Abstract
Most individuals in the United States have no history of a mental health condition yet are at risk for psychological distress due to the COVID-19 pandemic. The objective of this study was to assess the frequency and risk and protective factors of psychological distress, during the beginning of the COVID-19 pandemic, in this group. Data comes from the Pew Research Center’s American Trends Panel (ATP), a probability-based online survey panel representative of the US adult population. The analytic sample consisted of 9,687 individuals with no prior history of a mental health condition who completed the survey between March 19–24, 2020. Explanatory variables included sociodemographic factors and items related to behavior, perceptions, and experiences surrounding the pandemic. The outcome was psychological distress, measured by five items on symptoms of anxiety, depression, loneliness, sleep difficulties, and hyperarousal. A multivariable linear regression model was used to identify risk and protective factors for psychological distress. Fifteen percent of the sample experienced 2 psychological distress symptoms for at least 3 days over the past week; 13% had three or more symptoms. Risk factors for higher distress included searching online or using social media to post about coronavirus, reporting that the outbreak caused major changes to personal life, and perception that the virus was a threat to the US economy, the individual’s personal health or finances. This has important implications for mental health service delivery.
Keywords: COVID-19, pandemic, psychological distress, epidemiology
The COVID-19 pandemic has dramatically changed the day-to-day life of all Americans. A robust body of work has demonstrated that smaller-scale public health disasters may negatively impact mental health (Bonanno et al., 2007; Douglas et al., 2009; Havenaar et al., 1997; Henriksen et al., 2010; Huremović, 2019; Kunii et al., 2016). Previous outbreaks indicate acute mental health decrements due to the effects of quarantining, lack of clear information, fears of infection, boredom, and frustration. Longer-term mental health impacts were concentrated among those who were impacted financially, felt stigmatized due to having been ill and/or quarantined, and those who reported having a history of mental health concerns (Brooks et al., 2020; Cao et al., 2020). However, the global scope of the COVID-19 pandemic is unprecedented. Social distancing measures, needed to prevent the spread of infections, are severely limiting interpersonal interactions (Unacast, 2020). Widespread job losses and furloughs of uncertain duration have contributed to rising anxiety over financial well-being (Shiller, 2020). Finally, the force of morbidity and mortality associated with COVID-19 is both substantial and wide-spread; as of July 11, 2020, there were over 3 million cases and 130,000 deaths in the United States (US) alone (Johns Hopkins University, 2020).
The path of devastation laid by COVID-19 raises serious concerns about mental health in the US population, both in the midst of the pandemic and beyond. Recent data from China indicate that the impact of the COVID-19 pandemic on psychological distress has been significant (Qiu et al., 2020; Wang et al., 2020). In the United States, data gathered from the nationally representative Understanding America Study (UAS), collected during the very beginning of the outbreak in early March 2020, suggest a linear relationship between time (as cases increased) and psychological distress among individuals living in states with the most severe outbreaks (Holingue et al., In Press). Data gathered from the Kaiser Family Foundation provides additional evidence that the COVID-19 pandemic is impacting the public’s mental health (Kirzinger et al., 2020).
It is expected that the COVID-19 pandemic will exacerbate latent or existing mental health symptoms among individuals with a history of a mental condition (Druss, 2020). However, the influence of the pandemic on individuals with no prior history of a mental condition is still unknown. It is likely this group is experiencing psychological distress, given the unique and severe impacts of the pandemic on daily life. Understanding the impact on this group is critical for several reasons. First, this group represents the majority of adults in the US (Substance Abuse and Mental Health Services Administration, 2019). The mental health system is likely ill-prepared to accommodate such a large increase in mental health disorders (Auerbach & Miller, 2020). Second, those with no history of psychological distress are likely wholly unfamiliar with the mental health system and may need specific public mental health messaging to help them navigate this system. Third, this population may experience confusion and self-stigmatization since these symptoms or degree of distress may be unprecedented (Bathje & Pryor, 2011). Fourth and finally, there are many activities (World Health Organization, 2020), such as meditation (Behan, 2020), exercise (Stathopoulou et al., 2006), and establishing regular sleep patterns (Altena et al., 2020) which can be used to prevent further exacerbation of symptoms. These activities may be more amenable and perhaps appropriate for those with emerging, but not significantly impairing, psychological distress.
The primary goal of this study was to describe the frequency of psychological distress during the COVID-19 pandemic within a nationally-representative sample of adults in the US with no reported history of a pre-existing mental health condition. In addition, multivariable analyses were conducted to identify independent risk factors, such as sociodemographic variables and behavior, perceptions, and experiences surrounding the coronavirus outbreak, for psychological distress in this group.
Methods
Study Sample
Data for this study come from the Pew Research Center’s American Trends Panel (ATP), an online survey panel recruited through random sampling of residential addresses throughout the US, in accordance with the best practice guideline set forth by the American Association for Public Opinion Research (AAPOR) (Task Force on Address-based Sampling, 2016). Panelists who do not have internet access are provided a tablet and wireless internet connection in order to complete self-administered web surveys. The current study drew from the panel wave conducted from March 19–24, 2020. Of the 15,433 individuals sampled, 11,537 completed the survey (75% response rate). Further details on panel construction can be found here: https://www.pewresearch.org/methods/u-s-survey-research/american-trends-panel/.
