PURPOSE:
Identifying nontechnical, teamwork competencies (knowledge, skills, and attitudes) underlying coordination within and across the network of teams—or multiteam system (MTS) involved in cancer care is foundational to optimizing high-quality cancer care.
METHODS:
A multidisciplinary group of cancer care stakeholders refined an initial list of competency statements during three rounds of a web-based modified Delphi survey.
RESULTS:
Panelists reached consensus on a final list of four domains and 20 associated team-based competencies important for effective coordination in cancer care MTS.
CONCLUSION:
This study provides an initial foundation for testing, modifying, measuring and evaluating the impact of identified competencies on care coordination, outcomes, and costs, for people being screened, treated, or surviving cancer.
INTRODUCTION
The concept of clinicians improving coordination of care for patients with cancer is not new.1 The relationship between better care coordination and lower costs, increased patient satisfaction, and improved patient outcomes is well established.2,3 For nearly 20 years, the National Academy of Sciences (NAS) and other organizations have called for better care coordination to improve the quality of cancer care delivery.1,3-5 Care coordination is the provision of a combination of health services and information that meets a patient's needs and includes the connections within and across those services and settings—putting them in the right order and appropriately using resources of the community. The goal is to focus on interactions with patients and families, clarify clinical care decisions, advise patients and their families, and help them cope with the social and emotional implications of disease or illness.6 Since the original call by the NAS to improve care coordination, several health system changes, information technology tools, and new models of care have been introduced to improve care coordination, yet limited research has examined the nontechnical teamwork competencies health care team members need to coordinate care effectively in the team-of-teams, or multiteam system (MTS), involved in cancer-related care from screening and diagnosis through treatment, and survivorship.
Building on work in other industries,7-13 research on teamwork in health care and interventions designed to strengthen teamwork competencies among health care workers has expanded over the past 15 years. For example, the highly successful, evidence-based Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) program developed by the Agency for Health Research and Quality,14 anesthesia resource management training,15 and team-oriented interprofessional education programs16 drew from this body of research. However, many interventions have focused on acute, in-patient care or on teamwork within a single specialty, clinic, or delivery organization. To improve coordination among the many disciplines involved in cancer care, there is a need to explore the teamwork competencies needed to team well across disciplinary, geographic, and organizational boundaries.
MTSs in Cancer Care
One method for conceptualizing the number of different players involved in cancer care is the concept of MTS. In the context of health care, a MTS is defined as “interdependent, highly specialized, and geographically dispersed ‘team-of-teams’ involved in the care and health of a particular person.”12 In cancer care, this “team-of-teams” responsible for coordinating patient care often include: physicians, nurses, advanced practice registered nurses, physician assistants, palliative care specialists, clinicians providing psychosocial support, spiritual workers, rehabilitation clinicians, pharmacists, hospice clinicians, and others.1 Figure 1 illustrates an example of a cancer care MTS. Although the figure is not intended to reflect the organization of teams by practice or clinic, it provides a heuristic for thinking about interactions and interdependencies among the teams or groups involved in delivering whole-person care for people with cancer. For example, in addition to oncology specialists, the figure includes other specialties that may be managing other chronic conditions,17 and hospitalists. The figure also shows the patient advocate team at the center of care coordination activities and recognizes the contribution of their boundary-spanning role to “facilitate transactions and the flow of information between people or groups who either have no physical or cognitive access to one another.”18 Compared with co-located procedure-driven teams, these cancer care MTSs must coordinate care tasks and decisions across geographic, organizational, and disciplinary boundaries. However, little work to date has developed consensus on the knowledge, skills, and attitudes needed to team effectively in these larger, more complex care-delivery systems.
Fig 1.
