Abstract
Background
Globally, reverse shoulder arthroplasty (RSA) has moved away from the Grammont design to modern prosthesis designs. The purpose of this study was to provide a focused, updated systematic review for each of the most common complications of RSA by limiting each search to publications after 2010. In this part II, the following were examined: (1) instability, (2) humerus/glenoid fracture, (3) acromial/scapular spine fractures (AF/SSF), and (4) problems/miscellaneous.
Methods
Four separate PubMed database searches were performed following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Overall, 137 studies for instability, 94 for humerus/glenoid fracture, 120 for AF/SSF, and 74 for problems/miscellaneous were included in each review, respectively. Univariate analysis was performed with chi-square and Fisher exact tests.
Results
The Grammont design had a higher instability rate vs. all other designs combined (4.0%, 1.3%; P < .001), and the onlay humerus design had a lower rate than the lateralized glenoid design (0.9%, 2.0%; P = .02). The rate for intraoperative humerus fracture was 1.8%; intraoperative glenoid fracture, 0.3%; postoperative humerus fracture, 1.2%; and postoperative glenoid fracture, 0.1%. The rate of AF/SSF was 2.6% (371/14235). The rate for complex regional pain syndrome was 0.4%; deltoid injury, 0.1%; hematoma, 0.3%; and heterotopic ossification, 0.8%.
Conclusions
Focused systematic reviews of recent literature with a large volume of shoulders demonstrate that using non-Grammont modern prosthesis designs, complications including instability, intraoperative humerus and glenoid fractures, and hematoma are significantly reduced compared with previous studies. As the indications continue to expand for RSA, it is imperative to accurately track the rate and types of complications in order to justify its cost and increased indications.
Keywords: Reverse shoulder arthroplasty, complications, instability, humeral fracture, glenoid fracture, acromial fracture, heterotopic ossification
Although initially indicated for patients with rotator cuff arthropathy,18,89 reverse shoulder arthroplasty (RSA) indications have recently expanded to include osteoarthritis with an intact rotator cuff286 as well as tumor resection, postinfectious sequelae,57 chronic dislocations, and revisions of failed arthroplasties.24 RSA is frequently used to treat difficult clinical diagnoses; consequently, it is not surprising to see a relatively high complication rate. Reports have concluded that indications such as rheumatoid arthritis have a higher risk of intraoperative and postoperative fracture290 and that prior nonarthroplasty shoulder surgery confers a higher complication rate post RSA compared with those with no prior surgery on the ipsilateral shoulder.76
The use of RSA has continued to rise, and it has become the majority shoulder arthroplasty since 2016. It has had an even more profound effect on revision shoulder arthroplasty than what previously has been documented in the primary setting.263 Thus, precise knowledge of the probability and implications of the various complications are imperative for judicious use of RSA.70 Complications have been well described; the studies in the literature, however, are heterogeneous (eg, different indications, different prostheses, and different populations) and definitions vary between authors.39,293 The reported complication rate is variable among reports and seems to be influenced substantially by the mix of primary and revision procedures included in each study.214 Patient factors including smoking status,104 diabetes,159 Parkinson disease,33 and preoperative American Society of Anesthesiologists score121 have all been linked to increased complications and/or unfavorable outcomes. Some advocate that primary shoulder arthroplasty is performed more efficiently by higher-volume surgeons,235 and complications have been reported to decrease with surgeon experience.269 Recent data have defined a volume-outcome relationship where, likely related to surgical experience, ancillary staff familiarity, and protocolized pathways, hospital surgical volumes of 54-70 RSAs/yr correlate with the highest outcomes.69
The majority of the published studies on RSA have historically reported on a Grammont-style RSA (glenosphere with medialized center of rotation [MG] along with an inlay humeral component that medializes the humerus [MH]). Lessons learned using this style of prosthesis have led to the introduction of new designs with multiple options for glenosphere lateral offset and eccentricity, different neck-shaft angulations, and humeral-based lateralization (LH). These design modifications translate into different biomechanics compared with the first generation of RSA. As the concept, design, and surgical technique of RSA continue to improve, the rates and types of complications may change over time. One study noted that after implant modifications, there have been statistically significant declines in baseplate failure, humeral dissociation, and glenosphere dissociation.240 Further, a recent study noted that primary RSA performed with contemporary implants and surgical techniques seems to be associated with a very low rate of reoperation.126
As the indications and use of RSA continue to expand, it is important to track the rate and types of complication as the procedure continues to develop over time. The purpose of this 2-part study was to provide a focused systematic review for the most common complications of RSA using contemporary prosthetic designs, therefore limiting studies to those published after 2010. In this part II, a systematic review was performed for (1) instability, (2) humerus/glenoid fracture, (3) acromial/scapular spine fractures, and (4) problems/miscellaneous. We established a study design and specific objectives before commencing each literature research.
Instability
Methods
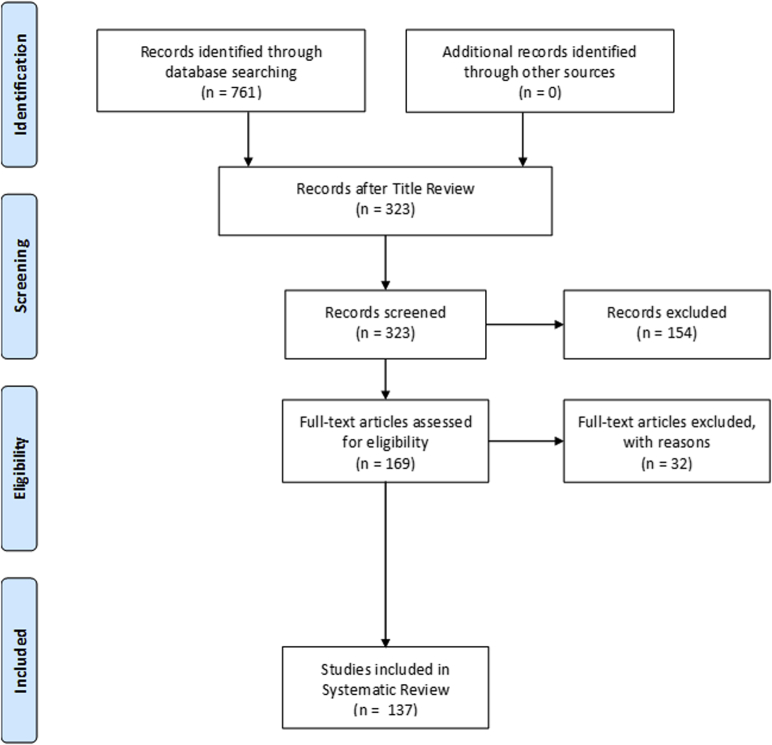
A systematic review was performed using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.180 The search was performed using the PubMed medical database in April 2020 (Fig. 1). The search terms used were [(Dislocation) OR (Instability) OR (Revision) OR (Reoperation) OR (Complication) AND (reverse shoulder arthroplasty) OR (reverse total shoulder) OR (reverse total shoulder arthroplasty)] with filters as follows: date range (1/1/2010 to 12/31/2019), species (human), and language (English). The search resulted in 761 total titles. Inclusion criteria were titles that specified primary or revision RSA. Exclusion criteria were duplicate titles, review articles, editorials, technique articles without reported patient outcomes, cadaveric studies, kinematic/finite element model/computer model analyses, case reports, survey studies, elastography/histologic studies, cost-benefit analyses, and instructional course lecture articles. After application of these criteria, 323 titles remained for abstract review. Articles that reported 2-year follow-up studies with clearly reported instability, reoperation, revision, or complication data were included. Articles with <15 patients, a minimum average follow-up of <24 months, and evaluated treatment of shoulder periprosthetic infection, blood transfusion rates, venous thromboembolism rates, RSA with concomitant tendon transfer, or RSA for tumor were excluded. This process eliminated 154 more articles, leaving 169 for full-text review. Articles with repeat data from publications prior to 2010 without further instability on long-term follow-up were also excluded in the full-text review. Definition of instability/dislocation was left to the discretion of each individual study. This final elimination stage resulted in 137 articles for inclusion in the analysis. Two authors (A.M.R. and S.S.S.) reviewed the articles and collected the data.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram for instability.
The rates of instability overall and according to (1) revision status (primary vs. revision arthroplasty vs. failed open reduction internal fixation [ORIF] proximal humerus fracture [PHF]), (2) publication date (2010-2016 vs. 2017-2020), (3) diagnosis, (4) center of rotation (CoR) (medialized vs. lateralized), and (5) prosthesis design were determined by pooled statistics. CoR and prosthesis design was defined according to Routman et al,210 who stated that a glenosphere with a CoR of ≤5 mm to the glenoid face is considered an MG, and a glenosphere with a CoR >5 mm lateral to the glenoid face is considered a lateralized glenoid (LG). Comparisons were also made to Zumstein et al.293
Statistical analysis was performed using SPSS (version 26; IBM Corp., Armonk, NY, USA). Univariate analysis was performed with the chi-square test, or with Fisher exact test when the expected count for at least 1 cell in the comparison was less than 5. The alpha level for statistical significance was set to 0.05.