The sample was restricted to individuals who reported no prior history of a mental health condition (n=9,687) (reported have never “been told by a doctor or other healthcare provider that [they] have a mental health condition”). The proportion of individuals with a history of a mental health condition (16%) is consistent with prior population-based studies (Substance Abuse and Mental Health Services Administration, 2019). Survey weights, used in all statistical analyses in this study, allow for inferences to the US adult population (Pew Research Center, 2020).
Mental Health Measures
The primary outcome was psychological distress, measured by a score derived from five questionnaire items in the survey. These items were adapted from the Center for Epidemiologic Studies Depression (CES-D) Scale (Radloff, 1977), the Generalized Anxiety Disorder-7 (GAD-7) (Spitzer et al., 2006), and the Impact of Event Scale – Revised (IES-R) (Weiss, 2007). Participants were asked how often in the past 7 days they: 1) felt nervous, anxious, or on edge; 2) felt depressed; 3) felt lonely; 4) had trouble sleeping; and 5) had physical reactions, such as sweating, trouble breathing, nausea, or a pounding heart when thinking about their experience with the coronavirus outbreak (hereafter referred to as hyperarousal). Response options for these five items were “rarely or none of the time (less than 1 day)”; “some or a little of the time (1–2 days)”; “occasionally or a moderate amount of time (3–4 days)”; or “most or all of the time (5–7 days)”. These four response options were given a weight of 1, 2, 3, and 4, respectively, to reflect increasing frequency of symptoms in the past week. A summary score for each person was derived by taking the sum of response weights across each of the five items (possible range 5–20). This scoring procedure yielded a scale with adequate internal consistency (Cronbach’s α = 0.73).
Demographic Variables
Demographic variables included age categories (18–29, 30–49, 50–64, 65+), sex, education level (high school graduate or less, some college, associate degree, college graduate, or post graduate), race/ethnicity (non-Hispanic white, non-Hispanic Black, Hispanic, other), marital status (married, never married, widowed, divorced or separated, living with partner), and income ranges (<40k, 40–49k, 50–74k, 75–99k, 100k+). Participants were asked how often they attended religious services (seldom or never, a few times a year, once or twice a month, once a week or more).
COVID-19 Context Variables
Panelists were also asked questions about their behavior, perceptions, and experiences surrounding the coronavirus outbreak. Participants reported whether or not they searched online or used social media to share or post information about the coronavirus (yes/no). They were asked how closely they had been following news of the outbreak (4-point response scale from not at all closely to very closely). Next, participants were asked whether they felt that the coronavirus was a threat to “the health of the US population as a whole,” to their “personal health,” “the US economy,” and to their “personal financial situation” (response options: not a threat, minor threat, major threat), and whether their personal life changed due to the coronavirus (response options: same, minor change, major change). Lastly, they reported whether or not anyone in their household had “been laid off or lost a job” or “had to take a cut in pay due to reduced hours or demand for [their] work,” because of the coronavirus pandemic (yes/no).
Statistical Analysis
Missingness ranged between 0–4% per variable. Because complete case analysis would have reduced the sample by 12% overall, multiple imputation with chained equations was used to impute missing data. All analytic variables were used for imputation and ten imputations, with ten iterations per imputation, were generated. In addition to examining descriptive statistics, a survey-weighted multivariable linear regression model was used to assess associations between explanatory variables and psychological distress summary score, among individuals with no reported history of mental condition. All statistical analyses were performed in RStudio (version 1.1.383) (RStudio Team, 2016) using the “pewmethods” (version 1.0) (Lau et al., 2020), “survey” (version 3.37) (Lumley, 2004, 2019), and “mice” (version 3.8.0) (Buuren & Groothuis-Oudshoorn, 2011) packages.
Ethical Considerations
As with all studies by Pew Research Center, the ethical implications of the research were evaluated and approved by the Vice President of Research at Pew Research Center and Senior Vice President for government and nonprofit research at the data collection firm, Ipsos. Both organizations have standing approval for general population surveys that (1) are limited to administering questions and do not feature more invasive data collections (e.g. biospecimens) and (2) explicitly inform participants that they may decline to answer any questions they wish. Pew Research Center also has extensive protocols in place to prevent accidental or malicious disclosure of personally identifying information about their panelists. The authors of this paper are not affiliated with the Pew Research Center, though they did consult on the design of the psychological distress items that were collected through this survey. Local IRB approval was not sought given these were secondary analyses of de-identified, publicly available data.
