PURPOSE:
Patients with cancer often prefer to avoid time in the hospital; however, data are lacking on the prevalence and predictors of potentially avoidable readmissions (PARs) among those with advanced cancer.
METHODS:
We enrolled patients with advanced cancer from September 2, 2014, to November 21, 2014, who had an unplanned hospitalization and assessed their patient-reported symptom burden (Edmonton Symptom Assessment System) at the time of admission. For 1 year after enrollment, we reviewed patients’ health records to determine the primary reason for every hospital readmission and we classified readmissions as PARs using adapted Graham’s criteria. We examined predictors of PARs using nonlinear mixed-effects models with binomial distribution.
RESULTS:
We enrolled 200 (86.2%) of 232 patients who were approached. For these 200 patients, we reviewed 277 total hospital readmissions and identified 108 (39.0%) of these as PARs. The most common reasons for PARs were premature discharge from a prior hospitalization (30.6%) and failure of timely follow-up (28.7%). PAR hospitalizations were more likely than non-PAR hospitalizations to experience symptoms as the primary reason for admission (28.7% v 13.0%; P = .001). We found that married patients were less likely to experience PARs (odds ratio, 0.30; 95% CI, 0.15 to 0.57; P < .001) and that those with a higher physical symptom burden were more likely to experience PARs (odds ratio, 1.03; 95% CI, 1.01 to 1.05; P = .012).
CONCLUSION:
We observed that a substantial proportion of hospital readmissions are potentially avoidable and found that patients’ symptom burdens predict PARs. These findings underscore the need to assess and address the symptom burden of hospitalized patients with advanced cancer in this highly symptomatic population.
INTRODUCTION
Patients with advanced cancer often experience numerous symptoms and stressors that can affect their quality of life.1-3 In addition, patients with cancer frequently require hospitalizations to help with the management of troubling symptoms, but hospital stays may cause additional distress for this population.4 Patients with cancer often wish to maximize their time away from the hospital5-7; however, those with cancer often experience frequent hospitalizations and readmissions, some of which may be potentially avoidable.8-10 Potentially avoidable readmissions (PARs) are hospital readmissions that might have been avoided because of either a preventable condition or treatment that was possible as an outpatient.8 To date, research investigating PARs among patients with advanced cancer is lacking; therefore, a critical need exists to understand the prevalence and predictors of PARs in this population with high health care utilization.
Much of the existing data on potentially avoidable hospital admissions originate from the general medicine literature, which suggests remarkably high rates of potentially avoidable health care utilization. In this population, studies demonstrate that nearly 30% of hospital admissions are potentially avoidable.10-14 Currently, the data in oncology suggest that nearly one third of hospitalizations may be potentially avoidable15-19; however, researchers, to date, have not studied the prevalence and predictors of subsequent readmissions that may be potentially avoidable. In addition, the current literature in oncology investigating potentially avoidable health care utilization has been conducted using data that lack patient-reported outcomes. Inclusion of patient-reported outcomes could help to deepen our understanding of the relationship between patients’ symptoms and potentially avoidable health care utilization. Of importance, hospitalized patients often experience worse symptom burdens than those in the outpatient setting,20 and the association between hospitalized patients’ symptom burdens and PARs is currently unknown. Thus, additional research is needed to help understand the predictors and characteristics of PARs among hospitalized patients with cancer as well as to investigate associations with patient-reported symptom burden.
In the current work, we sought to conduct a comprehensive study focused on identifying rates and predictors of PARs among patients with advanced cancer. Specifically, we aimed to examine associations among PARs, patient characteristics, and self-reported symptom burden. We anticipate that these findings will inform the development of future interventions targeting PARs in patients with advanced cancer.
METHODS
We prospectively enrolled consecutive hospitalized patients with advanced cancer in a previously described longitudinal cohort study.21 For the current study, we investigated patients with unplanned hospital admissions at Massachusetts General Hospital from September 2, 2014, to November 21, 2014. We identified and recruited patients by screening the daily in-patient oncology census. We obtained written, informed consent from eligible patients on the first weekday after admission, which was within 2 to 5 days of hospitalization, and then asked participants to complete a symptom burden questionnaire. We received approval for this study from the Dana-Farber/Harvard Cancer Center institutional review board.
Participants
Eligible patients included those who were age 18 years or older and admitted to Massachusetts General Hospital with a known diagnosis of advanced cancer, defined as patients not undergoing treatment with curative intent. We determined curative intent by reviewing the chemotherapy order entry treatment intent designation and clinical documentation in the electronic health record. We excluded patients who were unable to read and respond to study questionnaires in English or with minimal assistance from an interpreter, as well as those with elective or planned hospital admissions, defined as hospitalizations for chemotherapy administration, including desensitization, and scheduled surgical procedures.
