Abstract
India is yet to establish a national surveillance for birth defects (congenital disorders). The objective of this study was to describe the epidemiology of birth defects in the neonatal, post-neonatal, and 1–4-year age groups, using modelled estimates from the Global Burden of Disease (GBD) database. We extracted age- and condition-specific birth defect mortality data and analysed the magnitude and trends of these conditions in India, and across Indian states. We compared these trends with other neonatal causes of mortality for the period 1990–2017. The results indicate that birth defects caused 37,104 (95%UI 31,825–43,134) deaths in the early neonatal period and 27,120 (95%UI 23,490–30,777) deaths in the post-neonatal period in 2017 in India. These rates were double and five times higher when compared with the whole group of middle- and high-income countries respectively. There was a small decline in birth defect mortality between 1990 and 2017. However, with the exception of orofacial clefts, the proportion of deaths caused by selected birth defects increased between 1990 and 2017, relative to other causes of child mortality. In 70% of states ranked in the high and middle Socio-demographic Index (SDI) category, birth defects were the third leading cause of neonatal mortality. The analysis identifies the need for establishing birth defects services in the country. It demonstrates that modelled estimates of the GBD could be used as the best available data for understanding the epidemiology of birth defects in low- and middle-income countries till surveillance systems are put in place.
Electronic supplementary material
The online version of this article (10.1007/s12687-020-00487-z) contains supplementary material, which is available to authorized users.
Keywords: Birth defects, Congenital, India, Epidemiology, Child mortality, Global Burden of Disease
Introduction
India is yet to put in place a system for surveillance of birth defects. A limited number of studies and public data point to the sheer magnitude of birth defects in the country. A systematic review and meta-analysis estimated that the pooled national birth prevalence of congenital anomalies in the country was 184.48 per 10,000 births (95%CI 164.74–204.21) (Bhide and Kar 2018). A cohort study reported that the total prevalence of major congenital anomalies was 230.51 (95%CI 170.99–310.11) (Bhide et al. 2016). The latter estimated that major congenital anomalies affected one in 44 pregnancies and that there may be 589,990 (437,674–793,445) affected births in India each year. The only available public data on birth defects is from a government child health programme, the Rashtriya Bal Swasthya Karyakram (RBSK) (Ministry of Health and Family Welfare 2013). Under this programme, mobile teams of doctors screen children in the age group of 2 to 18 years for common childhood diseases, nutritional deficiencies, birth defects, and developmental delays and disabilities (Kar et al. 2020). Although all birth defects are reported, free-of-cost services are available at government hospitals for nine conditions (neural tube defects, Down syndrome, cleft lip/palate, clubfoot, developmental dysplasia of hip, congenital cataract, congenital deafness, congenital heart defects, retinopathy of prematurity, congenital hypothyroidism, sickle cell anaemia, and thalassemia). Monthly reports on number of confirmed cases are collated by the RBSK. In 2016, 300,000 of 187 million screened children were diagnosed with a birth defect (Government of India 2019). These statistics under-report birth defects, as data for children less than 2 years of age are not included. There is also a possibility that sick or disabled children may not attend the screening camps or attend schools or play centres. The statistics do not include data from private health care facilities, used by 70% of the Indian population. A little over half the deliveries (52%) occur at private hospitals (Indian Institute of Population Studies and ICF 2017), but there is no system to document the number of affected births from these facilities.
Other evidences urge the need to understand the epidemiology of birth defects in India. The country reports 24 million births, that is, nearly one-fifth of births occurring worldwide. Health and demographic data reflect evidences of epidemiological transition (Government of India Ministry of Health and Family Welfare 2019). The infant mortality rate is 33 per 1000 live births with a large urban (23)-rural (38) difference. Neonatal mortality rate is 24 per 1000 live births and shows a similar urban-rural difference (14 for urban and 27 for rural areas). In keeping with global trends (Hug et al. 2019), mortality from common infectious causes such as pneumonia, diarrhoea, and measles declined significantly by 5.4% for children aged 1–59 months (Government of India Ministry of Health and Family Welfare 2019; Sankar et al. 2016). The average annual decline in neonatal mortality rates from 2000 to 2015 was 3.3%, brought about by decrease in mortality from complications of prematurity, intrapartum complications and low birth weight (UN IGME 2017). Decrease in these causes indicates that the proportion of deaths due to birth defects are likely to increase, but there is no source of data to identify whether this phenomenon is occurring in the country or not.
In this study, we have used the modelled estimates from the Global Burden of Disease (GBD) database to describe the epidemiology of birth defects in India. Keeping in mind that different states and Union Territories (regions) of India have different Socio-demographic Index (SDI) levels (Sagar et al. 2020), we also analysed birth defects mortality in relation to other causes of neonatal and child mortality across the states of the country.
Methodology
Conditions
The GBD list consists of a series of “exhaustive but mutually exclusive” list of conditions that are hierarchically organised into four levels (Institute for Health Metrics and Evaluation 2020). Birth defects are categorised under the level 1 cause “non-communicable” diseases, and level 2 cause “other non-communicable conditions.” “Congenital birth defects” (B12.1) includes 11 level 4 conditions which consist of congenital anomalies (neural tube defects, congenital heart anomalies, orofacial clefts, congenital musculoskeletal and limb anomalies, urogenital congenital anomalies, digestive congenital anomalies, other congenital birth defects) and chromosomal abnormalities (Down syndrome, Turner syndrome, Klinefelter syndrome, and other chromosomal abnormalities).
