aR2=variance, NA=not associated
4. Discussion
In the present study of the BRIS-MHC project, PP reported higher rates of bad state resilience in comparison with both CC and UR. Inversely, no differences in state resilience were found in the comparison between CC and UR. PP who reported bad state resilience, but not CC and UR, also revealed having experienced unpleasant events during lockdown. Even after controlling for the effect exerted by lockdown unpleasant events, in the PP subgroup bad state resilience was found to be positively associated with depressive symptoms. No mental health outcome was found to be associated with bad state resilience both in the CC and in the UR subgroups. Independently from the subgroup, depressive and negative psychotic-like experiences were associated with bad state resilience. As for coping strategies and family environmental styles associated with good state resilience, a more organized family environment and having pursued hobbies or conducted home tasks represented predictors of good state resilience in PP. As for CC, a less controlling family environment represented a predictor of good state resilience. As for the relationship between specific affective temperaments and state resilience, independently from the subgroup, the cyclothymic and the anxious temperaments were associated with bad state resilience whilst the hyperthymic temperament with good state resilience. In the three subgroups, the association between resilience and depressive symptoms was partially mediated by temperaments. That is, even after controlling for these variables, the effect of bad state resilience on the presence of depressive symptoms remained significant. In PP, the temperament that exerted the strongest effect on depressive symptoms was the dysthymic temperament, whilst the hyperthymic temperament was negatively associated with depressive symptoms. In CC, the strongest effects were exerted by the cyclothymic and the irritable temperaments. Meanwhile, in UR the dysthymic temperament exerted a stronger effect.
The highest frequencies of bad state resilience were reported by PP. In a previous studies, low levels of resilience were described in psychotic (Wambua et al., 2020) and depressive patients (Pardeller et al., 2020). In both cases (Pardeller et al., 2020; Wambua et al., 2020), poorer resilience was associated with poorer psychological function. Interestingly, resilience was found to be associated with improved longitudinal rates of recovery in patients who experienced a first-episode of psychosis (Torgalsbøen et al., 2018) and also in bipolar disorder patients (Echezarraga et al., 2018), underlining the importance of resilience and positive mental health outcomes in PP.
In the present BRIS-MHC study, mental health outcomes, particularly depressive symptoms and negative psychotic-like experiences, were associated with lower levels of resilience, independently from being a patient, a relative or a control. In a U.S. study (Killgore et al., 2020) assessing psychological resilience during the COVID-19 in the general population, lower scores on resilience were associated with worse mental health outcomes, including more severe depression and anxiety. Lower resilience was also associated with greater worry about the effects of COVID-19.
As for negative symptoms, a direct association between negative psychotic symptoms and bad resilience was not identified in previous literature (Poloni et al., 2018). Nonetheless, an indirect relationship between resilience and negative symptoms can be hypothesized since low resilience and higher negative symptomatology were directly associated with depression severity in psychotic patients (Rossi et al., 2017).
Another important BRIS-MHC finding was that the presence of depressive symptoms was a mental health outcome associated with bad state resilience in PP. In facing adversities, such as the unpleasant events that could have been experienced during the lockdown due to the COVID-19 pandemic, PP might be more vulnerable and might have experienced more psychological distress, particularly those with lower levels of resilience. Bad state resilience, specifically in PP, was found to be associated with higher rates of depressive symptoms, more frequent unpleasant events experienced during the lockdown, and the sensation that things will take a long time to recover. The lockdown imposed as a measure to reduce the transmission of the SARS-CoV-2, and the information on increasing numbers of new cases and deaths might have caused feelings of distress and despair, with increasing severity of depressive symptoms in PP (Marazziti and Stahl, 2020; Pacchiarotti et al., 2020). The association between depressive symptoms and resilience was already observed in patients suffering from a chronic physical disease (García-Carrasco et al., 2019) or who lived traumatic life experiences (Bernstein et al., 2017). Also, a significant relationship between low resilience and depressive symptoms was identified in patients recently discharged from an acute psychiatric unit (Mizuno et al., 2016) and in those suffering from bipolar disorder (BD) (Meyers et al., 2020) or schizophrenia (Rossi et al., 2017).
