Abstract
Background
COVID-19 pandemic has decreased worldwide surgical activity, thus impairing the training of surgical residents. As a coping strategy, we opted for laparoscopic simulation with endotrainer; however, due to social distancing rules, a face-to-face tutoring training method is unfeasible. In this context telementoring using WhatsApp® Messenger (owned by Facebook Inc., Menlo Park, CA) with a Smartphone aims to train surgical residents in laparoscopy from their homes during the pandemic.
Methods
Trainers and surgical residents who were at home participated in this study. They used endotrainers with Smartphone cameras and were trained by video calls using WhatsApp. The baseline and final score of intracorporeal knotting was measured, according to the Fundamentals of Laparoscopic Surgery (FLS) methodology, measuring the difference in means with the paired t-test. Recommendations for virtual surgical tutoring were followed and user satisfaction was measured using the Likert scale.
Results
40 surgical residents participated. The average distance between the mentor and the trainee was 12.87 km. Average bandwidth was 32.5 Megabits per second (Mbits/s), latency was 424.5 ms (ms), good quality image with immediate feedback was achieved. The statistically significant difference between basal and final measurement was 23.7 points (p < 0.001). All participants found telementoring a good educational tool.
Conclusion
Smartphone telementoring using WhatsApp® Messenger is an effective educational tool for acquiring laparoscopic skills with a statistically significant difference. This type of training represents a new teaching resource in the light of the recommendations of social distancing during a pandemic.
Keywords: Telementoring, Simulation in surgery, Laparoscopic simulation, WhatsApp, Smartphone, COVID-19
Highlights
-
•
Smartphone laparoscopic telementoring using WhatsApp® is a valid educational tool with a statistically significant difference.
-
•
This type of training represents a new teaching method considering social distancing recommendations during a pandemic.
-
•
These results can be the initiation for larger studies and introduces the idea of future surgical residency training programs.
1. Introduction
In December 2019, a new type of Coronavirus pneumonia emerged in Wuhan-China, hereafter called COVID-19 [1]. The infection spread worldwide in the following months and on March 11, 2020 it was recognized as a pandemic by the WHO.
As an initial containment measure, all elective surgeries were suspended and only emergency cases were attended in order to allocate all health resources to the attendance of COVID-19 cases [2]. This situation led to a decrease in surgical activity worldwide [3], thus impairing the training of surgical residents as well [4], as scientific societies recommended that surgeries be performed by experienced surgeons [5].
In a context in which a surgical resident needs to maintain his surgical performance, simulation with an endotrainer appears as a valid resource; however, this activity requires to be tutored by an expert surgeon in order to correct errors, unnecessary movements and technical details during training, to give feedback and make learning meaningful. However, due to social distancing rules, a face-to-face tutoring training method is unfeasible [6].
To cope with this situation, alternative laparoscopic training methods emerged, thus the objective of this study was to enable surgical residents to practice laparoscopy during the pandemic from their homes using mobile phones through a video call via WhatsApp® Messenger. For this purpose, laparoscopic training modules that use previously validated mobile phones cameras were used [[7], [8], [9]].
2. Methods
This is a cohort study with a before-and-after design and no comparison group This work has been reported in line with the Strengthening The Reporting Of Cohort Studies in Surgery (STROCSS) criteria [10]. The study was carried out between April and May 2020, during the quarantine period due to the COVID-19 pandemic. Study participants signed an informed consent virtually. The article has been registered with UIN of researchregistry6440. Hyperlink to your specific registration: www.researchregistry.com/browse-theregistry#home/registrationdetails/5ffc7579c5c568001b675ebd/
Inclusion criteria: Be a general surgical resident, with no previous laparoscopic training, have an endotrainer, forceps and materials to carry out the training at home.
Exclusion criteria: Prior training in basic and/or advanced laparoscopy and do not have internet access.
Demographic variables: Gender, age, dominant hand, year of residency.
Variables related to training: Training session, training distance, intracorporeal suture time, distance between suture edges, distance of knot placing, bandwidth, latency.
