Abstract
Background
Accurate acute care medical utilization history is an important outcome for clinicians and investigators concerned with improving trauma center care. The objective of this study was to examine the accuracy of self-report emergency department (ED) utilization compared with utilization obtained from the Emergency Department Information Exchange (EDIE) in admitted trauma surgery patients with comorbid mental health and substance use problems.
Methods
This is a retrospective cohort study of 169 injured patients admitted to the University of Washington’s Harborview Level I Trauma Center. Patients had high levels of post-traumatic stress disorder and depressive symptoms, suicidal ideation and alcohol comorbidity. The investigation used EDIE, a novel health technology tool that collects information at the time a patient checks into any ED in Washington and other US states. Patterns of EDIE-documented visits were described, and the accuracy of injured patients’ self-report visits was compared with EDIE-recorded visits during the course of the 12 months prior to the index trauma center admission.
Results
Overall, 45% of the sample (n=76) inaccurately recalled their ED visits during the past year, with 36 participants (21%) reporting less ED visits than EDIE indicated and 40 (24%) reporting more ED visits than EDIE indicated. Patients with histories of alcohol use problems and major psychiatric illness were more likely to either under-report or over-report ED health service use.
Discussion
Nearly half of all patients were unable to accurately recall ED visits in the previous 12 months compared with EDIE, with almost one-quarter of patients demonstrating high levels of disagreement. The improved accuracy and ease of use when compared with self-report make EDIE an important tool for both clinical and pragmatic trial longitudinal outcome assessments. Orchestrated investigative and policy efforts could further examine the benefits of introducing EDIE and other information exchanges into routine acute care clinical workflows.
Level of evidence
II/III.
Trial registration number
ClinicalTrials.gov NCT02274688.
Keywords: patient reported outcome measures, stress disorders, post-traumatic, substance-related disorders, wounds and injuries
Introduction
Increasingly, trauma centers are being encouraged to collect self-report outcome data from patients to capture key longitudinal injury outcomes.1–3 The American College of Surgeons Committee on Trauma may recommend the routine collection of outcomes, including physical and mental health symptoms, functional outcomes, and patterns of health service utilization, during the course of the weeks and months after injury. A series of large-scale trauma center prospective cohort and clinical trial investigations have relied exclusively on patient self-report to ascertain rates of physical and mental health symptoms, functional outcomes, and patterns of health service utilization.4–6 Increasingly, large-scale pragmatic clinical trials are being implemented in acute care medical settings and with injury survivors.7–9 Pragmatic clinical trials are designed to harness data collected in clinical settings under conditions of routine practice and encourage the use of real-time, workflow-integrated outcome data collection in the conduct of comparative effectiveness research.10 11
Leveraging large-scale electronic medical data collection is therefore an increasingly essential element of both acute care clinical and pragmatic trial longitudinal outcome data assessments.1 10–12 Health information exchanges represent one potential and currently underused source of large-scale electronic medical record (EMR) data in acute care medical settings.1 12–16 A key initial step in integrating health information exchanges into routine trauma center clinical and research longitudinal outcome assessments is understanding the accuracy of self-report health service utilization in comparison to real-time, workflow-integrated administrative data sources.
However, literature review revealed few studies that have compared self-report outcomes versus administrative data from a health information exchange. Specifically, one study examined acute care utilization in hospitalized patients with substance use disorders and documented consistent under-reporting of visits when comparing patient self-reports to objective emergency department (ED) exchange data sources.17 Similarly, in other areas of health services research, self-report utilization measures have been associated with recall biases,18 and it appears that error in recall increases as utilization increases.19 20 Additionally, previous studies have investigated acute care patterns of service utilization with administrative data in cohorts of patients at risk for high utilization.21 22 However, none of these studies are of trauma patients and many of these studies are limited to single health systems,23 whereas other studies include only a small geography that may cross health systems22 24 or are limited to one specific condition.17 25 To date, no studies substantiate the utility of administrative data from health information exchanges in documenting ED utilization patterns across broad patient populations and state-wide geographic regions, despite reliance on this measure to determine effective clinical outcomes for trauma surgery patients.
The Emergency Department Information Exchange (EDIE) is a type of health information exchange or care coordination platform that collects EMR information14 26 at the time a patient checks into any ED. Patients do not need to opt in or request their information be shared; rather, hospitals decide to participate for their entire population. For any patient, a hospital follows a standard registration process, and an admission, discharge and/or transfer message containing patient demographics is delivered to Collective Medical, which then packages health information on the patient and sends a notification to treating providers in the ED.27 The information package, or EDIE ‘alert’, generated at each ED visit includes counts of prior ED visits during the past 12 months and specific EDs visited, which is obtained through EMR data from each participating hospital. EDIE is unique for an intraoperability platform given its reach and spread across the country; as of June 2020, EDIE has participation in 99% of EDs in Washington and Oregon, as well as many sites in California and over 20 other states across the country.28
The objective of this article was to first assess the patterns of past 12-month state-wide ED utilization among a cohort of injured patients admitted to a level I trauma center with comorbid medical, psychiatric and substance use conditions using EDIE. Next, the investigation compared self-report ED utilization with EDIE-documented ED visits to assess patterns of patient over-reporting and under-reporting. Finally, the investigation aimed to determine if there were patient demographics or clinical characteristics associated with the over-reporting or under-reporting of ED utilization.