On the contrary, a positive family environment was a predictor of good state resilience in both PP and CC. In particular, good state resilience was associated with a more organized family environment in PP and a less controlling environment in CC. Prime and colleagues (Prime et al., 2020) studied risk and resilience factors associated with family well-being during the COVID-19 pandemic and underlined that vulnerabilities within families might increase the risk to the sequelae of the pandemic, whilst intact family styles would protect families from such stressors. Organization indicates a system maintenance mechanism associated with a better family environment (González-Pinto et al., 2011) and based on adaptability, connectedness, and access to social and economic resources. In university students, control in family was positively associated with depression (Yu et al., 2015). A previous study of our group identified that negative family styles were associated with worse functional outcomes after two years from a first-episode psychosis (Verdolini et al., 2021). Also, González-Pinto and colleagues (González-Pinto et al., 2011) found that over-control in the family could impact on the onset of psychosis. Also, the presence of controlling parents was associated with an increased overall risk of psychiatric symptoms in children (Young et al., 2011). In BD patients, individual psychosocial functioning positively correlated with cohesion within the family and negatively correlated with control (Reinares et al., 2016). As a consequence, it is easy to understand how a positive family environment might enhance resilience during a stressful situation, such as the COVID-19 pandemic, in both patients and the general population.
Another good state resilience predictor during the pandemic in PP was having pursued hobbies or conducted home tasks. A recent study identified that the most used coping strategies during the COVID-19 lockdown were watching television, listening to music, doing mundane house chores like cleaning and washing, among others (Aga et al., 2020). A Spanish online survey identified that following a routine and taking the opportunity to pursue hobbies were the best predictors of low levels of depressive symptoms in the general population during the lockdown (Fullana et al., 2020). This reinforces the concept of “positive psychiatry”, which is defined as the science and practice of psychiatry willing to understand and promote well-being in PP through interventions that involve positive psychosocial characteristics, such as personality traits (i.e. optimism) and environmental factors (i.e. social support) (Jeste et al., 2015). Lifestyle interventions for PP based on practicing exercise, meditation, mindfulness and yoga can help promoting well-being (Jeste et al., 2015). Indeed, most of the PP that participated in the BRIS-MHC learnt how to deal with stressful situations since they received psychoeducational advice from psychiatrists and psychologists at our institution.
As for affective temperaments, we identified that the cyclothymic and the anxious temperaments were associated with bad state resilience whilst the hyperthymic temperament with good state resilience, independently from the subgroups. In the seminal article on this survey (Solé et al., 2021), we already underlined how both the cyclothymic and the anxious temperaments display increased stress reactivity in daily life (Walsh et al., 2013). Conversely, the hyperthymic temperament could be protective against the development of psychological symptoms in the face of a stressful event. Indeed, a positive association between the hyperthymic temperament and resilience in major depressive disorder was previously identified (Kesebir et al., 2013). In addition, in the BRIS-MHC we detected that the association of bad state resilience with depressive symptoms in the three groups was only partially mediated by affective temperaments, particularly the dysthymic temperament in the PP and UR subgroups and the cyclothymic and irritable temperaments in CC. This is in line with the findings of a recent Italian study identifying that, in the general population during the COVID-19, the cyclothymic and the dysthymic temperaments were risk factors for moderate-to-severe psychological distress (Moccia et al., 2020).