Results
Frequency of psychological distress symptoms
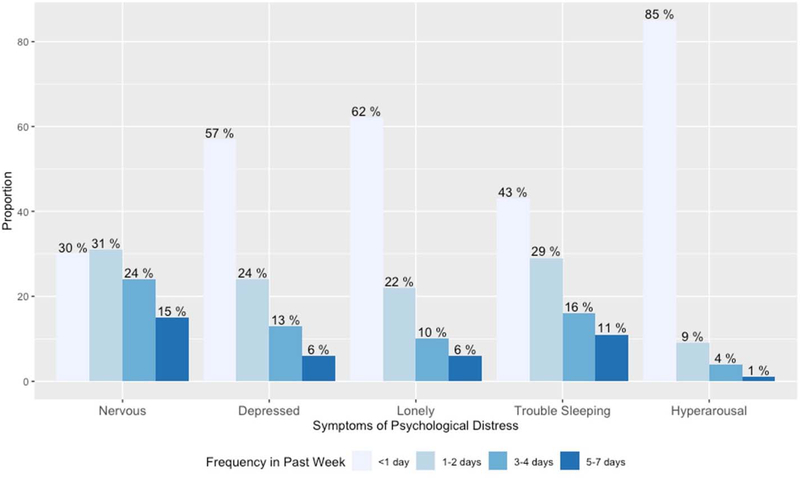
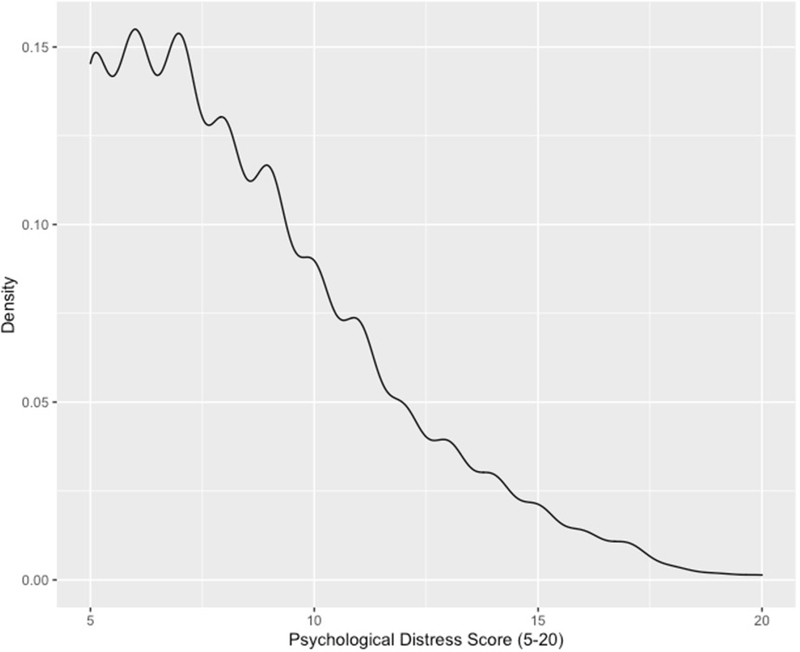
The weighted population reflects the distribution of characteristics of individuals in the United States with no reported history of a mental condition (Table 1). The most common symptom of psychological distress experienced for at least 3 days in the past week was feeling nervous, anxious, or on edge (mean 39% [95% CI: 0.37-.40]). The next most common symptom was trouble sleeping (27% [95% CI: 0.26–0.29]), followed by feeling depressed (19% [95% CI: 0.17–0.20]), feeling lonely (15% [95% CI: 0.14–0.17]), and having hyperarousal symptoms (5% [95% CI: 0.04–0.07]) (Figure 1). The mean score for psychological distress (range 5–20) was 8.69 (SD=5.3) (Figure 2). Over the past week, over seventy percent (72%) of individuals had 0–1 symptoms, 15% had two symptoms, and 13% had three or more symptoms for at least 3 days.
Table 1.
Demographic characteristics in a nationally representative sample of individuals in the United States with no history of mental disorder (N=9687).
| Number of Distress Symptoms | |||
|---|---|---|---|
| 0–1 (n=7008) | 2 (n=1402) | 3–5 (n=1227) | |
| Age (%) | |||
| 18–29 | 16 | 23 | 25 |
| 30–49 | 31 | 33 | 34 |
| 50–64 | 27 | 25 | 25 |
| 65+ | 26 | 19 | 16 |
| Sex (%) | |||
| Male | 54 | 44 | 39 |
| Female | 46 | 56 | 61 |
| Education (%) | |||
| High school graduate or less | 36 | 34 | 42 |
| Some college | 21 | 23 | 22 |
| Associate degree | 9 | 10 | 9 |
| College graduate | 19 | 19 | 16 |
| Post graduate | 14 | 15 | 11 |
| Race (%) | |||
| Non-Hispanic White | 65 | 62 | 57 |
| Non-Hispanic Black | 11 | 13 | 14 |
| Hispanic | 15 | 17 | 21 |
| Other | 9 | 9 | 8 |
| Marital Status (%) | |||
| Married | 53 | 46 | 37 |
| Never married | 21 | 26 | 31 |
| Widowed | 7 | 5 | 4 |
| Divorced/Separated | 12 | 13 | 16 |
| Living with partner | 8 | 10 | 13 |
| Income (%) | |||
| <40k | 34 | 37 | 50 |
| 40–49k | 11 | 8 | 10 |
| 50–74k | 17 | 17 | 14 |
| 75–99k | 14 | 14 | 8 |
| 100k+ | 24 | 24 | 18 |
| Attends religious services (%) | |||
| Seldom or Never | 50 | 55 | 60 |
| A few times a year | 15 | 18 | 17 |
| Once or twice a month | 7 | 9 | 8 |
| Once a week+ | 28 | 18 | 15 |
Demographic characteristics are stratified by number of symptoms occurring 3+ days in past week (0–1, 2, 3–5). Chi-squared differences for each variable by number of symptoms occurring 3+ days in past week are all statistically significant at p<0.001.
Figure 1.
Frequency of psychological distress symptoms in past week.
Bar plot shows frequency of five symptoms of psychological distress in past week, in a nationally representative sample of individuals in the United States with no history of a mental health condition (N=9687). Surveys were taken between March 19–24, 2020.