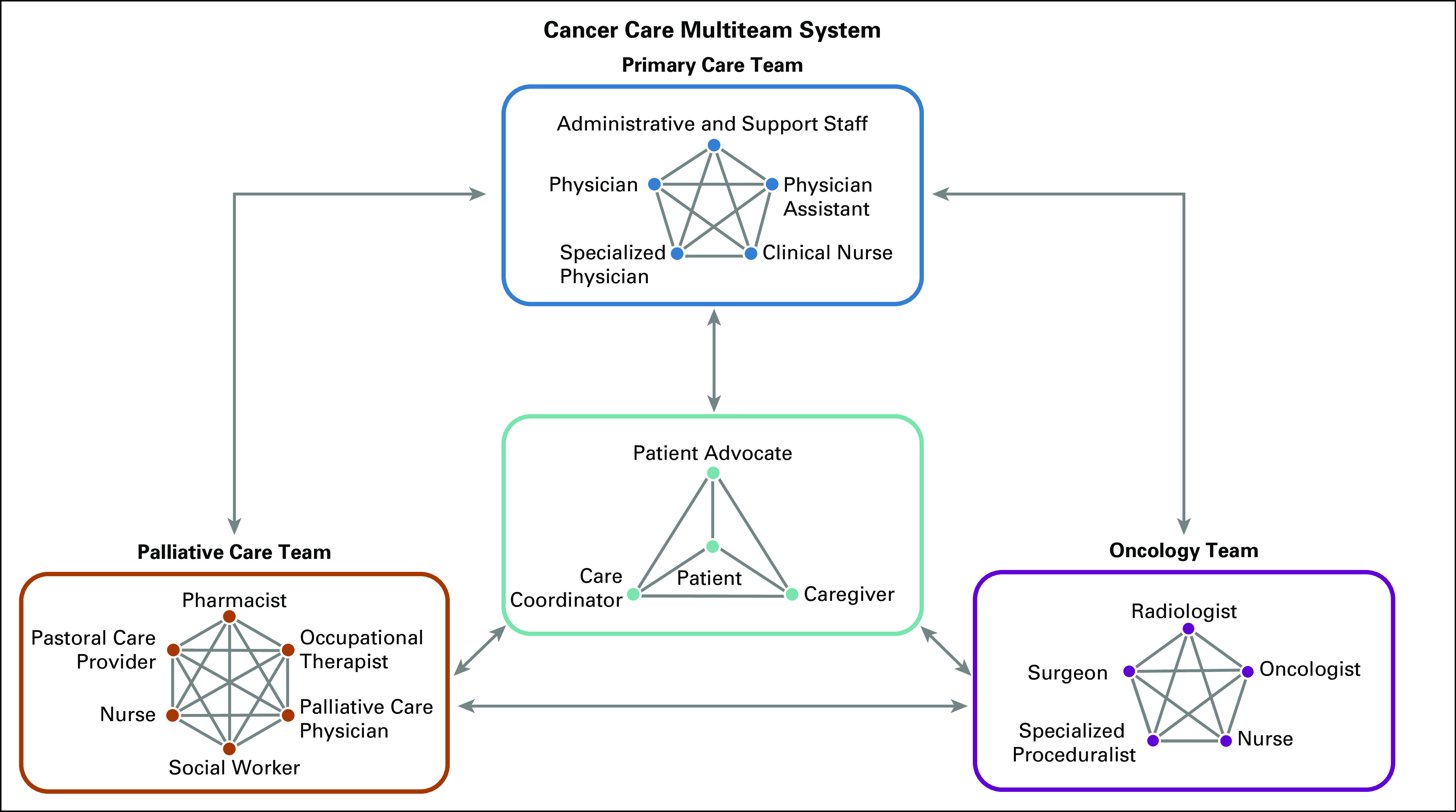
Cancer care multiteam system. A specialized physician is defined, for purposes of this study, as a physician who provides care for patients with diabetes, hypertension, mental health, and other chronic conditions. A specialized proceduralist is defined, for purposes of this study, as a hospital-based physician who specializes in performing various invasive, skilled procedures.
The scant literature on effective care coordination within the context of cancer care MTSs19 and the success of other industries7-13 to improve operations, safety, and coordination in larger teams-of-teams inspired our interest to understand nontechnical teamwork competencies in cancer MTS.
Expert Panel Discussion
To begin identifying potential teamwork competencies for effective teaming in a cancer care MTS, we convened a panel session at the 2017 Interdisciplinary Network of Group Research conference. Session panelists had extensive research careers studying team performance in health care and health services research. Panelists were asked to consider what team-oriented competences are important for MTS performance in cancer care delivery. Their recommendations provided an initial foundation for developing a Delphi study instrument.