The present BRIS-MHC study has limitations. First of all, the results may not be generalizable to all PP since results come from a voluntary online survey, and also are restricted to a specific geographical and sociocultural context. Even though most of the PP attended the Mental Healthcare facilities of the Hospital Clinic of Barcelona and were invited to complete the survey, they had to self-report their psychiatric diagnoses as well as their psychiatric symptoms. Similarly, UR and CC self-reported not suffering from a psychiatric disorder. In addition, this is a cross-sectional study, so the design precludes establishing causal inferences. We found no differences in terms of resilience according to working conditions (i.e. working or not remotely), to the risk of exposure to the virus or other COVID-19 related factors. This could be probably due to the high heterogeneity within the subgroups, particularly in the CC. Another explication can be that results might vary, depending on the different levels of restrictions. As for the UR subgroup, another important limitation was the small sample size. As a consequence, our findings need replication in studies with a larger sample size of UR. Lastly, our survey use proxies of different validated scales to make it easier for participants to answer and complete the survey, so results should be interpreted with caution.
The BRIS-MHC project wanted to provide a focus on resilience during the COVID-19 pandemic. Specific mental health outcomes associated with bad state resilience, particularly depressive symptoms in psychiatric patients, and predictors of good state resilience, such as family environmental styles and coping strategies, were identified. We also assessed the contribution of specific affective temperaments on the development of psychiatric symptomatology and their effect on resilience.
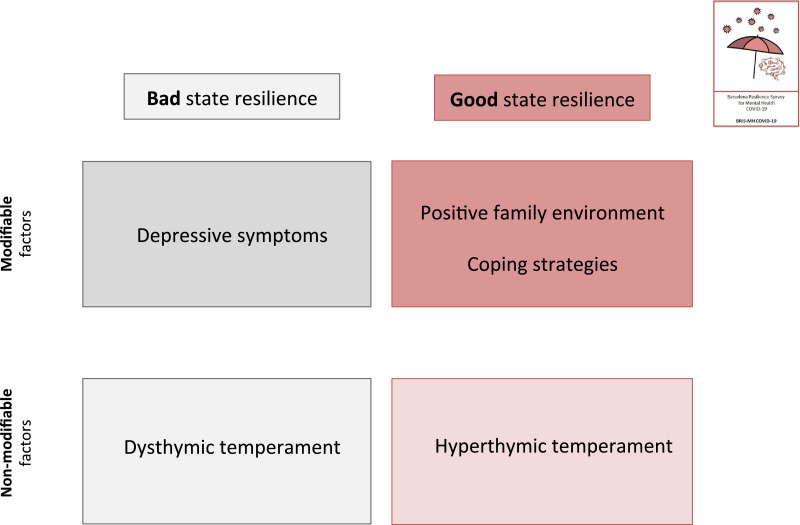
Since the evolution of the COVID-19 pandemic still remains unpredictable and little is known on the psychological impact on the long-term, enhancing resilience and coping strategies not only in the general population but specifically in patients already suffering from a psychiatric disorder should be an intervention target in the short-term. In particular, modifiable factors associated with resilience should be a major focus (Figure 2 ). For example, family interventions aimed at improving the family environment could be useful.
Figure 2.
Targets of resilience-based intervention for psychiatric patients in the Barcelona ResIlience Survey for Mental Health COVID-19 (BRIS-MHC) project
The development of on-line interventions focused on resilience and the availability of psychological/psychiatric assistance to help coping with stress during the COVID-19 pandemic and to face the long-term sequelae on personal functioning, quality of life and well-being, should be the gold standards of care.
Author Statement
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
We understand that the Corresponding Authors are the sole contacts for the Editorial process (including Editorial Manager and direct communications with the office). They are responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs. We confirm that we have provided a current, correct email address which is accessible by the Corresponding Authors and which has been configured to accept email from (evieta@clinic.cat, ctorrent@clinic.cat).
Author Contributions
Prof. Vieta and Dr. Torrent had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Verdolini, Amoretti, Montejo, Torrent, Solé and Vieta. Acquisition, analysis, or interpretation of data: Verdolini, Amoretti, Montejo, Torrent, Solé, Rabelo-da-Ponte and Vieta. Drafting of the manuscript: All authors. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Verdolini and Amoretti. Administrative, technical, or material support: Hogg, Mezquida, Verdolini, Amoretti, Montejo, Torrent and Solé.