Mortality data
Age- and condition-specific mortality data were extracted from the GBD database (IHME GBD Compare Data Visualization 2018a) for the early neonatal (EN) period (0–6 days), late neonatal (LN) period (7–27 days), post-neonatal (PN) period (28–364 days), and in the 1–4-year age group for the years 1990 to 2017. For comparing birth defect mortality with other prevalent causes of neonatal and child mortality, data were extracted for neonatal preterm birth, neonatal encephalopathy due to birth asphyxia and trauma, neonatal sepsis, and other neonatal infections, diarrhoeal diseases, and lower respiratory tract infections (LRI). For comparing Indian birth defect mortality statistics with the global situation, data were extracted for the year 2017 for countries grouped by SDI as high, high-middle, low-middle, and low SDI regions. The data were extracted using the GBD results tool (IHME GBD Results Tool 2018b).
State-level data
The states of India are at different levels of development and have been categorised into three groups, based on their SDI. SDI is a composite indicator of development status, which includes per capita income, mean education in people aged 15 years and older, and total fertility rate in people younger than 25 years (Murray et al. 2018). States and Union Territories have been grouped into three categories based on their SDI level (Supplementary Table 1). State-level data on birth defect mortality were extracted from GBD India Visualization Hub (IHME GBD India Compare 2018c).
Analysis
Descriptive statistics were used to report the data. Mortality in the early neonatal, late neonatal, post-neonatal period, and in the 1–4-year age group were expressed in absolute numbers, or as rates per 1000 live births or per 100,000 population. Change in mortality due to birth defects, preterm birth complications, neonatal encephalopathy, neonatal sepsis, LRI, and diarrhoea were examined for the period 1990 to 2017. Change in mortality was reported as percentage change in absolute numbers of deaths between time periods, or from estimates available from the GBD India Visualization Hub (IHME GBD India Compare 2018c). Statistical significance was reported using Pearson’s chi-square statistic with significance level set at P < 0.05. GBD estimates are reported with 95% uncertainty intervals (UI).
Results
Birth defect mortality globally and India
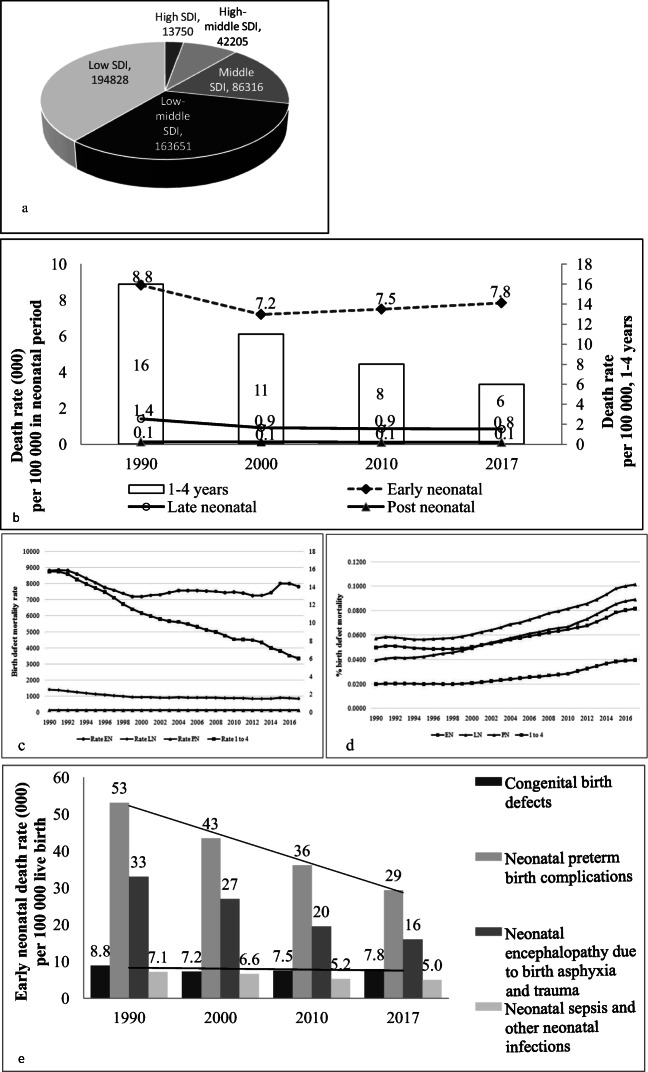
In absolute numbers, the estimates indicated that globally, there were a total of 501,764 (95%UI 474,132–534,019) birth defect deaths among children under 5 years of age in 2017 (Table 1, Supplementary Table 2). Over 70% of these deaths occurred in low (194,828; 176,323–216,684) and low-middle (163,651; 150,962–179,246) SDI countries (Fig. 1a). The number of deaths were lower, but not insignificant, in middle SDI 86,316 (95%UI 80,230–91,640) and high-middle SDI (42,205; 39,794–45,293), and were lowest in high SDI (13,750; 12,529–15,416) countries. Globally, birth defect mortality was highest in the early neonatal (174,420, 35%) and the post-neonatal (193,365, 39%) periods, and lowest in the 1- to 4-year age group (75,939, 3%) (Table 1).