METHODS
We conducted a 3-round modified Delphi survey of 104 panelists to identify gaps in an initial list of competencies and to develop a consensus-based list of nontechnical competencies for teaming effectively in cancer MTSs. Respondents who consented to participate in the first round were invited to rounds 2 and 3. Each survey included an introduction with basic definitions and an explanation of the survey method. After rounds 1 and 2, responses were aggregated and shared with the respondents to facilitate continued participation and consensus building. Each survey can be found in the Data Supplement. The modified Delphi method20,21 is used widely for consensus development, evaluation, and program planning to inform research agendas and policy determinations, and as a method to generate theoretical frameworks or models.
This study was deemed nonhuman subjects’ research by the National Cancer Institute Office of Human Subjects Research Protections (19-NCI-00825) and the Westat Institutional Review Board (No. 00000695).
Establishing the Survey Panel
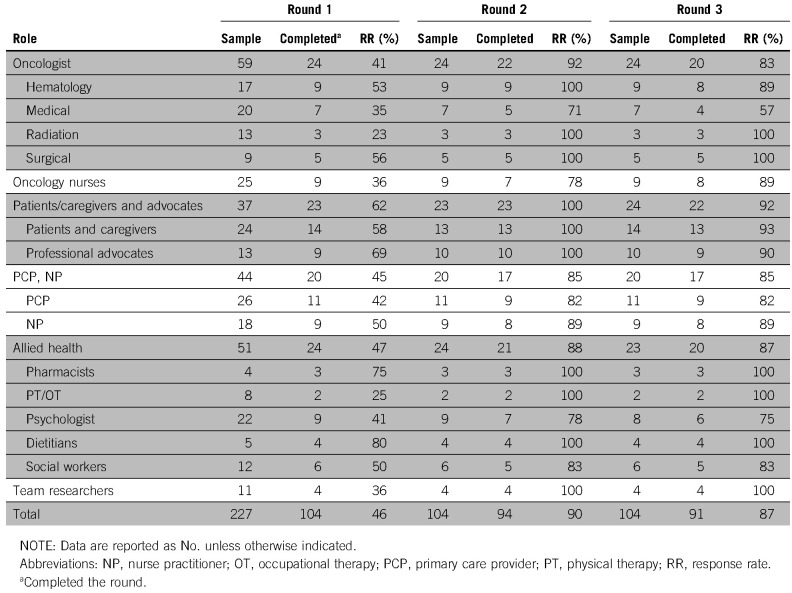
A multidisciplinary list of 227 professionals involved in cancer care delivery were invited to participate in the study. The composition of respondents for each survey round is listed in Table 1. Participants’ roles in health care were as follows: oncologists, 24%; oncology nurses, 11%; patients and patient advocates, 16%; primary doctors and nurses, 19%; allied health professionals (eg, pharmacists, physical and occupational therapists, psychologists, dietitians, social workers), 22%; and team researchers, 4%.
TABLE 1.
Sample and Response Rates by Respondent Category and Survey Round
RESULTS
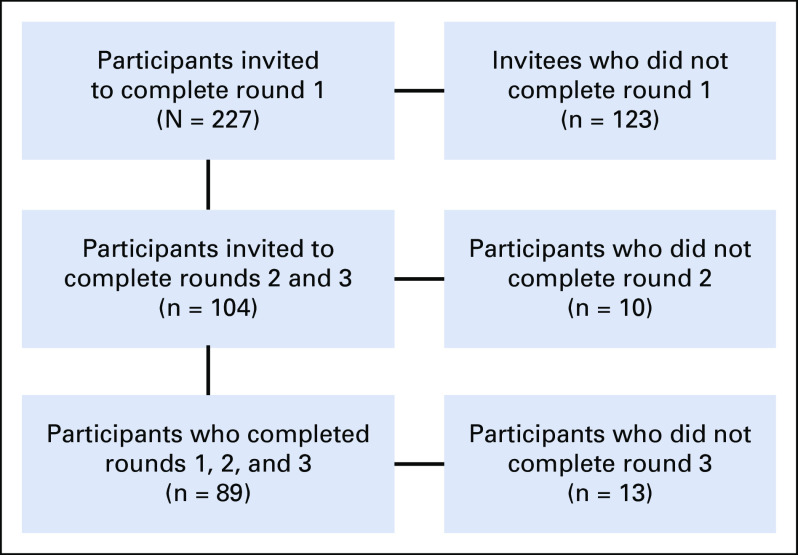
A total of 227 participants were invited to participate in the online Delphi surveys. A total of 104 completed round 1 (response rate, 46%). Of the 104 completing round 1, 94 completed round 2 and 91 completed round 3 (Fig 2). Eighty-nine respondents completed all 3 rounds.