Figure 2.
Distribution of psychological distress score.
Plot shows distribution of psychological distress score in past week, in a nationally representative sample of individuals in the United States with no history of a mental health condition (N=9687). Surveys were taken between March 19–24, 2020.
Risk factors for Psychological Distress
Results of the survey-weighted multivariable linear regression model showed several independent risk factors significantly associated with higher psychological distress scores among individuals with no reported prior history of a mental condition. These included being female, never having been married, being divorced or separated, searching online for coronavirus information, using social media to post about the coronavirus, reporting that the coronavirus caused major changes to personal life, or that it was a minor or major threat to their own personal health. Additionally, having someone in the household with a pay cut or reduced hours was a risk factor for psychological distress, as were perceptions that the coronavirus is a minor or major threat to the US economy, and a major threat to personal finances
Protective factors against Psychological Distress
Conversely, old age (50–64 and 65+) was protective against levels of psychological distress, as was being Hispanic, or having an “other” race/ethnicity, having an income of 50k or higher, and attending religious services on average once a week or more prior to this pandemic (Figure 3 and Table 3). The distributions of explanatory variables, stratified by number of psychological distress symptoms occurring for at least 3 days in the past week, are shown in Tables 1 and 2.
Figure 3.
Multivariable linear regression model estimating association between explanatory variables and psychological distress score.
Plots show results of single multivariable linear regression model estimating association between explanatory variables and psychological distress score, in a nationally representative sample of individuals in the United States with no history of mental disorder (N=9687). Vertical line represents null of Beta=0. Bars denote 95% Confidence Intervals. Both panels together represent one single model. Surveys were taken between March 19–24, 2020.
Table 3.
Multivariable linear regression model estimating association between explanatory variables and psychological distress score.
| Beta (95% CI) | ||
|---|---|---|
| Age | ||
| 30–40 | −0.29 | (−0.64, 0.06) |
| 50–64 | −0.59 | (−0.96, −0.23)*** |
| 65+ | −1.06 | (−1.44, −0.68) *** |
| Sex | ||
| Female | 0.75 | (0.55, 0.95)*** |
| Education | ||
| Some college | −0.15 | (−0.44, 0.13) |
| Associate degree | −0.22 | (−0.54, 0.11) |
| College graduate | −0.26 | (−0.54, 0.02) |
| Post-graduate | −0.13 | (−0.43, 0.16) |
| Race | ||
| Black, non-hispanic | −0.31 | (−0.72, 0.10) |
| Hispanic | −0.74 | (−1.06, −0.42)*** |
| Other | −0.49 | (−0.84, −0.15) *** |
| Marital Status | ||
| Never married | 0.78 | (0.47, 1.09)*** |
| Widowed | 0.11 | (−0.27, 0.50) |
| Divorced/Separated | 0.73 | (0.40, 1.06) *** |
| Living with partner | 0.38 | (−0.02, 0.78) |
| Income | ||
| 40–49k | −0.34 | (−0.73, 0.05) |
| 50–74k | −0.38 | (−0.68, −0.09)** |
| 75–99k | −0.62 | (−0.91, −0.34)*** |
| 100k | −0.37 | (−0.66, −0.08) ** |
| Attends religious services | ||
| A few times a year | −0.09 | (−0.35, 0.18) |
| Once or twice per month | −0.11 | (−0.51, 0.30) |
| Once a week or more | −0.79 | (−1.02, −0.55)*** |
| Search online for coronavirus info | ||
| Yes | 0.35 | (0.09, 0.61)* |
| Used social media to post about coronavirus | ||
| Yes | 0.27 | (0.06, 0.49)* |
| How closely following news on COVID-19 | ||
| Not too closely | −0.30 | (−2.06, 1.46) |
| Fairly closely | −0.66 | (−2.35, 1.04) |
| Very closely | −0.50 | (−2.19, 1.18) |
| Personal life change as result of coronavirus | ||
| Major change | 0.99 | (0.61, 1.37)*** |
| Minor change | 0.11 | (−0.24, 0.46) |
| Threat of coronavirus for US population health | ||
| Major threat | −0.40 | (−1.21, 0.4) |
| Minor threat | −0.66 | (−1.45, 0.14) |
| Threat of coronavirus for personal health | ||
| Major threat | 1.37 | (1.00, 1.73)*** |
| Minor threat | 0.69 | (0.37, 1.00) *** |
| Laid off/lost job due to COVID (household) | ||
| Yes | 0.04 | (−0.25, 0.34) |
| Pay cut, reduced hours due to COVID (household) | ||
| Yes | 0.32 | (0.06, 0.58)* |
| Threat of coronavirus to US economy | ||
| Major threat | 1.08 | (0.18, 1.97)* |
| Minor threat | 0.96 | (0.03, 1.90) * |
| Threat of coronavirus for personal finances | ||
| Major threat | 0.51 | (0.18, 0.84)*** |
| Minor threat | 0.04 | (−0.27, 0.35) |
Multivariable linear regression models estimating association between explanatory variables and psychological distress score, in a nationally representative sample of individuals in the United States with no history of mental disorder (N=9687).
Table 2.
