Abstract
Background
The coronavirus disease (COVID-19) pandemic may have negatively affected bystander interventions, emergency medical service (EMS) personnel activities, and patient outcomes after out-of-hospital cardiac arrest (OHCA). This study assessed bystander interventions, EMS activities, and patient outcomes during the COVID-19 pandemic era and compared them with those during the non-COVID-19 pandemic era in Osaka City, Japan, where public-access automated external defibrillators (AEDs) are well established.
Methods
We conducted this population-based cohort study that included all cases with non-traumatic OHCA treated by EMS personnel and excluded cases with no resuscitation attempt, traumatic cases, cases occurring in healthcare facilities, or cases witnessed by EMS personnel. Data were compared between the COVID-19 pandemic period (February 1, 2020 to July 31, 2020) and the non-COVID-19 pandemic period (February 1, 2019 to July 31, 2019).
Results
During the study periods, 1687 patients were eligible for analyses (COVID-19: n = 825; non-COVID-19: n = 862). Patients with OHCA during the COVID-19 pandemic period were significantly less likely to receive bystander cardiopulmonary resuscitation (CPR) (COVID-19: 33.0%; non-COVID-19: 41.3%; p < 0.001) and public-access AED pad application (COVID-19: 2.9%; non-COVID-19: 6.1%; p = 0.002) compared with patients during the non-COVID-19 pandemic period. There were no significant differences in 1-month survival with favorable neurological outcomes between the two periods (COVID-19: 4.6%; non-COVID-19: 6.1%; p = 0.196).
Conclusion
The COVID-19 pandemic period did not affect patient outcomes after OHCA but changed bystander behaviors in Osaka City, Japan.
Keywords: COVID-19, Out-of-hospital cardiac arrest, Bystander CPR, AED
Introduction
The number of people with coronavirus disease (COVID-19) is continuously increasing, reaching 93,527 (as of October 20, 2020) in Japan.1 The COVID-19 pandemic could have inimical effects on prehospital emergency care worldwide, such as decreasing bystander cardiopulmonary resuscitation (CPR), increasing delays in emergency medical service (EMS) response time, or increasing out-of-hospital cardiac arrest (OHCA) incidences and mortality rates.2, 3, 4
Under all conditions, bystander CPR and public-access defibrillation initiation play critical roles in saving lives after OHCA.5 It is hypothesized that chest compressions and CPR generate aerosols that increase the risk of COVID-19, which may negatively affect bystander interventions or EMS personnel activities. Japan, despite having relatively low infection and case fatality rates during the first surge of COVID-19, is no exception.1 Herein, we assessed bystander interventions, EMS activities, and patient outcomes during the COVID-19 pandemic era and compared them with those during the non-COVID-19 era in Osaka City, Japan, where public-access automated external defibrillators (AEDs) are well established.
Methods
Study design
We conducted this population-based cohort study that included all OHCA cases treated by EMS personnel according to the Utstein-style guidelines in Osaka City, Japan, which has a population of approximately 2.7 million. The methodology of this registry has been previously described.6 Based on the Infectious Diseases Control Law, COVID-19 was designated as an infectious disease in Japan since February 1, 2020. This study compared OHCA data during the COVID-19 pandemic (February 1, 2020 to July 31, 2020) with those during the same period in 2019 (non-COVID-19 pandemic; February 1, 2019 to July 31, 2019).
Study setting and subjects
During the study period, 1825 cases of COVID-19 were documented in Osaka City.7 All patients with non-traumatic OHCA treated by EMS personnel were included, whereas cases with no resuscitation attempt, traumatic cases, cases that occurred in health care facilities (e.g., nursing home and long-term care facilities), or cases witnessed by EMS personnel were excluded. Since EMS personnel were not allowed to terminate resuscitation in a prehospital setting, all OHCA cases were transported to a medical institution and registered in our registry.8 This EMS protocol did not change during the pandemic study period; however, the EMS protocol encouraged paramedics to use supraglottic airway management instead of endotracheal intubation since April 24, 2020.
Statistical analyses
The chi-squared test (for categorical variables) and the Mann-Whitney U test (for continuous variables) were used to compare patient characteristics and outcomes between the two periods. All tests were two tailed, and a p-value <0.05 was considered statistically significant. All statistical analyses were conducted using SPSS ver.24.0J (IBM Corp. Armonk, NY).
Ethics
This study was approved by the Ethics Committee of Kyoto University (R0416). Personal identifiers were removed in the Osaka Fire Department. The individual informed consent requirement was waived because of the Personal Information Protection Law and the National Research Ethics Guidelines of Japan.