2.1. Technical aspects of telementoring
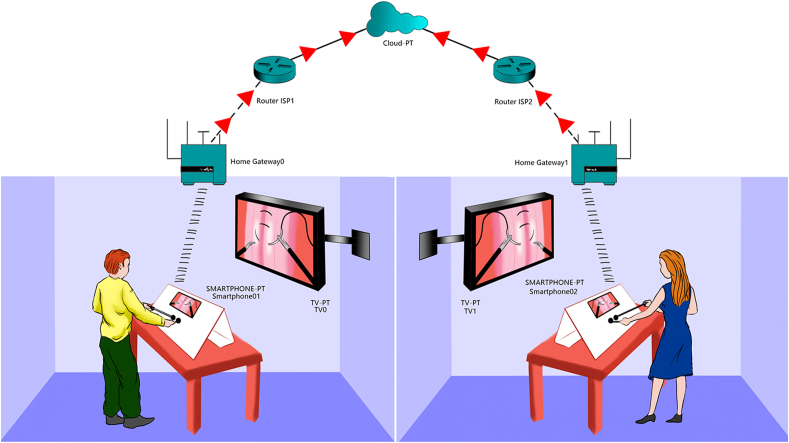
A mobile phone was used as an endotrainer camera to transmit to a television. Afterwards, the trainer made a video call to the participant using WhatsApp Messenger (Fig. 1). The bandwidth (bit rate of available or consumed information) was according to network characteristics of each participant. The latency (time in which a data packet travels between two points) was measured using the WisdomStar Ping application (v1 .3 developer Fujin St, Songshan Dist, Taipei, Taiwan). The IP address of WhatsApp web is pinged and the time it takes for the server to respond after being bombarded by a ten data packets of 64-bytes is measured. The mean number of ping measured by the application is obtained both of the trainer's and trainee's connection and then both values are added to calculate the total latency (Ping, acronym for Packet Internetwork Groper, program to determine the time it takes for data packets to reach a remote computer) [11,12].
Fig. 1.
Physical diagram of Telementoring connectivity. Home Gateway: In-home modem. Router ISPNº: Internet service provider hub router. Cloud: Internet.
2.2. Training description
Remote intracorporeal suture training was performed and scored according to the methodology validated by the Fundamentals of Laparoscopic Surgery (FLS), where a score of a 100 is considered excellent (highest scores are the best) [13,14]. Participants were evaluated with a baseline score, after which, a 2-h telementoring session is given. Participants are then asked to train for 10 h according to the guidelines given and the next day are evaluated obtaining a final score. The trainers were 2 general surgeons with training in advanced laparoscopic surgery.
2.3. Statistical analysis
To evaluate the normality of the data set, the Shapiro-Wilk test was used. Mean differences of baseline and final scores of intracorporeal suture were measured using the paired t-test. Statistical analysis was performed with the Software for Statistics and Data Science software (v15.0; STATA, Lakeway, TX), p < 0.001 was considered statistically significant.
3. Results
Forty general surgical residents from Lima-Peru participated. The average age was 29.7 years (range: 28–42), 30 men and 10 women, the dominant hand and the year of residency were also recorded (Table 1). Both trainers and residents were at home at an average distance of 12.87 km (range: 8–20 km). The average bandwidth used was 32.5 Megabits per second (Mbits/s) with a mean latency of 424.5 ms (ms) (range: 402–447 ms). Telementoring sessions were performed with a good image quality, with immediate and real-time feedback.
Table 1.
Demographic variables of surgical residents participating in Telementoring using a smartphone.
| Number of participants | (n = 40) |
|---|---|
| Age (years) | 29.7 (28–42) |
| Women | 10 (25%) |
| Male | 30 (75%) |
| Dominant right hand | 34 (85%) |
| Dominant left hand First year residents |
6 (15%) 14 (35%) |
| Second year residents | 14 (35%) |
| Third year residents | 12 (30%) |
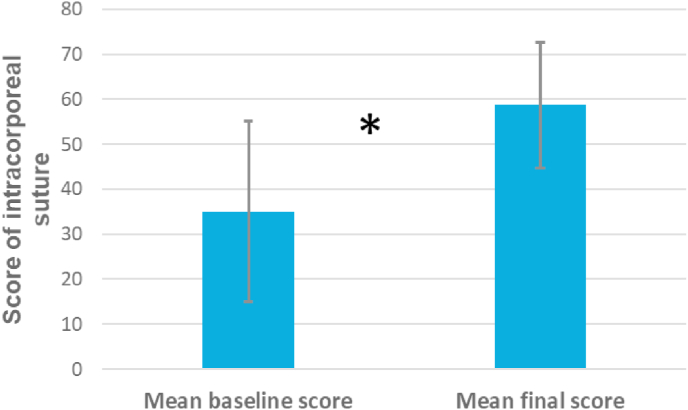
The mean baseline score of the placement of a suture and intracorporeal knot tying was 35.04 (range: 3.5–66.5, SD: 20), the mean score obtained by the participants after telementoring was 58.745 (range: 30.9–80.1, DS: 13.9). All participants had a higher score after remote training and the mean difference between the final and baseline measurement is 23.7 points, the difference is statistically significant (p < 0.001) (Fig. 2).