COVID-19 context variables in a nationally representative sample of individuals in the United States with no history of mental disorder (N=9687).
| Number of Distress Symptoms | |||
|---|---|---|---|
| 0–1 (n=7008) | 2 (n=1402) | 3–5 (n=1277) | |
| Search online for info (%) | |||
| No | 31 | 22 | 22 |
| Yes | 69 | 78 | 78 |
| Used social media to post (%) | |||
| No | 65 | 59 | 55 |
| Yes | 35 | 41 | 45 |
| How closely following news (%) | |||
| Not at all closely | 1 | 0 | 2 |
| Not too closely | 6 | 7 | 7 |
| Fairly closely | 37 | 30 | 28 |
| Very closely | 56 | 63 | 62 |
| Personal life change coronavirus (%) | |||
| Same | 13 | 8 | 8 |
| Major change | 40 | 54 | 60 |
| Minor change | 48 | 38 | 31 |
| Threat for US population health (%) | |||
| Not a threat | 3 | 1 | 3 |
| Major threat | 62 | 75 | 78 |
| Minor threat | 35 | 25 | 19 |
| Threat for personal health (%) | |||
| Not a threat | 13 | 7 | 6 |
| Major threat | 32 | 41 | 53 |
| Minor threat | 55 | 52 | 42 |
| Laid off/lost job (household) (%) | |||
| No | 83 | 79 | 72 |
| Yes | 17 | 21 | 28 |
| Pay cut/reduced hours (household) (%) | |||
| No | 77 | 68 | 63 |
| Yes | 23 | 32 | 37 |
| Threat to US economy (%) | |||
| Not a threat | 1 | 1 | 1 |
| Major threat | 87 | 93 | 92 |
| Minor threat | 12 | 6 | 8 |
| Threat for personal finances (%) | |||
| Not a threat | 13 | 9 | 7 |
| Major threat | 44 | 58 | 66 |
| Minor threat | 44 | 33 | 27 |
COVID-19 context variables are stratified by number of symptoms occurring 3+ days in past week (0–1, 2, 3–5). Chi-squared differences for each variable by number of symptoms occurring 3+ days in past week are all statistically significant at p<0.001.
Discussion
In this nationally-representative sample of US adults with no reported prior history of a mental condition, more than 1 in 4 are experiencing psychological distress in the early phases of the COVID-19 pandemic. Specifically, 15% experienced some psychological distress (2 symptoms for at least 3 days in the past week) and 13% experienced significant psychological distress (3–5 symptoms for at least 3 days) during the beginning of the COVID-19 pandemic (March 19–24, 2020). These findings raise concerns about a generalized burden of psychological distress, and potential risks for emergent psychological disorders, in a population with no reported history of a mental health condition.
Symptoms of anxiety and depression were the most prevalent symptoms of psychological distress. We found that 39% of individuals reported symptoms of anxiety and 19% reported depressive symptoms for at least 3 days in the past week. Recent benchmarks for the U.S. population can help contextualize our findings at the symptom level. According to January–June 2019 estimates from the National Health Interview Survey, 8.2% of the U.S. adult population experienced symptoms of anxiety disorder and 6.6% experienced symptoms of depressive disorder. The above suggests elevated levels of psychological distress among the U.S. population at the beginning of the COVID-19 pandemic, compared to the months before the pandemic began.
Searching online and using social media to post information about the coronavirus were both independent risk factors associated with higher psychological distress. Although the media represents an important avenue for disseminating information during public health disasters and causality cannot be inferred from our analysis, this finding is consistent with prior studies demonstrating a positive association between increased exposure to disaster-related media content and poor mental health (Lubens & Holman, 2017), including within the COVID-19 pandemic (Gao et al., 2020; Riehm et al., 2020). Other researchers have provided guidance on responsible media communication during the COVID-19 pandemic (Garfin et al., 2020), such as avoiding the use of sensationalized headlines and refraining from publishing disturbing images. At the individual level, it is recommended that social media users avoid passive activities (Verduyn et al., 2015), such as repetitive “scrolling” and observation of others; instead, social media can be used to obtain accurate information from trusted sources, engage in purposeful connections with others, and obtain social support throughout periods of social distancing.
Individuals who reported that the virus had caused a major change to their life showed significantly higher psychological distress. Importantly, this variable was associated with distress even after adjusting for sociodemographic factors and lost employment or wages secondary to COVID-19, suggesting it may be capturing changes and stressors independent of financial ones. Although information on the specific changes people underwent is not available, these could plausibly include homeschooling children and increased parenting responsibilities (Brown et al., 2020; Canady, 2020; Kantamneni, 2020), working from home, moving, caretaking for sick relatives (Kantamneni, 2020), increased social isolation or loneliness(Usher et al., 2020), and major changes in work-related habits, among others. These changes are likely to be concomitant with reduced time for self-care and disrupted work-life balance, which can contribute to increased distress (Ensel & Lin, 1991; Haines et al., 2015; Kessler, 1979; Pfefferbaum & North, 2020; Sprang & Silman, 2013; Tausig & Fenwick, 2001; Vinokur & Selzer, 1975).
We also found that those who reported that the virus was a threat to the US economy or to their own personal finances had significantly higher distress, consistent with an initial report by Pew Research Center (Keeter, 2020). As millions of Americans continue to experience financial and health insurance loss due to the pandemic (Woolhandler & Himmelstein, 2020), there may be a continued deterioration in public mental health. Policies and interventions, such as access to healthcare (including mental health care) irrespective of employment status, may significantly alleviate this burden of psychological distress.