Results
The majority of the studies were Level IV (96) and III (37), with only 3 Level II and 1 Level I evidence studies.∗ A total of 9306 shoulders were included in the analysis with a mean age of 72.1 years and 69.0% of female sex. The overall instability rate was 3.3% (308/9306 shoulders) at a mean follow-up of 3.2 years. When stratified by reoperations required and time to instability, 73.5% of dislocations required revision of components and 59.5% of shoulders with instability occurred within the first 90 days postoperatively (Table I). In total, there were 20 different implant systems encountered. Primary RSA instability rates were significantly lower at 2.5% vs. revision RSA (5.7%) or RSA for failed ORIF PHF rates (5.3%) (P < .001, P = .01, respectively) (Table II). The Grammont design (MG/MH) had a significantly higher instability rate vs. all other designs combined (4.0%, 1.3%; P < .001). Instability rates, especially modern non-Grammont designs, have significantly decreased compared with Zumstein et al293 (Table III).
Table I.
Instability rates overall, stratified by reoperations required and time to instability
| Studies included | Shoulders | Instability present | Rate, % (n/n) | |
|---|---|---|---|---|
| Overall | 137 | 9306 | 308 | 33 (308/9306) |
| Stratified by reoperations | 127 | 6620 | 226 | — |
| Revision of components | — | — | 166 | 73.5 (166/226) |
| Closed reduction | — | — | 41 | 18.1 (41/226) |
| Open reduction | — | — | 1 | 0.4 (1/226) |
| Stratified by time to instability | 32 | 1712 | 84 | — |
| <90 d | — | — | 50 | 59.5 (50/84) |
| >90 d | — | — | 34 | 40.5 (34/84) |
The majority of shoulders with instability occurred within the first 90 days postoperatively and were treated with revision of components as final treatment.
Table II.
Rates of instability according to (1) publication date (2010-2016 vs. 2017-2020), (2) revision status (primary vs. revision arthroplasty vs. failed ORIF PHF), and (3) center of rotation
| Studies included | Shoulders | Instability present | Rate, % | P value | |
|---|---|---|---|---|---|
| Year published | |||||
| 2010-2016 | 68 | 4638 | 165 | 3.6 | .18 |
| 2017-2020 | 69 | 4668 | 143 | 3.1 | — |
| Primary vs. revision | |||||
| Primary RSA | 86 | 6607 | 168 | 2.5 | <.001 vs. revision; .01 vs. ORIF |
| Revision arthroplasty | 37 | 1404 | 80 | 5.7 | .81 vs. ORIF |
| Failed ORIF PHF | 9 | 226 | 12 | 5.3 | — |
| Center of rotation | |||||
| Medialized | 88 | 4950 | 141 | 2.8 | .15 |
| Lateralized | 22 | 1065 | 22 | 2.1 | — |
ORIF, open reduction internal fixation; PHF, proximal humerus fracture; RSA, reverse shoulder arthroplasty.
Primary RSA had significantly lower instability rates compared to both revision and failed ORIF PHF.
Table III.
Rates of instability according to diagnosis and prosthesis design
| Studies included | Shoulders | Instability present | Rate, % | P value | |
|---|---|---|---|---|---|
| Diagnosis | |||||
| Cuff tear arthropathy | 15 | 905 | 21 | 2.3 | .02 vs. PHF; <.001 vs. failed arthroplasty |
| PHF | 36 | 1654 | 67 | 4.1 | .03 vs. failed arthroplasty |
| Failed arthroplasty | 29 | 1243 | 72 | 5.8 | .62∗ vs. instability arthropathy |
| Instability arthropathy | 4 | 80 | 3 | 3.8 | >.99∗ vs. PHF; .44∗ vs. CTA |
| Prothesis design | |||||
| LG/MH | 22 | 1021 | 20 | 2.0 | .02 vs. MG/LH |
| MG/LH | 16 | 1888 | 17 | 0.9 | .02 vs. LG/MH |
| LG/LH | 1 | 45 | 2 | 4.4 | — |
| Subtotal | 39 | 2954 | 39 | 1.3 | <.001 vs. MG/MH |
| MG/MH | 73 | 2932 | 116 | 4.0 | — |
| Author | P value vs. Zumstein et al | ||||
| Zumstein et al | 21 | 782 | 37 | 4.7 | — |
| Current study | 137 | 9303 | 308 | 3.3 | .04 |
| Current study: subtotal of non-Grammont designs | 39 | 2954 | 39 | 1.3 | <.001 |
PHF, proximal humerus fracture; LG, lateralized glenoid; MH, medialized humerus; MG, medialized glenoid; LH, lateralized humerus; CTA, cuff tear arthropathy; JSES, Journal of Shoulder and Elbow Surgery.
The Grammont design (MG/MH) had a significantly higher instability rate vs. all other designs combined (4.0%, 1.3%; P < .001), instability rates, especially modern non-Grammont designs, have significantly decreased compared to Zumstein et al (JSES, 2011).
Bold indicates statistical significance (P < .05).
Fisher exact test.
Humerus/glenoid fracture
Methods
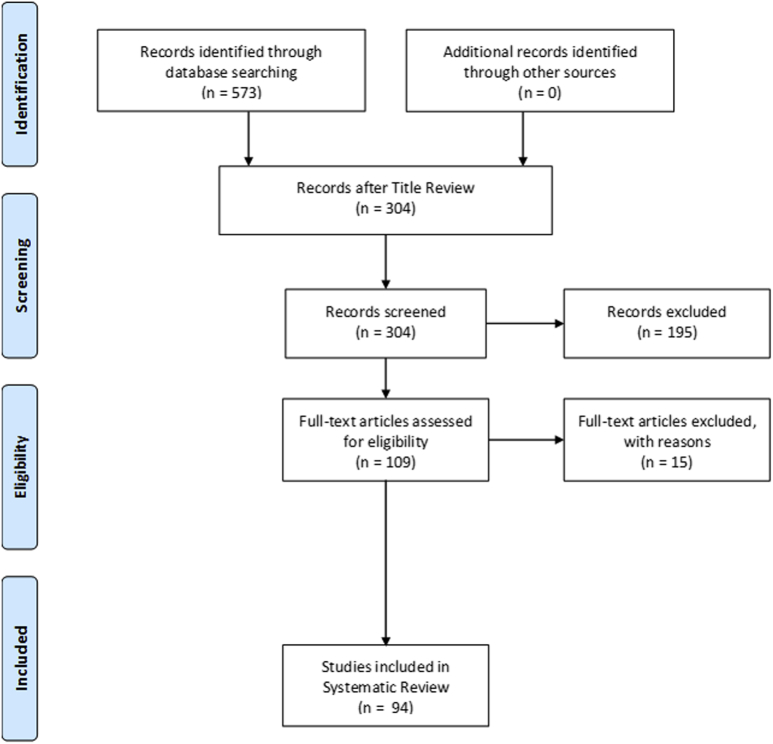
A systematic review was performed using PRISMA guidelines.180 The search was performed using the PubMed medical database in July 2019 (Fig. 2). The search terms used were [(perioperative complication) OR (Complication) OR (Humerus fracture) OR (Glenoid Fracture) OR (Fracture) OR (Intraoperative fracture) OR (postoperative fracture) OR (revision) OR (reoperation)] AND [(reverse shoulder arthroplasty) OR (reverse total shoulder) OR (reverse total shoulder arthroplasty)] with filters as follows: date range (1/1/2010 to 5/1/2019), species (human), and language (English). The search resulted in 573 total titles. Inclusion criteria were titles that specified primary or revision RSA. Exclusion criteria were duplicate titles, review articles, editorials, technique articles without reported patient outcomes, cadaveric studies, kinematic/finite element model/computer model analyses, case reports, survey studies, elastography/histologic studies, cost-benefit analyses, and instructional course lecture articles. After application of these criteria, 304 titles remained for abstract review. Articles that reported 2-year follow-up studies with perioperative complication data, postoperative complication data, or clearly reported humerus fracture, glenoid fracture, intraoperative fracture, and postoperative fracture were lincluded. Articles with <25 patients, a minimum average follow-up of <24 months, and evaluated treatment of shoulder periprosthetic infection, blood transfusion rates, venous thromboembolism rates, RSA with concomitant tendon transfer, or RSA for tumor were excluded. This process eliminated 195 more articles, leaving 109 for full-text review. Definition of glenoid/humerus fracture was left to the discretion of each individual study. This final elimination stage resulted in 94 articles for inclusion in the analysis. Two authors (B.G. and S.S.S.) reviewed the articles and collected the data.
Figure 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram for humerus/glenoid fracture.
The rates of intraoperative humerus fracture (IHF), intraoperative glenoid fracture (IGF), postoperative humerus fracture (PostHF), postoperative glenoid fracture (PGF), overall and according to (1) diagnosis and (2) prosthesis design were determined by pooled statistics. Prosthesis design was defined according to Routman et al.210 Comparisons were also made to Zumstein et al.293
Statistical analysis was performed using SPSS (version 26). Univariate analysis was performed with the chi-square test, or with Fisher exact test when the expected count for at least 1 cell in the comparison was less than 5. The alpha level for statistical significance was set to 0.05.
Results
The vast majority of the studies were Level IV and III evidence studies.† A total of 5539 shoulders were included in the analysis with a mean age of 71.3 years and 67.4% of female sex at a mean follow-up of 3.5 years. The overall rate was as follows: IHF = 1.8% (91/5539 shoulders), IGF = 0.3% (15/5539), PostHF = 1.2% (69/5539), and PGF = 0.1% (6/5539). In total, there were 20 different implant systems encountered. IGF and IHF rates using modern non-Grammont designs have significantly decreased compared with Zumstein et al (Table IV). Additionally, 62.7% of the postoperative fractures were attributed to traumatic events. When stratified by management, the majority of IHF and IGF were treated conservatively (Table V).