Study Measures
Sociodemographic and Clinical Factors.
For all participants, we obtained sociodemographic information from the electronic health record, including date of birth, sex, race, relationship status, education, and religion. We reviewed patients’ oncology clinic notes to ascertain Charlson comorbidity index, date of diagnosis with advanced cancer, and cancer type. We reviewed the electronic medical record to obtain information from a standardized questionnaire that was conducted by nurses within 1 day of admission to assess whether patients had impaired mobility.22,23
Patient-Reported Symptom Burden.
We used the self-administered Edmonton Symptom Assessment System Revised (ESAS-r) to assess patients’ symptom burden at the time of index hospital admission.21,24,25 The ESAS-r asks patients about symptoms, such as pain, fatigue, drowsiness, nausea, appetite, dyspnea, depression, anxiety, and well-being, over the prior 24 hours. We also included constipation as a result of the pervasiveness of this symptom among patients with advanced cancer.26 With the ESAS-r, patients report their symptom severity on a scale of 0 to 10 (0 indicating the absence of the symptom and 10 indicating the worst possible severity). Consistent with prior work, we categorized ESAS scores as follows: none (0), mild (1 to 3), moderate (4 to 6), and severe (7 to 10).27 We also created a composite ESAS physical symptom variable that incorporates pain, fatigue, drowsiness, nausea, appetite, dyspnea, and constipation. The ESAS physical symptom score is well validated and has been previously used in oncology research.21,25,28
Reasons for Hospital Readmissions.
We conducted a comprehensive chart review to obtain information on all hospital admissions for patients from the time of enrollment (index hospitalization) to 1 year after enrollment. We adapted a coding schema previously developed in patients with leukemia to determine reasons for hospital readmission.16 The reasons for hospital readmission in the schema for our study included symptoms, GI bleeding, hemoptysis, fever without a source, febrile neutropenia, confirmed infection, GI or biliary obstruction, dehydration/electrolyte abnormalities, planned hospitalization, hospitalization as a result of a noncancer medical condition, cancer progression, and end-of-life care.19 Two coders, both physicians, independently reviewed patient medical records and used this coding schema to identify the primary reason for hospital readmission. A consensus panel of two board-certified oncologists reviewed each of the admissions from the initial coders to clarify any discrepancies.
PARs.
To identify and characterize PARs, we used an adaptation of Graham’s criteria, which is consistent with prior work.14,19,29 PAR categories in our study included inadequate medical management, premature discharge from prior hospitalization, failure of timely outpatient follow-up, social problems leading to admission, patient nonadherence to medical care, inadequate rehabilitation, patient receiving hospice or supportive care alone, and potential for outpatient management of medical issue. We reviewed each hospital readmission using a two-stage review process, as previously used in studies that involved patients with leukemia and GI malignancies.15,19 The first stage involved two coders, both physicians, who independently reviewed the medical record for each readmission to determine and classify PARs via adapted Graham’s criteria. When coding PARs, we achieved 77.3% agreement (κ = 0.54; 95% CI, 0.44 to 0.65), which is a moderate level of agreement. In the second stage of review, a consensus panel that consisted of the first two coders and two board-certified oncologists reviewed any readmission considered to be potentially avoidable by at least one coder for a final consensus determination of PARs.
Statistical Analysis.
We used descriptive statistics to summarize patients’ sociodemographic and clinical characteristics, the primary reason for hospital readmission, and PAR classification. To account for patients who had multiple hospital readmissions in our sample, we used nonlinear mixed-effects models with binomial distribution to assess associations among patient characteristics, self-reported symptom burden, and PARs. In these models, we investigated age, sex, marital status, comorbidities, cancer type, months since advanced cancer diagnosis, impaired mobility, and ESAS physical symptoms as predictors of PARs. We performed statistical analyses using STATA software (version 14.2; STATA, College Station, TX; Computing Resource Center, Santa Monica, CA).