Table 1.
Estimated birth defect deaths in the early neonatal (0–6 days), late neonatal (7–27), post-neonatal (28–364 days), and 1- to 4-year age group by global regions and India (2017)†
| Early neonatal | Late neonatal | Post-neonatal | 1 to 4 years | Total (under 5 years) | |
|---|---|---|---|---|---|
| Global | 174,420 | 58,040 | 193,365 | 75,939 | 501,764 |
| High SDI | 5436 (3) | 2133(4) | 4585 (2) | 1596 (2) | 13,750 (2) |
| High-middle SDI | 13,424 (8) | 5363 (9) | 17,787 (9) | 5631 (2) | 42,205 (2) |
| Middle SDI | 30,841 (18) | 10,578 (18) | 35,291 (18) | 9606 (13) | 86,316 (13) |
| Low-middle SDI | 58,542 (34) | 20,020 (34) | 61,170 (32) | 23,919 (31) | 163,651 (31) |
| Low SDI | 65,905 (38) | 19,828 (34) | 74,043 (38) | 35,052 (46) | 194,828 (46) |
| India | 37,104 (21) | 11,864 (20) | 27,120 (14) | 6348 (8) | 82,436 (16) |
†Estimated absolute number of deaths. Numbers in parenthesis indicate the percentage of deaths for the region/India as compared with total numbers of global deaths Detailed data is shown in Supplementary Table 1
Fig. 1.
Birth defect mortality burden globally and in India. a Estimated number of birth defect deaths in children under 5 years of age by SDI regions, illustrating the mortality burden in low and low-middle SDI regions. b Birth defect mortality rate in children less than 5 years of age in thousands per 100,000 population in India, indicating that this rate is highest in the early neonatal period, but decreases during the post-neonatal, late neonatal periods, and 1–4-year age group. c Although the birth defect mortality rate in the early neonatal (EN), late neonatal (LN), post-neonatal (PN), and 1 to 4-year age group shows a decline, d it shows that there is an increase in the proportion of birth defect deaths per 100,000 population in India over time. e Early neonatal mortality rate caused by preterm birth complications, neonatal encephalopathy, neonatal sepsis, and birth defects. The declining rates of the first three causes and constancy in birth defect mortality rates explain the increasing contribution of birth defects to major causes of deaths in the early neonatal period
Mortality data from India indicated that in 2017, 16% (that is 82,436 out of 501,764) of global birth defect deaths among children younger than 5 years of age occurred in India (Table 1). Worldwide, India contributed to 21% (37,104 out of 174,420) of birth defect deaths in the early neonatal period, 20% (11,864 out of 58,040) deaths in the late neonatal period, 14% in the post-neonatal period (27,120 out of 193,365), and 8% (6348 out of 75,939) in the 1 to 4 age group. The magnitude of deaths occurring in India in the early neonatal period was nearly seven times that of high SDI countries (82,436 versus 13,750), and double that of high-middle SDI countries (82,436 versus 42,205). Half of birth defect mortality occurring in low-middle SD I countries (82,436 out of 163,651) occurred in India. The birth defect mortality rate was higher for India (7842 deaths per 100,000), as compared with low-middle SDI group of countries (7611 deaths per 100,000). High SDI countries had the lowest birth defect mortality rates (2450 per 100,000 population) (Supplementary Table 2).
Magnitude and trends in India
Birth defect mortality was highest in the early and late neonatal periods, and declined thereafter. In 2017, these rates were 7842 per 100,000 population (95%UI 6726–9116) in India, but declined thereafter, in the late neonatal period (846; 730–955), post-neonatal period (122; 105–137), and age group of 1–4 years (6; 4.8–7.3) (Supplementary Table 1). Between 1990 and 2017, birth defect mortality rates in India declined (Fig. 1b). In the early neonatal period for example, the rate declined from 44,744 deaths (death rate 88 per 1000 population) in 1990 to 37,104 deaths (death rate 78 per 1000 population) in 2017. Of significance however, was the observation that although there was a decline in birth defect deaths in India between 1990 and 2017 for the early and late neonatal periods, post-neonatal period, and 1- to 4-year age group (Fig. 1c), there was an increase in the proportion of mortality caused by birth defects as compared with all-cause mortality in children less than 5 years of age (Fig. 1d). This increase was from 4.0% in 1990 to 7.9% in 2017. This increasing proportion of deaths from birth defects could be explained by reduction in mortality from other major causes of mortality. In the early neonatal period for example, between 1990 and 2017, neonatal encephalopathy deaths reduced by 52%, preterm birth complications reduced by 45%, and neonatal sepsis reduced by 30%, while there was only 11% reduction in birth defect mortality over this period (Fig. 1e).
