Rheumatoid arthritis in the shoulder can lead to significant rotator cuff tears, glenohumeral arthritis, and eventually, a scenario consistent with cuff tear arthropathy. Several case reports have previously shown that massive rotator cuff tears and cuff tear arthropathy can lead to large cysts extending from the subacromial space through the acromioclavicular joint into a subcutaneous cyst, with a characteristic “geyser sign” on imaging.2,3,9,11,13,14 A single study has reported extension into the trapezius, but extension through the deltoid has not been reported.7
In 1993, Grammont and Baulot, in their series on reverse shoulder arthroplasty (RSA) for cuff-deficient shoulders, argued that the deltoid could compensate for cuff deficiency in the biomechanical setting of an RSA.6 Deltoid deficiency has long been considered a contraindication to RSA, as the deltoid is the primary driver of shoulder elevation postoperatively. Proper functioning of an RSA in cuff-deficient shoulders is predicated on an intact deltoid.6 Dysfunction, tears, or defects of the deltoid can lead to poor function, poor forward elevation, or even instability.1,8 Over time, some reports have started to emerge on repair or reconstruction of deltoid deficiency in patients undergoing RSA, leading to good outcomes.4,5,10
We present the case of a synovial cyst in a patient with cuff tear arthropathy and rheumatoid arthritis, with extension from the subacromial space through the middle head of the deltoid and into the subcutaneous tissue, leaving a large defect in the deltoid. The patient was scheduled to undergo RSA, as well as concomitant cyst excision, repair of the deltoid defect, and possible allograft augmentation or deltoid rotationplasty if necessary. Given the importance of the deltoid for the function of an RSA, as well as the importance of the wrapping or compressive effect of the deltoid on the humerus to prevent instability,12 we were concerned that a defect would allow the humerus to buttonhole through the deltoid, leading to weakness and/or instability. As a result, we considered it critical to excise the cyst and securely restore the integrity of the middle deltoid.
Case description
The patient was a 58-year-old female patient with end-stage cuff tear arthropathy of the right shoulder. She had widespread rheumatoid arthritis, with multiple sites of involvement. Because of significant side effects of her antirheumatic medications and because widespread end-stage degeneration still developed while she was taking them, she decided to stop taking the antirheumatic medications several years ago.
The patient presented with significant shoulder pain and dysfunction and was unable to perform many activities of daily living. Conservative treatments including activity modification, corticosteroid injections, and oral analgesics had failed. Her range of motion was as follows: forward elevation, 30° actively and 95° passively; external rotation at the side, 15°; and internal rotation to the back pocket. She had significant pain and crepitus with any attempts at range of motion.
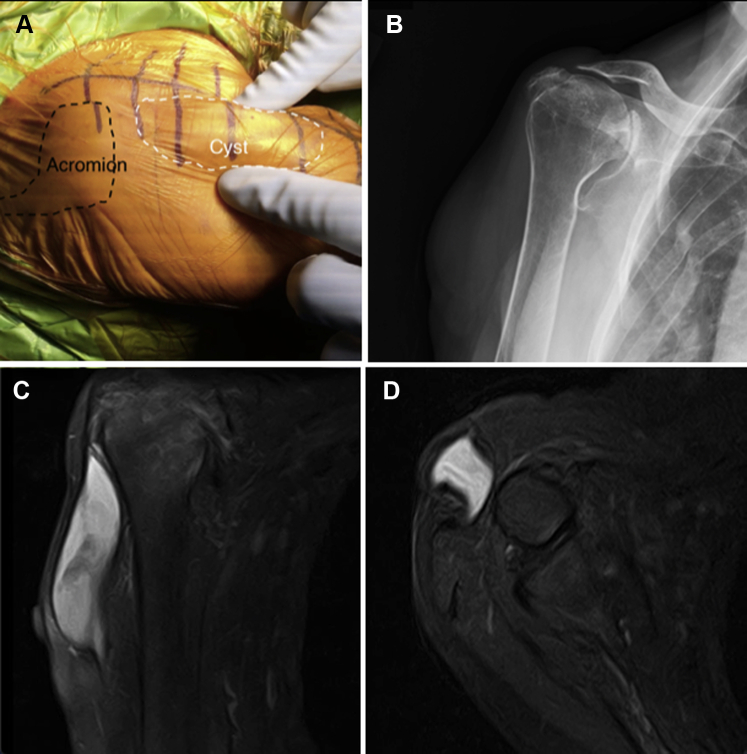
There was a palpable and visible soft-tissue mass on the anterolateral aspect of the shoulder, clinically measuring 7 × 2 × 2 cm (Fig. 1, A). It was soft and mobile, overlying the anterolateral deltoid. There were no overlying skin changes. The patient had normal function in the axillary nerve, including normal sensation in the lateral shoulder and intact function to all 3 heads of the deltoid.