RESULTS
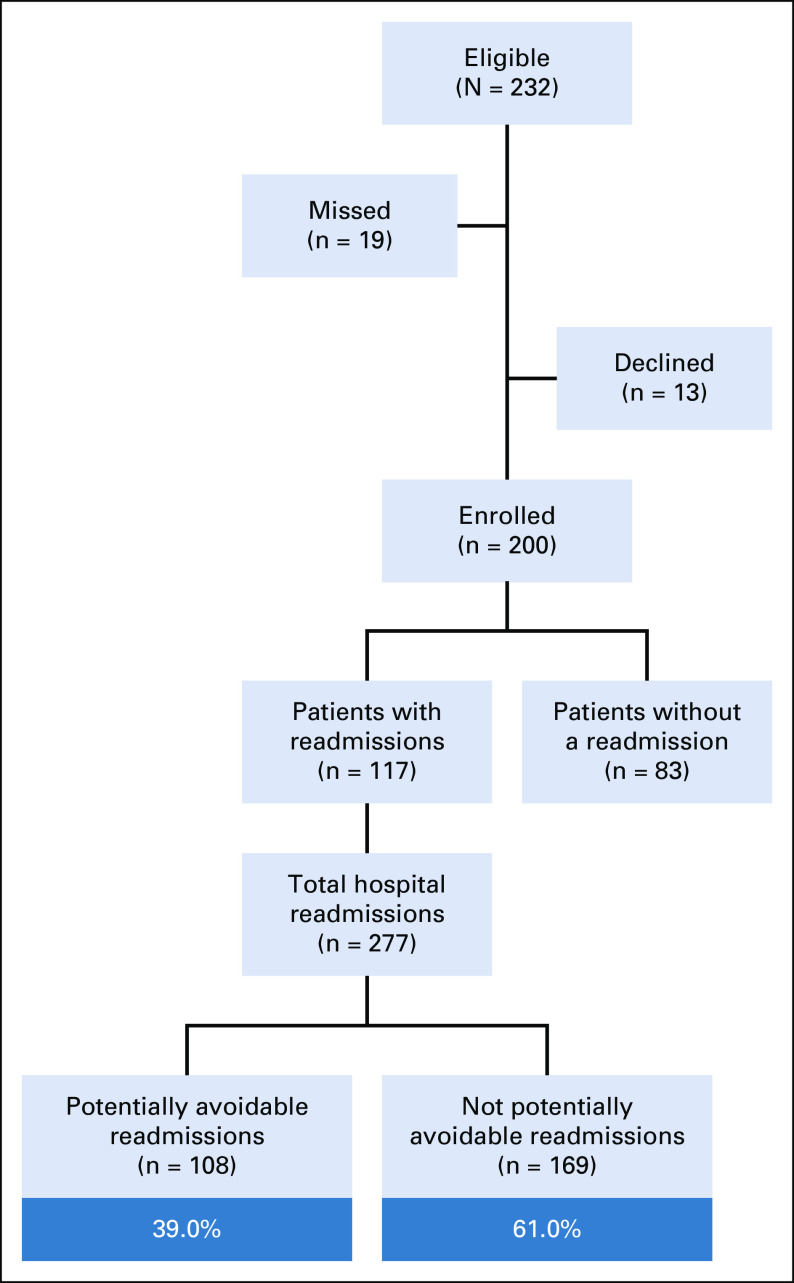
Among 232 eligible patients, we enrolled 200 (86.2% enrollment rate). For these 200 patients, 117 (58.5%) had at least one readmission in the year after their index hospitalization. For these 117 patients with at least one readmission, we reviewed 277 total hospital readmissions to investigate rates of PARs (Fig 1). Of the 117 patients with at least one readmission, patients (mean age, 63.80 years; standard deviation [SD], 13.04 years) were primarily white (94.0%), married (70.9%), and educated beyond high school (66.7%; Table 1). Patients had a mean time since diagnosis of advanced cancer of 18.04 months (SD, 24.11 months). Mean time from index hospitalization discharge to first readmission was 1.93 months (SD, 2.07 months). GI cancer was the most common cancer type (42.7%). We found that the most common reasons for patients’ hospital readmissions were infections (26.0%) and symptoms (19.1%; Table 2).
Fig 1.
Flow diagram.
TABLE 1.