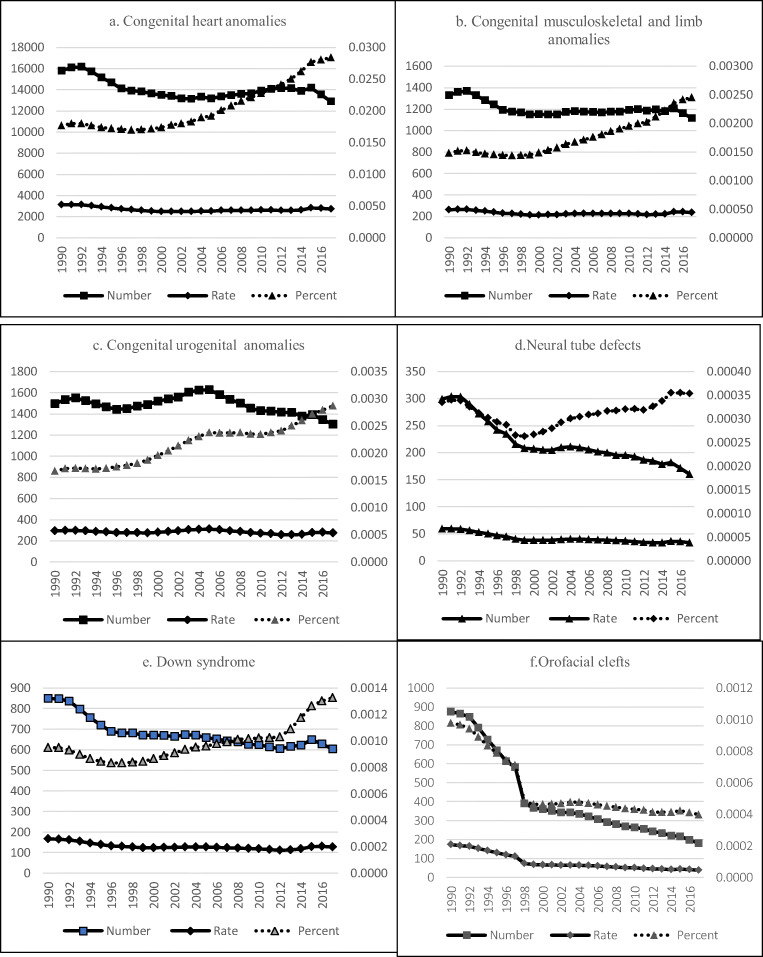
By type of birth defect
Like overall trends, there was a decrease in the number and rates of three common birth defects (congenital heart defects, congenital musculoskeletal anomalies, and urogenital congenital anomalies), although the proportion of birth defect mortality among total deaths increased (Fig. 2, Table 2). Congenital heart defects showed a decrease (the rate decreased from 45.5; 22.2–65.01 to 30.09; 21.15–38.0) but the proportion among total deaths increased from 1.955 (0.94–2.8) to 3.76 (2.65–4.69) between 1990 and 2017. Congenital musculoskeletal anomalies showed a similar decrease in rate from 2.01 (0.94–3.96) to 1.44 (0.8–2.38), but the proportion among total deaths increased from 0.086 (0.041–0.17) to 0.18 (0.099–0.3) between 1990 and 2017. Urogenital congenital anomalies also showed a decrease from 2.05 (0.82–3.46) to 1.57 (0.84–2.44), with identical increase in proportion among total deaths from 0.088 (0.035–0.15) to 0.2 (0.11–0.3) between 1990 and 2017. Mortality rates for neural tube defect decreased from 0.57 (0.28–1.187) to 0.23 (0.14–0.35) but the proportion did not show an increase (0.024; 0.012–0.048 to 0.028; 0.018–0.044) between 1990 and 2017. A similar trend was seen for Down syndrome, that is, although the rate decreased from 2.37(0.74–5.18) to 1.36(0.72–2.76), the proportion remained unchanged between 1990 and 2017 (0.1; 0.031–0.22 to 0.17; 0.091–0.34). However, the most notable change was observed for orofacial clefts, where the rate decreased from 45.5 (22.2–65.01) to 30.09 (21.15–38), but the proportion of mortality associated with orofacial cleft showed a marked decrease in proportion to total deaths from 0.057 (0.017–0.17) to 0.027 (0.012–0.06).
Fig. 2.
Trends in specific types of birth defects in India 1990–2017. The primary axis shows the number (square boxes) and rates (diamonds) of birth defects and the secondary axis shows the percent change in selected birth defects between 1990 and 2017 in India. With the exception of orofacial clefts, birth defect death rates have declined, but the proportion of birth defect mortality has increased over time. This increase is not marked for neural tube defects and Down syndrome, while there is a marked decrease in the proportion of orofacial cleft mortality over time
Table 2.
