Abstract
Toll-like receptor 2 (TLR2) recognizes and responds to threats early on in bacterial infections and can influence the downstream immune response to the host’s benefit or detriment. Therapeutically modulating TLR2 signaling represents an under-utilized opportunity to moderate the immune response to infection to promote improved outcome for the host.
Keywords: innate immunity, TLR2, bacterial infection, immunotherapy
TLR2 Signaling and the Immune Response
Toll-like receptors (TLRs) are a family of pattern recognition receptors (PRRs) within the innate immune system responsible for early recognition of invading pathogens. While all 10 TLRs expressed in humans are capable of responding to pathogen-associated molecular patterns (PAMPs), Toll-like receptor 2 is considered to be the most promiscuous receptor among them, as it recognizes a vast repertoire of ligands derived from a variety of pathogen sources. In addition, TLR2 is also capable of recognizing endogenous danger-associated molecular patterns (DAMPs), including heat shock proteins and high mobility group box 1 protein (HMGB1), which are released as a result of necrosis and tissue damage during infection. This wide-ranging library of PAMPs and DAMPs is due to the unique ability of TLR2 to heterodimerize with its fellow receptors TLR1 or TLR6. These TLR2/1 and TLR2/6 heterodimers are capable of differentiating and binding different ligands, further broadening the scope of TLR2 signaling. Furthermore, TLR2 is expressed on a wide range of cell types, including immune, endothelial, and epithelial cells. Taken together, these characteristics highlight the importance of TLR2 as a frontline receptor during bacterial infection [1].
Following ligand binding, the TLR2 heterodimer initiates an intracellular signaling cascade culminating in NF-κB activation, inflammasome assembly, and the subsequent production of key inflammatory cytokines. This early response to bacterial infection can help shape the downstream immune response, which can have critical implications in disease course and host outcome. As a result, TLR2 often plays a dual role during infection. On one hand, activation of TLR2 can generate beneficial pro-inflammatory responses critical in controlling infection and promoting bacterial clearance [2–3]. On the other hand, however, excessive TLR2 signaling can contribute to tissue damage and disease progression due to the disproportionate amounts of inflammation produced [4–5]. Therefore, it is vital to understand how TLR2 signaling contributes to the host immune response during bacterial infection. Because TLR2 signaling is implicated in a wide range of bacterial infections and has been shown to influence downstream immune responses, this receptor represents an appealing target for therapeutic intervention. Furthermore, its unique ability among the TLRs to heterodimerize with TLR1 or TLR6 presents novel opportunities to design more targeted therapies to reduce detrimental off-target effects. For these reasons, we will review the potential of TLR2 as a therapeutic target and highlight avenues regarding its application within the realm of immunotherapy that remain open to investigation.
Therapeutic Inhibition of TLR2: Sepsis and C. difficile Infection
The rapid initiation of pro-inflammatory responses by TLR2 is critical in controlling infection, however, dysregulation of this signaling can lead to excessive release of pro-inflammatory cytokines. Therefore, inhibiting TLR2 activation can help in curbing an overactive immune response and avoid damaging immunopathology. In a mouse model of polymicrobial sepsis, treatment with an anti-TLR2 antibody decreased systemic inflammation and bacterial burden, promoting overall improved outcome in mice experiencing severe sepsis [4]. TLR2 signaling is also detrimental in a mouse model of Clostridium difficile infection (CDI). TLR2 signaling contributes to CDI pathogenesis via its ability to recognize one of the virulence factors produced by C. difficile, CDT, leading to a robust generation of inflammation. Inhibiting the response of TLR2 to this virulence factor may reduce host tissue damage during infection, thus leading to overall improved outcome during CDI [5].
Among the tools available for studying the therapeutic potential of TLR2 inhibition are anti-TLR2 antibodies [4], small molecule inhibitors, synthetic inhibitory peptides [6], and TLR2 inhibitors produced by other pathogens (Figure 1), such as the TLR2 antagonist sulfoglycolipid made by Mycobacterium tuberculosis [7]. While these tools are available within the research setting, TLR2 inhibitors have yet to make the jump from bench to bedside application. The design and development of clinically relevant TLR2 inhibitors represents a therapeutic opportunity not yet exploited and would greatly benefit from further advancement.