Methods
Study design
This is a secondary data analysis from the screening and baseline assessment phase of a comparative effectiveness trial of patient-centered care transitions for patients with injuries and elevated risk for post-traumatic stress disorder (PTSD).29
Study setting and population
Participants were recruited from Harborview Medical Center (HMC), a large urban level I trauma center located in Seattle, Washington; HMC is the only level I trauma center for the five-state (Washington, Wyoming, Alaska, Montana and Idaho) region. Participants were recruited by trained research assistants (RAs) Monday through Friday from 07:00 to 18:00, including a sampling of evenings and weekends from March 2014 through September 2015. RAs reviewed the EMR of patients aged 14 years or older presenting to the ED and admitted for injury care for at least 24 hours to find those at elevated risk for PTSD based on a validated 10-item population-based EMR prescreen.30 Those with elevated risk for PTSD based on the EMR prescreen were approached to participate. Participants were excluded if they required immediate psychiatric care (eg, suicide attempt survivors), did not live in Washington state, were incarcerated, did not speak English, did not have a Glasgow Coma Scale score of 15 and a score of at least 7/10 on the Mini-Mental Status Exam. Adult participants provided written informed consent, and parental consent was obtained for adolescent participants with subsequent adolescent assent. Differences in demographic and injury characteristics among patients enrolled in the trial compared with all other patients admitted to HMC during the time period of the study have previously been described.29 On average, patients in the trial were approached to participate at 6.2 days after admission (SD 4.9 days).
Measurements
Mental health and substance use screening
The RAs asked participants about their postinjury concerns with the open-ended question, ‘Of everything that has happened to you since you were injured, what concerns you the most?’, allowing for an unlimited amount of concerns. Enrolled participants were required to have at least three post-traumatic concerns at the time of recruitment.31 All participants were screened for mental health comorbidity. Specifically, an RA-assisted interview was performed including the PTSD CheckList-Civilian Version,32 which is a validated 17-item screen for PTSD since the injury for which they were being treated in the hospital. A score of 35 or greater on the PTSD Checklist represents an elevated risk for PTSD,30 and the measure has been used previously in the acute postinjury phase to determine patients at risk for PTSD.6 33 Depression in the previous 2 weeks was assessed with the validated Patient Health Questionnaire 9 (PHQ-9).34 A score of 10 or higher on the PHQ-9 is sensitive for moderate depression, and the PHQ-9 has previously been used in ED and acute care settings.35 Participants with elevated risk for PTSD based on a score of ≥35 on the PTSD Checklist, or with moderate depression based on a score of ≥10 on the PHQ-9, or with suicidal thoughts based on a score of ≥1 on the suicide assessment item within the PHQ-9 were included and completed the baseline interview. Patients were also screened for alcohol use problems with the three-item Alcohol Use Disorders Identification Test (AUDIT-C)36 to assess problem drinking in the 12 months prior to injury. A score of ≥4 for males and ≥3 for females suggests alcohol misuse in the year prior to injury. The AUDIT-C is a validated instrument and has been previously used in the ED and other medical settings. History of alcohol use and history of major psychiatric illness were abstracted from the 2014–2015 trauma registry. Specifically, ‘previous history of major psychiatric illness’ includes any documented International Classification of Diseases (ICD-9) code within the HMC EMR of preinjury major depressive disorder, bipolar disorder, schizophrenia, anxiety/panic disorder, borderline or antisocial personality disorder and/or adjustment disorder or PTSD. ‘Previous history of alcohol use’ includes evidence of chronic use within the HMC EMR, including documentation of ICD-9 codes pertinent to chronic use such as alcohol withdrawal. This variable did not include toxicology information from the acute visit.
Baseline measures
Demographics
Demographic questions including age, sex and race were asked as part of the baseline interview. A single item was used to assess living situation and answers were dichotomized to ‘homeless’ (eg, homeless, shelter or temporary residence) or ‘not homeless’ (eg, home, apartment, group home or skilled nursing home). Insurance status was abstracted from the trauma registry.
Clinical characteristics
Injury Severity Score (ISS) at baseline was determined from ICD-9 codes and intensive care unit stay was determined from the trauma registry. Patients were asked to report medications taken in the 3 months before their injury hospitalization. All recorded opioid pain medications, which included hydrocodone, tramadol, oxycodone, methadone and fentanyl, were collapsed to form a variable of ‘opioid pain medication at baseline’.
ED utilization
Participants were asked to report their ED utilization in the year prior to their injury. Specifically, participants were asked, ‘During the past year prior to your injury, how many visits did you make to a hospital emergency room?’ to determine their self-report ED utilization during the 12 months prior to their injury. Information from EDIE26 was obtained to determine ED utilization within Washington and Oregon in the same time period. From EDIE, we determined the number of ED visits to any ED in Oregon and Washington for the 12 months prior to injury, as well as the number of different EDs visited by each patient during the same period.