Results
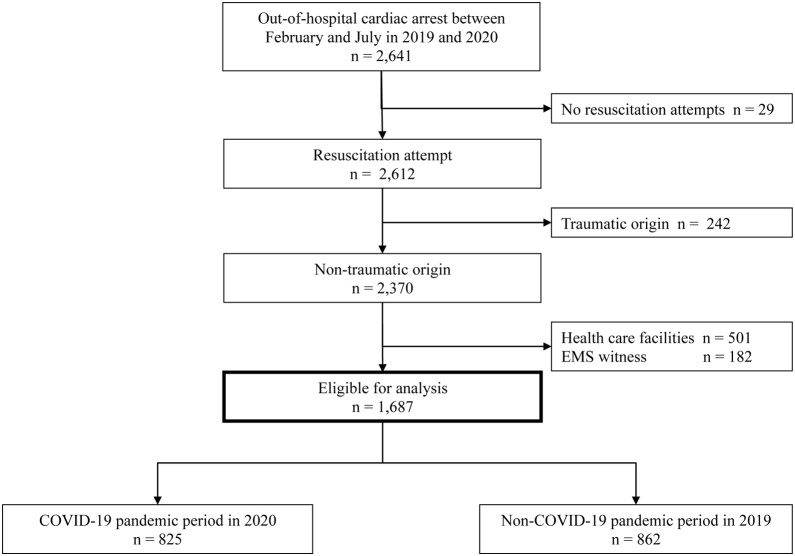
During the study periods, there were 2641 OHCA cases, among which 954 were excluded (no resuscitation attempts [n = 29], traumatic origin [n = 242], occurring in health care facilities [n = 501], and cases witnessed by EMS personnel [n = 182]). In total, 1687 patients were eligible for analyses (COVID-19: n = 825; non-COVID-19: n = 862) (Fig. 1).
Fig. 1.
OHCA patients in Osaka City during the COVID-19 pandemic period (February 1, 2020 to July 31, 2020) and the non-COVID-19 period (February 1, 2019 to July 31, 2019). OHCA, out-of-hospital cardiac arrest; EMS, emergency medical service.
Table 1 shows patient characteristics and outcomes in OHCA and EMS activities during the study periods. Patient characteristics were similar, but 5.7% less cases occurred in public during the COVID-19 period than during the non-COVID-19 period (COVID-19: 20.4%; non-COVID-19: 26.1%; p = 0.006). OHCA patients were significantly less likely to receive bystander CPR (COVID-19: 33.0%; non-COVID-19: 41.3%; p < 0.001) and public-access AED pad application (COVID-19: 2.9%; non-COVID-19: 6.1%; p = 0.002) during the COVID-19 period compared with during the non-COVID-19 period.
Table 1.
Characteristics and outcomes of OHCA patients between the non-COVID-19 pandemic period and the COVID-19 pandemic period.
| COVID-19 pandemic period (Feb-July, 2020) |
Non-COVID-19 pandemic period (Feb-July, 2019) |
p-value | |||
|---|---|---|---|---|---|
| (n = 825) | (n = 862) | ||||
| Age, years, median (IQR) | 77.0 | (66.0−85.0) | 75.0 | (63.0−83.0) | 0.002 |
| Men, n (%) | 529 | (64.1) | 551 | (63.9) | 0.589 |
| Good ADL before arrest, n (%) | 592 | (71.8) | 614 | (71.2) | 0.778 |
| Witnessed by bystander, n (%) | 282 | (34.2) | 310 | (36.0) | 0.445 |
| Location of arrest, public place, n (%) | 168 | (20.4) | 225 | (26.1) | 0.006 |
| Origin of arrest, cardiac origin, n (%) | 742 | (89.9) | 746 | (86.5) | 0.034 |
| VF as the first documented rhythm, n (%) | 85 | (10.3) | 69 | (8.0) | 0.108 |
| Bystander CPR, n (%) | 272 | (33.0) | 356 | (41.3) | <0.001 |
| Public-access AED pad application, n (%) | 24 | (2.9) | 53 | (6.1) | 0.002 |
| Shocks by public-access AEDs, n (%) | 10 | (1.2) | 16 | (1.9) | 0.326 |
| Dispatcher instruction, n (%) | 511 | (61.9) | 507 | (58.8) | 0.196 |
| Adrenaline administration, (%) | 222 | (26.9) | 254 | (29.5) | 0.256 |
| Advanced airway management, n (%) | |||||
| Endotracheal intubation | 96 | (11.6) | 166 | (19.3) | <0.001 |
| Supraglottic airway | 422 | (51.2) | 345 | (40.0) | |
| No advanced airway management | 307 | (37.2) | 351 | (40.7) | |
| Response time (call to contact with patients), min, median (IQR) | 6.0 | (5.0−8.0) | 7.0 | (6.0−9.0) | <0.001 |
| On-scene time (arrival at the scene to dispatch at the hospital), min, median (IQR) | 15.0 | (11.0−18.0) | 15.0 | (11.0−19.0) | 0.713 |
| Hospital arrival time (call to hospital arrival), min, median (IQR) | 27.0 | (22.0−32.0) | 28.0 | (23.0−32.0) | 0.006 |
| Prehospital ROSC, n (%) | 75 | (9.1) | 108 | (12.5) | 0.028 |
| One-month survival, n (%) | 68 | (8.2) | 80 | (9.3) | 0.491 |
| Neurologically favorable outcome, n (%) | 38 | (4.6) | 53 | (6.1) | 0.196 |
OHCA indicaed out-of-hospital cardiac arres; ADL, activities of daily living; CPR, cardiopulmonary resuscitation; AED, automated external defibrillator; VF, ventricular fibrillation; EMS, emergency medical service; ROSC, return of spontaneous circulation; IQR, interquartile range.