Figure 1 -.
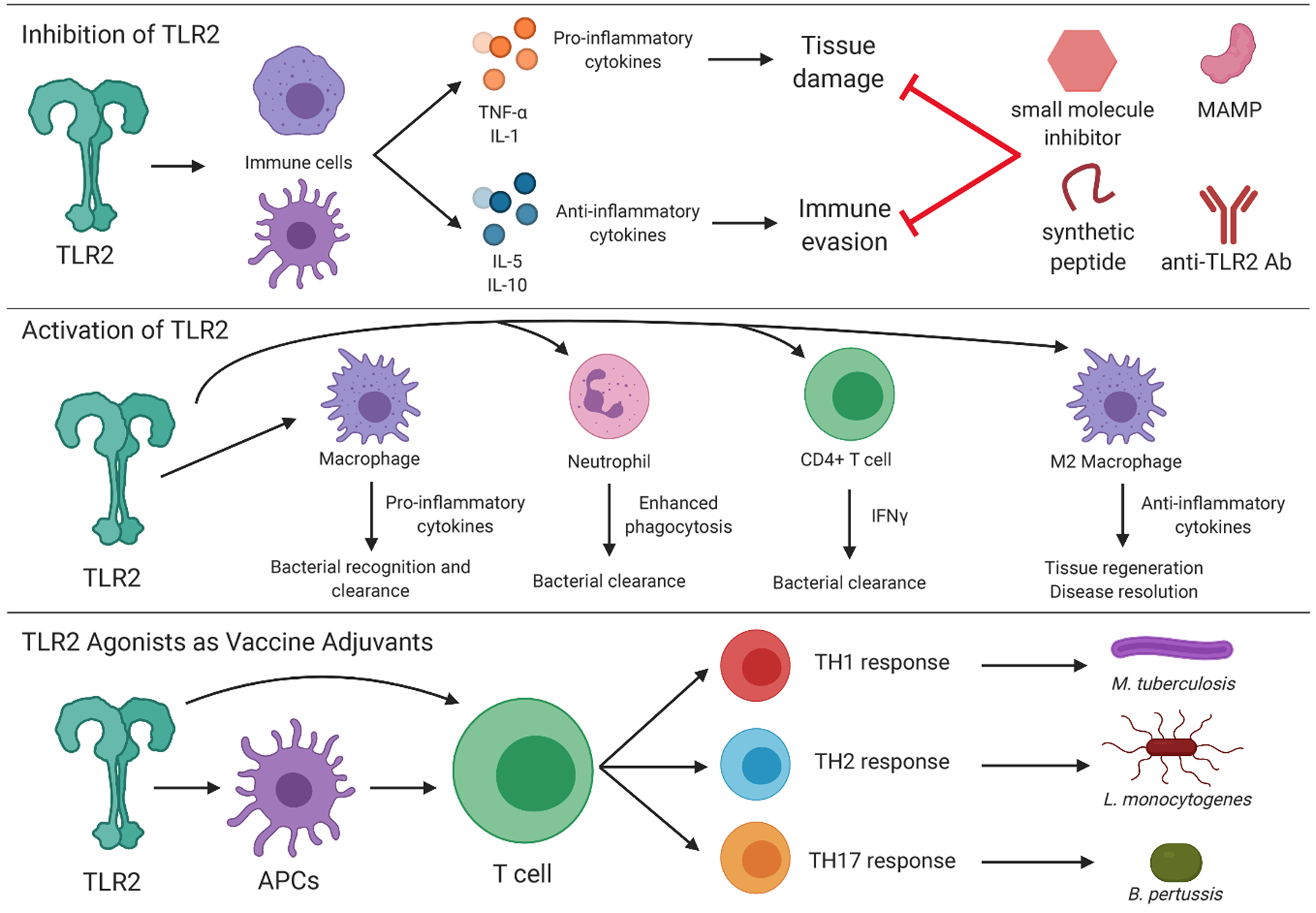
Therapeutic modulation of TLR2 can influence the downstream immune response and promote better host outcome during bacterial infection. TLR2-targeted inhibitors can serve to limit generation of excessive, tissue-damaging pro-inflammatory cytokines or evasion of the host immune system, while activation of TLR2 signaling can aid in the production of beneficial host immune responses generated by a wide variety of cell types. TLR2 agonists can also act as potent vaccine adjuvants due to their ability to induce many different T cell responses. MAMP = microbe-associated molecular pattern
Overall, dysregulated TLR2 signaling can contribute to disease pathology and inhibition of this response could improve disease outcome by reducing damaging inflammation.