Figure 1.
Trans-deltoid synovial cyst. (A) A photograph of the patient in the semi–beach-chair position shows the outlined acromion (black dashed line) and outlined cyst (white dashed line). The mass was visible and palpable through the middle head of the deltoid. (B) Preoperative Grashey radiograph showing severe cuff tear arthropathy with significant superior erosion, a Sirveaux type E2 deformity, and 27° of superior inclination. (C) Coronal image showing the communication of the subcutaneous fluid-filled cyst with the subacromial space, as well as the craniocaudal extension of the cyst. (D) Axial image at the level of the glenoid showing the trans-deltoid communication of the cyst through the middle head of the deltoid.
The patient’s radiographs revealed end-stage cuff tear arthropathy, with a severe Sirveaux type E2 pattern of superior wear and 27° of inclination, with a small portion of intact glenoid inferiorly (Fig. 1, B). We planned to perform an RSA with autologous humeral head bone grafting to the glenoid, as well as removal of the mass. The patient underwent a computed tomography scan for preoperative planning for the glenoid component and a magnetic resonance imaging (MRI) scan for evaluation of the mass.
The MRI scan revealed a fluid-filled synovial cyst extending from the subacromial space through the middle head of the deltoid, with a 4 × 1–cm defect in the muscle belly (Fig. 1, C and D). The 1-cm deltoid defect was in an anterior-posterior orientation. The cyst appeared to have undergone septation into 2 parts, the first measuring 8 × 3 × 2 cm and the second, immediately adjacent, measuring 2 × 2 × 1 cm. There also appeared to be some early detachment of the adjacent segments of the middle deltoid away from the acromion. We obtained the patient’s consent to perform excision of the cyst and repair of the deltoid. Given the middle deltoid’s importance in RSA, we planned to possibly augment the repair with human dermal allograft if repair to the acromion was necessary. If primary repair was not possible, we planned to perform a deltoid rotationplasty to restore the integrity of the middle head of the deltoid.10
To reach the cyst and perform the arthroplasty through the same incision, we made a longer-than-usual incision for a deltopectoral approach and began more laterally at the acromioclavicular joint, rather than at the tip of the coracoid. We made full-thickness skin flaps medially to the fat stripe of the deltopectoral interval and laterally to the cyst. The cyst was dissected circumferentially away from the adjacent deltoid musculature (Fig. 2, A). The distal aspect of the cyst did not penetrate the bursal side of the deltoid; therefore, we decided not to identify the axillary nerve. When the cyst wall was inadvertently breached, there was egress of yellow, thick, opaque material (Fig. 2, B). To rule out infection, this was submitted to an intraoperative gram stain, which showed negative findings for organisms, and frozen section, which showed results consistent with chronic inflammation within the cyst wall and caseous material within the cyst. The specimen is shown in Figure 2, C. Final culture results, including a 14-day hold, were negative, and permanent pathologic analysis revealed an inflammatory pseudocyst with granulomatous inflammation, multinucleated giant cell reaction, and dystrophic calcification, consistent with a rheumatoid nodule.
Figure 2.
Exposed cyst. (A) Intraoperative photograph of the exposed cyst (white dashed line) and the adjacent anterior (∗) and middle (∗∗) portions of the deltoid. (B) Intraoperative photograph showing the caseous material expressed from the cyst. An intraoperative gram stain showed negative findings, and frozen section showed chronic inflammation and caseous necrosis. The results of the final cultures and permanent pathologic analysis were consistent with the intraoperative findings. (C) Intraoperative photograph showing the excised cyst, demonstrating the long craniocaudal extension.
The resulting defect demonstrated that the deltoid was attached to the acromion, and the defect was amenable to side-to-side repair (Fig. 3, A). This was performed using No. 2-0 FiberWire (Arthrex, Naples, FL, USA) in a figure-of-8 fashion with the knots buried beneath the fascia. The defect was reinforced with a running-locking No. 0 Vicryl suture (Ethicon, Somerville, NJ, USA) to seal the repair site (Fig. 3, B).
Figure 3.