The distributions of the advanced airway management types were statistically different between periods (p < 0.001). The response time and hospital arrival time shortened; however, the scene times between the two periods did not differ (p = 0.713). There were no significant differences in 1-month survival after OHCA (COVID-19: 8.2%; non-COVID-19: 9.3%; p = 0.491) and 1-month survival with favorable neurological outcomes (COVID-19: 4.6%; non-COVID-19: 6.1%; p = 0.196) between the periods.
Discussion
This study assessed bystander interventions, EMS activities, and patient outcomes during the COVID-19 pandemic era in the metropolitan area of Osaka City, Japan, where the EMS system and public-access AEDs are well established. Changes in bystander behaviors, such as bystander CPR and public-access AED pad application, were demonstrated, while patient outcomes remained unchanged.
In contrast to Lombardy, Italy, and Paris, France, where a drastic decrease in OHCA survival rate has been reported,2, 3 patient outcomes were maintained during the pandemic study period, similar to findings in the Province of Padua, Northeast Italy, and Bologna, Italy.9, 10 Consistent with previous studies,11, 12 fewer patients received endotracheal intubation in Osaka City because of changing EMS protocols. Scene times did not differ between periods; however, the response time and hospital arrival time were shorter during the COVID-19 period. These results were in contrast to previously reported data that the response time was longer during the COVID-19 pandemic period.11, 12 One possible explanation is traffic reduction owing to the stay home policy. Elmer et al. showed there were no differences in the provision of laypersons, AED use, and prehospital return of spontaneous circulation in areas with a low COVID-19 prevalence.13 Regional differences in the spread of the COVID-19 might also explain the differential patterns of bystander CPR and patient outcomes during the pandemic worldwide. Lim et al. reported that resuscitation practices varied greatly with respect to countries or areas during the COVID-19 pandemic.12 A better understanding of the COVID-19 prevalence in areas might be useful for public health interventions to save more lives from OHCA.
Importantly, bystander CPR and AED pad application significantly decreased during the COVID-19 pandemic. Possible explanations included a decline in the proportion of OHCA events that occurred in public locations and OHCA events witnessed by bystanders because people stayed at home, avoiding unnecessary outings. Additionally, direct physical contact with patients required in AED pad application and rescue breathing could be a barrier for bystanders. Sayre et al. estimated that the risk of death from COVID-19 for the bystander while performing CPR was very low.14 Placing a cloth or mask over the patient’s mouth and providing chest compression-only resuscitation allows resuscitation to be started.15 Considering the proven effectiveness of early defibrillation with public-access AEDs and chest compressions by bystanders in saving lives in OHCA cases and the low risk of transmission of COVID-19 to bystanders performing CPR, we need to encourage bystanders to perform chest compressions and use an AED while asking them to keep their personal safety as much as possible.
This study had some limitations. First, our data represented a single city in Japan (Osaka City); thus, our findings might not be generalizable to other countries. Second, the sample size might be too small to observe differences in survival outcomes. Further study is needed to evaluate outcome trends and factors associated with bystander interventions and EMS activities using the national registry called the All-Japan Utstein Registry of the Fire and Disaster Management Agency. Third, because we did not perform a polymerase chain reaction test for all OHCA cases in Osaka City, the number of OHCA patients with COVID-19 included in this study was unknown.
Conclusions
This population-based study showed that the COVID-19 pandemic did not affect outcomes after OHCA but appeared to change bystander behaviors, such as CPR and public-access AED pad application.
Funding sources
This study was supported by scientific research grants from the Ministry of Education, Culture, Sports, Science and Technology of Japan (15H05006 and 19K09393). The funding organization has not contributed to the study design, collection, management, analysis, interpretation of data, writing of the report, or the decision to submit the report for publication.