Therapeutic Activation of TLR2: TB and MRSA
The early induction of robust inflammatory responses by TLR2 is critical in fighting bacterial infection, therefore, therapeutic activation of TLR2 can further enhance the host ability to control and clear the pathogen. In a mouse model of M. tuberculosis infection, TLR2 activation on CD4+ T cells leads to an increase in protective IFN-γ secreting T cells [3]. In addition, administration of a TLR2 agonist protected mice against infection with methicillin-resistant Staphylococcus aureus by enhancing phagocytosis and the bactericidal activity of neutrophils [2]. Finally, TLR2 activation via a bacterially-derived protein induced differentiation of M2 macrophages, reduction of pro-inflammatory cytokines, and promoted survival in a mouse model of polymicrobial sepsis [8]. Despite the differing cell types and mechanisms involved in protection (Figure 1), activation of TLR2 is beneficial to the host in these models of bacterial infection.
In the previous section, we highlighted how inhibition of TLR2 was protective during sepsis [4], however, in the example given above, activation of TLR2 was also protective in the same model [8]. Though the upstream mechanisms seem to act in opposition to each other, therapeutic manipulation of TLR2 signaling ultimately culminates in a reduction of the pro-inflammatory cytokine TNF-α and provides protection in a disease model characterized by overwhelming systemic inflammation. This highlights how vital it is to understand the role of TLR2 signaling within the context of a specific infection, the effect of this signaling on the host immune response, and what manipulations of that signaling will produce a desirable end result, regardless of what the specific manipulation is. That understanding, in turn, can aid in design, development, and selection of the best suited TLR2-targeted therapeutic treatment.
Overall, activating TLR2 signaling in contexts where generation of robust pro-inflammatory responses are beneficial to the host and aid in controlling/clearing bacterial infection serves as a promising therapeutic option during bacterial infection.
TLR2 Agonists: Vaccine Adjuvants
Many TLR2 agonists have potential as vaccine adjuvants due to their ability to induce robust and diverse pro-inflammatory immune responses. For example, in an experimental Bordetella pertussis vaccine tested in mice, combining a B. pertussis-derived TLR2 agonist with a STING agonist was capable of inducing protective B. pertussis-specific Th17 responses [9]. However, during murine immunization with the Mycobacterium bovis BCG strain, TLR2 agonists were identified as potent Th1 polarizing adjuvants [10]. Finally, a Neisseria meningitidis-derived TLR2 agonist was capable of inducing antigen specific responses, including elevated Th1 and Th2 cytokines [11]. It is clear that TLR2 agonists are capable of inducing a wide variety of T cell responses to immunization (Figure 1), a characteristic that can aid in tailoring vaccines to elicit specific immune responses. Including TLR2-derived adjuvants capable of generating specific T cell responses to the vaccine antigen in question will allow for the design of more effective, targeted vaccines. Therefore, understanding the role of TLR2 signaling and the downstream T cell response in the context of interest is an important factor to consider when utilizing TLR2 agonists during vaccine development. Overall, TLR2 agonists can serve as promising vaccine adjuvants and should be considered when designing novel or next-generation vaccines.
Conclusion
TLR2 plays a vital role in the early innate immune response to bacterial infection through its ability to initiate pro-inflammatory cytokine release and influence the downstream immune response. Therefore, modulation of TLR2 signaling represents a novel target for therapeutic intervention. The dual role of TLR2 during infection highlights the critical need to fully understand the mechanisms of signaling within specific disease contexts. TLR2 inhibition can help dampen an overwhelming inflammatory response and prevent tissue damage, while activation can induce the release of pro-inflammatory mediators to control and/or clear bacterial infection. Additionally, TLR2 agonists can help generate protective immune responses when used as vaccine adjuvants. Understanding which downstream responses are desirable in which disease models can aid in the design, development, and selection of novel therapeutics. Overall, the TLR2 signaling axis represents a promising target for therapeutic intervention in a number of bacterial infection models, and can serve as another tool in the realm of immunotherapy.