Number of deaths, mortality rates, and percent change between 1990 and 2017 for selected birth defects in India#
| 1990 | Change | 2017 | Change | |||
|---|---|---|---|---|---|---|
| Number* | Rate** | Percent*** | Number* | Rate** | Percent*** | |
| Congenital heart anomalies |
54,654 (26,660–78,087) |
45.5 (22.2–65.01) |
1.95 (0.94–2.8) |
38,920 (27,355–49,142) |
30.09 (21.15–38.0) |
3.76 (2.65–4.69) |
| Congenital musculoskeletal and limb anomalies |
2420 (1133–4761) |
2.01 (0.94–3.96) |
0.086 (0.041–0.17) |
1863 (1037–3072) |
1.44 (0.8–2.38) |
0.18 (0.099–0.3) |
| Urogenital congenital anomalies |
2458 (988–4155) |
2.05 (0.82–3.46) |
0.088 (0.035–0.15) |
2026 (1089–3155) |
1.57 (0.84–2.44) |
0.2 (0.11–0.3) |
| Neural tube defects |
682.97 (337.44–1357.22) |
0.57 (0.28–1.187) |
0.024 (0.012–0.048) |
292.62 (186.49–457.46) |
0.23 (0.14–0.35) |
0.028 (0.018–0.044) |
| Down syndrome |
2851 (891–6216) |
2.37 (0.74–5.18) |
0.1 (0.031–0.22) |
1761 (935–3574) |
1.36 (0.72–2.76) |
0.17 (0.091–0.34) |
| Orofacial clefts |
1603 (483–4939) |
45.5 (22.2–65.01) |
0.057 (0.017–0.17) |
284 (935–3574) |
30.09 (21.15–38) |
0.027 (0.012–0.06) |
#Data from the GBD India Visualization Hub (IHME GBD India Compare 2018c)
*Number of birth defect deaths
**Per 100,000 population
***Proportion of deaths for the specific type of birth defect relative to deaths from all causes
Gender
There was a difference in birth defect mortality by gender, with mortality being higher among girls than boys (Table 3). Using data from the year 2017, statistically significant differences were observed in the early neonatal period (7985 girls, versus boys 7711) (P < 0.00001), late neonatal period (girls 939 versus boys 761) (P < 0.00001), and post-neonatal period, (girls 135 against 109 for boys) (P < 0.00001).
Table 3.
Gender difference in birth defect mortality in India (2017)
| Numbers* | Rate ** | Percent *** | ||||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | |
| Early neonatal |
19,103.53 (15,076.25–22,907.64) |
18,000.54 (15,009.29–21,861.78) |
7711.52 (6085.83–9247.12) |
7985.91 (6658.85–9698.95) |
7.62 (6.07–9.1) |
8.84 (7.35–10.64) |
| Late neonatal |
5588.68 (4426.24–6522.65) |
6275.09 (5172.5–7303.58) |
761.06 (602.76–888.25) |
938.78 (773.83–1092.65) |
10.24 (8.1–11.81) |
10.02 (8.31–11.58) |
| Post-neonatal |
12,785.94 (10,306.36–15,084.03) |
14,334.03 (12,066.93–16,806.04) |
109.36 (88.15–129.02) |
135.01 (113.66–158.3) |
9.05 (7.25–10.51) |
8.78 (7.38–10.18) |
| 1 to 4 years |
2803.539 (2205.22–3458.44) |
3544.27 (2774.65–4393.08) |
5.09 (4.01–6.28) |
7.07 (5.54–8.77) |
3.86 (3.03–4.67) |
4.08 (3.22–4.95) |
| < 5 years |
40,281.68 (32,475.1–45,438.97) |
42,153.93 (36,563.38–47,666.27) |
59.48 (47.95–67.1) |
68.42 (59.35–77.37) |
7.75 (6.29–8.68) |
8.16 (7.19–9.11) |
#Data from the GBD India Visualization Hub (IHME GBD India Compare 2018c)
*Number of deaths
**Per 100,000 population
***Total death
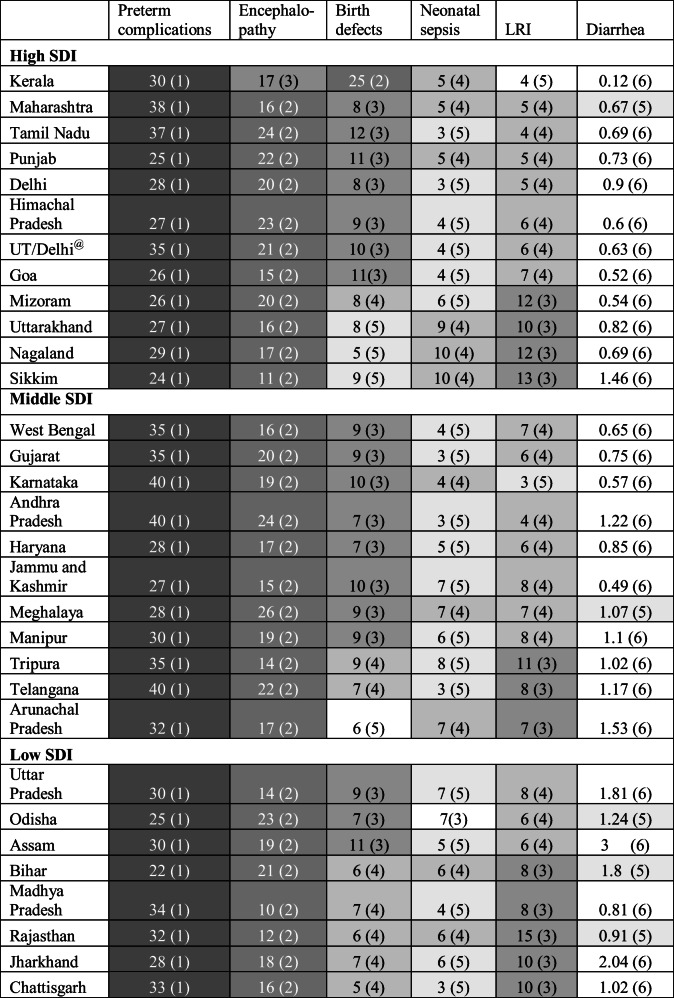
Birth defect deaths across Indian states by SDI categories
The states of India have been categorised into high, middle, and lower SDI groups (Supplementary Table 1). Table 4 shows that in only one high SDI state (Kerala), congenital birth defects were the second largest cause of mortality. In seven of 12 high SDI states, eight out of 11 middle SDI states, and three out of eight low SDI states, congenital birth defects were the third leading cause of early neonatal mortality. Thus in 17 out of 31 states/regions of the country, congenital birth defects were the third leading cause of neonatal mortality. As described above, reduction in other causes of mortality (neonatal sepsis and other infections, LRI and diarrhoea) was responsible for congenital birth defects deaths emerging as a major cause of child mortality the high and middle SDI, and three of the most populous low SDI states of the country.