Study supervision: García-Rizo, Martinez-Aran, Pacchiarotti, Rosa, Bernardo, Radua, Solé, Vieta and Torrent.
Funding
This work was supported by the Spanish Ministry of Science and Innovation, ISCIII, through a ‘Miguel Servet’ postdoctoral contract (CPI14/00175 to CT, MS14/00041 to JR) and the Miguel Servet II (CPII19/00018 to CT, CPII19/00009 to JR). The study has been supported by a BITRECS project conceded to NV. BITRECS project has received funding from the European Union's Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No 754550 and from “La Caixa” Foundation (ID 100010434), under the agreement LCF/PR/GN18/50310006. This work has also been supported by the projects SLT006/17/00357 and SLT006/17/00345 in the “Pla estrategic de Recerca i Innovacio en Salut 2016–2020” (Health Department), CERCA (Programme/Generalitat de Catalunya) and by the Spanish Ministry of Science and Innovation through a FIS project (PI18/01001) to IP.
Role of the Funding Source
The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Declaration-of-Competing-Interests
Dr. Vieta has received grants and served as consultant, advisor or CME speaker for the following entities (work unrelated to the topic of this manuscript): AB-Biotics, Abbott, Allergan, Angelini, AstraZeneca, Bristol-Myers Squibb, Dainippon Sumitomo Pharma, Farmindustria, Ferrer, Forest Research Institute, Gedeon Richter, GH Research, Glaxo-Smith-Kline, Janssen, Lundbeck, Otsuka, Pfizer, Roche, SAGE, Sanofi-Aventis, Servier, Shire, Sunovion, Takeda, the Brain and Behaviour Foundation, the Generalitat de Catalunya (PERIS), the Spanish Ministry of Science and Innovation (CIBERSAM), EU Horizon 2020, and the Stanley Medical Research Institute.
Dr Pacchiarotti has received CME-related honoraria, or consulting fees from ADAMED, Janssen-Cilag and Lundbeck.
Dr. Martínez-Aran has received funding for research projects and/or honoraria as a consultant or speaker for the following companies and institutions (work unrelated to the topic of this manuscript): Otsuka, Pfizer, AstraZeneca, Bristol-Myers Squibb, Lundbeck, the Spanish Ministry of Economy and Competitiveness and Instituto de Salud Carlos III.
Acknowledgments
The authors would like to thank the support of the Spanish Ministry of Science and Innovation; the CIBER of Mental Health (CIBERSAM); the Secretaria d'Universitats i Recerca del Departament d'Economia i Coneixement (2017 SGR 1365; 2017 SGR 1355) and the CERCA Programme / Generalitat de Catalunya.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.01.055.