Fig 2.
Survey participation per round.
The Data Supplement details the progression of condensing and refining 53 initial competency statements across 6 domains, which represent teamwork challenge areas commonly faced by clinical teams, to 27 items in round 2, and to 17 competency statements across 4 domains in round 3. Competency domains were developed through qualitative analysis on the expert-panel discussion transcripts and represented 6 teamwork challenge areas commonly faced by clinical teams: understanding of interactions among multiple teams, appreciation of other teams’ perspectives, coordination among teams, support of other teams, patient integration in teams, and leadership. The threshold used to define consensus for each competency was 70% agreement across respondents, similar to recent Delphi studies on developing competencies in health-related professions.21-24 Importance ratings for each item by round and list of domains are summarized in the Data Supplement.
Round 1
The average mean score in round 1 across all 53 items was 4.20 (standard deviation [SD], 0.34), with 45 items rated as “important” or “extremely important” by ≥ 70% of all respondents. Twenty-one percent of these 45 items were also ranked by participants in their personal list of top 10 competencies they viewed as most important. Eighteen items were rated “not relevant” or duplicative by > 3 respondents. When comparing items across domains, competencies related to “patients being perceived as integral members of the healthcare team” received consistently high importance scores and were more often ranked extremely important compared with other domains. Conversely, competencies related to “supporting and enabling MTS work” were most often rated as duplicative or not relevant.
After rating the competencies in each domain, respondents were also asked to comment on the wording of items, point to duplicative items, and add any competencies relevant to each domain not listed. Open-ended responses highlighted the importance of team equity, trust, interdisciplinary collaboration, and the inclusion of the patients, caregivers, patient advocates, and navigators in the cancer care MTS model. Several respondents expressed that competencies regarding the “lack of appreciation of other teams’ perspectives” were unrealistic given the limited information available across the teams and with patients or caregivers. An emergent theme surrounding “intentional coordination” was the importance of effective communication, considering the variations in best practices and culture across teams and disciplines. Few commented on striking the right balance between advocating for one's team versus participating in shared decision-making with members in other teams. Respondents offered varied opinions about the relative importance of being proficient in using communication technologies versus interpersonal communication skills. Others noted that competency statements related to leadership transcend all areas of team functioning and that MTSs typically do not function under formal hierarchical leadership structures. On the basis of the ratings, rankings, and qualitative responses from the round 1 survey, 7 items were rephrased and combined with other items to be more actionable, and 19 items were dropped (Data Supplement).
Round 2
In round 2, competency statements were presented without predefined domains and randomly ordered for each respondent. Respondents were asked to again select their top 10 items. The 27 retained competencies were, on average, ranked in the top 10 by 37% of respondents, with 5 items ranked as top 10 by > 50% of respondents. Respondents were also asked to comment on how they ranked competencies, still noting duplicate and overlapping or varying order items. Seven items were dropped from round 2 because of redundancy and perceived lack of specificity.
Round 3
Of the 20 competency statements advanced to round 3, 17 were rated as “important” or “extremely important” by ≥ 70% of all respondents, with an average mean score of 4.26 (SD, 0.20) and 3 items scoring below the consensus threshold were dropped (Data Supplement). The list of 17 competencies included 7 that were qualitatively reviewed and grouped into 4 domains: shared mental models in a multiteam, communication across teams, coordination, and providing patient-centered care in a multiteam. When comparing items across the final 4 domains, the highest-rated competency statements related to providing patient-centered care (mean, 4.6; SD, 0.63), communication (mean, 4.25; SD, 0.8), coordination (mean, 4.19; SD, 0.85), and shared mental models (mean, 4.15; SD, 0.76).