Analysis
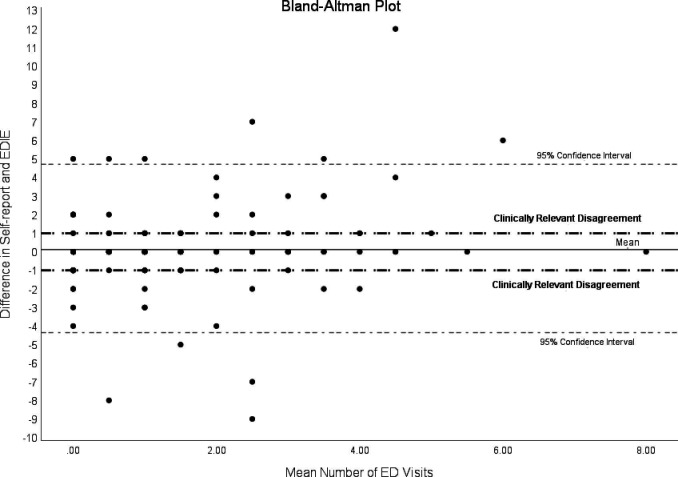
Descriptive statistics for demographic, clinical and ED utilization variables were calculated for all patients included in the cohort. Participants with incomplete self-report ED utilization data (n=2) were excluded from the sample. Next, the study documented and compared patterns of EDIE and self-report ED utilization including a quantitative description of amount of discordance. Linear regression was used to assess for a significant association between EDIE-documented ED visits and number of distinct hospitals visited as documented by EDIE. A Bland-Altman analysis37 was performed to assess the degree of agreement between self-report ED visits and ED visits documented by EDIE; for the Bland-Altman analysis, an absolute cut-off of >1 visit was used to define clinically relevant disagreement when comparing self-report to EDIE-documented utilization.37 38
To assess the hypothesis that patients who misreport ED visits would be more likely to have psychiatric and substance use problems, we evaluated participant ability to accurately self-report ED visits. For this analysis, self-report visits were compared with the visit history obtained from the health information exchange, or the EDIE-documented ED visits. These analyses demonstrated three categories of visit comparisons: participants were identified as ‘matching’ if their self-report value matched the EDIE value, ‘under-reporting’ if their self-report value was lower than the EDIE value and ‘over-reporting’ if their self-report value was greater than the EDIE value. First, we compared those with matching self-report and EDIE values for ‘0’ visit in the past year to those with any other value of matching self-report and EDIE visits. Baseline group differences were examined using independent group t-tests for continuous variables and χ2 tests for categorical variables. No differences were found between these groups on any variables, and therefore these groups were combined to form the ‘matching’ group. Next, we used one-way analysis of variance for continuous variables and χ2 tests for categorical variables to identify differences across the three groups in demographics, mental health comorbidity, clinical characteristics and ED visit utilization among the matching, under-reporting and over-reporting groups. Planned post hoc differences were examined using Bonferroni comparisons. Analyses were performed using SPSS V.24.
Results
A total of 169 patients with trauma and elevated risk for mental health and substance use problems were included in the cohort (table 1). The average age was 42.1 years (SD 15.9 years), 56.8% (n=96) were female and approximately half identified as white (55.6%). The majority had public insurance (n=163, 96.4%) and 8.3% (n=14) were homeless. Most of the sample endorsed moderate depression in the past 2 weeks (n=155, 91.7%) or risk for PTSD (n=127, 75.1%) whereas a quarter had some degree of suicidal thoughts (n=41, 24.3%) which is consistent with the recruitment effort of the trial.29 Additionally, half (n=83, 49.1%) had past year alcohol misuse and 13.6% (n=23) had a record of chronic alcohol use documented in the EMR.
Table 1.
Demographics, mental health and substance use, clinical characteristics and emergency department (ED) visit utilization among trauma patients with elevated risk for mental health and substance use comorbidity (n=169)
| Characteristic | n (%)/m (SD) |
| Demographics | |
| Age | 42.1 (15.9) |
| Female | 96 (56.8) |
| Race | |
| White | 94 (55.6) |
| African-American | 27 (16.0) |
| Native American | 22 (13.0) |
| Asian/Pacific Islander | 14 (8.3) |
| Hispanic | 12 (7.1) |
| Homeless at baseline | 14 (8.3) |
| Public insurance | 163 (96.4) |
| Mental health and substance use | |
| PCL-C score ≥35 (risk for PTSD) | 127 (75.1) |
| PHQ-9 ≥10 (current moderate depression) | 155 (91.7) |
| PHQ-9 item 9 score ≥1 (current suicidality) | 41 (24.3) |
| AUDIT-C score positive (current alcohol use disorder) | 83 (49.1) |
| History of alcohol use | 23 (13.6) |
| History of major psychiatric illness | 54 (32.0) |
| Clinical characteristics | |
| Injury Severity Score | 15.1 (11.3) |
| ICU admit | 96 (56.8) |
| Emergency department utilization | |
| Self-report ED visits in past year | 1.3 (2.4) |
| EDIE ED visits in past year | 1.5 (2.5) |
| EDIE distinct hospitals visited in past year | 0.69 (0.97) |
| Self-report ED visits match EDIE | 93 (55.0) |
| Self-report is less than EDIE (under-reporting) | 36 (21.3) |
| Self-report is more than EDIE (over-reporting) | 40 (23.6) |
AUDIT-C, Alcohol Use Disorders Identification Test Consumption; ED, emergency department; EDIE, Emergency Department Information Exchange; ICU, intensive care unit; PCL-C, PTSD CheckList-Civilian version; PHQ-9, Patient Health Questionnaire 9; PTSD, post-traumatic stress disorder.
During the year prior to the index admission, the average number of self-report ED visits was 1.3 (SD 2.4) with EDIE showing an average of 1.5 (SD 2.5) ED visits in the past 12 months (table 1). By the self-report measure, 51.5% (n=88) of participants reported no past year ED visits, 18.9% (n=32) reported one ED visit, 22.5% (n=38) reported two to four ED visits and 6.5% (n=11) reported five or more ED visits in the past year. Evaluation of EDIE data for past year visits revealed 56.0% (n=96) of participants had no ED visits, 12.9% (n=22) had one ED visit, 19.3% had two to four ED visits and 11.7% (n=20) had five or more ED visits.