Individuals who perceived that the virus was a threat to their personal health also had significantly elevated psychological distress, even after adjusting for age. This might represent individuals with a physical health condition that makes them more susceptible to COVID-19. Alternatively, individuals who perceive the virus is a greater threat to their personal health may be in occupations that do not permit them to practice social distancing (e.g., grocers) or that expose them to higher risk of contracting the virus (e.g., healthcare workers). Research from China shows that healthcare workers have experienced significant distress due to the pandemic (Chen et al., 2020; Dai et al., 2020; Huang & rong Liu, 2020; Qi et al., 2020; Zhu et al., 2020), and this is expected to be occurring in the US as well (Greenberg et al., 2020; World Health Organization, 2020). Lastly, higher perception of threat could simply be a proxy for higher symptoms of anxiety or worries about the virus.
Beyond COVID-19 specific factors, sociodemographic variables were also associated with higher distress. Being female, never married, divorced/separated, or white non-Hispanic race were all risk factors, while older age and higher income were protective. These findings are consistent with decades of psychiatric epidemiology studies (Breslau et al., 2005; Kessler, Berglund, et al., 2005; Kessler, Chiu, et al., 2005; Manderscheid & Sonnenschein, 1998; Regier et al., 1988, 1993). While examining correlates of distress among those with a previous history of a mental health was out-of-scope for this study, our findings were consistent with previous psychiatric epidemiologic research among this population (see citations above).
It is important to recognize that the group under study--those with no reported prior mental health condition--may not be well equipped to handle incident mental health symptoms, especially in the context of a pandemic. Typical buffers against psychological distress such as in-person social supports, attending religious services, outdoor time, and gym attendance may be harder to access. Further, treatment-naïve individuals may not know how to navigate the mental health services system, and financial distress related to the pandemic may act as yet another barrier to accessing treatment. A mental health care system already struggling to meet the treatment need prior to this pandemic (Kohn et al., 2004) may now need to accommodate these individuals. Thus, measures that improve accessibility such as increased availability of telehealth, insurance coverage for phone and video psychotherapy, co-pay waivers, and license reciprocity to enable telehealth across state lines should be continued. It also suggests bolstering access to mental health care through primary care (Ross et al., 2019), when appropriate. Use of psychological care needs to not just be made more accessible, but also less stigmatized. Public health campaigns that normalize distress in reaction to highly stressful events, promote self-care resources and strategies, and disseminate simple, useful information on how to access mental health services will be critical over the course of and following this pandemic. Together these measures could increase access to those newly experiencing mental health concerns, who are experiencing relapses or increased symptomatology, and to those who live in areas with few psychological healthcare providers (e.g., rural areas) and ensure continued access and support long after the acute needs have subsided and longer-term impacts are felt.
This study is not without limitations. First, while items to assess psychological distress were derived from established, well-validated measures, including the CES-D (Radloff, 1977), GAD-7 (Spitzer et al., 2006), and IES-R (Weiss, 2007), their response options had to be adjusted to the last week to reflect the recent onset and highly dynamic course of the pandemic, which could have altered the psychometric properties and may limit comparability with other samples. Since the wording of the questions themselves did not change substantially, it is less likely that the face, construct, or content validity of the scale was negatively affected, but more likely than the reliability may be compromised. The Cronbach’s α of 0.73 suggests this scale has adequate but not excellent internal reliability. Second, all data were self-reported by respondents and may be susceptible to misclassification errors or biases. In addition, participants who do not belong to the white, Black, or Hispanic racial/ethnic groups were combined together into an “other” group in this publicly available dataset. Therefore, the associations between other racial groups, such as Asian American individuals, and degree of psychological distress could not be assessed. Lastly, while a strength of this study is that the data come from a large, nationally-representative sample of US adults, the descriptive and analytic inferences made from this analysis are generalizable to the adult US population under the assumption that non-response is unrelated to any factors that are not included in the construction of the survey weights (sex, age, race and ethnicity, educational attainment, and geographic region). This survey also remains a web-based survey of thousands of individuals, which limits the depth of information that can be obtained, and may influence the composition of the sample.
Nevertheless, this study provides a unique opportunity to analyze the risk and protective factors that were collected during this time, allowing us to identify at-risk groups and suggest interventions for reducing the burden of this pandemic on the public’s mental health. In sum, this study reports evidence of substantial levels of psychological distress among US adults with no prior diagnosis of a mental condition during the rise of the COVID-19 pandemic. Given the scope and expected duration of this pandemic, there are numerous opportunities to address public mental health through campaigns that de-stigmatize mental health, primary care screenings, expansion of and continued funding for telehealth, and promoting self-care through nutrition, exercise, and contact with friends and families, while observing recommended measures of social distancing. It is essential that prevention efforts, interventions, and policies be put in place to mitigate the potential fallout.
Acknowledgements
We are grateful to Scott Keeter and the Pew Research Center for making this data available. Work on the current manuscript was in part supported by the National Institute of Child Health and Human Development (U54 HD079123). Dr. Veldhuis’ participation in this research was made possible through an NIH/NIAAA Ruth Kirschstein Postdoctoral Research Fellowship (F32AA025816). Ms. Riehm was supported by the NIMH Mental Health Services and Systems Training Program (5T32MH109436-03) and by a Doctoral Foreign Study Award from the Canadian Institutes of Health Research.