Importance by Respondent Group
Figure 3 shows the percentage of respondents in each disciplinary group who rated items as important or extremely important by domain in round 3. Although importance ratings differed among some groups, differences were not statistically significant in an overall 1-way analysis of variance (ANOVA) across all items (F(5,85) = 1.92; P = .10). We then collapsed responses of oncologists, primary care providers, and nurse practitioners into a single providers group and combined responses of oncology nurses with other allied health professions. A second 1-way ANOVA revealed that the providers group perceived coordination competencies to be less important (F(3,86) = 3.16; P = .03), and perceived patient-centered competencies to be less important (F(3,87) = 3.01; P = .03) than those in the group of nurses and allied health professions.
Fig 3.
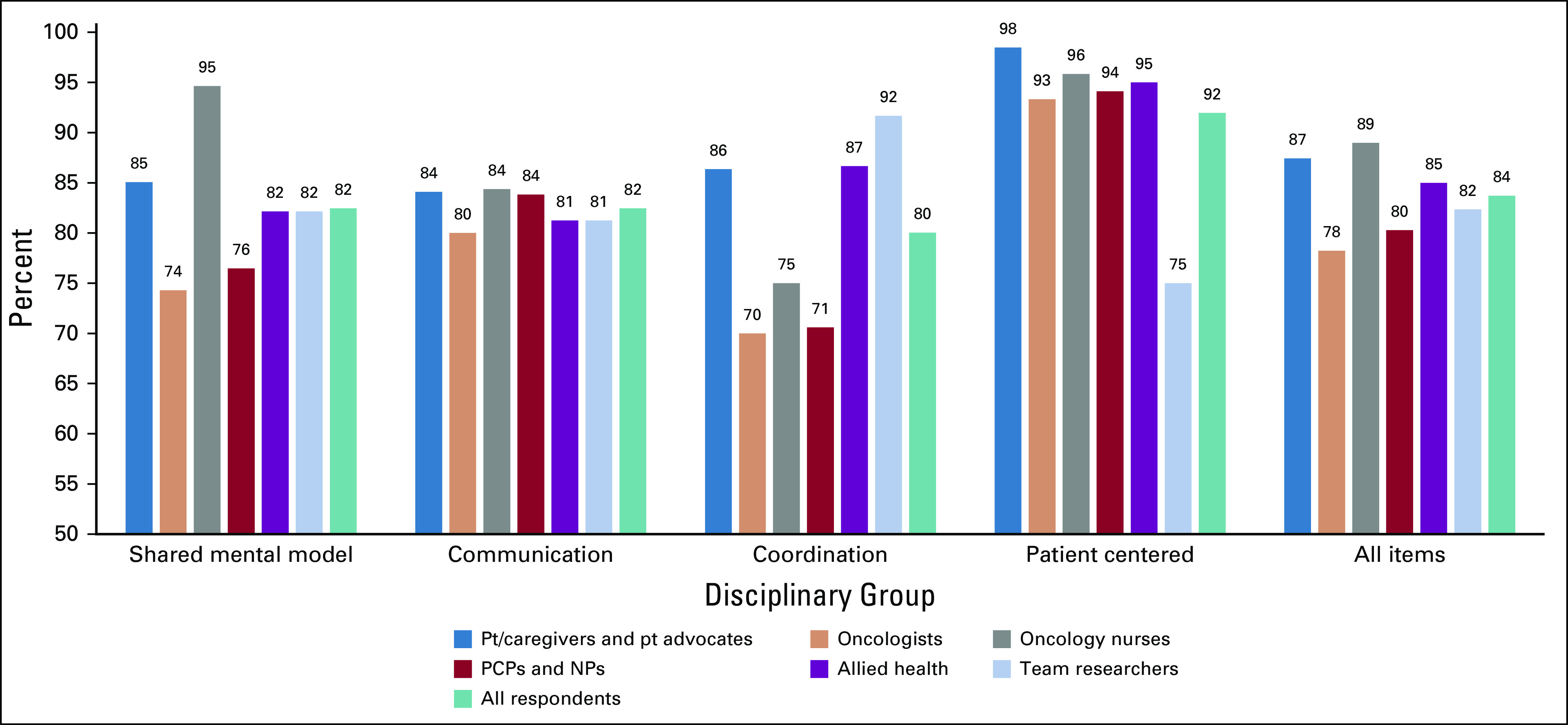
Percentage of respondents in each disciplinary group who rated items as important or extremely important by domain in round 3. NP, nurse practitioner; PCP, primary care provider; Pt, patient.