Patient Characteristics (N = 117)
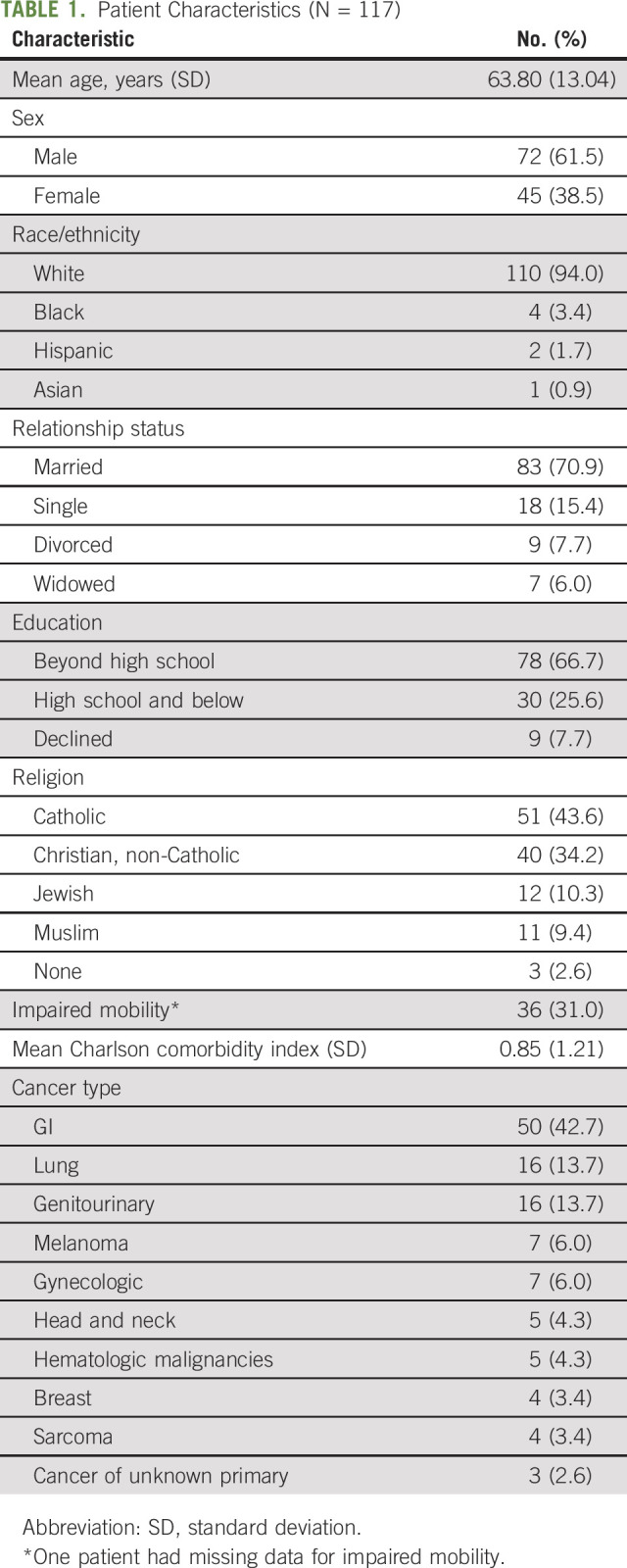
TABLE 2.
Reason for Hospital Readmission and Classification of PAR
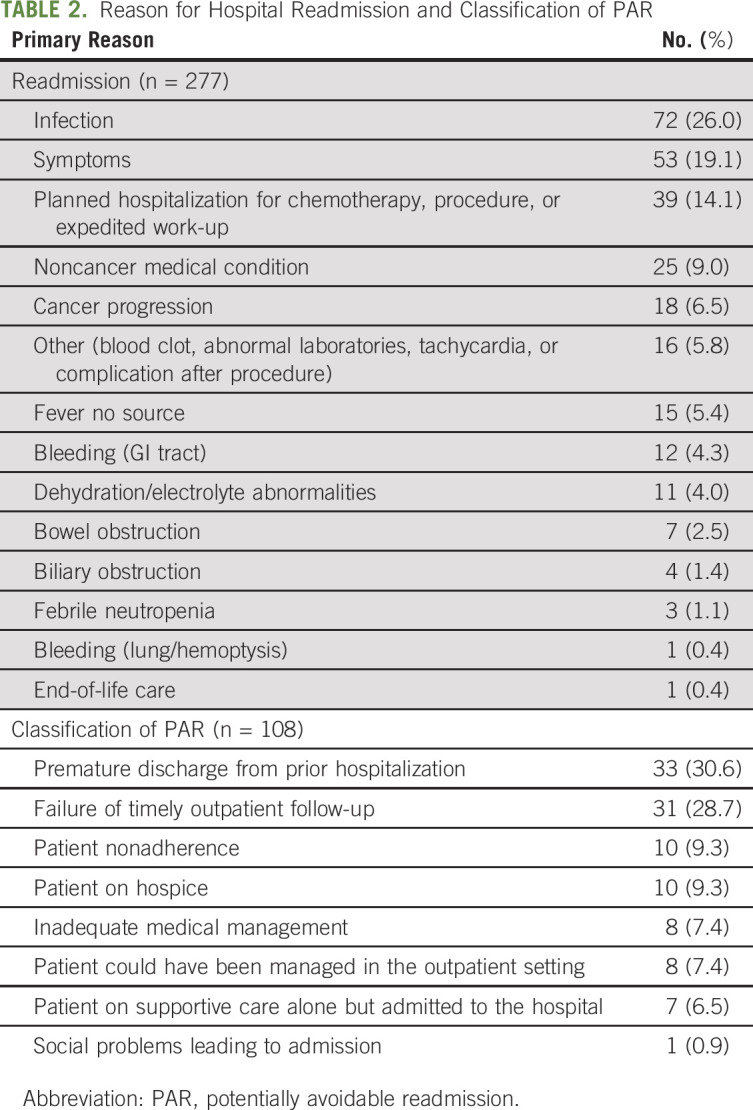
We identified 108 readmissions (39.0%) as potentially avoidable. The most common reasons for classifying a readmission as a PAR were premature discharge from a prior hospitalization (30.6%) and failure of timely outpatient follow-up (28.7%; Table 2). Of note, PAR hospitalizations were more likely to have symptoms as their primary reason for hospital readmission compared with non-PAR hospitalizations (28.7% v 13.0%; P = .001).