Comparing these reporting methods, 55% (n=93) matched with self-report and EDIE methods providing the same value, 9.9% (n=17) under-reported with EDIE having a value of exactly 1 more than self-report and 13.5% (n=23) under-reported with EDIE having a value of 2 or more higher than self-report. A total of 11.7% (n=20) reported more visits than EDIE by exactly 1 and 9.5% (n=16) had a self-report value of 2 or more higher than EDIE. Overall, the self-reports of 23% (n=39) of participants differed by the clinically relevant absolute cut-off of >1 visit when compared with EDIE-documented utilization (figure 1).
Figure 1.
Bland-Altman plot of differences between participants’ self-report and EDIE-documented number of emergency department (ED) visits versus the mean number of ED visits. EDIE, Emergency Department Information Exchange.
By tracking both the number of EDs visited and the number of distinct hospital EDs visited, EDIE facilitated an assessment of the association between these two indices of acute care health service utilization. Linear regression was used to predict the total number of ED visits in the year prior by EDIE from the number of distinct EDs visited in the same time period, and as the number of different EDs visited increased, the number of total ED visits increased linearly (R2=0.671).
Next, the ‘matching’ group was further examined. While half (n=93, 55%) of the total sample had matching self-report ED visits and EDIE-documented ED visits during the past year (ie, matching), the majority (n=75, 80.1%) of those had zero ED visit. Within this matching group, those with matching self-report and EDIE for one or more ED visits in the past 12 months (n=18) were compared with those with zero visit (n=75) to determine if any significant differences existed between these groups. There were no statistically significant differences among demographics, current mental health characteristics, or clinical characteristics. Therefore, these two subgroups were combined (n=93) to form the ‘All Matching’ group for further analysis (table 2). In the ‘Under-reporting’ group, the mean number of self-report visits was 1.6 (SD 1.7) compared with the EDIE-documented ED visits of 4.4 (SD 3.0), and these EDIE-documented visits occurred at 1.9 different hospitals (SD 1.0). In the ‘Over-reporting’ group, the mean number of self-report visits was 3.5 (SD 3.8) compared with the EDIE-documented ED visits of 1.2 (2.4), and these visits occurred at 0.6 different hospitals (SD 0.65). Among those in the ‘Matching emergency department visits’ group with at least one ED visit in the past 12 months (n=18), the mean number of ED visits was 1.6 (SD 0.7), with these visits occurring at 1.1 different hospitals (SD 0.32).
Table 2.
Demographics, clinical characteristics and emergency department (ED) visit utilization reporting patterns (n=169)
| Characteristic | No ED visits n=75 |
Matching ED visits n=18 |
P value | All matching n=93 |
Over- reporting n=36 |
Under- reporting n=40 |
P value | Post hoc differences |
| Demographics | ||||||||
| Age, mean (SD) | 41.2 (18.0) | 37.9 (11.3) | 0.46 | 40.6 (16.9) | 44.3 (14.9) | 43.5 (14.2) | 0.4 | |
| Female, n (%) | 38 (50.7) | 14 (77.8) | 0.06 | 52 (55.9) | 20 (55.6) | 24 (60.0) | 0.98 | |
| Race, n (%) | ||||||||
| White | 45 (60.0) | 10 (55.6) | 55 (59.1) | 21 (58.3) | 18 (45.0) | |||
| African-American | 11 (14.7) | 3 (16.7) | 14 (15.1) | 6 (16.7) | 7 (17.5) | |||
| Native American | 5 (6.7) | 1 (5.6) | 0.9 | 6 (6.5) | 5 (13.9) | 11 (27.5) | 0.08 | |
| Asian/Pacific Islander | 7 (9.3) | 3 (16.7) | 10 (10.8) | 3 (8.3) | 1 (2.5) | |||
| Hispanic | 7 (9.3) | 1 (5.6) | 8 (8.6) | 1 (2.8) | 3 (7.5) | |||
| Homeless at baseline | 4 (5.3) | 0 (0) | 1 | 4 (4.3) | 1 (2.8) | 9 (22.5) | 0.001 | UR>others |
| Public insurance | 73 (97.3) | 18 (100) | 1 | 91 (97.8) | 34 (94.4) | 38 (95.0) | 0.36 | |
| Mental health and substance use | ||||||||
| Risk for PTSD, n (%) | 52 (69.3) | 14 (77.8) | 0.57 | 66 (71.0) | 27 (75.0) | 34 (85.0) | 0.23 | |
| Current moderate depression, n (%) | 67 (89.3) | 17 (94.4) | 1 | 84 (90.3) | 35 (97.2) | 36 (90.0) | 0.4 | |
| Current suicidality | 23 (30.7) | 3 (16.7) | 0.38 | 26 (28.0) | 6 (16.7) | 9 (22.5) | 0.39 | |
| Current alcohol use disorder | 34 (45.3) | 10 (55.6) | 0.6 | 44 (47.3) | 18 (50.0) | 21 (52.5) | 0.85 | |
| History of alcohol use | 6 (8.0) | 2 (11.1) | 0.65 | 8 (8.6) | 5 (13.9) | 10 (25.0) | 0.04 | Match<UR |
| History of major psychiatric illness | 20 (26.7) | 5 (27.8) | 1 | 25 (26.9) | 10 (27.8) | 19 (47.5) | 0.05 | Match<UR |
| Clinical characteristics | ||||||||
| Injury Severity Score | 11.1 (17.2) | 11.4 (12.0) | 0.08 | 11.2 (16.2) | 13.0 (15.3) | 9.6 (12.5) | 0.23 | |
| ICU admit, n (%) | 51 (68.0) | 8 (44.4) | 0.1 | 59 (63.4) | 20 (55.6) | 17 (42.5) | 0.08 | |
ICU, intensive care unit; PTSD, post-traumatic stress disorder; UR, under reporting.