DISCUSSION
Better coordination contributes to high-quality cancer care delivery and is critical to manage mindfully because the systems in which care is delivered have rapidly evolved from solo practice to large, comprehensive, multiteam care delivery systems spanning large geographic regions.2 In this study, we attempted to borrow the concept of team competencies in MTS from high-risk industries, systems engineering, and human factors research and apply it to the science of cancer care delivery in an effort to enhance the delivery of high-quality cancer care.
Using a modified Delphi process, 53 nontechnical teamwork competency statements were refined to 17 statements across 4 domains: patient-centered care, effective communication, coordination, and shared mental models. Notably, the highest-rated domain was patient-centered care, defined as “providing care that is respectful of, and responsive to, individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions.”25 This finding may indicate clinicians and patients believe patient-centered care is challenging for cancer care teams to provide, or for patients to receive, in large fragmented MTSs, or both.
Practically, this work provides an initial foundation for practicing clinicians and administrators interested in advancing coordination and sustained use of these competencies in daily practice. For example, practices might consider adapting or integrating parts of the free TeamSTEPPS 2.0 curriculum (https://www.ahrq.gov/teamstepps) into practice continuous learning opportunities or leverage other curricula targeting some of the competencies identified. Also, simply thinking and talking regularly about the multiple teams engaged in delivering whole-person care for a particular patient or panel of patients and the interdependencies among these teams can be a useful way to integrate the concept of MTS into practice culture.26
Future research should focus on developing or identifying measures of the teamwork knowledge, skills, attitudes, and behaviors identified, as well as interventional strategies for efficiently developing and sustaining these skills and behaviors in practice. Although measures of some of the identified competency areas exist, they need to be adapted or validated for use in cancer care and in MTS scenarios where multiple, distributed teams are involved in coordinating comprehensive care.27-29 Best practices for assessing these competencies in practice could also be adapted from existing interprofessional education recommendations and guidelines (eg, ASCO and Oncology Nursing Society assessment recommendations; Interprofessional Education Collaborative recommendations30). As evaluations of prior teamwork-oriented interventions like TeamSTEPPS have found,31-34 innovative multilevel intervention strategies are likely needed to effectively prepare and support health care team members, patients, and caregivers teaming in complex organizational systems like cancer care delivery. In addition, given the increased use of technology-based communication and coordination tools, evidence-based strategies for developing and sustaining these skills in increasingly virtual MTSs is important. More research is needed to understand the requirements needed to achieve consistent improvement in coordinating MTS team-based care. Future studies should examine the modes and methods of training acceptable for the broadest group of cancer care stakeholders, as well as determining if there is equity in who is trained and whether training should include executive leadership of MTS. Identification of acceptable methods for strengthening patient and caregiver knowledge and skills to become better collaborators is also needed.
Although clinical teams may be motivated to practice team-based care, structural and system changes may create barriers to teams achieving optimal coordination across the disciplinary, geographic, and organizational boundaries that often characterize clinical MTSs. More research is needed to identify practical strategies for health care teams’ adaptation to the evolving structural and worksite policy changes that impede effective team-based care in an MTS.
Our study is limited in several ways. There are no clear guidelines for defining experts for a modified Delphi study. Other limitations included use of the modified Delphi method, which excludes face-to-face interaction; through a variety of statistical and qualitative analyses, we determined the consensus of competency statements, not the stakeholders. Our sample was small and may not be representative of all US licensed professionals. Finally, we had a higher proportion of patients and patient advocates represented in our sample compared with other stakeholder categories.
The competencies identified through the Delphi survey provide an initial basis for testing, modifying, measuring, and evaluating their impact on care coordination, costs, and patient outcomes. Observational and interventional research is needed to validate, refine, or refute this initial work. This framework provides grounding for research examining how to develop and sustain these competencies in daily practice, what modes and methods training are acceptable, and how best to facilitate patient and caregiver’s roles as the central team in the cancer care MTS. We also invite readers to explore the Journal of Oncology Practice Special Series on Teams and Cancer Care35 to access the foundational work of the National Cancer Institute and ASCO to explore team-based approaches to delivering coordinated, patient-centered cancer care from the perspective of oncology clinicians, researchers who study teams, and, most importantly, the perspective of patients and their advocates.