Fig. 2.
Comparison of mean baseline and final scores of intracorporeal suture in Telementoring. The difference is statistically significant (p < 0.001).
Level of satisfaction of the telementoring participants was measured with a 5-point Likert scale with 4 questions (Table 2).
Table 2.
Telementoring user satisfaction.
| Question | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Good image quality during telementoring | 32 | 6 | 2 | 0 | 0 |
| Teaching tutoring was adequate and immediate | 32 | 8 | 0 | 0 | 0 |
| Telementoring seemed useful for training intracorporeal knots | 36 | 4 | 0 | 0 | 0 |
| Telementoring seemed like a good educational tool | 40 | 0 | 0 | 0 | 0 |
Five-point Likert scale. 1 Strongly agree, 2 agree, 3 neutral, 4 Disagree, 5 Strongly disagree.
4. Discussion
In this study, we found that real-time laparoscopic telementoring using a Smartphone represents a useful educational tool. It was demonstrated, with a statistically significant difference, the acquisition of intracorporeal suturing skills after training at home being remotely tutored by an expert surgeon.
Laparoscopic training using mobile phones or tablets has been carried out for several years. For instance, in 2013 Bahsoun AN et al. published the validation of an endotrainer developed using this technology, then in 2014 Yoon R et al. carried out a study in which they compare an endotrainer using a Tablet with a standard laparoscopic endotrainer for testing of basic laparoscopic skills [15] and concluded that the first one had superior image quality and resolution, besides of being inexpensive, portable and easily available. In this study, an endotrainer with a design similar to the previous ones using a Tablet or a mobile phone is used, with characteristics resembling those published by Thinggaard E et al., in 2015 (8) and by Sanguinetti J in 2019 (9).
WhatsApp application is used in medicine as an effective way of communication between doctors to report the status of hospitalized patients, as well as, to improve communication between resident and specialist [16]. Studies show this application is being more frequently used within surgical specialties, thus, the usage of Whatsapp Messenger over other type of video calling software [17], becoming especially important during the COVID-19 pandemic as an educational tool, used to share scientific articles, photographs and questions for educational purposes [18]. The present study, unlike others, is the first to use the WhatsApp application to telementor laparoscopic surgery.
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), defined surgical telementoring as “a relationship facilitated by telecommunications technology, in which an expert provides guidance to a less experienced student, from a remote location” [19], This definition is related to what is described in this article, where an expert surgeon supervises the laparoscopic training in real time for resident doctors.
In 2016, the SAGES convened the “Project 6 Summit” to review the art of virtual surgical teaching. In this context, 5 working groups were formed, one of these was the Technology Working Group, that established considerations for surgical telementoring. It should be conducted across 40 Mbits/s bandwidths with a latency not greater than 450 ms, video should have a 1080 p resolution at 30 frames per second (fps) and must have telestration capability (draw virtually on the student's video screen to improve communication). In our work, the average bandwidth was 32.5 Mbits/s, latency 424.5 ms, the resolution was 1080p at 30 fps in all cases, and telestration was achieved by drawing on the screenshot of the video. Although average bandwidth was less than recommended, telementoring went smoothly. Recommendations regarding patient safety and cost do not apply to the present work [11]. Therefore, this study meets the considerations of surgical telementorship, so it is important to consider these aspects in the results.
Telementoring was designed for expert surgeons to tutor surgeons in training from a remote location, especially for those who work in rural areas or in developing countries [20,21]. In this study, telementoring was used for laparoscopic training with an endotrainer, in which expert surgeons tutored surgical residents, both from their homes as established by social distancing rules due to COVID-19 pandemic.
There are 2 studies with similar characteristics to our study. One was carried out in Africa in 2009 and the other in Colombia in 2013; in both studies the Skype TM software (Technologies SA, Luxembourg) was used, web cameras and computers were utilized for video calls, as well as, the 5 tasks of the FLS [22,23]. Unlike these works, in our study the WhatsApp application and a mobile phone camera were used to conduct the telementoring, allowing in-home training. We also study telementoring technology such as bandwidth, latency and telestration. Only 1 task of the FLS is used corresponding to intracorporeal suture.
Studies of telementoring in surgery have been published, where surgeries in experimental surgery, thyroidectomies, cholecystectomies and with augmented reality simulators are tutored [24]. Unlike those studies, this article uses an endotrainer, being therefore more economical and free from ethical implications for not involving patients or experimental animals.