Table 4.
Birth defect early neonatal mortality rate and rank of Indian states by SDI group*
*The states of India are grouped by SDI categories. Numbers indicate rates per 100,000 of selected common causes of neonatal and child mortality (preterm birth complications, neonatal encephalopathy, birth defects, neonatal sepsis, lower respiratory tract infections (LRI), and diarrhoea). Numbers in parenthesis indicate rate rank in descending order of magnitude, also indicated by darker to lighter shading. @Union territories other than Delhi
Discussion
In this study on the epidemiology of birth defects in India, we used data available from the GBDI database to describe the person, place, and time distribution of birth defect deaths in the country. Although the GBDI data are modelled estimates, and the data excludes stillbirths and terminations of pregnancy for foetal anomalies (TOPFA), they represent the best available data in a setting where a birth defect surveillance is not yet in place. The first finding from this analysis was that birth defects are a problem of LMICs, as the largest numbers of birth defect deaths, accounting for nearly 70% of global deaths, occur in these settings. India accounted for nearly 16% of global birth defect deaths among children less than 5 years of age, indicating the need for expanding the existing interventions into a full-fledged birth defects service with prevention, surveillance, and care as essential components. Birth defect mortality was highest in the early neonatal period in India. Similar findings have been recently reported by the India State-Level Disease Burden Initiative Child Mortality Collaborators, who noted that nationally, congenital birth defect mortality (8.6%) ranked as the fourth leading cause of neonatal death, after neonatal preterm birth (27·7%), neonatal encephalopathy due to birth asphyxia and trauma (14·5%), and lower respiratory infections (11·0%) (India State-Level Disease Burden Initiative Child Mortality Collaborators 2020). Although all causes of mortality showed a steep decline between 2000 and 2017, the decline was the least for congenital birth defects.
The current study, which is a detailed analysis of congenital birth defects using the GBDI data, has implications for the ongoing neonatal mortality reduction activities in the country. The data indicate that activities to reduce neonatal mortality would be hampered unless the capacity to manage/treat infants with birth defects are addressed. Several congenital malformations can be surgically treated, provided skilled staff and facilities are available. The India Newborn Action plan has committed to addressing birth defects (Government of India 2014), and services for small and sick newborns have been put in place in several parts of the country. The RBSK programme in India has put in place free-of-cost services for common birth defects, but a mechanism to strengthen surgical services for neonates is yet to be clearly enunciated. This is in line with reports of a large unmet need for paediatric surgery for common congenital anomalies globally, but especially in LMICs (Higashi et al. 2015).
The observation that birth defect deaths were highest among children in the first year of life has implications for the public data from the RBSK. The RBSK reports birth defects among school-going children between the ages of 2 and 18 years, indicating that without data at birth, and in the first 2 years of life, RBSK data underestimate the number of birth defects in the country. Another observation from the study was the impact of neonatal mortality reduction activities, furthered by global agendas like the Millennium Development Goals and the Sustainable Development Goals. As mortality from common causes of infant deaths decrease, the proportion of deaths due to birth defects increase (Christianson et al. 2006). The analysis identified that compared with the larger reduction in mortality due to prematurity, intrapartum complications, and neonatal sepsis, reduction in the numbers of deaths due to birth defects was nearly negligible. These observations were in line with global (Hug et al. 2019; Liu et al. 2019) and Indian (India State-Level Disease Burden Initiative Child Mortality Collaborators 2020) data, which reported that there was very little decrease in the number of neonatal deaths caused by birth defects in India over one and a half decades. For specific types of birth defects, a similar relationship was observed. While there was a small decrease in rates between 1990 and 2017, the proportion of deaths as compared with all causes of deaths increased. This increase was not observed for two common birth defects, neural tube defects, and Down syndrome, and there was a marked decrease in the proportion of mortality associated with orofacial clefts between 1990 and 2017. These data might reflect increasing elective termination of pregnancy for neural tube defects, Down syndrome, and orofacial cleft.