Table IV.
Fracture rates overall and compared to Zumstein et al
| Studies included | Shoulders | Fx present | Rate, % | P value | |
|---|---|---|---|---|---|
| Current study | Vs. Zumstein et al | ||||
| Intraop. humerus Fx | 94 | 5539 | 97 | 1.8 | .56 |
| Intraop. glenoid Fx | 94 | 5539 | 15 | 0.3 | .01∗ |
| Postop. humerus Fx | 94 | 5539 | 69 | 1.2 | .71 |
| Postop. glenoid Fx | 94 | 5539 | 6 | 0.1 | — |
| Zumstein et al | Vs. current study | ||||
| Intraop. humerus Fx | 21 | 782 | 16 | 2.0 | .56 |
| Intraop. glenoid Fx | 21 | 782 | 7 | 0.9 | .01∗ |
| Postop. humerus Fx | 21 | 782 | 11 | 1.4 | .71 |
| Postop. glenoid Fx | 21 | 782 | NR | NR | — |
| Current study: subtotal of non-Grammont designs | Vs. Zumstein et al | ||||
| Intraop. humerus Fx | 1057 | 0 | 0.0 | <.001 | |
| Intraop. glenoid Fx | 1057 | 1 | 0.1 | .01∗ | |
| Postop. humerus Fx | 1057 | 23 | 2.2 | .23 | |
| Postop. glenoid Fx | 1057 | 1 | 0.1 | — | |
Intraop, intraoperatively; Postop., postoperatively; Fx, fracture; NR, not reported; JSES, Journal of Shoulder and Elbow Surgery.
Intraoperative glenoid fracture rates and intraoperative humerus fracture using modern non-Grammont designs have significantly decreased compared with Zumstein et al (JSES, 2011).
Bold indicates statistical significance (P < .05).
Table V.
Number of fractures treated conservatively and fracture rates stratified by diagnosis and prosthesis design
| Number of Fx treated conservatively | Rate, % (n/n) | |||
|---|---|---|---|---|
| Intraop. humerus Fx | 52 | 53.6 (52/97) | ||
| Intraop. glenoid Fx | 10 | 66.7 (10/15) | ||
| Postop. humerus Fx | 25 | 36.2 (25/69) | ||
| Postop. glenoid Fx |
3 |
50 (3/6) |
||
| Diagnosis |
CTA |
RCT |
PHF |
Failed arthroplasty |
| Shoulders | 990 | 247 | 1443 | 1290 |
| Intraop. humerus Fx | 0.3 (3/990) | 0 (0/247) | 0.8 (11/1443) | 5.5 (71/1290)∗ |
| Intraop. glenoid Fx | 0.3 (3/990) | 0 (0/247) | 0.1 (2/1443) | 0.2 (3/1290) |
| Postop. humerus Fx | 0.2 (2/990) | 0.8 (2/247) | 0.5 (7/1443) | 2.6 (33/1290)† |
| Postop. glenoid Fx |
0.2 (2/990) |
0 (0/247) |
0 (0/1443) |
0 (0/1290) |
| Prosthesis design |
LG/MH |
MG/LH |
LG/LH |
MG/MH |
| Shoulders | 711 | 318 | 28 | 2839 |
| Intraop. humerus Fx | 0 (0/711) | 0 (0/318) | 0 (0/28) | 1.6 (46/2839)‡ |
| Intraop. glenoid Fx | 0 (0/711) | 0.3 (1/318) | 0 (0/28) | 0.1 (3/2839) |
| Postop. humerus Fx | 2.1 (15/711) | 2.5 (8/318) | 0 (0/28) | 1.1 (31/2839)§ |
| Postop. glenoid Fx | 0 (0/711) | 0.3 (1/318) | 0 (0/28) | 0.2 (5/2839) |
Intraop., intraoperatively; Postop., postoperatively; Fx, fracture; CTA, cuff tear arthropathy; RCT, rotator cuff tear; PHF, proximal humerus fracture; LG, lateralized glenoid; MH, medialized humerus; MG, medialized glenoid; LH, lateralized humerus.
P < .001 vs. CTA; P < .001 vs. RCT; P < .001 vs. PHF.
P < .001 vs. CTA; P = .09 vs. RCT; P < .001 vs. PHF.
P = .001 vs. LG/MH.
P = .03 vs. MG/LH; P = .03 vs. LG/MH.
Acromial and scapular spine fractures
Methods
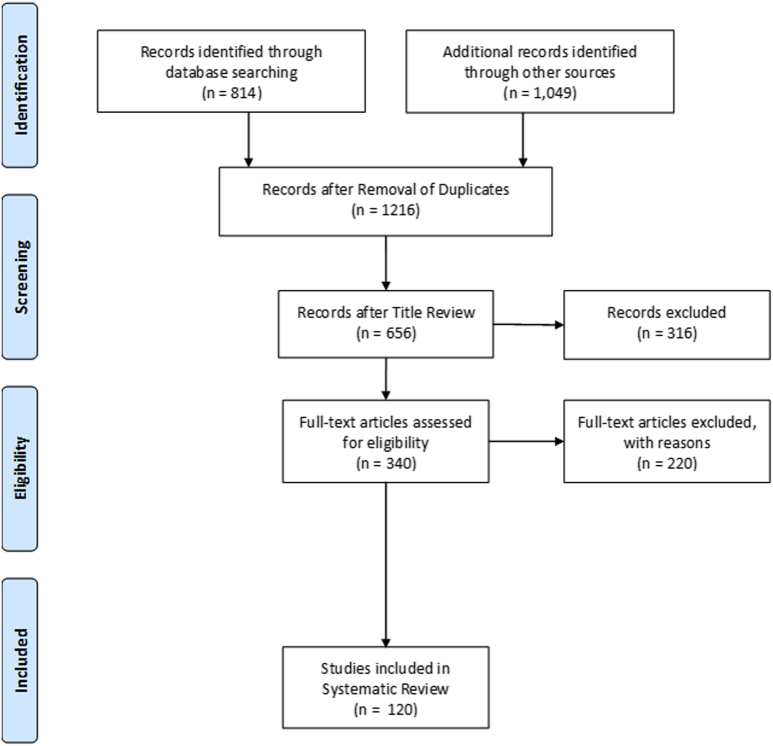
A systematic review was performed using PRISMA guidelines.180 The search was performed using the PubMed and Web of Science databases in March 2020 (Fig. 3). The search terms used were [(reverse shoulder) OR (reverse total shoulder) OR (inverted shoulder)] with filters as follows: date range (1/1/2010- 12/31/2019), species (human), and language (English). The search resulted in 1863 total titles. Studies were included if they (1) reported clinical outcomes of RSA and (2) reported the incidence of acromial and scapular spine fractures. Duplicate titles, review articles, meta-analyses/systematic reviews, editorials, technique studies, or studies with fewer than 10 patients were excluded. Abstract review was then performed. Exclusion criteria were biomechanical studies, anatomic/cadaver studies, computer modeling studies, studies focusing on one outcome or complication other than AF, RSA for oncologic indications, isolated radiographic studies, and studies that excluded AF or SSF. Title and abstract review excluded 876 articles, leaving 340 articles for full-text review. In addition to the prior exclusion criteria, studies that did not mention AF and/or SSF were excluded; however, studies that had no acromial or scapular spine stress fractures in their population were included if they specifically mentioned a lack of these fractures. This final elimination stage excluded 220 articles, resulting in 120 articles included for final analysis. Two of 4 authors (S.D./J.K./A.S./S.S.S.) reviewed the articles and collected the data.
Figure 3.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram for Acromial/Scapular Spine fractures
Acromial and scapular spine fracture rates overall and according to (1) revision status (primary vs. revision arthroplasty), (2) preoperative diagnoses, and (3) implant design were determined by pooled statistics. Prosthesis design was defined according to Routman et al.210 Comparisons were also made to Zumstein et al.293
Statistical analysis was performed using SPSS (version 26). Univariate analysis was performed with the chi-square test, or with Fisher exact test when the expected count for at least 1 cell in the comparison was less than 5. The alpha level for statistical significance was set to 0.05.
Results
The studies were mostly retrospective and provided Level III (38 studies) and Level IV evidence (78 studies), with 3 studies at Level II and 1 study providing Level I evidence.‡ A total of 14,235 shoulders were included in the analysis with a mean age of 72.1 years and 58.7% of female sex. The overall rate of AF and/or SSF was 2.6% (371 of 14,235 RSAs) at a mean follow-up of 4.3 years. When stratified by type, AF were more commonly reported than SSF. A diagnosis of inflammatory arthritis had significantly higher rates of AF/SSF compared with CTA, RCT, and PHF. Despite improved surgeon awareness in diagnosing acromial/scapular fracture, there was no significant increase in fracture rates compared with Zumstein et al293 (Table VI). The fracture rate was 2.5% after primary RSA and 2.7% after revision RSA (P = .76). There was no difference in acromial/scapular fracture rates for the Grammont design (MG/MH), at 2.5% (71/2817), vs. all other designs combined, at 2.5% (133/5420) (Table VII).
Table VI.