One systematic review states that there is limited evidence to support telementoring effectiveness and further studies are needed to provide evidence for it to be comparable with in-situ mentoring [25]. This study demonstrates telementoring is effective to acquire laparoscopic skills with a statistically significant difference; however, it is not comparable with face-to-face mentoring.
It is important to mention that advances in telecommunication technology have facilitated innovative teaching resources for laparoscopy surgery. For instance, at the Hospital Clinic of Barcelona-Spain [26], an expert surgeon performs advanced laparoscopic surgery that is transmitted in real time to a remote place, explaining each step as is being performed. This also postulates the idea that surgeries can be tutored in real time from a remote place; however, this type of mentoring arises an ethical problem in which legal responsibility in the event of possible complication is not well defined yet. Compared to this article, we provided practical laparoscopic learning skills for surgical residents, where surgery is not tutored but laparoscopic tasks. It should be also noted that this an economic way of training as well. However, one of the limitations of the study is that participants must have an endotrainer, forceps and laparoscopic needle holders at home, thus limiting the number of participants in the study. Also, the evaluation of penalty scores was measured by the resident and not by an evaluator. Educational impact is therefore demonstrated as shown by the acquisition of laparoscopic skills in performing intracorporeal suture; however, clinical impact has not yet been established, which could be done in later studies.
These results can serve as a starting point for further studies with a larger number of participants and opens up the possibility of future training programs for surgical residents, not only at this time of urgent need during a pandemic, but also to be included in the standardized training program, mainly in the first years of residence, providing more practice hours, FLS exercises, suturing exercises and needle manipulation in a cavity with more complex characteristics.
The acquisition of laparoscopic skills is demonstrated with a statistically significant difference, which is an objective measure. Although user satisfaction appears to be subjective, it was measured with a Likert scale, which has been used previously in surgical education studies.
5. Conclusion
Remote laparoscopic training in real time with a smartphone is effective in terms of the acquisition of laparoscopic skills after telementoring, with a statistically significant difference. In addition, this type of training represents a new educational tool for laparoscopic in-home training in the light of social distancing measures that must be followed during a pandemic.
Disclosure
Yeray Trujillo Loli, have no conflict of interest or financial ties to disclose.
Mario D'Carlo Trejo Huamán, have no conflict of interest or financial ties to disclose.
Stefanie Campos Medina, have no conflict of interest or financial ties to disclose.
Acknowledgments
Jubal Trujillo Loli: electronic engineer.
Juan Pablo Aparco: statistical analysis.
Josue Ismael Vega Landa. Medical Illustrator.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.amsu.2021.01.085.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China [published online ahead of print, 2020 Feb 7] J. Am. Med. Assoc. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bundu I., Patel A., Mansaray A., Kamara T.B., Hunt L.M. Surgery in the time of Ebola: how events impacted on a single surgical institution in Sierra Leone. JRAMC. 2016:1–5. doi: 10.1136/jramc-2015-000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans [published online ahead of print, 2020 May 12] Br. J. Surg. 2020 doi: 10.1002/bjs.11746. 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferrario L., Maffioli A., Bondurri A.A., Guerci C., Lazzarin F., Danelli P. COVID-19 and surgical training in Italy: residents and young consultants perspectives from the battlefield [published online ahead of print, 2020 Jun 1] Am. J. Surg. 2020;S0002–9610(20) doi: 10.1016/j.amjsurg.2020.05.036. 30349-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balibrea J.M., Badia J.M., Rubio Pérez I., Martín Antona E., Álvarez Peña E., García Botella S., Álvarez Gallego M., Martín Pérez E., Martínez Cortijo S., Pascual Miguelañez I., Pérez Díaz L., Ramos Rodriguez J.L., Espin Basany E., Sánchez Santos R., Soria A. Manejo quirúrgico de pacientes con infección por COVID-19. Recomendaciones de la Asociación Española de Cirujanos. Cirugía Española. 