Appendix. Supplementary materials
References
- Aga S.S., Khan M.A., Nissar S.S., Banday M.Z. Évaluation de la santé mentale et des diverses stratégies d'adaptation dans la population générale vivant sous l'emprise de la COVID à travers le monde : Une étude transversal. Ethics, Med. Public Heal. 2020 doi: 10.1016/j.jemep.2020.100571. [DOI] [Google Scholar]
- Akiskal K.K., Akiskal H.S. The theoretical underpinnings of affective temperaments: Implications for evolutionary foundations of bipolar disorder and human nature. J. Affect. Disord. 2005;85:231–239. doi: 10.1016/j.jad.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Amering M., Schmolke M. Recovery - basics and concepts. Recovery in Mental Health: Reshaping Scientific and Clinical Responsibilities. 2009:9–57. [Google Scholar]
- Ayed N., Toner S., Priebe S. Conceptualizing resilience in adult mental health literature: A systematic review and narrative synthesis. Psychol. Psychother. Theory, Res. Pract. 2019 doi: 10.1111/papt.12185. [DOI] [PubMed] [Google Scholar]
- Baron R.M., Kenny D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bernstein K., Park S.Y., Nokes K.M. Resilience and Depressive Symptoms among Korean Americans with History of Traumatic Life Experience. Community Ment. Health J. 2017;53:793–801. doi: 10.1007/s10597-017-0142-7. [DOI] [PubMed] [Google Scholar]
- Blanc J., Rahill G.J., Laconi S., Mouchenik Y. Religious Beliefs, PTSD, Depression and Resilience in Survivors of the 2010 Haiti Earthquake. J. Affect. Disord. 2016;190:697–703. doi: 10.1016/j.jad.2015.10.046. [DOI] [PubMed] [Google Scholar]
- Echezarraga A., Calvete E., González-Pinto A.M., Las Hayas C. Resilience dimensions and mental health outcomes in bipolar disorder in a follow-up study. Stress Heal. 2018;34:115–126. doi: 10.1002/smi.2767. [DOI] [PubMed] [Google Scholar]
- Fullana M.A., Hidalgo-Mazzei D., Vieta E., Radua J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Carrasco M., Mendoza-Pinto C., León-Vázquez J., Méndez-Martínez S., Munguía-Realpozo P., Etchegaray-Morales I., Montiel-Jarquín Á., de Lara L.G.V., Alonso-García N.E., Gándara-Ramírez J.L., López-Colombo A. Associations between resilience and sociodemographic factors and depressive symptoms in women with systemic lupus erythematosus. J. Psychosom. Res. 2019;122:39–42. doi: 10.1016/j.jpsychores.2019.05.002. [DOI] [PubMed] [Google Scholar]
- González-Pinto A., de Azúa S.R., Ibáñez B., Otero-Cuesta S., Castro-Fornieles J., Graell-Berna M., Ugarte A., Parellada M., Moreno D., Soutullo C., Baeza I., Arango C. Can positive family factors be protective against the development of psychosis? Psychiatry Res. 2011;186:28–33. doi: 10.1016/j.psychres.2010.05.015. [DOI] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M.Á., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain. Behav. Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedges L. Distribution Theory for Glass's Estimator of Effect Size and Related Estimators. J. Educ. Stat. 1981;6:107–128. [Google Scholar]
- Hedges L.V., Olkin I. San Diego, CA; 1985. Statistical methods for meta-analysis., Academic P. [Google Scholar]
- Henley, J., 2020. More than 250 million in lockdown in EU as Belgium and Germany adopt measures [WWW Document]. Guard. URL https://www.msn.com/en-ca/news/world/more-than-250m-in-lockdown-in-eu-as-belgium-and-germany-adopt-measures/ar-BB11mIJF.
- Jeste D.V., Palmer B.W., Rettew D.C., Boardman S. Positive psychiatry: Its time has come. J. Clin. Psychiatry. 2015 doi: 10.4088/JCP.14nr09599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesebir S., Gündoǧar D., Küçüksubaşi Y., Tatlidil Yaylaci E. The relation between affective temperament and resilience in depression: A controlled study. J. Affect. Disord. 2013;148:352–356. doi: 10.1016/j.jad.2012.12.023. [DOI] [PubMed] [Google Scholar]