Deltoid defect after cyst excision and repair. (A) Intraoperative photograph showing the residual defect (white dashed line) within the middle head of the deltoid after excision of the cyst. ∗Anterior deltoid. ∗∗Middle deltoid. (B) The defect was repaired in a side-to-side manner (white dashed line) using multiple interrupted No. 2-0 FiberWire sutures with the knots buried beneath the fascia. The defect was further reinforced and sealed using a running-locking No. 0 Vicryl suture to minimize the risk of recurrence and to seal off the subcutaneous space from the deep joint space. ∗Anterior deltoid. ∗∗Middle deltoid.
The arthroplasty then proceeded as planned. The humeral head was cut and shaped to fit the glenoid defect and was placed beneath the baseplate. We placed an additional partially threaded cancellous screw and washer above the baseplate to further secure the graft (Fig. 4).
Figure 4.

Postoperative Grashey radiograph showing reverse shoulder arthroplasty with an additional screw and washer superiorly to secure the humeral head bone graft.
Because of the deltoid repair, the structural bone grafting, and the significant osteopenia, the patient was placed in an abduction sling (Slingshot 2; Breg, Carlsbad, CA, USA) for 6 weeks. Passive motion ensued from weeks 6-12, and active motion and progressive strengthening started at 12 weeks.
At 2 years after surgery, there was no recurrence of the cyst, and the deltoid defect was intact by palpation. The patient regained 130° of forward elevation and 30° of external rotation at the side and could internally rotate to L1.
Discussion
This case represents an important variation of synovial cyst formation that can occur with massive rotator cuff tears or cuff tear arthropathy. Previous reports have discussed large cysts extending from the subacromial space through the acromioclavicular joint into the subcutaneous cyst. In these prior reports, the acromioclavicular joint cysts were managed with a combination of cyst excision, distal clavicle resection, rotator cuff repair, and/or RSA. The subcutaneous location of the cyst, superior to the acromioclavicular joint, in prior reports has not compromised the integrity of the deltoid muscle, which is pivotal to a successful outcome following an RSA. Our case is unique in the fact that the cyst had penetrated through the middle head of the deltoid and the resultant defect in a patient undergoing RSA requires a different approach than previously reported cysts that penetrated the acromioclavicular joint. Proper functioning of an RSA in cuff-deficient shoulders is predicated on an intact deltoid.6 Dysfunction, tears, or defects of the deltoid can lead to poor function, poor forward elevation, or even instability.1,8 In addition, complete repair or reconstruction of the deltoid was necessary to prevent cyst recurrence and communication of the subcutaneous tissue with the deep joint space.
As a result, we decided to excise the cyst and, if possible, directly repair any deltoid defect. If the deltoid had some detachment off of the acromion, as the MRI scan suggested, we planned to primarily repair this defect and augment with human dermal allograft. If the deltoid tear was not amenable to direct repair, we prepared to reconstruct the defect using a deltoid rotationplasty to restore the integrity of the middle deltoid.5,10
In this situation, because the defect was only a side-to-side defect, without detachment from the acromion, we performed a side-to-side repair. Moreover, rather than having the patient begin immediate passive range of motion, we placed her in an abduction sling and slowed down the usual rehabilitation regimen to begin passive range of motion at 6 weeks.
This case also highlights the fact that the integrity of the deltoid should not be assumed, particularly in an individual undergoing RSA. In our patient, the cyst was immediately apparent on visual inspection because of her thin stature (body mass index, 17.2 kg/m2), but this may not have been so apparent in a larger individual. This patient, in particular, had a long history of rheumatoid arthritis and had foregone antirheumatic medications for many years because of their side effects. The inflammatory disease, not surprisingly, led to end-stage cuff tear arthropathy, as well as extensive synovitis, that eventually eroded the deltoid and led to a synovial cyst. Therefore, in patients with severe inflammatory disease who present with rotator cuff arthropathy and a large soft-tissue mass overlying the deltoid muscle, the clinician should consider the possibility of a trans-deltoid synovial cyst and obtain an MRI scan for further diagnostic workup. Failure to recognize this may have led to less-than-ideal function or possibly instability.
Conclusion
The integrity of the deltoid should be directly examined and evaluated in each patient undergoing RSA and should not be assumed. The clinician should be aware of this entity, the trans-deltoid synovial cyst, and should be prepared to excise the cyst and repair the deltoid to maximize the function of the RSA and to prevent instability if the wrapping or compressive force of the deltoid on the humerus is lost. As long as it is recognized preoperatively, management of the cyst and repair of the deltoid can lead to a good functional outcome without instability and this entity need not be a contraindication to RSA.