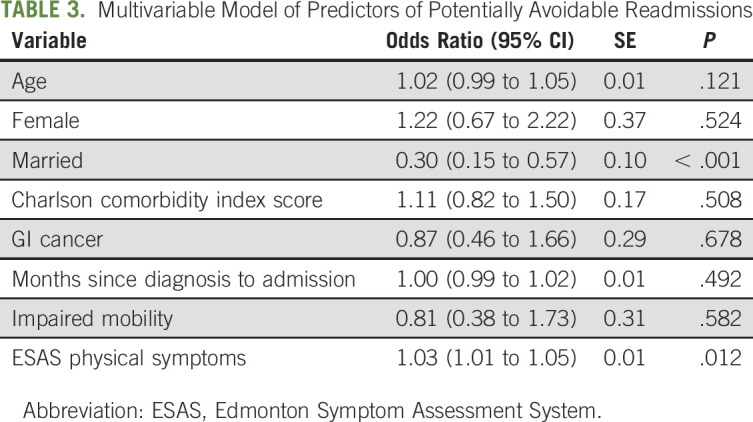
Using nonlinear mixed-effects models, we identified factors associated with PARs (Table 3). Specifically, we found that being married was associated with a lower likelihood of experiencing a PAR (odds ratio, 0.30; 95% CI, 0.15 to 0.57; P < .001). In addition, we found that a higher physical symptom burden was associated with a greater likelihood of having a PAR (odds ratio, 1.03; 95% CI, 1.01 to 1.05; P = .012).
TABLE 3.
Multivariable Model of Predictors of Potentially Avoidable Readmissions
DISCUSSION
Our analysis is a comprehensive study that identifies and characterizes PARs in patients with advanced cancer. Of note, we found a remarkably high rate of PARs, with more than one third of readmissions in our cohort classified as PARs. Premature hospital discharge and failure of timely outpatient follow-up were the most common reasons that a readmission was characterized as a PAR. We also investigated predictors of PARs, observing that marital status and physical symptom burden were significantly associated with PARs. Collectively, these findings highlight the need for targeted interventions to reduce PARs and help to elucidate the characteristics of patients who are at greatest risk for PARs and may benefit from such interventions.
Of importance, we identified the most common reasons for categorizing readmissions as PARs. Specifically, we found that premature discharge from a prior hospitalization and failure of timely outpatient follow-up after hospital discharge were the most common reasons for a readmission to be categorized as a PAR. This underscores the importance of hospital discharge as a key transition point for patients with cancer.23 Specifically, these findings suggest that efforts to prevent PARs should focus on the care transition that occurs as patients leave the hospital and resume care in the outpatient setting with their cancer team, which could be adapted from care transition efforts in the general medicine population, such as the development of discharge checklists or the use of health care professionals as patient aids in care transitions.30,31 In addition, patients with limited support may have more difficulty with the logistics of follow-up care and hospital discharge transition. This likely puts those patients with limited social support, a predictor of PARs in our study, at high risk for readmission around the time of discharge. Taken together, our findings support the need to focus clinical resources on increasing support for patients around the time of discharge as a potential strategy for reducing PARs within oncology care.
To our knowledge, this study is the first to demonstrate a relationship between symptom burden and the risk of experiencing a PAR among patients with cancer. Although previous research has demonstrated relationships between patient-reported symptom burden and health care utilization,21,32 investigators, to date, had not studied the association between patients’ symptom burden and PARs. In prior work, we found that hospitalized patients with advanced cancer experience a remarkably high symptom burden, which is associated with their hospital length of stay, risk for readmission, and discharge location.21,23 In the current study, we expand on our prior work to demonstrate that a higher physical symptom burden at the time of the index hospitalization predicted for greater risk of PAR. Clinicians may struggle to fully address all the physical and psychological symptoms of their patients,33-36 and our data suggest that this can place patients at risk for experiencing a subsequent PAR. Our findings underscore the need for additional research that focuses on identifying effective methods for monitoring and addressing the symptom burden of patients with advanced cancer postdischarge to reduce PARs. Recent data have demonstrated that patient-reported symptom monitoring interventions can improve quality of life, decrease health care utilization, and potentially enhance survival in patients with cancer.32,37 Thus, interventions that focus on patients’ symptom burden, a potentially modifiable risk factor, have the potential to affect these individuals’ health care utilization and diminish the prevalence of PARs among this population with high symptom burdens.