- Killgore W.D.S., Taylor E.C., Cloonan S.A., Dailey N.S. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J. Resilience and Developmental Psychopathology. Child Adolesc. Psychiatr. Clin. N. Am. 2007 doi: 10.1016/j.chc.2006.11.003. [DOI] [PubMed] [Google Scholar]
- Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – A systematic review and meta-analysis. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marazziti D., Stahl S.M. The relevance of COVID -19 pandemic to psychiatry. World Psychiatry. 2020;19 doi: 10.1002/wps.20764. 261–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers E., Lin A., Lester E., Shaffer K., Rosand J., Vranceanu A.M. Baseline resilience and depression symptoms predict trajectory of depression in dyads of patients and their informal caregivers following discharge from the Neuro-ICU. Gen. Hosp. Psychiatry. 2020;62:87–92. doi: 10.1016/j.genhosppsych.2019.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizuno Y., Hofer A., Suzuki T., Frajo-Apor B., Wartelsteiner F., Kemmler G., Saruta J., Tsukinoki K., Mimura M., Fleischhacker W.W., Uchida H. Clinical and biological correlates of resilience in patients with schizophrenia and bipolar disorder: A cross-sectional study. Schizophr. Res. 2016;175:148–153. doi: 10.1016/j.schres.2016.04.047. [DOI] [PubMed] [Google Scholar]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V., Chieffo D., Janiri L., Fiorillo A., Sani G., Di Nicola M. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain. Behav. Immun. 2020;87:75–79. doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno C., Wykes T., Galderisi S., Nordentoft M., Crossley N., Jones N., Cannon M., Correll C.U., Byrne L., Carr S., Chen E.Y.H., Gorwood P., Johnson S., Kärkkäinen H., Krystal J.H., Lee J., Lieberman J., López-Jaramillo C., Männikkö M., Phillips M.R., Uchida H., Vieta E., Vita A., Arango C. How mental health care should change as a consequence of the COVID-19 pandemic. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osofsky H.J., Osofsky J.D. Hurricane katrina and the gulf oil spill: Lessons learned. Psychiatr. Clin. North Am. 2013 doi: 10.1016/j.psc.2013.05.009. [DOI] [PubMed] [Google Scholar]
- Pacchiarotti I., Anmella G., Fico G., Verdolini N., Vieta E. A psychiatrist's perspective from a COVID-19 epicentre: a personal account. BJPsych open. 2020;6:e108. doi: 10.1192/bjo.2020.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardeller S., Kemmler G., Hoertnagl C.M., Hofer A. Associations between resilience and quality of life in patients experiencing a depressive episode. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113353. [DOI] [PubMed] [Google Scholar]
- Poloni N., Zizolfi D., Ielmini M., Pagani R., Caselli I., Diurni M., Milano A., Callegari C. A naturalistic study on the relationship among resilient factors, psychiatric symptoms, and psychosocial functioning in a sample of residential patients with psychosis. Psychol. Res. Behav. Manag. 2018;11:123–131. doi: 10.2147/PRBM.S159571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020;75:631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Reinares M., Bonnín C.M., Hidalgo-Mazzei D., Colom F., Solé B., Jiménez E., Torrent C., Comes M., Martínez-Arán A., Sánchez-Moreno J., Vieta E. Family functioning in bipolar disorder: Characteristics, congruity between patients and relatives, and clinical correlates. Psychiatry Res. 2016;245:66–73. doi: 10.1016/j.psychres.2016.08.010. [DOI] [PubMed] [Google Scholar]