Disclaimer
Michael H. Amini has received consultant payments from Stryker, which are related to the subject of this work. The other author, his immediate family, and any research foundation with which he is affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
References
- 1.Abdelfattah A., Otto R.J., Simon P., Christmas K.N., Tanner G., LaMartina J., II Classification of instability after reverse shoulder arthroplasty guides surgical management and outcomes. J Shoulder Elbow Surg. 2018;27:E107–E118. doi: 10.1016/j.jse.2017.09.031. [DOI] [PubMed] [Google Scholar]
- 2.Cooper H.J., Milillo R., Klein D.A., DiFelice G.S. The MRI geyser sign: acromioclavicular joint cysts in the setting of a chronic rotator cuff tear. Am J Orthop (Belle Mead NJ) 2011;40:E118–E121. [PubMed] [Google Scholar]
- 3.Craig E.V. The acromioclavicular joint cyst. An unusual presentation of a rotator cuff tear. Clin Orthop Relat Res. 1986;202:189–192. [PubMed] [Google Scholar]
- 4.Elhassan B.T., Wagner E.R., Werthel J.D., Lehanneur M., Lee J. Outcome of reverse shoulder arthroplasty with pedicled pectoralis transfer in patients with deltoid paralysis. J Shoulder Elbow Surg. 2018;27:96–103. doi: 10.1016/j.jse.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Garofalo R., Flanagin B., Castagna A., Calvisi V., Krishnan S.G. Massive irreparable rotator cuff tear and associated deltoid tear. Does the reverse shoulder arthroplasty and deltoid repair be a possible option of treatment? J Orthop Sci. 2016;21:753–758. doi: 10.1016/j.jos.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 6.Grammont P.M., Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–68. doi: 10.3928/0147-7447-19930101-11. [DOI] [PubMed] [Google Scholar]
- 7.Griesser M.J., Harris J.D., Jones G.L. Intramuscular synovial cyst of the shoulder. Am J Orthop (Belle Mead NJ) 2011;40:E198–E201. [PubMed] [Google Scholar]
- 8.Lädermann A., Walch G., Denard P.J., Collin P., Sirveaux F., Favard L. Reverse shoulder arthroplasty in patients with pre-operative impairment of the deltoid muscle. Bone Joint J. 2013;95-B:1106–1113. doi: 10.1302/0301-620X.95B8.31173. [DOI] [PubMed] [Google Scholar]
- 9.Lizaur Utrilla A., Marco Gomez L., Perez Aznar A., Cebrian Gomez R. Rotator cuff tear and acromioclavicular joint cyst. Acta Orthop Belg. 1995;61:144–146. [PubMed] [Google Scholar]
- 10.Marinello P.G., Amini M.H., Peers S., O'Donnell J., Iannotti J.P. Reverse total shoulder arthroplasty with combined deltoid reconstruction in patients with anterior and/or middle deltoid tears. J Shoulder Elbow Surg. 2016;25:936–941. doi: 10.1016/j.jse.2015.10.026. [DOI] [PubMed] [Google Scholar]
- 11.Postacchini F., Perugia D., Gumina S. Acromioclavicular joint cyst associated with rotator cuff tear. A report of three cases. Clin Orthop Relat Res. 1993;294:111–113. [PubMed] [Google Scholar]
- 12.Routman H.D., Flurin P.H., Wright T.W., Zuckerman J.D., Hamilton M.A., Roche C.P. Reverse shoulder arthroplasty prosthesis design classification system. Bull Hosp Jt Dis (2013) 2015;73(Suppl 1):S5–S14. [PubMed] [Google Scholar]
- 13.Selvi E., De Stefano R., Frati E., Manganelli S., Manca S., Marcolongo R. Rotator cuff tear associated with an acromioclavicular cyst in rheumatoid arthritis. Clin Rheumatol. 1998;17:170–171. doi: 10.1007/BF01452269. [DOI] [PubMed] [Google Scholar]
- 14.Tshering Vogel D.W., Steinbach L.S., Hertel R., Bernhard J., Stauffer E., Anderson S.E. Acromioclavicular joint cyst: nine cases of a pseudotumor of the shoulder. Skeletal Radiol. 2005;34:260–265. doi: 10.1007/s00256-004-0883-6. [DOI] [PubMed] [Google Scholar]