Acromial/scapular fractures rates overall and stratified by diagnosis
| Studies included | Shoulders | Acromial/scapular Fx | Rate, % | P value | |
|---|---|---|---|---|---|
| Current study overall | 120 | 14,235 | 371 | 2.6 | .06 |
| Zumstein et al | 21 | 782 | 12 | 1.5 | — |
| Current study: subtotal of non-Grammont designs | 30 | 5420 | 133 | 2.5 | .11 vs. Zumstein et al |
| Stratified by type | 116 | 12,688 | 327 | — | — |
| Acromial Fx | — | — | 205 | 1.6 (205/12,688) | — |
| Scapular spine Fx | — | — | 122 | 1.0 (122/12,688) | — |
| Diagnosis | |||||
| CTA | 21 | 1407 | 36 | 2.6 | .04 vs. PHF; .91 vs. RCT; .002∗ vs. inflammatory |
| PHF | 12 | 307 | 2 | 0.7 | .053 vs. RCT |
| RCT | 8 | 647 | 16 | 2.5 | — |
| Inflammatory | 5 | 153 | 12 | 7.8 | .001 vs. RCT; <.001∗ vs. PHF |
Fx, Fracture; CTA, cuff tear arthropathy; PHF, proximal humerus fracture; RCT, massive rotator cuff tear; JSES, Journal of Shoulder and Elbow Surgery.
A diagnosis of Inflammatory arthritis had significantly higher rates compared to CTA, RCT, and PHF. Despite improved surgeon awareness in diagnosing Acromial/Scapular Fx, there was no significant increase in rates compared to Zumstein et al (JSES, 2011).
Fisher exact test.
Table VII.
Acromial/scapular fracture rates according to (1) revision status (primary vs. revision) and (2) prosthesis design
| Studies included | Shoulders | Acromial/scapular fractures | Rate, % | P value | |
|---|---|---|---|---|---|
| Primary vs. revision | |||||
| Primary RSA | 82 | 7244 | 181 | 2.5 | .76 |
| Revision RSA | 21 | 707 | 19 | 2.7 | — |
| Prothesis design | |||||
| LG/MH | 16 | 2534 | 72 | 2.8 | .13 vs. MG/LH; .18∗ vs. LG/LH; .47 vs. MG/MH |
| MG/LH | 13 | 2746 | 60 | 2.2 | .37∗ vs. LG/LH; .41 vs. MG/MH |
| LG/LH | 1 | 140 | 1 | 0.7 | .26∗ vs. MG/MH |
| Subtotal | — | 5420 | 133 | 2.5 | — |
| MG/MH | 45 | 2817 | 71 | 2.5 | — |
RSA, reverse shoulder arthroplasty; LG, lateralized glenoid; MH, medialized humerus; MG, medialized glenoid; LH, lateralized humerus.
There was no difference in acromial/scapular fractures rates for the Grammont design (MG/MH) at 2.5% (71/2817) vs. all other designs combined at 2.5% (133/5420).
Fisher exact test.
Problems and miscellaneous
Methods
A systematic review was performed using PRISMA guidelines.180 The search was performed using the PubMed medical database in July 2019 (Fig. 4). The search terms used were [(Complication) OR (Revision) OR (Reoperation) OR (Algodystrophy) OR (CRPS) OR (Deltoid rupture) OR (Deltoid Injury) OR (Hematoma) OR (Seroma) OR (Heterotopic ossification) AND (reverse shoulder arthroplasty) OR (reverse total shoulder) OR (reverse total shoulder arthroplasty)] with filters as follows: date range (1/1/2010 to 05/31/2019), species (human), and language (English). The search resulted in 1008 total titles. Inclusion criteria were titles that specified primary or revision RSA. Exclusion criteria were duplicate titles, review articles, editorials, technique articles without reported patient outcomes, cadaveric studies, kinematic/finite-element model/computer model analyses, case reports, survey studies, elastography/histologic studies, cost-benefit analyses, and instructional course lecture articles. After application of these criteria, 209 titles remained for abstract review. Articles that reported 2-year follow-up studies clearly reported algodystrophy, complex regional pain syndrome (CRPS), deltoid rupture, deltoid injury, hematoma, seroma, heterotopic ossification (HO), reoperation, revision, or complication data were included. Articles with <15 patients, a minimum average follow-up of <24 months, and evaluated treatment of shoulder periprosthetic infection, blood transfusion rates, venous thromboembolism rates, RSA with concomitant tendon transfer, or RSA for tumor were excluded. This process eliminated 96 more articles, leaving 113 for full-text review. Definition of deltoid rupture, deltoid injury, hematoma, seroma, and/or HO was left to the discretion of each individual study. As there was rarely specific notation for algodystrophy/CRPS, any study with a description of pain as a postoperative problem/complication without an etiology was included; this was typically defined as “persistent pain” or “chronic pain.” This final elimination stage resulted in 74 articles for inclusion in the analysis. Two authors (S.W.S. and S.S.S.) reviewed the articles and collected the data. Comparisons were made to Zumstein et al.293
Figure 4.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram for problems/miscellaneous.
Statistical analysis was performed using SPSS (version 26). Univariate analysis was performed with the chi-square test, or with Fisher exact test when the expected count for at least 1 cell in the comparison was less than 5. The alpha level for statistical significance was set to 0.05.
Results
The studies were mostly retrospective and provided Level III or IV evidence.§ A total of 5529 shoulders were included in the analysis with a mean age of 71.5 years and 67.3% of female sex at a mean follow-up of 3.4 years. The overall rate was algodystrophy/CRPS = 0.4% (23/5529 shoulders), deltoid injury = 0.1% (5/5529), hematoma = 0.3% (15/5529), and HO = 0.8% (46/5529). Hematoma rates have significantly decreased compared to Zumstein et al (Table VIII). Additionally, 46.7% of all cases of hematoma were reported as requiring OR drainage.
Table VIII.
Pooled estimates of CRPS, deltoid injury, hematoma, and heterotopic ossification following RSA
| Studies included | Shoulders | Incidence | Current study rate, % (n/n) | Zumstein et al rate, % (n/n) | P value current study vs. Zumstein et al | |
|---|---|---|---|---|---|---|
| CRPS | 74 | 5529 | 23 | 0.4 (23/5529) | 0.5 (4/782) | .77∗ |
| Deltoid injury | 74 | 5529 | 5 | 0.1 (5/5529) | — | — |
| Hematoma | 74 | 5529 | 15 | 0.3 (15/5529) | 2.6 (20/782) | <.001∗ |
| Heterotopic ossification | 74 | 5529 | 46 | 0.8 (46/5529) | 0.8 (6/782) | .86 |
CRPS, complex regional pain syndrome; RSA, reverse shoulder arthroplasty; JSES, Journal of Shoulder and Elbow Surgery.
Hematoma rates have significantly decreased compared with Zumstein et al (JSES, 2011).
Fisher exact test.
Discussion
RSA has had wide adoption, with authors reporting good results in patients <55 years of age195 and patients >65 years of age and OA with an intact rotator cuff.239,244 Given the ubiquitous utility of RSA, it is not surprising to see variable complication rates being reported. However, as the indications continue to expand, the implants and prosthesis design improve as well. By limiting each search to publications after 2010 and by performing a systematic review for each complication, our study was able to examine large sample sizes and provide useful analyses based on diagnosis and prosthesis design that are typically difficult with registry studies or case series. Registry studies have large sample sizes, but classically only report revision rates and lack data on specific complication rates without revision.144,179 By contrast, case series usually lack a large sample size that is necessary to make specific comparisons with increased power. The results of this study will serve for better patient education and be helpful for surgeon planning for RSA based on diagnosis and prosthesis design.