Globally, data are reported as aggregated national statistics, but our analysis indicates that such aggregated data masks changes in the causes of child mortality occurring within countries. Analysis of causes of early neonatal mortality data by states/regions of India indicated the relevance of examining data by SDI regions. In over half the states of India, birth defects have emerged as the third leading cause of mortality, alerting health services for the need for initiating birth defects prevention and care services. This observation identifies the need for other LMICs to consider the analysis of desegregated data by SDI levels within the country. Such analysis would identify the areas within the country where birth defect services need to be implemented on a priority basis. From a health service perspective, birth defects services could be launched in a phased manner by regions with highest birth defect death rates. One of the observations of our study was excess female birth defect mortality. Whether this data is due to the skewed sex ratio of the country could not be determined. The data however suggests another health service responsibility, that of disability sensitisation, community awareness on services, and care for children with special health care needs.
Our study has certain limitations. The description of birth defects in this study is a reflection of the GBD data on congenital birth defects and does not include all conditions that can be classified as birth defects. Therefore, the data is likely to be an underestimate. In this context, it is relevant to note that the term “birth defects” is often used interchangeably with that of congenital anomalies (Modell et al. 2018). However, the World Health Organization describes birth defects as “any potential pathological condition arising before birth, whether evident at birth or manifesting later in life” (World Health Organization 2006). The latter definition expands the usage of the term birth defects to include a range of conditions including those caused by environmental agents, chromosomal and single gene disorders, in addition to congenital anomalies. The lack of consensus on the term birth defects has considerable public health implications, as without a working definition, it is difficult to measure the magnitude of these conditions. Another limitation of the GBD data is that GBD statistics do not include still births and terminations of pregnancy for foetal anomalies (TOPFA), which is another source of under-estimation (Boyle et al. 2018). Furthermore, another challenge of using GBD data is that they are frequently updated and archived data cannot be retrieved.
In conclusion, our study shows that in lieu of any other pan-country data, the GBD statistics remain the best available source to describe the epidemiology of birth defects in countries where surveillance systems are yet to be put in place. However, GBD data can in no way substitute for primary data collected through a robust birth defects surveillance system. Furthermore, for a country like India where elective termination of pregnancy for a congenital malformation is permitted, GBD data will be underestimated. However, for the current time, in lieu of a nationwide birth defects surveillance, the study identifies the magnitude of mortality caused by birth defects. The data urges the need to establish services and surveillance, so that birth defects can be prevented and neonatal mortality reduction targets can be improved. Importantly, the study illustrates how, within a country, birth defects emerge as a major cause of child deaths in more developed regions of the country, providing an opportunity for phased introduction of interventions.
Electronic supplementary material
(DOCX 26.1 kb)
Funding
The study was funded by the University Grants Commission-University with Potential for Excellence Holistic area “Translation research in the Health of Women and Children” to AK.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Bhide P, Kar A. A national estimate of the birth prevalence of congenital anomalies in India: systematic review and meta-analysis. BMC Pediatr. 2018;18(1):175. doi: 10.1186/s12887-018-1149-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhide P, Gund P, Kar A. Prevalence of congenital anomalies in an Indian maternal cohort: healthcare, prevention, and surveillance implications. PLoS One. 2016;11(11):e0166408. doi: 10.1371/journal.pone.0166408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle B, Addor MC, Arriola L, Barisic I, Bianchi F, Csáky-Szunyogh M, de Walle HEK, Dias CM, Draper E, Gatt M, Garne E, Haeusler M, Källén K, Latos-Bielenska A, McDonnell B, Mullaney C, Nelen V, Neville AJ, O’Mahony M, Queisser-Wahrendorf A, Randrianaivo H, Rankin J, Rissmann A, Ritvanen A, Rounding C, Tucker D, Verellen-Dumoulin C, Wellesley D, Wreyford B, Zymak-Zakutnia N, Dolk H. Estimating Global Burden of Disease due to congenital anomaly: an analysis of European data. Arch Dis Child Fetal Neonatal Ed. 2018;103(1):F22–F28. doi: 10.1136/archdischild-2016-311845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christianson A, Howson CP, Modell B. March of Dimes Global Report on Birth Defects: the hidden toll of dying and disabled children. White Plains: March of Dimes Birth Defects Foundation; 2006. [Google Scholar]
- Government of India (2019) National Health Profile 2019 14th issue. https://www.thehinducentre.com/resources/article29841374.ece/binary/8603321691572511495.pdf. Accessed 18 Nov 2019