Baseline variables were compared among the ‘All Matching’, ‘Over-reporting’ and ‘Under-reporting’ groups (table 2). Among demographic characteristics, there were no statistically significant differences with the exception of homelessness. While the frequency of homelessness was low among the whole cohort (n=14), there were differences across the three groups, with the ‘Under-reporting’ group having more homelessness than the ‘All Matching’ or ‘Over-reporting’ groups. Participants in all groups had high rates of current mental health characteristics, and no differences existed across groups for current risk for PTSD, current major depression or suicidality. However, significant differences existed between the groups for history of alcohol use problems and history of major psychiatric illness as determined by the EMR. Post hoc comparisons revealed the ‘All Matching’ group to have less alcohol use than the ‘Under-reporting’ group and less psychiatric disease than the ‘Under-reporting’ group.
Discussion
Using data derived from EDIE for a cohort of 169 injured trauma survivors to describe patterns of health service utilization is feasible, and highlights the difficulty in accuracy of self-report in patients with complex medical, psychiatric and substance-related comorbidity admitted to a single level I trauma center in the Pacific Northwest Region of the USA. Approximately half (45%) of the injured patients with injury, mental illness and substance use comorbidity were unable to accurately report their ED utilization within the past year when compared with EDIE, a health information exchange or intraoperability platform gold standard. Additionally, just under one-quarter of patients had self-report ED use that was more than one visit over or under the EDIE gold standard. Among those that could not accurately recall or report their ED visits, approximately half under-reported their visits and half over-reported their visits. Those that under-reported ED visits were more likely to have a history of alcohol use, a history of major psychiatric illness or report homelessness compared with those that correctly recalled their ED visits. Prior investigations in hospitalized patients with substance use disorders also document inaccuracies in self-report acute care utilization.17 However, unlike the current study, substance users’ self-report errors were unidirectional, with only significant under-reporting of ED utilization.
Prospective cohort and population-based epidemiologic studies suggest that a subgroup of injured trauma survivors will develop a chronic condition characterized by multiple comorbid diagnoses including mental health, substance use and medical disorders, as well as suicide attempts and violence-related life events such as firearm injuries.4 39–41 Trauma centers are developing longitudinal outcome assessment procedures, as well as pragmatic screening and intervention procedures and policy to address the complex needs of injured patients with substance use and mental health comorbidity.1 9 42 Essential to these efforts are assessments of acute care health service utilization patterns that realistically account for potential data inaccuracies.16 43 This current investigation demonstrates the value of EDIE, one particular health information exchange, for providing a more accurate ED utilization history than can be obtained by self-report in a patient population with multiple comorbidities. This study demonstrates the ability for more accurate assessment of care through the frequently used metric of recidivistic visits in a population at risk for ED/trauma center recidivism.44 As ED visits increase, the risk for inaccurate self-report increases as well. Patients at risk for repeat ED visits, such as those with substance use and mental health comorbidity, often require trauma center care coordination.29 Likewise, developing interventions for this population requires an accurate understanding of healthcare utilization.42
Additionally, when considering recommendations for routine longitudinal outcome research from trauma centers,1 4 real-time, workflow-integrated administrative data such as EDIE provide the unique advantage of ≥90% follow-up without relying on patient-reported outcomes and interviews. Also, utilization outcome data obtained through EMRs are often limited to one health system, and many patients will visit at least two different EDs in the course of a year,22 45 46 making health information exchange systems such as EDIE an important source of these data. EDIE is unique for an intraoperability platform given its density and implementation around the country.
Health information exchanges have potential to affect trauma center clinical practice and outcomes assessment above and beyond accurate visit reporting. In addition to accurate utilization data for clinicians and outcomes researchers, health information exchanges have the potential to assess clinical quality measures,13 47 48 although this potential has yet to be used. Further, this information has potential to serve as an invaluable repository of data for health services researchers aiming to trauma center health services utilization. Important challenges to implementation of health information exchange platforms in clinical care and research include adoption and functionality. Information that is difficult to access and requires separate login and interruption of clinical workflow can lead to low usability.49 Clinical investigators working in acute care settings can help evaluate health information exchanges or intraoperability platforms such as EDIE, but need to design studies and consider issues such as patient privacy and data sharing to collect this type of information.
Limitations
Despite these novel observations, there are some important limitations to note. First, all participants included in this study were recruited from a single site, and results may not generalize to other types of hospitals. Additionally, the sample size was fixed, as this was a secondary analysis of a randomized clinical trial and certain groups were small, limiting the power to detect significant differences. Though participants had to report residency in Washington to be included, it is possible they could have recently moved into the region, limiting data availability from EDIE for the 12 months prior. This would inflate the number of participants we found to be over-reporting in our sample. The self-report recall period was 1 year in duration, and it is known that shorter recall times result in improved accuracy of self-report.18 All health information exchanges, including EDIE, are imperfect systems with internal limitations, specifically related to matching and data accuracy, although previous research demonstrated current matching algorithms using minimal identifying data such as first name, last name and date of birth are extremely accurate.50 Patients unable to provide this information at the time of check-in would be missed in any health information exchange.