Conflict of interest
All authors declare that they have no competing interests.
CRediT authorship contribution statement
Chika Nishiyama: Conceptualization, Methodology, Formal analysis, Writing - original draft, Project administration. Kosuke Kiyohara: Methodology, Writing - review & editing. Taku Iwami: Conceptualization, Methodology, Writing - review & editing, Funding acquisition, Supervision. Sumito Hayashida: Resources, Supervision. Takeyuki Kiguchi: Writing - review & editing. Tasuku Matsuyama: Writing - review & editing. Yusuke Katayama: Writing - review & editing. Takeshi Shimazu: Writing - review & editing. Tetsuhisa Kitamura: Methodology, Writing - review & editing, Funding acquisition.
Acknowledgments
We are deeply grateful to all the EMS personnel and concerned physicians in Osaka City for their cooperation in establishing and maintaining ambulance records, including the Utstein database. We thank our colleagues from Osaka University Center of Medical Data Science and Advanced Clinical Epidemiology Investigator’s Research Project for providing insight and expertise for our research.
References
- 1.Novel coronavirus (COVID-19) Situation report, Current situation in Japan. Ministry of Health, Labour and Welfare. (Accessed 25 October 2020, at https://www.mhlw.go.jp/stf/covid-19/kokunainohasseijoukyou_00006.html#1-1).
- 2.Baldi E., Sechi G.M., Mare C. COVID-19 kills at home: The close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41:3045–3054. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marijon E., Karam N., Jost D. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: A population-based, observational study. Lancet Public Health. 2020;5:e437–443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai P.H., Lancet E.A., Weiden M.D. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020;5:1154–1163. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perkins G.D., Morley P.T., Nolan J.P. International Liaison Committee on Resuscitation: COVID-19 consensus on science, treatment recommendations and task force insights. Resuscitation. 2020;151:145–147. doi: 10.1016/j.resuscitation.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nishiyama C., Iwami T., Kawamura T. Prodromal symptoms of out-of-hospital cardiac arrests: A report from a large-scale population-based cohort study. Resuscitation. 2013;84:558–563. doi: 10.1016/j.resuscitation.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 7.Osaka infectious disease measures information. About new coronavirus infectious disease, the outbreak situation of patients with new coronavirus infectious disease in Osaka. Osaka Prefecture Government (Accessed 23 October 2020, at http://www.pref.osaka.lg.jp.e.agb.hp.transer.com/iryo/osakakansensho/corona.html).
- 8.Kajino K., Kitamura T., Iwami T. Current termination of resuscitation (TOR) guidelines predict neurologically favorable outcome in Japan. Resuscitation. 2013;84:54–59. doi: 10.1016/j.resuscitation.2012.05.027. [DOI] [PubMed] [Google Scholar]
- 9.Paoli A., Brischigliaro L., Scquizzato T., Favaretto A., Spagna A. Out-of-hospital cardiac arrest during the COVID-19 pandemic in the Province of Padua, Northeast Italy. Resuscitation. 2020;154:47–49. doi: 10.1016/j.resuscitation.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Semeraro F., Gamberini L., Tartaglione M. Out-of-hospital cardiac arrest during the COVID-19 era in Bologna: System response to preserve performances. Resuscitation. 2020;157:1–2. doi: 10.1016/j.resuscitation.2020.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scquizzato T., Landoni G., Paoli A. Effects of COVID-19 pandemic on out-of-hospital cardiac arrests: A systematic review. Resuscitation. 2020;157:241–247. doi: 10.1016/j.resuscitation.2020.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lim Z.J., Reddy M.P., Afroz A., Billah B., Shekar K., Subramaniam A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: A systematic review and meta-analysis. Resuscitation. 2020;157:248–258. doi: 10.1016/j.resuscitation.2020.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elmer J., Okubo M., Guyette F.X., Martin-Gill C. Indirect effects of COVID-19 on OHCA in a low prevalence region. Resuscitation. 2020;156:282–283. doi: 10.1016/j.resuscitation.2020.08.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sayre M.R., Barnard L.M., Counts C.R. Prevalence of COVID-19 in out-of-hospital cardiac arrest: Implications for bystander CPR. Circulation. 2020;142:507–509. doi: 10.1161/CIRCULATIONAHA.120.048951. [DOI] [PubMed] [Google Scholar]
- 15.Edelson D.P., Sasson C., Chan P.S. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: From the Emergency Cardiovascular Care Committee and Get with the guidelines-resuscitation adult and Pediatric Task Forces of the American Heart Association. Circulation. 2020;141:e933–943. doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]