- Government of India Ministry of Health and Family Welfare (2014) India Newborn Action Plan https://nhm.gov.in/images/pdf/programmes/inap-final.pdf. Accessed 6 August 2019
- Government of India Ministry of Health and Family Welfare (2019) Answers data of Rajya Sabha questions for session 240/year wise physical status Rashtriya Bal Swasthya Karyakram (RBSK) during 2014-15 and 2015-16. https://data.gov.in/node/3978901/download. Accessed 18 Nov 2019
- Government of India Ministry of Health and Family Welfare National Health Mission (2013) Rashtriya Bal Swasthya Karyakram A child health screening and early intervention services under NRHM, Ministry of Health and Family Welfare. http://nhm.gov.in/images/pdf/programmes/RBSK/Operational_Guidelines/Operational%20Guidelines_RBSK.pdf. Accessed 6 Aug 2019
- Higashi H, Barendregt JJ, Kassebaum NJ, Weiser TG, Bickler SW, Vos T. The burden of selected congenital anomalies amenable to surgery in low and middle-income regions: cleft lip and palate, congenital heart anomalies and neural tube defects. Arch Dis Child. 2015;100(3):233–238. doi: 10.1136/archdischild-2014-306175. [DOI] [PubMed] [Google Scholar]
- Hug L, Alexander M, You D, Alkema L, UN Inter-agency Group for Child Mortality Estimation National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Glob Health. 2019;7(6):e710–e720. doi: 10.1016/S2214-109X(19)30163-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- India State-Level Disease Burden Initiative Child Mortality Collaborators Subnational mapping of under-5 and neonatal mortality trends in India: the Global Burden of Disease Study 2000-17. Lancet. 2020;395(10237):1640–1658. doi: 10.1016/S0140-6736(20)30471-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation (2020) Protocol for the global burden of diseases, injuries, and risk factors study (GBD) Version 4.0; Issued March 2020 http://www.healthdata.org/sites/default/files/files/Projects/GBD/March2020_GBD%20Protocol_v4.pdf. Accessed 20 Mar 2020
- Institute for Health Metrics and Evaluation (IHME) (2018a) GBD Compare Data Visualization. IHME, University of Washington, Seattle http://vizhub.healthdata.org/gbd-compare. Accessed 9 May 2018
- Institute for Health Metrics and Evaluation (IHME) (2018b) GBD Results Tool. IHME, University of Washington, Seattle http://ghdx.healthdata.org/gbd-results-tool. Accessed 9 May 2018
- Institute for Health Metrics and Evaluation (IHME) (2018c) GBD India Compare VizHub. IHME, University of Washington, Seattle https://vizhub.healthdata.org/gbd-compare/india. Accessed 9 May 2018
- International Institute for Population Sciences (IIPS) and ICF . National Family Health Survey (NFHS-4), 2015–16. India. Mumbai: IIPS; 2017. [Google Scholar]
- Kar A, Radhakrishnan B, Girase T, Ujagare D, Patil A. Community-based screening and early intervention for birth defects and developmental disabilities: lessons from the RBSK programme in India. Disability, CBR & Inclusive Development. 2020;31(1):30–46. doi: 10.5463/dcid.v31i1.890. [DOI] [Google Scholar]
- Liu L, Chu Y, Oza S, Hogan D, Perin J, Bassani DG, Ram U, Fadel SA, Pandey A, Dhingra N, Sahu D, Kumar P, Cibulskis R, Wahl B, Shet A, Mathers C, Lawn J, Jha P, Kumar R, Black RE, Cousens S. National, regional, and state-level all-cause and cause-specific under-5 mortality in India in 2000–15: a systematic analysis with implications for the sustainable development goals. Lancet Glob Health. 2019;7(6):e721–e734. doi: 10.1016/S2214-109X(19)30080-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modell B, Darlison MW, Malherbe H, Moorthie S, Blencowe H, Mahaini R, el-Adawy M. Congenital disorders: epidemiological methods for answering calls for action. J Community Genet. 2018;9(4):335–340. doi: 10.1007/s12687-018-0390-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJ, Callender CS, Kulikoff XR, et al. Population and fertility by age and sex for 195 countries and territories, 1950–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1995–2051. doi: 10.1016/S0140-6736(18)32278-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagar R, Dandona R, Gururaj G, Dhaliwal RS, Singh A, Ferrari A, Dua T, Ganguli A, Varghese M, Chakma JK, Kumar GA, Shaji KS, Ambekar A, Rangaswamy T, Vijayakumar L, Agarwal V, Krishnankutty RP, Bhatia R, Charlson F, Chowdhary N, Erskine HE, Glenn SD, Krish V, Mantilla Herrera AM, Mutreja P, Odell CM, Pal PK, Prakash S, Santomauro D, Shukla DK, Singh R, Singh RKL, Thakur JS, ThekkePurakkal AS, Varghese CM, Reddy KS, Swaminathan S, Whiteford H, Bekedam HJ, Murray CJL, Vos T, Dandona L. The burden of mental disorders across the states of India: the Global Burden of Disease Study 1990–2017. Lancet Psychiatry. 2020;7(2):148–161. doi: 10.1016/S2215-0366(19)30475-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankar MJ, Neogi SB, Sharma J, Chauhan M, Srivastava R, Prabhakar PK, Khera A, Kumar R, Zodpey S, Paul VK. State of newborn health in India. J Perinatol. 2016;36(s3):S3–S8. doi: 10.1038/jp.2016.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Inter-agency Group for Child Mortality Estimation (UN IGME) (2017) Levels and trends in child mortality: Report 2017, Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation, United Nations Children’s Fund, New York, 2017 https://www.unicef.org/publications/files/Child_Mortality_Report_2017.pdf. Accessed July 09 2018
- World Health Organization, March of Dimes . Management of birth defects and haemoglobin disorders: report of a joint WHO-March of Dimes meeting, Geneva, Switzerland, 17–19 May 2006. Geneva: World Health Organization; 2006. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 26.1 kb)