References
- Altena E, Baglioni C, Espie CA, Ellis J, Gavriloff D, Holzinger B, Schlarb A, Frase L, Jernelöv S, & Riemann D (2020). Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. Journal of Sleep Research, e13052. [DOI] [PubMed] [Google Scholar]
- Auerbach J, & Miller BF (2020). COVID-19 Exposes the Cracks in Our Already Fragile Mental Health System. American Public Health Association. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bathje G, & Pryor J (2011). The relationships of public and self-stigma to seeking mental health services. Journal of Mental Health Counseling, 33(2), 161–176. [Google Scholar]
- Behan C (2020). The benefits of Meditation and Mindfulness practices during times of crisis such as Covid-19. Irish Journal of Psychological Medicine, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno GA, Galea S, Bucciarelli A, & Vlahov D (2007). What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology, 75(5), 671. [DOI] [PubMed] [Google Scholar]
- Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, & Kessler RC (2005). Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychological Medicine, 35(3), 317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SM, Doom J, Watamura SE, Lechuga-Pena S, & Koppels T (2020). Stress and Parenting during the Global COVID-19 Pandemic. [DOI] [PMC free article] [PubMed]
- Buuren S. van, & Groothuis-Oudshoorn K (2011). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3), 1–67. https://www.jstatsoft.org/v45/i03/ [Google Scholar]
- Canady VA (2020). APA stress report amid COVID-19 points to parental challenges. Mental Health Weekly, 30(22), 3–4. [Google Scholar]
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, & Zheng J (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research, 112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, He L, Sheng C, Cai Y, & Li X (2020). Mental health care for medical staff in China during the COVID-19 outbreak. The Lancet Psychiatry, 7(4), e15–e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai Y, Hu G, Xiong H, Qiu H, & Yuan X (2020). Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. MedRxiv. [Google Scholar]
- Douglas PK, Douglas DB, Harrigan DC, & Douglas KM (2009). Preparing for pandemic influenza and its aftermath: mental health issues considered. International Journal of Emergency Mental Health, 11(3), 137. [PubMed] [Google Scholar]
- Druss BG (2020). Addressing the COVID-19 Pandemic in Populations With Serious Mental Illness. JAMA Psychiatry. [DOI] [PubMed] [Google Scholar]
- Ensel WM, & Lin N (1991). The life stress paradigm and psychological distress. Journal of Health and Social Behavior, 321–341. [PubMed] [Google Scholar]
- Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, Wang Y, Fu H, & Dai J (2020). Mental health problems and social media exposure during COVID-19 outbreak. Plos One, 15(4), e0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfin DR, Silver RC, & Holman EA (2020). The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg N, Docherty M, Gnanapragasam S, & Wessely S (2020). Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ, 368. [DOI] [PubMed] [Google Scholar]
- Haines KJ, Denehy L, Skinner EH, Warrillow S, & Berney S (2015). Psychosocial outcomes in informal caregivers of the critically ill: a systematic review. Critical Care Medicine, 43(5), 1112–1120. [DOI] [PubMed] [Google Scholar]
- Havenaar JM, Rumyantzeva GM, van den Brink W, Poelijoe NW, Van den Bout J, van Engeland H, & Koeter MWJ (1997). Long-term mental health effects of the Chernobyl disaster: an epidemiologic survey in two former Soviet regions. American Journal of Psychiatry, 154(11), 1605–1607. [DOI] [PubMed] [Google Scholar]
- Henriksen CA, Bolton JM, & Sareen J (2010). The psychological impact of terrorist attacks: examining a dose–response relationship between exposure to 9/11 and Axis I mental disorders. Depression and Anxiety, 27(11), 993–1000. [DOI] [PubMed] [Google Scholar]
- Holingue C, Kalb LG, Bennett D, Kapteyn A, Veldhuis C, Johnson R, Fallin MD, Kreuter F, Stuart E, & Thrul J (n.d.). Mental Distress in the United Sates at the Beginning of COVID-19. American Journal of Public Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang L, & rong Liu H (2020). Emotional responses and coping strategies of nurses and nursing college students during COVID-19 outbreak. MedRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huremović D (2019). Psychiatry of Pandemics: A Mental Health Response to Infection Outbreak. Springer. [Google Scholar]
- Johns Hopkins University. (2020). Coronavirus COVID-19 Global Cases. https://coronavirus.jhu.edu/map-faq.html
- Kantamneni N (2020). The impact of the COVID-19 pandemic on marginalized populations in the United States: A research agenda. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keeter S (2020, March 30). People financially affected by COVID-19 outbreak are experiencing more psychological distress than others. Pew Research Center; https://www.pewresearch.org/fact-tank/2020/03/30/people-financially-affected-by-covid-19-outbreak-are-experiencing-more-psychological-distress-than-others/ [Google Scholar]
- Kessler RC (1979). Stress, social status, and psychological distress. Journal of Health and Social Behavior, 259–272. [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirzinger A, Kearney A, Hamel L, & Brodie M (2020). KFF Health Tracking Poll - Early April 2020: The Impact of Coronavirus on Life in America. Kaiser Family Foundation Health Reform. [Google Scholar]
- Kohn R, Saxena S, Levav I, & Saraceno B (2004). The treatment gap in mental health care. Bulletin of the World Health Organization, 82, 858–866. [PMC free article] [PubMed] [Google Scholar]
- Kunii Y, Suzuki Y, Shiga T, Yabe H, Yasumura S, Maeda M, Niwa S, Otsuru A, Mashiko H, & Abe M (2016). Severe psychological distress of evacuees in evacuation zone caused by the Fukushima Daiichi Nuclear Power Plant accident: the Fukushima Health Management Survey. PLoS One, 11(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau A, Mercer A, & Hatley N (2020). pewmethods: Pew Research Center Methods Miscellaneous Functions (R Package 1.0). [Google Scholar]
- Lubens P, & Holman EA (2017). The unintended consequences of disaster-related media coverage. Textbook of Disaster Psychiatry, 181–193. [Google Scholar]
- Lumley T (2004). Analysis of complex survey samples. Journal of Statistical Software, 9(1), 1–19. [Google Scholar]
- Lumley T (2019). survey: analysis of complex survey samples (R package version 3.35–1).