2020;98(5):251–259. doi: 10.1016/j.ciresp.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chu D.K., Akl E.A., Duda S. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bahsoun A.N., Malik M.M., Ahmed K., El-Hage O., Jaye P., Dasgupta P. Tablet based simulation provides a new solution to accessing laparoscopic skills training. J. Surg. Educ. 2013;70(1):161–163. doi: 10.1016/j.jsurg.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Thinggaard E., Bjerrum F., Strandbygaard J., Gögenur I., Konge L. Validity of a cross-specialty test in basic laparoscopic techniques (TABLT) Br. J. Surg. 2015;102(9):1106–1113. doi: 10.1002/bjs.9857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanguinetti J., Viola M., Tarabochia C. Mobile app for laparoscopic surgery training. EC Gastroenterology and Digestive System. 2019;6(3):1–9. [Google Scholar]
- 10.Agha R., Abdall-Razak A., Crossley E., Dowlut N., Iosifidis C., Mathew G., for the STROCSS Group The STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Bogen E.M., Schlachta C.M., Ponsky T. White paper: technology for surgical telementoring-SAGES project 6 technology working group. Surg. Endosc. 2019;33(3):684–690. doi: 10.1007/s00464-018-06631-8. [DOI] [PubMed] [Google Scholar]
- 12.Griera J., Barceló J.M. UOC; Barcelona: 2009. Estructura de redes de computadoras; pp. 494–495. En. [Google Scholar]
- 13.Derossis A.M., Fried G.M., Abrahamowicz M., Sigman H.H., Barkun J.S., Meakins J.L. Development of a model for training and evaluation of laparoscopic skills. Am. J. Surg. 1998;175(6):482–487. doi: 10.1016/s0002-9610(98)00080-4. [DOI] [PubMed] [Google Scholar]
- 14.Peters J.H., Fried G.M., Swanstrom L.L. Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery. 2004;135(1):21–27. doi: 10.1016/s0039-6060(03)00156-9. [DOI] [PubMed] [Google Scholar]
- 15.Yoon R., Del Junco M., Kaplan A. Development of a novel iPad-based laparoscopic trainer and comparison with a standard laparoscopic trainer for basic laparoscopic skills testing. J. Surg. Educ. 2015;72(1):41–46. doi: 10.1016/j.jsurg.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 16.Gould G., Nilforooshan R. WhatsApp Doc? BMJ Innov. 2016;2(3):109–110. doi: 10.1136/bmjinnov-2016-000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mars M., Scott R.E. WhatsApp in clinical practice: a literature review. Stud. Health Technol. Inf. 2016;231:82–90. [PubMed] [Google Scholar]
- 18.Hughes B.A., Stallard J., West C.C. The use of WhatsappⓇ as a way to deliver plastic surgery teaching during the COVID-19 pandemic. J. Plast. Reconstr. Aesthetic Surg. 2020;73(7):e1–e2. doi: 10.1016/j.bjps.2020.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schlachta C.M., Nguyen N.T., Ponsky T., Dunkin B. Project 6 Summit: SAGES telementoring initiative. Surg. Endosc. 2016;30(9):3665–3672. doi: 10.1007/s00464-016-4988-5. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen N.T., Okrainec A., Anvari M. Sleeve gastrectomy telementoring: a SAGES multi-institutional quality improvement initiative. Surg. Endosc. 2018;32(2):682–687. doi: 10.1007/s00464-017-5721-8. [DOI] [PubMed] [Google Scholar]
- 21.Glenn I.C., Bruns N.E., Hayek D., Hughes T., Ponsky T.A. Rural surgeons would embrace surgical telementoring for help with difficult cases and acquisition of new skills. Surg. Endosc. 2017;31(3):1264–1268. doi: 10.1007/s00464-016-5104-6. [DOI] [PubMed] [Google Scholar]
- 22.Okrainec A., Henao O., Azzie G. Telesimulation: an effective method for teaching the fundamentals of laparoscopic surgery in resource-restricted countries. Surg. Endosc. 2010;24(2):417–422. doi: 10.1007/s00464-009-0572-6. [DOI] [PubMed] [Google Scholar]
- 23.Ó Henao, Escallón J., Green J. Fundamentals of laparoscopic surgery in Colombia using telesimulation: an effective educational tool for distance learning. Biomedica. 2013;33(1):107–114. doi: 10.1590/S0120-41572013000100013. [DOI] [PubMed] [Google Scholar]
- 24.Augestad K.M., Han H., Paige J. Educational implications for surgical telementoring: a current review with recommendations for future practice, policy, and research. Surg. Endosc. 2017;31(10):3836–3846. doi: 10.1007/s00464-017-5690-y. [DOI] [PubMed] [Google Scholar]
- 25.Bilgic E., Turkdogan S., Watanabe Y. Effectiveness of telementoring in surgery compared with on-site mentoring: a systematic review. Surg. Innovat. 2017;24(4):379–385. doi: 10.1177/1553350617708725. [DOI] [PubMed] [Google Scholar]
- 26.Lacy A.M., Bravo R., Otero-Piñeiro A.M. 5G-assisted telementored surgery. Br. J. Surg. 2019;106(12):1576–1579. doi: 10.1002/bjs.11364. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.