On the basis of this study, the global instability rate was 3.3% (308/9306) at a mean follow-up of 3.2 years. Instability rates, especially modern non-Grammont designs, have significantly decreased compared with Zumstein et al. The majority of dislocations required revision of components and occurred within the first 90 days postoperatively. Primary RSA instability rates were significantly lower vs. revision RSA or RSA for failed ORIF PHF. The Grammont design (MG/MH) had a significantly higher instability rate vs. all other designs combined. Finally, the MG/LH design had a significantly lower rate than the LG/MH. Once instability occurs, it is difficult to manage. Instability can be treated with closed reduction but may have limited success, ultimately leading to revision or poor outcome without further intervention.204 However, revision may still lead to recurrent instability.40,137 Furthermore, it is important to note that the definition of instability was left to each study; the incidence of more subtle forms of instability has been shown to have negative effects on ASES scores compared with patients without signs of instability.246
There are multiple variables that may play a role in the etiology of instability: male gender, prior open operations, preoperative diagnoses of proximal humeral or tuberosity nonunion,40 superior baseplate inclination,246 and intraoperative resection of tuberosities.192,204 Furthermore, achieving anatomic soft tissue tensioning, specifically of the deltoid, plays a role in the overall stability of the prosthesis. It has been suggested that obesity may prevent the surgeon from accurately evaluating soft tissue tensioning during surgery, leading to subsequent instability.38 Additionally although some reports have found absence of subscapularis repair being significantly associated with prosthetic instability,40 others found no difference between repair vs. no repair,261 and using a lateralized RSA subscapularis repair may not be necessary.207
On the basis of this study, the global rate for IHF was 1.8% (91/5539 shoulders); IGF, 0.3% (15/5539); PostHF, 1.2% (69/5539); and PGF, 0.1% (6/5539), with the majority of intraoperative fractures, both glenoid and humerus, treated with no additional intervention. IGF and IHF rates using modern non-Grammont designs, have significantly decreased compared to Zumstein et al. Numerous factors play a role in the incidence of fracture. Risk of IHF has been shown to be increased by female sex, history of instability, prior hemiarthroplasty, and revision RSA cases.265 To avoid IHF during revision surgery, lateral humeral split has been suggested as the least aggressive means of extracting the humeral implant. Glenoid fractures during surgery are rare, typically related to the reaming or fixation process; IGFs may occur in PHF cases as a result of overreaming because there is less sclerotic bone in the typically unaffected glenoid.211 Although many glenoid fractures can be addressed by fixation or redirection of the baseplate, in the case of substantial glenoid fractures it may be necessary to implement a 2-stage bone grafting and reimplantation process. Patients treated with RSA combined with allograft-prosthetic composite48 and cement-within-cement fixation of the humeral component in revision RSA have both been discussed as at risk for PostHF.266 PostHF are most commonly associated with traumatic events, can have significant negative impacts on clinical outcomes, and has been shown to be more likely to occur in older patients, females, and those operated on via a transdeltoid approach.11
An explanation for some recent studies reporting fracture is the “the learning curve” of a new implant.14 Many intraoperative fractures occurred early on with the use of a short-stem prosthesis14 as well as stemless implants.150 Because of the technically demanding nature of stemless implants, there is a high susceptibility to fracture both intraoperatively and postoperatively, especially fracture of the humeral metaphysis due to excessive bone impaction in soft bone.150
On the basis of this study, the overall rate of AF and/or SSF was 2.6% (371 of 14,235 RSAs [1.6% for AF and 1.0% for SSF]). This is similar to the recent King et al132 study (2.8%); however, our study is inclusive of 2 more years of data with approximately 5000 more shoulders included. A diagnosis of inflammatory arthritis had significantly higher rates of AF/SSF compared with CTA, RCT, and PHF. Despite improved surgeon awareness (including expansion of previous definition168 to include persistent pain without magnetic resonance imaging or bone scan changes and improved diagnostic imaging) for diagnosing acromial/scapular fracture, there was no significant increase in rates compared with Zumstein et al. Some authors have theorized that acromion fractures are caused by excessive tensioning of the deltoid with RSA that causes significant inferior stress on the acromion70,148 possibly influenced by the anatomic position of the acromion.227 Excessive lowering of the humerus can lead to arm lengthening and thus increased resting tension of the deltoid on the tip of the acromion.278 Also, excessive medialization may create a lower deltoid wrapping angle, leading to a more vertical line of pull from the deltoid producing an increased bending moment arm applied to the acromion, further placing the acromion at risk for fracture. In these cases, the greater tuberosity cannot act as a pulley of reflection for the deltoid anymore.278
In our study, the LG/MH design had the highest reported incidence of AF/SSF at 2.8%. This compares to 2.5% and 2.2% in the MG/MH and MG/LH designs, respectively. All comparisons were not statistically significant. A finite element study by Wong et al284 showed that glenosphere lateralization significantly increased acromial stress by 17%. Other studies have shown a decreased deltoid moment arm with glenosphere lateralization, which may also affect acromial stresses.86,97 As the moment arm decreases, there is increased force required by the deltoid to abduct the arm in elevation, thus increasing stress on the acromion.
AF and SSF can lead to worse outcomes after RSA105,148,168,242,249,268; however, these patients typically still have better functional scores compared with preoperative values.105,148,249 Some authors advocate operative intervention for displaced AF affecting a large portion of the deltoid; however, operative intervention has not been shown to improve overall outcomes.168 No consensus on the recommended treatment of these fractures has been reached.105,168,268 Risk factors for AF and SSF reported in clinical studies are osteoporosis, a smaller lateral offset of the greater tuberosity, and increased arm lengthening.196,278 One theory about how to prevent SSF is to avoid putting screws through the junction of the scapular spine and the scapular body, which may act as a stress riser. One study showed a significantly lower rate of SSF when no superior screws were used (0% of 112 RSAs) compared with when screws were used above the metaglene central cage (4.4% of 209 RSAs).130 Another study suggests that coracoacromial ligament transection during surgical exposure for RSA alters strain patterns along acromion and scapular spine, leading to an accumulation of microtrauma, which may lead to stress fracture.247
The term problem refers to events perceived as adverse but unlikely to affect the final outcome, that is, algodystrophy/CRPS, hematoma, and heterotopic ossification.16 On the basis of this study, the overall rate for algodystrophy/CRPS is 0.4% (23/5529 shoulders); deltoid injury, 0.1% (5/5529); hematoma, 0.3% (15/5529); and HO, 0.8% (46/5529). Hematoma rates have significantly decreased compared with Zumstein et al. CRPS may perhaps be underreported in the literature; many studies report persistent pain,59,67,182 chronic pain,81 or greater than moderate pain.4 Thus, in an attempt to accurately gauge the rates of CRPS, we included any description of pain listed as a postoperative problem or complication without an etiology. However, there is typically a delayed diagnosis following orthopedic surgery with a mean time delay of 3.9 years before diagnosis of CRPS. A lack of attention to more subtle signs of autonomic dysfunction may be an important contributing factor for a missing CRPS diagnosis.158 Deltoid injury may be attributed to arm lengthening140 whereas massive rotator cuff tears with retraction and patients with prior open rotator cuff surgery have been shown to be risk factors for postoperative deltoid rupture.279 Patients with preoperative deltoid impairment or postoperative rupture can still obtain good range of motion and pain scores.141,279 A wide range of rates for postoperative hematoma have been reported in the literature, which can be attributed to the lack of reporting in situations in which intervention was not required. Although hematomas are unlikely to affect the final outcome, they may pose an increased risk for the development of infection. Most cases of HO are benign, requiring neither nonsteroidal anti-inflammatory drugs, prophylaxis, or treatment. Only grade 2 HO is clinically relevant, with a negative effect on the function of the shoulder during its development.257 Factors reported to increase the risk of HO include surgical approach, the extent of operative release of soft tissues such as release of the triceps in the superolateral approach,257 procedures where bone graft is used,80 and RSA with cerclage for complex proximal humerus fracture with extended diaphyseal involvement.81
Limitations of this study are similar to any systematic review, including many retrospective studies with possible reporting bias, differing follow-up times, publication bias, and possible conflicting definitions of complications among studies. Furthermore, complication rates in this study are only from published data predominantly out of high-volume centers; this may not capture the rate or distribution of complications in the general population, “many of whom perform only a few of these procedures each year.”236 High-volume centers have been reported to have better perioperative quality metrics235 and maximized outcomes after RSA, likely related to surgical experience.69 Thus, complex procedures, such as RSA, have been advised to be performed at high-volume destinations, or it has been encouraged that lower-volume institutions strategize to function as a higher-volume center.69 Also, a statistician reviewed the collected data and concluded that a multivariate analysis of the results was not possible because of the heterogeneity of the reported outcomes, the lack of reporting of standard deviation in most studies, and the lack of control groups in the included studies. Another limitation is that patient outcomes were not collected; however, our study was able to examine multiple complications with large sample sizes and provide useful analyses based on diagnosis and prosthesis design that are difficult with registry studies (secondary to lack of specific data) or case series, as many lack a large sample size necessary to make comparisons with clinical value.
Conclusion
Focused systematic reviews of recent literature with a large volume of shoulders demonstrate that using modern non-Grammont prosthesis designs, complications including instability, intraoperative humerus and glenoid fractures, and hematoma are significantly reduced compared with previous studies. In addition, modern RSA designs carry an AF/SSF rate of 2.5%. As the indications continue to expand for RSA, it is imperative to accurately track the rate and types of complications in order to justify its cost and increased indications.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional Review Board approval was not required for this systematic review.
References 1, 4, 5, 7, 8, 9, 14, 20, 25, 26, 29, 30, 31, 35, 37, 40, 41, 42, 44, 46, 47, 48, 49, 51, 52, 53, 54, 55, 58, 61, 62, 64, 66, 68, 72, 73, 75, 77, 78, 80, 81, 83, 84, 85, 87, 91, 92, 93, 98, 102, 103, 106, 107, 108, 110, 111, 113, 114, 116, 117, 118, 119, 123, 125, 128, 131, 133, 136, 137, 138, 143, 146, 147, 149, 154, 155, 157, 160, 162, 163, 164, 169, 172, 173, 174, 178, 183, 185, 186, 188, 192, 194, 195, 197, 198, 200, 202, 204, 207, 208, 209, 213, 215, 217, 219, 220, 223, 224, 225, 228, 229, 231, 237, 245, 246, 250, 251, 252, 253, 254, 255, 258, 259, 260, 261, 262, 264, 266, 267, 270, 273, 275, 277, 281, 287, 290, 292.
References 1, 4, 5, 14, 15, 17, 20, 24, 27, 28, 31, 34, 35, 36, 37, 42, 44, 48, 54, 56, 61, 63, 68, 79, 80, 82, 87, 91, 92, 93, 98, 102, 108, 111, 112, 113, 116, 117, 119, 124, 125, 128, 131, 133, 138, 143, 147, 150, 154, 160, 164, 169, 170, 171, 172, 173, 174, 176, 185, 186, 189, 191, 192, 194, 195, 198, 202, 203, 204, 211, 213, 215, 219, 223, 224, 225, 228, 234, 237, 241, 250, 252, 253, 254, 262, 265, 266, 267, 269, 275, 281, 282, 291, 292.