Conclusion
Emergency Department Health Information Exchange administrative data can provide more accurate information regarding patterns of ED utilization in patients with high levels of medical, mental health and substance-related comorbidity than self-report. As a prospective outcome assessment tool, ED health information exchanges such as EDIE have the advantages of enhanced accuracy and ease of longitudinal follow-up when compared with self-report. Orchestrated investigative and policy efforts could further examine the benefits of introducing EDIE and other information exchanges into routine trauma center and emergency care workflows.
Acknowledgments
The authors wish to thank Karl Jablonowski, clinical data analyst in the Department of Emergency Medicine, for his contribution to the study, and special thanks is owed to the patients and staff at Harborview Medical Center.
Footnotes
Contributors: LKW and DFZ conceived and designed the study and the analysis plan. LKW, MCV, DN, EMB, KM, and DFZ conducted a review of the relevant literature. LKW, JR, and KM designed the tables and figures for the article. LKW and DFZ conducted the primary data collection for the study. LKW, JR, and DFZ coordinated the collection and management of study data. LKW, JR, and DFZ conducted data analysis and interpretation. All authors contributed intellectual content during the drafting and revision of the article and have reviewed and approved the final version.
Funding: This project was supported by the Patient Centered Outcomes Research Institute (PCORI) (IH-1304-6319) and the National Institutes of Health (NIH) (K23DA039974). Preparation of this article was supported in part by the Implementation Research Institute (IRI) through an award through the NIH (R25MH08091607). This research was also supported within the National Institutes of Health (NIH) Health Care Systems Research Collaboratory by cooperative agreement 1UH2MH106338-01/4UH3MH106338-02 from the NIH Common Fund and by UH3 MH 106338-05S1 from NIMH. The content is solely the responsibility of the authors and does not necessarily represent the official views of PCORI or the NIH.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of PCORI, its Board of Governors or Methodology Committee, or the NIH.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This project was approved by the University of Washington Institutional Review Board (46085) prior to beginning data collection. All participants provided informed consent before participating.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. Data used in this study are available from the corresponding author upon reasonable request. All personal identifiers found in the data will be removed prior to sharing.
References
- 1.Sakran JV, Ezzeddine H, Schwab CW, Bonne S, Brasel KJ, Burd RS, Cuschieri J, Ficke J, Gaines BA, Giacino JT, et al. . Proceedings from the consensus conference on trauma patient-reported outcome measures. J Am Coll Surg 2020;230:819–35. 10.1016/j.jamcollsurg.2020.01.032 [DOI] [PubMed] [Google Scholar]
- 2.Godat LN, Jensen AR, Stein DM, Coalition for National Trauma Research Scientific Advisory Council . Patient-centered outcomes research and the injured patient: a summary of application. Trauma Surg Acute Care Open 2020;5:e000422. 10.1136/tsaco-2019-000422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenberg GM, Stave C, Spain DA, Weiser TG. Patient-reported outcomes in trauma: a scoping study of published research. Trauma Surg Acute Care Open 2018;3:e000202. 10.1136/tsaco-2018-000202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haider AH, Herrera-Escobar JP, Al Rafai SS, Harlow AF, Apoj M, Nehra D, Kasotakis G, Brasel K, Kaafarani HMA, Velmahos G, et al. . Factors associated with long-term outcomes after injury: results of the functional outcomes and recovery after trauma emergencies (FORTE) multicenter cohort study. Ann Surg 2020;271:1165–73. 10.1097/SLA.0000000000003101 [DOI] [PubMed] [Google Scholar]
- 5.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med 2006;354:366–78. 10.1056/NEJMsa052049 [DOI] [PubMed] [Google Scholar]
- 6.Zatzick D, Jurkovich G, Rivara FP, Russo J, Wagner A, Wang J, Dunn C, Lord SP, Petrie M, Oʼconnor SS, et al. . A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Ann Surg 2013;257:390–9. 10.1097/SLA.0b013e31826bc313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melnick ER, Jeffery MM, Dziura JD, Mao JA, Hess EP, Platts-Mills TF, Solad Y, Paek H, Martel S, Patel MD, et al. . User-centred clinical decision support to implement emergency department-initiated buprenorphine for opioid use disorder: protocol for the pragmatic group randomised embed trial. BMJ Open 2019;9:e028488. 10.1136/bmjopen-2018-028488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grudzen CR, Brody AA, Chung FR, Cuthel AM, Mann D, McQuilkin JA, Rubin AL, Swartz J, Tan A, Goldfeld KS, et al. . Primary palliative care for emergency medicine (PRIM-ER): protocol for a pragmatic, cluster-randomised, stepped wedge design to test the effectiveness of primary palliative care education, training and technical support for emergency medicine. BMJ Open 2019;9:e030099. 