Acknowledgments
Work from the authors’ laboratory was support by NIH grants R01 AI124214 (WP) and T32AI007496 (MS)
References
- 1.de Oliviera Nascimento L, Massari P, & Wetzler L (2012). The Role of TLR2 in Infection and Immunity . Frontiers in Immunology . Retrieved from https://www.frontiersin.org/article/10.3389/fimmu.2012.00079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen Y-G, Zhang Y, Deng L-Q, Chen H, Zhang Y-J, Zhou N-J, … Min W-P (2016). Control of Methicillin-Resistant Staphylococcus aureus Pneumonia Utilizing TLR2 Agonist Pam3CSK4. PloS One, 11(3), e0149233–e0149233. 10.1371/journal.pone.0149233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reba SM, Li Q, Onwuzulike S, Ding X, Karim AF, Hernandez Y, … Rojas RE (2014). TLR2 engagement on CD4(+) T cells enhances effector functions and protective responses to Mycobacterium tuberculosis. European Journal of Immunology, 44(5), 1410–1421. 10.1002/eji.201344100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lima CX, Souza DG, Amaral FA, Fagundes CT, Rodrigues IPS, Alves-Filho JC, … Teixeira MM (2015). Therapeutic Effects of Treatment with Anti-TLR2 and Anti-TLR4 Monoclonal Antibodies in Polymicrobial Sepsis. PloS One, 10(7), e0132336–e0132336. 10.1371/journal.pone.0132336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cowardin CA, Buonomo EL, Saleh MM, et al. The binary toxin CDT enhances Clostridium difficile virulence by suppressing protective colonic eosinophilia. Nat Microbiol. 2016;1(8):16108 Published 2016 Jul 11. doi: 10.1038/nmicrobiol.2016.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ebner S, Trieb M, Schönfeld M, Wietzorrek G, & Santos-Sierra S (2018). Decoy peptides derived from the extracellular domain of toll-like receptor 2 (TLR2) show anti-inflammatory properties. Bioorganic & Medicinal Chemistry, 26(16), 4615–4623. 10.1016/j.bmc.2018.07.013 [DOI] [PubMed] [Google Scholar]
- 7.Blanc L, Gilleron M, Prandi J, Song O-R, Jang M-S, Gicquel B, … Nigou J (2017). Mycobacterium tuberculosis inhibits human innate immune responses via the production of TLR2 antagonist glycolipids. Proceedings of the National Academy of Sciences of the United States of America, 114(42), 11205–11210. 10.1073/pnas.1707840114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed A, Dolasia K, & Mukhopadhyay S (2018). Mycobacterium tuberculosis PPE18 Protein Reduces Inflammation and Increases Survival in Animal Model of Sepsis. The Journal of Immunology, 200(10), 3587 LP – 3598. 10.4049/jimmunol.1602065 [DOI] [PubMed] [Google Scholar]
- 9.Allen AC, Wilk MM, Misiak A, Borkner L, Murphy D, & Mills KHG (2018). Sustained protective immunity against Bordetella pertussis nasal colonization by intranasal immunization with a vaccine-adjuvant combination that induces IL-17-secreting TRM cells. Mucosal Immunology, 11(6), 1763–1776. 10.1038/s41385-018-0080-x [DOI] [PubMed] [Google Scholar]
- 10.Johndrow CT, Goldberg MF, Johnson AJ, Ng TW, Kunnath-Velayudhan S, Lauvau G, … Porcelli SA (2018). Suppression of Th1 Priming by TLR2 Agonists during Cutaneous Immunization Is Mediated by Recruited CCR2(+) Monocytes. Journal of Immunology (Baltimore, Md. : 1950), 201(12), 3604–3616. 10.4049/jimmunol.1801185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mosaheb M, & Wetzler LM (2018). Meningococcal PorB induces a robust and diverse antigen specific T cell response as a vaccine adjuvant. Vaccine, 36(50), 7689–7699. 10.1016/j.vaccine.2018.10.074 [DOI] [PMC free article] [PubMed] [Google Scholar]