References 2, 5, 12, 13, 14, 15, 19, 21, 24, 28, 42, 43, 44, 46, 47, 50, 54, 58, 63, 65, 68, 71, 74, 77, 81, 84, 90, 91, 92, 95, 96, 99, 100, 101, 102, 105, 106, 109, 110, 111, 113, 115, 118, 119, 120, 127, 129, 130, 131, 134, 135, 138, 139, 143, 145, 147, 149, 150, 152, 153, 155, 156, 161, 162, 166, 167, 169, 171, 173, 174, 175, 181, 182, 183, 184, 186, 187, 189, 190, 191, 195, 200, 201, 202, 206, 213, 214, 218, 221, 224, 225, 226, 229, 230, 231, 232, 233, 234, 238, 241, 243, 248, 249, 250, 252, 256, 259, 269, 270, 271, 272, 273, 276, 280, 285, 288, 289, 290.
References 3, 4, 6, 10, 15, 22, 23, 27, 32, 41, 42, 45, 48, 49, 51, 52, 55, 56, 58, 59, 60, 67, 74, 80, 81, 84, 88, 94, 98, 102, 106, 111, 113, 119, 122, 123, 127, 128, 142, 147, 151, 165, 169, 171, 173, 174, 177, 182, 187, 190, 192, 193, 195, 199, 202, 205, 206, 212, 216, 219, 222, 223, 231, 252, 257, 261, 262, 264, 269, 270, 274, 282, 283, 292.
References
- 1.Abdel M.P., Hattrup S.J., Sperling J.W., Cofield R.H., Kreofsky C.R., Sanchez-Sotelo J. Revision of an unstable hemiarthroplasty or anatomical total shoulder replacement using a reverse design prosthesis. Bone Joint J. 2013;95-B:668–672. doi: 10.1302/0301-620x.95b5.30964. [DOI] [PubMed] [Google Scholar]
- 2.Abdelfattah A., Otto R.J., Simon P., Christmas K.N., Tanner G., LaMartina J., 2nd Classification of instability after reverse shoulder arthroplasty guides surgical management and outcomes. J Shoulder Elbow Surg. 2018;27:e107–e118. doi: 10.1016/j.jse.2017.09.031. [DOI] [PubMed] [Google Scholar]
- 3.Aibinder W.R., Clark N.J., Schoch B.S., Steinmann S.P. Assessing glenosphere position: superior approach versus deltopectoral for reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27:455–462. doi: 10.1016/j.jse.2017.10.013. [DOI] [PubMed] [Google Scholar]
- 4.Aibinder W.R., Schoch B.S., Cofield R.H., Sperling J.W., Sánchez-Sotelo J. Reverse shoulder arthroplasty in patients with os acromiale. J Shoulder Elbow Surg. 2017;26:1598–1602. doi: 10.1016/j.jse.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Al-Hadithy N., Domos P., Sewell M.D., Pandit R. Reverse shoulder arthroplasty in 41 patients with cuff tear arthropathy with a mean follow-up period of 5 years. J Shoulder Elbow Surg. 2014;23:1662–1668. doi: 10.1016/j.jse.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Aleem A.W., Feeley B.T., Austin L.S., Ma C.B., Krupp R.J., Ramsey M.L. Effect of humeral component version on outcomes in reverse shoulder arthroplasty. Orthopedics. 2017;40:179–186. doi: 10.3928/01477447-20170117-04. [DOI] [PubMed] [Google Scholar]
- 7.Alentorn-Geli E., Clark N.J., Assenmacher A.T., Samuelsen B.T., Sánchez-Sotelo J., Cofield R.H. What are the complications, survival, and outcomes after revision to reverse shoulder arthroplasty in patients older than 80 years? Clin Orthop Relat Res. 2017;475:2744–2751. doi: 10.1007/s11999-017-5406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alentorn-Geli E., Guirro P., Santana F., Torrens C. Treatment of fracture sequelae of the proximal humerus: comparison of hemiarthroplasty and reverse total shoulder arthroplasty. Arch Orthop Trauma Surg. 2014;134:1545–1550. doi: 10.1007/s00402-014-2074-9. [DOI] [PubMed] [Google Scholar]
- 9.Alentorn-Geli E., Wanderman N.R., Assenmacher A.T., Sperling J.W., Cofield R.H., Sánchez-Sotelo J. Anatomic total shoulder arthroplasty with posterior capsular plication versus reverse shoulder arthroplasty in patients with biconcave glenoids: a matched cohort study. J Orthop Surg (Hong Kong) 2018;26 doi: 10.1177/2309499018768570. 2309499018768570. [DOI] [PubMed] [Google Scholar]
- 10.Allert J.W., Sellers T.R., Simon P., Christmas K.N., Patel S., Frankle M.A. Massive rotator cuff tears in patients older than sixty-five: indications for cuff repair versus reverse total shoulder arthroplasty. Am J Orthop (Belle Mead NJ) 2018;47 doi: 10.12788/ajo.2018.0109. [DOI] [PubMed] [Google Scholar]
- 11.Ascione F., Domos P., Guarrella V., Chelli M., Boileau P., Walch G. Long-term humeral complications after Grammont-style reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27:1065–1071. doi: 10.1016/j.jse.2017.11.028. [DOI] [PubMed] [Google Scholar]
- 12.Ascione F., Kilian C.M., Laughlin M.S., Bugelli G., Domos P., Neyton L. Increased scapular spine fractures after reverse shoulder arthroplasty with a humeral onlay short stem: an analysis of 485 consecutive cases. J Shoulder Elbow Surg. 2018;27:2183–2190. doi: 10.1016/j.jse.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 13.Athwal G.S., Faber K.J. Outcomes of reverse shoulder arthroplasty using a mini 25-mm glenoid baseplate. Int Orthop. 2016;40:109–113. doi: 10.1007/s00264-015-2945-x. [DOI] [PubMed] [Google Scholar]
- 14.Atoun E., Van Tongel A., Hous N., Narvani A., Relwani J., Abraham R. Reverse shoulder arthroplasty with a short metaphyseal humeral stem. Int Orthop. 2014;38:1213–1218. doi: 10.1007/s00264-014-2328-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ballas R., Béguin L. Results of a stemless reverse shoulder prosthesis at more than 58 months mean without loosening. J Shoulder Elbow Surg. 2013;22:e1–e6. doi: 10.1016/j.jse.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Barco R., Savvidou O.D., Sperling J.W., Sanchez-Sotelo J., Cofield R.H. Complications in reverse shoulder arthroplasty. EFORT Open Rev. 2016;1:72–80. doi: 10.1302/2058-5241.1.160003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baudi P., Campochiaro G., Serafini F., Gazzotti G., Matino G., Rovesta C. Hemiarthroplasty versus reverse shoulder arthroplasty: comparative study of functional and radiological outcomes in the treatment of acute proximal humerus fracture. Musculoskelet Surg. 2014;98(Suppl 1):19–25. doi: 10.1007/s12306-014-0322-3. [DOI] [PubMed] [Google Scholar]
- 18.Baulot E., Sirveaux F., Boileau P. Grammont's idea: The story of Paul Grammont's functional surgery concept and the development of the reverse principle. Clin Orthop Relat Res. 2011;469:2425–2431. doi: 10.1007/s11999-010-1757-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beazley J., Evans J.P., Furness N.D., Smith C.D. Comparative learning curves for early complications in anatomical and reverse shoulder arthroplasty. Ann R Coll Surg Engl. 2018;100:491–496. doi: 10.1308/rcsann.2018.0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beck J.D., Irgit K.S., Andreychik C.M., Maloney P.J., Tang X., Harter G.D. Reverse total shoulder arthroplasty in obese patients. J Hand Surg Am. 2013;38:965–970. doi: 10.1016/j.jhsa.2013.02.025. [DOI] [PubMed] [Google Scholar]
- 21.Beltrame A., Di Benedetto P., Cicuto C., Cainero V., Chisoni R., Causero A. Onlay versus inlay humeral steam in reverse shoulder arthroplasty (RSA): clinical and biomechanical study. Acta Biomed. 2019;90:54–63. doi: 10.23750/abm.v90i12-S.8983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berglund D.D., Mijic D., Law T.Y., Kurowicki J., Rosas S., Levy J.C. Value comparison of humeral component press-fit and cemented techniques in reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28:496–502. doi: 10.1016/j.jse.2018.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bigorre N., Lancigu R., Bizot P., Hubert L. Predictive factors of scapular notching in patients with reverse shoulder arthroplasty. Orthop Traumatol Surg Res. 2014;100:711–714. doi: 10.1016/j.otsr.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 24.Black E.M., Roberts S.M., Siegel E., Yannopoulos P., Higgins L.D., Warner J.J. Reverse shoulder arthroplasty as salvage for failed prior arthroplasty in patients 65 years of age or younger. J Shoulder Elbow Surg. 2014;23:1036–1042. doi: 10.1016/j.jse.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 25.Black E.M., Roberts S.M., Siegel E., Yannopoulos P., Higgins L.D., Warner J.J. Failure after reverse total shoulder arthroplasty: what is the success of component revision? J Shoulder Elbow Surg. 2015;24:1908–1914. doi: 10.1016/j.jse.2015.05.029. [DOI] [PubMed] [Google Scholar]
- 26.Bloch H.R., Budassi P., Bischof A., Agneskirchner J., Domenghini C., Frattini M. Influence of glenosphere design and material on clinical outcomes of reverse total shoulder arthroplasty. Shoulder Elbow. 2014;6:156–164. doi: 10.1177/1758573214535574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boileau P., Alta T.D., Decroocq L., Sirveaux F., Clavert P., Favard L. Reverse shoulder arthroplasty for acute fractures in the elderly: is it worth reattaching the tuberosities? J Shoulder Elbow Surg. 2019;28:437–444. doi: 10.1016/j.jse.2018.08.025. [DOI] [PubMed] [Google Scholar]