SUPPORT
Supported by the Division of Cancer Control and Population Sciences, National Cancer Institute.
AUTHOR CONTRIBUTIONS
Conception and design: Veronica Chollette, Sallie J. Weaver, Grace Huang, Sophia Tsakraklides
Administrative support: Sophia Tsakraklides
Provision of study material or patients: Grace Huang
Collection and assembly of data: Veronica Chollette, Grace Huang, Sophia Tsakraklides, Shin-Ping Tu
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Identifying Cancer Care Team Competencies to Improve Care Coordination in Multiteam Systems: A Modified Delphi Study
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Shin-Ping Tu
Stock and Other Ownership Interests: AbbVie (I), Abbott Laboratories (I), Conduent (I), Johnson & Johnson (I), McKesson (I), Medtronic (I), Pfizer (I)
No other potential conflicts of interest were reported.
REFERENCES
- 1. Balogh E, Ganz PA, Levit L (eds): Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC, The National Academies Press, 2013. [PubMed] [Google Scholar]
- 2. Institute of Medicine, Committee on Quality of Health Care in America: Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC, National Academies Press, 2001. [Google Scholar]
- 3. Hewitt M, Simone JV (eds): Ensuring Quality Cancer Care. Washington, DC, The National Academies Press, 1999. [PubMed] [Google Scholar]
- 4. ASCO: The state of cancer care in America, 2017: A report by the American Society of Clinical Oncology. J Oncol Pract 13:e353-e394, 2017. [DOI] [PubMed]
- 5. Nass SJ, Amankwah FK, Madhavan G, et al (eds): Guiding Cancer Control: A Path to Transformation. Washington, DC, The National Academies Press, 2019. [PubMed] [Google Scholar]
- 6. Donaldson MS, Yordy KD, Lohr KN, et al (eds): Primary Care: America’s Health in a New Era. Washington, DC, National Academies Press, 1996. [PubMed] [Google Scholar]
- 7.DeChurch LA, Burke CS, Shuffler ML.at al: A historiometric analysis of leadership in mission critical multiteam environments. Leadersh Q 22:152-1692011 [Google Scholar]
- 8. Zaccaro SJ, Marks MA, DeChurch LA: Multiteam Systems: An Organization Form for Dynamic and Complex Environments. New York, NY, Routledge, 2011. [Google Scholar]
- 9. Marissa LS, Ramón R, Eduardo S, eds: Pushing the Boundaries: Multiteam Systems in Research and Practice. Bingley, UK, Emerald Group Publishing Limited, 2014:iii.
- 10. Vessey WB: Multiteam systems in the spaceflight context: Current and future challenges, in Marissa LS, Ramón R, Eduardo S, eds, Pushing the Boundaries: Multiteam Systems in Research and Practice. Bingley, UK, Emerald Group Publishing Limited, 2014:135-153. [Google Scholar]
- 11.Goodwin GF, Blacksmith N, Coats MR: The science of teams in the military: Contributions from over 60 years of research. Am Psychol 73:322-3332018 [DOI] [PubMed] [Google Scholar]
- 12. Anderson N, Ones DS, Sinangil HK, et al (eds): Handbook of Industrial Work, and Organizational Psychology. Newbury Park, CA, SAGE Publications Ltd, 2001. [Google Scholar]
- 13.Shuffler ML, Carter DR: Teamwork situated in multiteam systems: Key lessons learned and future opportunities. Am Psychol 73:390-4062018 [DOI] [PubMed] [Google Scholar]
- 14. https://www.ahrq.gov/teamstepps/evidence-base/teamstepps-research.html Agency for Healthcare Research and Quality: TeamSTEPPS: National Implementation Research/Evidence Base.