10.1136/bmjopen-2019-030099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zatzick DF, Russo J, Darnell D, Chambers DA, Palinkas L, Van Eaton E, Wang J, Ingraham LM, Guiney R, Heagerty P, et al. . An effectiveness-implementation hybrid trial study protocol targeting posttraumatic stress disorder and comorbidity. Implement Sci 2016;11:58. 10.1186/s13012-016-0424-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loudon K, Treweek S, Sullivan F, Donnan P, Thorpe KE, Zwarenstein M. The PRECIS-2 tool: designing trials that are fit for purpose. BMJ 2015;350:h2147. 10.1136/bmj.h2147 [DOI] [PubMed] [Google Scholar]
- 11.Califf RM, Sugarman J. Exploring the ethical and regulatory issues in pragmatic clinical trials. Clin Trials 2015;12:436–41. 10.1177/1740774515598334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Eaton EG, Zatzick DF, Gallagher TH, Tarczy-Hornoch P, Rivara FP, Flum DR, Peterson R, Maier RV. A nationwide survey of trauma center information technology leverage capacity for mental health comorbidity screening. J Am Coll Surg 2014;219:505–10. 10.1016/j.jamcollsurg.2014.02.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin TJ, Ranney ML, Dorroh J, Asselin N, Sarkar IN. Health information exchange in emergency medical services. Appl Clin Inform 2018;9:884–91. 10.1055/s-0038-1676041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shapiro JS, Crowley D, Hoxhaj S, Langabeer J, Panik B, Taylor TB, Weltge A, Nielson JA. Health information exchange in emergency medicine. Ann Emerg Med 2016;67:216–26. 10.1016/j.annemergmed.2015.06.018 [DOI] [PubMed] [Google Scholar]
- 15.Kimmel HJ, Brice YN, Trikalinos TA, Sarkar IN, Ranney ML. Real-Time emergency department electronic notifications regarding high-risk patients: a systematic review. Telemed J E Health 2019;25:604–18. 10.1089/tmj.2018.0117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khurshid A, Diana ML, Jain R. Health information exchange readiness for demonstrating return on investment and quality of care. Perspect Health Inf Manag 2015;12:1d. [PMC free article] [PubMed] [Google Scholar]
- 17.Gryczynski J, Nordeck CD, Martin RD, Welsh C, Schwartz RP, Mitchell SG, Jaffe JH. Leveraging health information exchange for clinical research: extreme underreporting of hospital service utilization among patients with substance use disorders. Drug Alcohol Depend 2020;212:107992. 10.1016/j.drugalcdep.2020.107992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev 2006;63:217–35. 10.1177/1077558705285298 [DOI] [PubMed] [Google Scholar]
- 19.Cleary PD, Jette AM. The validity of self-reported physician utilization measures. Med Care 1984;22:796–803. 10.1097/00005650-198409000-00003 [DOI] [PubMed] [Google Scholar]
- 20.Glass JE, Bucholz KK. Concordance between self-reports and archival records of physician visits: a case-control study comparing individuals with and without alcohol use disorders in the community. Drug Alcohol Depend 2011;116:57–63. 10.1016/j.drugalcdep.2010.11.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baillargeon J, Thomas CR, Williams B, Begley CE, Sharma S, Pollock BH, Murray OJ, Pulvino JS, Raimer B. Medical emergency department utilization patterns among uninsured patients with psychiatric disorders. Psychiatr Serv 2008;59:808–11. 10.1176/ps.2008.59.7.808 [DOI] [PubMed] [Google Scholar]
- 22.Shapiro JS, Johnson SA, Angiollilo J, Fleischman W, Onyile A, Kuperman G. Health information exchange improves identification of frequent emergency department users. Health Aff 2013;32:2193–8. 10.1377/hlthaff.2013.0167 [DOI] [PubMed] [Google Scholar]
- 23.Selby JV, Fireman BH, Swain BE. Effect of a copayment on use of the emergency department in a health maintenance organization. N Engl J Med Overseas Ed 1996;334:635–42. 10.1056/NEJM199603073341006 [DOI] [PubMed] [Google Scholar]
- 24.Finnell JT, Overhage JM, Dexter PR, Perkins SM, Lane KA, McDonald CJ, 2003. Community clinical data exchange for emergency medicine patients. AMIA Annual Symposium proceedings AMIA Symposium 235–8. [PMC free article] [PubMed] [Google Scholar]
- 25.Grinspan ZM, Abramson EL, Banerjee S, Kern LM, Kaushal R, Shapiro JS, 2013. Potential value of health information exchange for people with epilepsy: crossover patterns and missing clinical data. AMIA Annual Symposium proceedings AMIA Symposium 527–36. [PMC free article] [PubMed] [Google Scholar]
- 26.Collective Medical Technologies The Emergency Department Information Exchange. http://collectivemedicaltech.com/what-we-do-2/edie-option-2/ (11 Apr 2016).
- 27.Collective Medical Hospitals using Collective Medical for notifications will fully meet the requirements of the new conditions for participation. 2020. https://collectivemedical.com/cures-act-compliance/ (20 Aug 2020).
- 28.Collective Network Information: Collective Medical. 2020.