- 28.Boileau P., Melis B., Duperron D., Moineau G., Rumian A.P., Han Y. Revision surgery of reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:1359–1370. doi: 10.1016/j.jse.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 29.Boileau P., Morin-Salvo N., Gauci M.O., Seeto B.L., Chalmers P.N., Holzer N. Angled BIO-RSA (bony-increased offset-reverse shoulder arthroplasty): a solution for the management of glenoid bone loss and erosion. J Shoulder Elbow Surg. 2017;26:2133–2142. doi: 10.1016/j.jse.2017.05.024. [DOI] [PubMed] [Google Scholar]
- 30.Bonnevialle N., Ohl X., Clavert P., Favard L., Frégeac A., Obert L. Should the supraspinatus tendon be excised in the case of reverse shoulder arthroplasty for fracture? Eur J Orthop Surg Traumatol. 2020;30:231–235. doi: 10.1007/s00590-019-02572-7. [DOI] [PubMed] [Google Scholar]
- 31.Bonnevialle N., Tournier C., Clavert P., Ohl X., Sirveaux F., Saragaglia D. Hemiarthroplasty versus reverse shoulder arthroplasty in 4-part displaced fractures of the proximal humerus: multicenter retrospective study. Orthop Traumatol Surg Res. 2016;102:569–573. doi: 10.1016/j.otsr.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 32.Budge M.D., Moravek J.E., Zimel M.N., Nolan E.M., Wiater J.M. Reverse total shoulder arthroplasty for the management of failed shoulder arthroplasty with proximal humeral bone loss: is allograft augmentation necessary? J Shoulder Elbow Surg. 2013;22:739–744. doi: 10.1016/j.jse.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 33.Burrus M.T., Werner B.C., Cancienne J.M., Gwathmey F.W., Brockmeier S.F. Shoulder arthroplasty in patients with Parkinson's disease is associated with increased complications. J Shoulder Elbow Surg. 2015;24:1881–1887. doi: 10.1016/j.jse.2015.05.048. [DOI] [PubMed] [Google Scholar]
- 34.Castagna A., Delcogliano M., de Caro F., Ziveri G., Borroni M., Gumina S. Conversion of shoulder arthroplasty to reverse implants: clinical and radiological results using a modular system. Int Orthop. 2013;37:1297–1305. doi: 10.1007/s00264-013-1907-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Castricini R., Gasparini G., Di Luggo F., De Benedetto M., De Gori M., Galasso O. Health-related quality of life and functionality after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:1639–1649. doi: 10.1016/j.jse.2013.01.020. [DOI] [PubMed] [Google Scholar]
- 36.Cazeneuve J.F., Cristofari D.J. The reverse shoulder prosthesis in the treatment of fractures of the proximal humerus in the elderly. J Bone Joint Surg Br. 2010;92:535–539. doi: 10.1302/0301-620x.92b4.22450. [DOI] [PubMed] [Google Scholar]
- 37.Cazeneuve J.F., Cristofari D.J. Long term functional outcome following reverse shoulder arthroplasty in the elderly. Orthop Traumatol Surg Res. 2011;97:583–589. doi: 10.1016/j.otsr.2011.03.025. [DOI] [PubMed] [Google Scholar]
- 38.Chalmers P.N., Rahman Z., Romeo A.A., Nicholson G.P. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:737–744. doi: 10.1016/j.jse.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 39.Cheung E., Willis M., Walker M., Clark R., Frankle M.A. Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2011;19:439–449. [PubMed] [Google Scholar]
- 40.Cheung E.V., Sarkissian E.J., Sox-Harris A., Comer G.C., Saleh J.R., Diaz R. Instability after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27:1946–1952. doi: 10.1016/j.jse.2018.04.015. [DOI] [PubMed] [Google Scholar]
- 41.Chivot M., Lami D., Bizzozero P., Galland A., Argenson J.N. Three- and four-part displaced proximal humeral fractures in patients older than 70 years: reverse shoulder arthroplasty or nonsurgical treatment? J Shoulder Elbow Surg. 2019;28:252–259. doi: 10.1016/j.jse.2018.07.019. [DOI] [PubMed] [Google Scholar]
- 42.Cho C.H., Song K.S., Koo T.W. Clinical outcomes and complications during the learning curve for reverse total shoulder arthroplasty: an analysis of the first 40 cases. Clin Orthop Surg. 2017;9:213–217. doi: 10.4055/cios.2017.9.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Choi C.H., Kim S.G., Lee J.J., Kwack B.H. Comparison of clinical and radiological results according to glenosphere position in reverse total shoulder arthroplasty: a short-term follow-up study. Clin Orthop Surg. 2017;9:83–90. doi: 10.4055/cios.2017.9.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Choi S., Bae J.H., Kwon Y.S., Kang H. Clinical outcomes and complications of cementless reverse total shoulder arthroplasty during the early learning curve period. J Orthop Surg Res. 2019;14:53. doi: 10.1186/s13018-019-1077-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cicak N., Klobucar H., Medancic N. Reverse shoulder arthroplasty in acute fractures provides better results than in revision procedures for fracture sequelae. Int Orthop. 2015;39:343–348. doi: 10.1007/s00264-014-2649-7. [DOI] [PubMed] [Google Scholar]
- 46.Clark N.J., Samuelsen B.T., Alentorn-Geli E., Assenmacher A.T., Cofield R.H., Sperling J.W. Primary reverse shoulder arthroplasty in patients older than 80 years of age: survival and outcomes. Bone Joint J. 2019;101-B:1520–1525. doi: 10.1302/0301-620x.101b12.Bjj-2018-1571. [DOI] [PubMed] [Google Scholar]
- 47.Clavert P., Kling A., Sirveaux F., Favard L., Mole D., Walch G. Reverse shoulder arthroplasty for instability arthropathy. Int Orthop. 2019;43:1653–1658. doi: 10.1007/s00264-018-4123-4. [DOI] [PubMed] [Google Scholar]
- 48.Cox J.L., McLendon P.B., Christmas K.N., Simon P., Mighell M.A., Frankle M.A. Clinical outcomes following reverse shoulder arthroplasty-allograft composite for revision of failed arthroplasty associated with proximal humeral bone deficiency: 2- to 15-year follow-up. J Shoulder Elbow Surg. 2019;28:900–907. doi: 10.1016/j.jse.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 49.Cox R.M., Padegimas E.M., Abboud J.A., Getz C.L., Lazarus M.D., Ramsey M.L. Outcomes of an anatomic total shoulder arthroplasty with a contralateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27:998–1003. doi: 10.1016/j.jse.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 50.Crosby L.A., Hamilton A., Twiss T. Scapula fractures after reverse total shoulder arthroplasty: classification and treatment. Clin Orthop Relat Res. 2011;469:2544–2549. doi: 10.1007/s11999-011-1881-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Crosby L.A., Wright T.W., Yu S., Zuckerman J.D. Conversion to reverse total shoulder arthroplasty with and without humeral stem retention: the role of a convertible-platform stem. J Bone Joint Surg Am. 2017;99:736–742. doi: 10.2106/jbjs.16.00683. [DOI] [PubMed] [Google Scholar]
- 52.Cuff D., Clark R., Pupello D., Frankle M. Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency: a concise follow-up, at a minimum of five years, of a previous report. J Bone Joint Surg Am. 2012;94:1996–2000. doi: 10.2106/jbjs.K.01206. [DOI] [PubMed] [Google Scholar]
- 53.Cuff D.J., Pupello D.R. Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. J Bone Joint Surg Am. 2013;95:2050–2055. doi: 10.2106/jbjs.L.01637. [DOI] [PubMed] [Google Scholar]
- 54.Cuff D.J., Pupello D.R., Santoni B.G., Clark R.E., Frankle M.A. Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency: a concise follow-up, at a minimum of 10 years, of previous reports. J Bone Joint Surg Am. 2017;99:1895–1899. doi: 10.2106/jbjs.17.00175. [DOI] [PubMed] [Google Scholar]
- 55.Cuff D.J., Santoni B.G. Anatomic total shoulder arthroplasty versus reverse total shoulder arthroplasty for post-capsulorrhaphy arthropathy. Orthopedics. 2018;41:275–280. doi: 10.3928/01477447-20180724-05. [DOI] [PubMed] [Google Scholar]
- 56.Cuff D.J., Santoni B.G. Reverse shoulder arthroplasty in the weight-bearing versus non-weight-bearing shoulder: mid-term outcomes with minimum 5-year follow-up. Orthopedics. 2018;41:e328–e333. doi: 10.3928/01477447-20180213-10. [DOI] [PubMed] [Google Scholar]
- 57.Cuff D.J., Virani N.A., Levy J., Frankle M.A., Derasari A., Hines B. The treatment of deep shoulder infection and glenohumeral instability with debridement, reverse shoulder arthroplasty and postoperative antibiotics. J Bone Joint Surg Br. 2008;90:336–342. doi: 10.1302/0301-620X.90B3.19408. [DOI] [PubMed] [Google Scholar]