In addition, we found that patients who were married were less likely to experience a PAR. Marital status likely represents a proxy for social support. Of note, patients with limited support can struggle to manage their health care needs, especially when facing burdensome symptoms, functional decline, and the logistical demands that accompany a cancer diagnosis. Our findings suggest that patients without social support who have an unplanned hospital admission may benefit from interventions to provide additional support, such as patient navigation, more intensive social work involvement, or care transition programs after hospital discharge.38 By identifying patients who are at higher risk for experiencing PARs, our work has the potential to inform efforts that target the specific care needs of patients with cancer to align their care with their preferences and maximize their time away from the hospital.
Addressing PARs in oncology represents an important goal in the changing landscape of health care delivery. The complexity and cost of oncologic care has led to the development of such programs as the Oncology Care Model, which was created to generate incentives toward promoting high-value care.39 A reduction in PARs experienced by patients with cancer is a goal well suited to the concepts in the Oncology Care Model, as it can promote improved value by enhancing the quality of care while also lowering costs. Moreover, augmenting the efficiency of outpatient follow-up after discharge and addressing the symptom burden of oncology patients are both strategies that may affect PARs while achieving the broader goals of delivering high-value cancer care.
Our study has several limitations worth considering. First, we conducted this study at a single site with limited racial and socioeconomic diversity, and GI cancers representing the most common cancer type; thus, our findings may not be generalizable to other populations. Second, we did not have information about patients’ hospital admissions outside of our health system and our rates of hospital admissions and PARs may therefore underestimate the true rates. Third, we included all consecutive patients with a hospitalization during our study period, rather than only those with an initial hospitalization, and patients with multiple prior admissions may differ from those with an initial admission with respect to their symptoms and risk of readmission. In addition, we tracked all hospital readmissions from the time of index hospitalization to 1 year after the index admission. Patients’ treatment course and symptom burdens may have fluctuated throughout this time, which could affect their risk of PARs. Fourth, we assessed patients’ symptoms at a single time (within 2 to 5 days of hospitalization) to better understand the association between initial symptom burden and future PARs. However, by assessing symptoms only once during the hospitalization, we lack information about changes over time and differences between the inpatient and outpatient settings. In addition, other important symptoms, such as diarrhea and fever, were not captured in our study. Finally, the reason for admission and classification of PARs both have inherent subjectivity and were determined by medical record review, including the discharge summary, which may be reflected in the moderate agreement observed in our κ statistics. Moreover, we recognize that the reasons for admission can be complex and evolving throughout each readmission, which may not be easily captured in a single coding. We attempted to maximize objectivity with a structured approach, but this remains an inherent limitation.
In conclusion, we have demonstrated that a substantial proportion of hospital readmissions are potentially avoidable among patients with advanced cancer. We also identified salient factors associated with PARs within this patient population. Of note, we observed that being unmarried and having a higher physical symptom burden were significantly associated with greater odds of experiencing a PAR. Collectively, our findings underscore the importance of addressing patients’ social support needs and physical symptoms when attempting to decrease potentially avoidable health care utilization. In addition, we found that premature discharge and failure of timely outpatient follow-up were the most common reasons for categorizing readmissions as PARs, thus reflecting the need for efforts to improve care transitions in patients with cancer. By demonstrating the remarkably high prevalence of PARs among patients with advanced cancer and identifying predictors of these unwanted outcomes, we highlight the need for future work to develop and test intensive supportive care interventions in this highly symptomatic population.
Footnotes
Presented at the 2017 Annual Meeting of the American Society of Clinical Oncology, Chicago, IL, June 2-6, 2017.
Funded by Grant No. K24-CA181253 from the National Cancer Institute (J.S.T.), Massachusetts General Hospital Cancer Center Funds (J.S.T.), and the Scullen Center for Cancer Data Analysis (E.P.H.).
AUTHOR CONTRIBUTIONS
Conception and design: P. Connor Johnson, Yian Xiao, Risa L. Wong, Sara D’Arpino, Daniel E. Lage, Ephraim P. Hochberg, Jennifer S. Temel, Areej El-Jawahri, Ryan D. Nipp
Collection and assembly of data: P. Connor Johnson, Yian Xiao, Risa L. Wong, Sara D’Arpino, Samantha M.C. Moran, Daniel E. Lage, Brandon Temel, Margaret Ruddy, Ephraim P. Hochberg, Areej El-Jawahri, Ryan D. Nipp
Data analysis and interpretation: P. Connor Johnson, Yian Xiao, Risa L. Wong, Sara D’Arpino, Lara N. Traeger, Joseph A. Greer, Ephraim P. Hochberg, Jennifer S. Temel, Areej El-Jawahri, Ryan D. Nipp
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Potentially Avoidable Hospital Readmissions in Patients With Advanced Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc/journal-policies.html.