- Rossi A., Galderisi S., Rocca P., Bertolino A., Rucci P., Gibertoni D., Stratta P., Bucci P., Mucci A., Aguglia E., Amodeo G., Amore M., Bellomo A., Brugnoli R., Caforio G., Carpiniello B., Dell'Osso L., di Fabio F., di Giannantonio M., Marchesi C., Monteleone P., Montemagni C., Oldani L., Roncone R., Sacchetti E., Santonastaso P., Siracusano A., Zeppegno P., Maj M., Andriola I., Paladini V., Mancini M., Ferrari B., Vita A., Barlati S., Galluzzo A., Pinna F., Primavera D., Sanna L., Signorelli M.S., Cannavò D., Minutolo G., Martinotti G., Lupi M., Corbo M., Ricca V., Burchi E., Altamura M., Carnevale R., Petito A., Murri M.B., Calcagno P., Corso A., Rossetti M.C., Rossi R., Santarelli V., Giusti L., Malavolta M., Ussorio D., Serati M., De Simone S., Vignapiano A., Montefusco V., Plescia G.M., Palumbo D., Iasevoli F., Gramaglia C., Feggi A., Gattoni E., Campagnola N., Collantoni E., Tenconi E., De Panfilis C., Tonna M., Ossola P., Gesi C., Rutigliano G., Landi P., Biondi M., Girardi P., Buzzanca A., Girardi N., De Carolis A., Di Lorenzo G., Niolu C., Ribolsi M., Corrivetti G., Bartoli L., Diasco F., Fagiolini A., Goracci A., Bolognesi S., Bava I., Mancini I., Cardillo S. Personal resources and depression in schizophrenia: The role of self-esteem, resilience and internalized stigma. Psychiatry Res. 2017;256:359–364. doi: 10.1016/j.psychres.2017.06.079. [DOI] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor Shna, Mohammadi M., Rasoulpoor Shabnam, Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Global. Health. 2020 doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solé B., Verdolini N., Amoretti S., Montejo L., Rosa A., Hogg B., Garcia-Rizo C., Mezquida G., Bernardo M., Martinez-Aran A., Vieta E., Torrent C. Vol. 281. Journal of Affective Disorders; 2021. Effects of the COVID-19 pandemic and lockdown in Spain: comparison between community controls and patients with a psychiatric disorder. Preliminary results from the BRIS-MHC STUDY; pp. 13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sominsky L., Walker D.W., Spencer S.J. One size does not fit all – Patterns of vulnerability and resilience in the COVID-19 pandemic and why heterogeneity of disease matters. Brain. Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torgalsbøen A.K., Fu S., Czajkowski N. Resilience trajectories to full recovery in first-episode schizophrenia. Eur. Psychiatry. 2018;52:54–60. doi: 10.1016/j.eurpsy.2018.04.007. [DOI] [PubMed] [Google Scholar]
- Verdolini N., Amoretti S., Mezquida G., Cuesta6 M., Pina-Camacho L., García-Rizo G., Lobo A., González-Pinto A., Merchán-Naranjo J., Corripio I., Salagre E., Baeza I., Bergé D., Garriga M., Bioque M., Vieta E., Bernardo M., Group. Pep. European Neuropsychopharmacology; 2021. The effect of family environment and psychiatric family history on psychosocial functioning in first-episode psychosis at baseline and after 2 years. In press. [DOI] [PubMed] [Google Scholar]
- Vieta E., Pérez V., Arango C. Psychiatry in the aftermath of COVID-19. Rev. Psiquiatr. Salud Ment. 2020;13:105–110. doi: 10.1016/j.rpsm.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh M.A., Brown L.H., Barrantes-Vidal N., Kwapil T.R. The expression of affective temperaments in daily life. J. Affect. Disord. 2013;145:179–186. doi: 10.1016/j.jad.2012.07.026. [DOI] [PubMed] [Google Scholar]
- Wambua G.N., Kilian S., Ntlantsana V., Chiliza B. The association between resilience and psychosocial functioning in schizophrenia: A systematic review and meta-analysis. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113374. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo W., Mayberry R., Bae S., Singh K., Peter He Q., Lillard J.W. A Study of Effects of MultiCollinearity in the Multivariable Analysis. Int. J. Appl. Sci. Technol. 2014;4:9–19. [PMC free article] [PubMed] [Google Scholar]
- Young R., Lennie S., Minnis H. Children's perceptions of parental emotional neglect and control and psychopathology. J. Child Psychol. Psychiatry. 2011;52:889–897. doi: 10.1111/j.1469-7610.2011.02390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y., Yang X., Yang Y., Chen L., Qiu X., Qiao Z., Zhou J., Pan H., Ban B., Zhu X., He J., Ding Y., Bai B. The Role of Family Environment in Depressive Symptoms among University Students: A Large Sample Survey in China. PLoS One. 2015;10 doi: 10.1371/journal.pone.0143612. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.