- 15.Howard SK, Gaba DM, Fish KJ, et al. : Anesthesia crisis resource management training: teaching anesthesiologists to handle critical incidents. Aviat Space Environ Med 63:763-7701992 [PubMed] [Google Scholar]
- 16.Johnson C: Team-based learning for health professions education: A guide to using small groups for improving learning [book review]. J Chiropr Educ 23:47-482009 [Google Scholar]
- 17.Larsen A, Broberger E, Petersson P: Complex caring needs without simple solutions: The experience of interprofessional collaboration among staff caring for older persons with multimorbidity at home care settings. Scand J Caring Sci 31:342-3502017 [DOI] [PubMed] [Google Scholar]
- 18.Long JC, Cunningham FC, Braithwaite J: Bridges, brokers and boundary spanners in collaborative networks: A systematic review. BMC Health Serv Res 13:158.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Walsh J, Harrison JD, Young JM, et al. : What are the current barriers to effective cancer care coordination? A qualitative study. BMC Health Serv Res 10:132.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Humphrey-Murto S, Varpio L, Wood TJ, et al. : The use of the Delphi and other consensus group methods in medical education research: A review. Acad Med 92:1491-14982017 [DOI] [PubMed] [Google Scholar]
- 21. Murphy MK, Black NA, Lamping DL, et al: Consensus development methods, and their use in clinical guideline development. Health Technol Assess 2:1-88, 1998. [PubMed]
- 22.Penciner R, Langhan T, Lee R, et al. : Using a Delphi process to establish consensus on emergency medicine clerkship competencies. Med Teach 33:e333-e3392011 [DOI] [PubMed] [Google Scholar]
- 23.Eubank BH, Mohtadi NG, Lafave MR, et al. : Using the modified Delphi method to establish clinical consensus for the diagnosis and treatment of patients with rotator cuff pathology. BMC Med Res Methodol 16:56.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Loblaw DA, Prestrud AA, Somerfield MR, et al. : American Society of Clinical Oncology Clinical Practice Guidelines: Formal systematic review-based consensus methodology. J Clin Oncol 30:3136-31402012 [DOI] [PubMed] [Google Scholar]
- 25.Okun S, Schoenbaum SC, Andrews D, et al. : Patients and health care teams forging effective partnerships.NAM Perspectives. Discussion Paper. National Academy of Medicine. 2014. https://nam.edu/perspectives-2014-patients-and-health-care-teams-forging-effective-partnerships/
- 26.Weaver SJ: From teams of experts to mindful expert teams and multiteam systems. J Oncol Pract 12:976-9792016 [DOI] [PubMed] [Google Scholar]
- 27.Baker DP, Amodeo AM, Krokos KJ, et al. : Assessing teamwork attitudes in healthcare: Development of the TeamSTEPPS teamwork attitudes questionnaire. Qual Saf Health Care 19:e492010 [DOI] [PubMed] [Google Scholar]
- 28.Keebler JR, Dietz AS, Lazzara EH, et al. : Validation of a teamwork perceptions measure to increase patient safety. BMJ Qual Saf 23:718-7262014 [DOI] [PubMed] [Google Scholar]
- 29. Marlow S, Bisbey T, Lacerenza C, et al: Performance measures for health care teams: A review. Small Group Res 49:306-356, 2018.
- 30. Interprofessional Education Collaborative: Recommendations. https://www.ipecollaborative.org/core-competencies.html.
- 31.Weaver SJ, Rosen MA, DiazGranados D, et al. : Does teamwork improve performance in the operating room? A multilevel evaluation. Jt Comm J Qual Patient Saf 36:133-1422010 [DOI] [PubMed] [Google Scholar]
- 32.McEwan D, Ruissen GR, Eys MA, et al. : The effectiveness of teamwork training on teamwork behaviors and team performance: A systematic review and meta-analysis of controlled interventions. PLoS One 12:e01696042017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller CJ, Kim B, Silverman A, et al. : A systematic review of team-building interventions in non-acute healthcare settings. BMC Health Serv Res 18:146.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mathieu J, Maynard MT, Rapp T, et al. : Team effectiveness 1997–2007: A review of recent advancements and a glimpse into the future. J Manage 34:410-4762008 [Google Scholar]
- 35.Salas E: Team science in cancer care: Questions, an observation, and a caution. J Oncol Pract 12:972-11472016 [DOI] [PubMed] [Google Scholar]