Joseph A. Greer
Consulting or Advisory Role: Vector Oncology
Research Funding: Pfizer (Inst)
Patents, Royalties, Other Intellectual Property: Royalties from Springer Publishing Company for edited book, “The Massachusetts General Hospital Handbook of Behavioral Medicine”
Ephraim P. Hochberg
Stock and Other Ownership Interests: Flatiron Health, Leuko, Intervention Insights
Consulting or Advisory Role: Intervention Insights
Jennifer S. Temel
Research Funding: Pfizer (Inst)
No other potential conflicts of interest were reported.
REFERENCES
- 1.Tuggey EM, Lewin WH: A multidisciplinary approach in providing transitional care for patients with advanced cancer. Ann Palliat Med 3:139-1432014 [DOI] [PubMed] [Google Scholar]
- 2.Walsh D, Donnelly S, Rybicki L: The symptoms of advanced cancer: Relationship to age, gender, and performance status in 1,000 patients. Support Care Cancer 8:175-1792000 [DOI] [PubMed] [Google Scholar]
- 3.Higginson IJ, Costantini M: Dying with cancer, living well with advanced cancer. Eur J Cancer 44:1414-14242008 [DOI] [PubMed] [Google Scholar]
- 4.Earle CC, Park ER, Lai B, et al. : Identifying potential indicators of the quality of end-of-life cancer care from administrative data. J Clin Oncol 21:1133-11382003 [DOI] [PubMed] [Google Scholar]
- 5.El-Jawahri AR, Abel GA, Steensma DP, et al. : Health care utilization and end-of-life care for older patients with acute myeloid leukemia. Cancer 121:2840-28482015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pritchard RS, Fisher ES, Teno JM, et al. : Influence of patient preferences and local health system characteristics on the place of death. SUPPORT investigators. Study to understand prognoses and preferences for risks and outcomes of treatment. J Am Geriatr Soc 46:1242-12501998 [DOI] [PubMed] [Google Scholar]
- 7.Higginson IJ, Sen-Gupta GJ: Place of care in advanced cancer: A qualitative systematic literature review of patient preferences. J Palliat Med 3:287-3002000 [DOI] [PubMed] [Google Scholar]
- 8.Bekelman JE, Halpern SD, Blankart CR, et al. : Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA 315:272-2832016 [DOI] [PubMed] [Google Scholar]
- 9.Earle CC, Neville BA, Landrum MB, et al. : Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol 22:315-3212004 [DOI] [PubMed] [Google Scholar]
- 10.Graham KL, Auerbach AD, Schnipper JL, et al. : Preventability of early versus late hospital readmissions in a national cohort of general medicine patients. Ann Intern Med 168:766-7742018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mcandrew RM, Grabowski DC, Dangi A, et al. : Prevalence and patterns of potentially avoidable hospitalizations in the US long-term care setting. Int J Qual Health Care 28:104-1092016 [DOI] [PubMed] [Google Scholar]
- 12.Segal M, Rollins E, Hodges K, et al. : Medicare-Medicaid eligible beneficiaries and potentially avoidable hospitalizations. Medicare Medicaid Res Rev 4:E1-E102014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thygesen LC, Christiansen T, Garcia-Armesto S, et al. : Potentially avoidable hospitalizations in five European countries in 2009 and time trends from 2002 to 2009 based on administrative data. Eur J Public Health 25:35-432015. (suppl 1) [DOI] [PubMed] [Google Scholar]
- 14.van Walraven C, Bennett C, Jennings A, et al. : Proportion of hospital readmissions deemed avoidable: A systematic review. CMAJ 183:E391-E4022011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brooks GA, Abrams TA, Meyerhardt JA, et al. : Identification of potentially avoidable hospitalizations in patients with GI cancer. J Clin Oncol 32:496-5032014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brooks GA, Jacobson JO, Schrag D: Clinician perspectives on potentially avoidable hospitalizations in patients with cancer. JAMA Oncol 1:109-1102015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donzé JD, Lipsitz S, Schnipper JL: Risk factors and patterns of potentially avoidable readmission in patients with cancer. J Oncol Pract 13:e68-e762017 [DOI] [PubMed] [Google Scholar]
- 18.Hatam N, Fanusi T, Dehghani M, et al. : Economic burden of avoidable hospitalizations among patients with cancer at Namazi Hospital in Shiraz, 2013. Asian Pac J Cancer Prev 18:177-1822017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.El-Jawahri A, Keenan T, Abel GA, et al. : Potentially avoidable hospital admissions in older patients with acute myeloid leukaemia in the USA: A retrospective analysis. Lancet Haematol 3:e276-e2832016 [DOI] [PubMed] [Google Scholar]