- Manderscheid RW, & Sonnenschein MA (1998). Mental health, United States, 1996. DIANE Publishing. [Google Scholar]
- Pew Research Center. (2020). The American Trends Panel survey methodology. [Google Scholar]
- Pfefferbaum B, & North CS (2020). preventi. New England Journal of Medicine. [Google Scholar]
- Qi J, Xu J, Li B, Huang J, Yang Y, Zhang Z, Yao D, Liu Q, Jia M, & Gong D (2020). The Evaluation of Sleep Disturbances for Chinese Frontline Medical Workers under the Outbreak of COVID-19. MedRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, & Xu Y (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry, 33(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Regier DA, Boyd JH, Burke JD, Rae DS, Myers JK, Kramer M, Robins LN, George LK, Karno M, & Locke BZ (1988). One-month prevalence of mental disorders in the United States: Based on five epidemiologic catchment area sites. Archives of General Psychiatry, 45(11), 977–986. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Myers JK, Kramer M, Robins LN, George LK, Karno M, & Locke BZ (1993). One-month prevalence of mental disorders in the United States and sociodemographic characteristics: the Epidemiologic Catchment Area study. Acta Psychiatrica Scandinavica, 88(1), 35–47. [DOI] [PubMed] [Google Scholar]
- Riehm K, Holingue C, Kalb L, Bennett D, Kapteyn A, Veldhuis C, Johnson R, Fallin M, Kreuter F, Stuart E, & Thrul J (2020). Associations between media exposure and mental distress among U.S. adults at the beginning of the COVID-19 pandemic. American Journal of Preventive Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross KM, Klein B, Ferro K, McQueeney DA, Gernon R, & Miller BF (2019). The Cost Effectiveness of Embedding a Behavioral Health Clinician into an Existing Primary Care Practice to Facilitate the Integration of Care: A Prospective, Case–Control Program Evaluation. Journal of Clinical Psychology in Medical Settings, 26(1), 59–67. [DOI] [PubMed] [Google Scholar]
- RStudio Team. (2016). RStudio: Integrated Development for R. RStudio, inc. [Google Scholar]
- Shiller RK (2020, April 3). COVID-19 has brought about a second pandemic: financial anxiety. World Economic Forum. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Sprang G, & Silman M (2013). Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness, 7(1), 105–110. [DOI] [PubMed] [Google Scholar]
- Stathopoulou G, Powers MB, Berry AC, Smits JAJ, & Otto MW (2006). Exercise interventions for mental health: a quantitative and qualitative review. Clinical Psychology: Science and Practice, 13(2), 179–193. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2019). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.pdf
- Task Force on Address-based Sampling. (2016). Address-based Sampling. https://www.aapor.org/Education-Resources/Reports/Address-based-Sampling.aspx
- Tausig M, & Fenwick R (2001). Unbinding time: Alternate work schedules and work-life balance. Journal of Family and Economic Issues, 22(2), 101–119. [Google Scholar]
- Unacast. (2020). Social Distancing Scoreboard.
- Usher K, Bhullar N, & Jackson D (2020). Life in the pandemic: Social isolation and mental health. Journal of Clinical Nursing. [DOI] [PubMed] [Google Scholar]
- Verduyn P, Lee DS, Park J, Shablack H, Orvell A, Bayer J, Ybarra O, Jonides J, & Kross E (2015). Passive Facebook usage undermines affective well-being: Experimental and longitudinal evidence. Journal of Experimental Psychology: General, 144(2), 480. [DOI] [PubMed] [Google Scholar]
- Vinokur A, & Selzer ML (1975). Desirable versus undesirable life events: their relationship to stress and mental distress. Journal of Personality and Social Psychology, 32(2), 329. [DOI] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, & Ho RC (2020). Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss DS (2007). The impact of event scale: revised In Cross-cultural assessment of psychological trauma and PTSD (pp. 219–238). Springer. [Google Scholar]
- Woolhandler S, & Himmelstein DU (2020). Intersecting US Epidemics: COVID-19 and Lack of Health Insurance. Annals of Internal Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Mental health and psychosocial considerations during the COVID-19 outbreak - 18 March 2020. World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/331490/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf
- Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, Miao J, Zhang C, Yang Y, & Sun W (2020). COVID-19 in Wuhan: Immediate Psychological Impact on 5062 Health Workers. MedRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]