- 29.Zatzick D, Russo J, Thomas P, Darnell D, Teter H, Ingraham L, Whiteside LK, Wang J, Guiney R, Parker L, et al. . Patient-Centered care transitions after injury hospitalization: a comparative effectiveness trial. Psychiatry 2018;81:141–57. 10.1080/00332747.2017.1354621 [DOI] [PubMed] [Google Scholar]
- 30.Russo J, Katon W, Zatzick D. The development of a population-based automated screening procedure for PTSD in acutely injured hospitalized trauma survivors. Gen Hosp Psychiatry 2013;35:485–91. 10.1016/j.genhosppsych.2013.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zatzick DF, Kang SM, Hinton WL, Kelly RH, Hilty DM, Franz CE, Le L, Kravitz RL. Posttraumatic concerns: a patient-centered approach to outcome assessment after traumatic physical injury. Med Care 2001;39:327–39. 10.1097/00005650-200104000-00004 [DOI] [PubMed] [Google Scholar]
- 32.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL). Behav Res Ther 1996;34:669–73. 10.1016/0005-7967(96)00033-2 [DOI] [PubMed] [Google Scholar]
- 33.Zatzick D, Donovan D, Dunn C, Russo J, Wang J, Jurkovich G, Rivara F, Whiteside L, Ries R, Gentilello L. Substance use and posttraumatic stress disorder symptoms in trauma center patients receiving mandated alcohol screening and brief intervention. J Subst Abuse Treat 2012;43:410–7. 10.1016/j.jsat.2012.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–13. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zatzick D, Russo J, Lord SP, Varley C, Wang J, Berliner L, Jurkovich G, Whiteside LK, O'Connor S, Rivara FP. Collaborative care intervention targeting violence risk behaviors, substance use, and posttraumatic stress and depressive symptoms in injured adolescents: a randomized clinical trial. JAMA Pediatr 2014;168:532–9. 10.1001/jamapediatrics.2013.4784 [DOI] [PubMed] [Google Scholar]
- 36.Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res 2007;31:1208–17. 10.1111/j.1530-0277.2007.00403.x [DOI] [PubMed] [Google Scholar]
- 37.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res 1999;8:135–60. 10.1177/096228029900800204 [DOI] [PubMed] [Google Scholar]
- 38.Giavarina D. Understanding Bland Altman analysis. Biochem Med 2015;25:141–51. 10.11613/BM.2015.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bulger EM, Kuhls DA, Campbell BT, Bonne S, Cunningham RM, Betz M, Dicker R, Ranney ML, Barsotti C, Hargarten S, et al. . Proceedings from the medical Summit on firearm injury prevention: a public health approach to reduce death and disability in the US. J Am Coll Surg 2019;229:415–30. e412. 10.1016/j.jamcollsurg.2019.05.018 [DOI] [PubMed] [Google Scholar]
- 40.Gabbe BJ, Simpson PM, Harrison JE, Lyons RA, Ameratunga S, Ponsford J, Fitzgerald M, Judson R, Collie A, Cameron PA. Return to work and functional outcomes after major trauma: who recovers, when, and how well? Ann Surg 2016;263:623–32. 10.1097/SLA.0000000000001564 [DOI] [PubMed] [Google Scholar]
- 41.Sims DW, Bivins BA, Obeid FN, Horst HM, Sorensen VJ, Fath JJ. Urban trauma: a chronic recurrent disease. J Trauma 1989;29:940–7. [PubMed] [Google Scholar]
- 42.Whiteside LK, Darnell D, Jackson K, Wang J, Russo J, Donovan DM, Zatzick DF. Collaborative care from the emergency department for injured patients with prescription drug misuse: an open feasibility study. J Subst Abuse Treat 2017;82:12–21. 10.1016/j.jsat.2017.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rahurkar S, Vest JR, Menachemi N. Despite the spread of health information exchange, there is little evidence of its impact on cost, use, and quality of care. Health Aff 2015;34:477–83. 10.1377/hlthaff.2014.0729 [DOI] [PubMed] [Google Scholar]
- 44.Rockett IRH, Putnam SL, Jia H, Chang CF, Smith GS. Unmet substance abuse treatment need, health services utilization, and cost: a population-based emergency department study. Ann Emerg Med 2005;45:118–27. 10.1016/j.annemergmed.2004.08.003 [DOI] [PubMed] [Google Scholar]
- 45.Finnell JT, Overhage JM, Grannis S, 2011. All health care is not local: an evaluation of the distribution of emergency department care delivered in Indiana. AMIA Annual Symposium proceedings AMIA Symposium 409–16. [PMC free article] [PubMed] [Google Scholar]
- 46.Horrocks D, Kinzer D, Afzal S, Alpern J, Sharfstein JM. The adequacy of individual hospital data to identify high Utilizers and assess community health. JAMA Intern Med 2016;176:856–8. 10.1001/jamainternmed.2016.1248 [DOI] [PubMed] [Google Scholar]
- 47.Massoudi BL, Marcial LH, Tant E, Adler-Milstein J, West SL. Using health information exchanges to calculate clinical quality measures: a study of barriers and facilitators. Healthc 2016;4:104–8. 10.1016/j.hjdsi.2016.04.003 [DOI] [PubMed] [Google Scholar]
- 48.American College of Surgeons Committee on Trauma Resources for optimal care of the injured patient: 2014. 6th edn Chicago, IL: American College of Surgeons, 2014. [Google Scholar]
- 49.Poon SJ, Greenwood-Ericksen MB, Gish RE, Neri PM, Takhar SS, Weiner SG, Schuur JD, Landman AB. Usability of the Massachusetts prescription drug monitoring program in the emergency department: a mixed-methods study. Acad Emerg Med 2016;23:406–14. 10.1111/acem.12905 [DOI] [PubMed] [Google Scholar]
- 50.Zech J, Husk G, Moore T, Shapiro J. Measuring the degree of unmatched patient records in a health information exchange using exact matching. Appl Clin Inform 2016;07:330–40. 10.4338/ACI-2015-11-RA-0158 [DOI] [PMC free article] [PubMed] [Google Scholar]