- 20.Portenoy RK, Thaler HT, Kornblith AB, et al. : Symptom prevalence, characteristics and distress in a cancer population. Qual Life Res 3:183-1891994 [DOI] [PubMed] [Google Scholar]
- 21.Nipp RD, El-Jawahri A, Moran SM, et al. : The relationship between physical and psychological symptoms and health care utilization in hospitalized patients with advanced cancer. Cancer 123:4720-47272017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pavon JM, Sloane R, Morey MC, et al. : Inpatient mobility measures as useful predictors of discharge destination in hospitalized older adults. J Am Geriatr Soc 65:224-2262017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lage DE, Nipp RD, D’Arpino SM, et al. : Predictors of posthospital transitions of care in patients with advanced cancer. J Clin Oncol 36:76-822018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Watanabe SM, Nekolaichuk C, Beaumont C, et al. : A multicenter study comparing two numerical versions of the Edmonton Symptom Assessment System in palliative care patients. J Pain Symptom Manage 41:456-4682011 [DOI] [PubMed] [Google Scholar]
- 25.Bruera E, Kuehn N, Miller MJ, et al. : The Edmonton Symptom Assessment System (ESAS): A simple method for the assessment of palliative care patients. J Palliat Care 7:6-91991 [PubMed] [Google Scholar]
- 26.Rhondali W, Nguyen L, Palmer L, et al. : Self-reported constipation in patients with advanced cancer: A preliminary report. J Pain Symptom Manage 45:23-322013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Selby D, Cascella A, Gardiner K, et al. : A single set of numerical cutpoints to define moderate and severe symptoms for the Edmonton Symptom Assessment System. J Pain Symptom Manage 39:241-2492010 [DOI] [PubMed] [Google Scholar]
- 28.Hui D, Shamieh O, Paiva CE, et al. : Minimal clinically important difference in the physical, emotional, and total symptom distress scores of the Edmonton Symptom Assessment System. J Pain Symptom Manage 51:262-2692016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Graham H, Livesley B: Can readmissions to a geriatric medical unit be prevented? Lancet 1:404-4061983 [DOI] [PubMed] [Google Scholar]
- 30.Halasyamani L, Kripalani S, Coleman E, et al. : Transition of care for hospitalized elderly patients: Development of a discharge checklist for hospitalists. J Hosp Med 1:354-3602006 [DOI] [PubMed] [Google Scholar]
- 31.Coleman EA, Parry C, Chalmers S, et al. : The care transitions intervention: Results of a randomized controlled trial. Arch Intern Med 166:1822-18282006 [DOI] [PubMed] [Google Scholar]
- 32.Basch E, Deal AM, Dueck AC, et al. : Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA 318:197-1982017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davis MP, Dreicer R, Walsh D, et al. : Appetite and cancer-associated anorexia: A review. J Clin Oncol 22:1510-15172004 [DOI] [PubMed] [Google Scholar]
- 34.Miovic M, Block S: Psychiatric disorders in advanced cancer. Cancer 110:1665-16762007 [DOI] [PubMed] [Google Scholar]
- 35.Teunissen SC, Wesker W, Kruitwagen C, et al. : Symptom prevalence in patients with incurable cancer: A systematic review. J Pain Symptom Manage 34:94-1042007 [DOI] [PubMed] [Google Scholar]
- 36.Nekolaichuk CL, Maguire TO, Suarez-Almazor M, et al. : Assessing the reliability of patient, nurse, and family caregiver symptom ratings in hospitalized advanced cancer patients. J Clin Oncol 17:3621-36301999 [DOI] [PubMed] [Google Scholar]
- 37.Denis F, Lethrosne C, Pourel N, et al. : Randomized trial comparing a Web-mediated follow-up with routine surveillance in lung cancer patients. J Natl Cancer Inst 109:djx029.2017 [DOI] [PubMed] [Google Scholar]
- 38.Naylor MD, Brooten DA, Campbell RL, et al. : Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. J Am Geriatr Soc 52:675-6842004 [DOI] [PubMed] [Google Scholar]
- 39.Kline R, Adelson K, Kirshner JJ, et al. : The Oncology Care Model: Perspectives from the Centers for Medicare & Medicaid Services and participating oncology practices in academia and the community. Am Soc Clin Oncol Educ Book 37:460-4662017 [DOI] [PubMed] [Google Scholar]