- 58.Cusick M.C., Otto R.J., Clark R.E., Frankle M.A. Outcome of reverse shoulder arthroplasty for patients with parkinson's disease: a matched cohort study. Orthopedics. 2017;40:e675–e680. doi: 10.3928/01477447-20170509-03. [DOI] [PubMed] [Google Scholar]
- 59.Cvetanovich G.L., Savin D.D., Frank R.M., Gowd A.K., Sumner S.A., Romeo A.A. Inferior outcomes and higher complication rates after shoulder arthroplasty in workers' compensation patients. J Shoulder Elbow Surg. 2019;28:875–881. doi: 10.1016/j.jse.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 60.De Biase C.F., Delcogliano M., Borroni M., Castagna A. Reverse total shoulder arthroplasty: radiological and clinical result using an eccentric glenosphere. Musculoskelet Surg. 2012;96(Suppl 1):S27–S34. doi: 10.1007/s12306-012-0193-4. [DOI] [PubMed] [Google Scholar]
- 61.Dilisio M.F., Miller L.R., Siegel E.J., Higgins L.D. Conversion to reverse shoulder arthroplasty: humeral stem retention versus revision. Orthopedics. 2015;38:e773–e779. doi: 10.3928/01477447-20150902-54. [DOI] [PubMed] [Google Scholar]
- 62.Dukan R., Bahman M., Rousseau M.A., Boyer P. Outcomes of reverse shoulder arthroplasty using a short stem through a superolateral approach. J Shoulder Elbow Surg. 2020;29:1197–1205. doi: 10.1016/j.jse.2019.09.025. [DOI] [PubMed] [Google Scholar]
- 63.Ek E.T., Neukom L., Catanzaro S., Gerber C. Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elbow Surg. 2013;22:1199–1208. doi: 10.1016/j.jse.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 64.Ekelund A., Nyberg R. Can reverse shoulder arthroplasty be used with few complications in rheumatoid arthritis? Clin Orthop Relat Res. 2011;469:2483–2488. doi: 10.1007/s11999-010-1654-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Elhassan B.T., Wagner E.R., Werthel J.D., Lehanneur M., Lee J. Outcome of reverse shoulder arthroplasty with pedicled pectoralis transfer in patients with deltoid paralysis. J Shoulder Elbow Surg. 2018;27:96–103. doi: 10.1016/j.jse.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 66.Ernstbrunner L., Rahm S., Suter A., Imam M.A., Catanzaro S., Grubhofer F. Salvage reverse total shoulder arthroplasty for failed operative treatment of proximal humeral fractures in patients younger than 60 years: long-term results. J Shoulder Elbow Surg. 2020;29:561–570. doi: 10.1016/j.jse.2019.07.040. [DOI] [PubMed] [Google Scholar]
- 67.Ernstbrunner L., Suter A., Catanzaro S., Rahm S., Gerber C. Reverse total shoulder arthroplasty for massive, irreparable rotator cuff tears before the age of 60 years: long-term results. J Bone Joint Surg Am. 2017;99:1721–1729. doi: 10.2106/JBJS.17.00095. [DOI] [PubMed] [Google Scholar]
- 68.Ernstbrunner L., Werthel J.D., Wagner E., Hatta T., Sperling J.W., Cofield R.H. Glenoid bone grafting in primary reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1441–1447. doi: 10.1016/j.jse.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 69.Farley K.X., Schwartz A.M., Boden S.H., Daly C.A., Gottschalk M.B., Wagner E.R. Defining the volume-outcome relationship in reverse shoulder arthroplasty: a nationwide analysis. J Bone Joint Surg Am. 2020;102:388–396. doi: 10.2106/JBJS.19.01012. [DOI] [PubMed] [Google Scholar]
- 70.Farshad M., Gerber C. Reverse total shoulder arthroplasty-from the most to the least common complication. Int Orthop. 2010;34:1075–1082. doi: 10.1007/s00264-010-1125-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Farshad M., Grögli M., Catanzaro S., Gerber C. Revision of reversed total shoulder arthroplasty. Indications and outcome. BMC Musculoskelet Disord. 2012;13:160. doi: 10.1186/1471-2474-13-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Flurin P.H., Marczuk Y., Janout M., Wright T.W., Zuckerman J., Roche C.P. Comparison of outcomes using anatomic and reverse total shoulder arthroplasty. Bull Hosp Jt Dis (2013) 2013;71(Suppl 2):101–107. [PubMed] [Google Scholar]
- 73.Flurin P.H., Roche C.P., Wright T.W., Marczuk Y., Zuckerman J.D. A comparison and correlation of clinical outcome metrics in anatomic and reverse total shoulder arthroplasty. Bull Hosp Jt Dis (2013) 2015;73(Suppl 1):S118–S123. [PubMed] [Google Scholar]
- 74.Flury M., Kwisda S., Kolling C., Audigé L. Latissimus dorsi muscle transfer reduces external rotation deficit at the cost of internal rotation in reverse shoulder arthroplasty patients: a cohort study. J Shoulder Elbow Surg. 2019;28:56–64. doi: 10.1016/j.jse.2018.06.032. [DOI] [PubMed] [Google Scholar]
- 75.Flury M.P., Frey P., Goldhahn J., Schwyzer H.K., Simmen B.R. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure—midterm results. Int Orthop. 2011;35:53–60. doi: 10.1007/s00264-010-0990-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Frank R.M., Lee S., Sumner S., Griffin J., Leroux T., Verma N.N. Shoulder arthroplasty outcomes after prior non-arthroplasty shoulder surgery. JB JS Open Access. 2018;3:e0055. doi: 10.2106/JBJS.OA.17.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Friedman R.J., Flurin P.H., Wright T.W., Zuckerman J.D., Roche C.P. Comparison of reverse total shoulder arthroplasty outcomes with and without subscapularis repair. J Shoulder Elbow Surg. 2017;26:662–668. doi: 10.1016/j.jse.2016.09.027. [DOI] [PubMed] [Google Scholar]
- 78.Gaeremynck P., Amouyel T., Saab M., Gadisseux B., Soudy K., Szymanski C. Clinical and radiological outcomes of 17 reverse shoulder arthroplasty cases performed after failed humeral head resurfacing. Orthop Traumatol Surg Res. 2019;105:1495–1501. doi: 10.1016/j.otsr.2019.06.017. [DOI] [PubMed] [Google Scholar]
- 79.Gallinet D., Adam A., Gasse N., Rochet S., Obert L. Improvement in shoulder rotation in complex shoulder fractures treated by reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:38–44. doi: 10.1016/j.jse.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 80.Garofalo R., Brody F., Castagna A., Ceccarelli E., Krishnan S.G. Reverse shoulder arthroplasty with glenoid bone grafting for anterior glenoid rim fracture associated with glenohumeral dislocation and proximal humerus fracture. Orthop Traumatol Surg Res. 2016;102:989–994. doi: 10.1016/j.otsr.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 81.Garofalo R., Flanagin B., Castagna A., Lo E.Y., Krishnan S.G. Long stem reverse shoulder arthroplasty and cerclage for treatment of complex long segment proximal humeral fractures with diaphyseal extension in patients more than 65 years old. Injury. 2015;46:2379–2383. doi: 10.1016/j.injury.2015.09.024. [DOI] [PubMed] [Google Scholar]
- 82.Garofalo R., Flanagin B., Castagna A., Lo E.Y., Krishnan S.G. Reverse shoulder arthroplasty for proximal humerus fracture using a dedicated stem: radiological outcomes at a minimum 2 years of follow-up-case series. J Orthop Surg Res. 2015;10:129. doi: 10.1186/s13018-015-0261-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gasbarro G., Crasto J.A., Rocha J., Henry S., Kano D., Tarkin I.S. Reverse total shoulder arthroplasty for geriatric proximal humerus fracture dislocation with concomitant nerve injury. Geriatr Orthop Surg Rehabil. 2019;10 doi: 10.1177/2151459319855318. 2151459319855318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gerber C., Canonica S., Catanzaro S., Ernstbrunner L. Longitudinal observational study of reverse total shoulder arthroplasty for irreparable rotator cuff dysfunction: results after 15 years. J Shoulder Elbow Surg. 2018;27:831–838. doi: 10.1016/j.jse.2017.10.037. [DOI] [PubMed] [Google Scholar]
- 85.Giardella A., Ascione F., Mocchi M., Berlusconi M., Romano A.M., Oliva F. Reverse total shoulder versus angular stable plate treatment for proximal humeral fractures in over 65 years old patients. Muscles Ligaments Tendons J. 2017;7:271–278. doi: 10.11138/mltj/2017.7.2.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Giles J.W., Langohr G.D., Johnson J.A., Athwal G.S. Implant design variations in reverse total shoulder arthroplasty influence the required deltoid force and resultant joint load. Clin Orthop Relat Res. 2015;473:3615–3626. doi: 10.1007/s11999-015-4526-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Giuseffi S.A., Streubel P., Sperling J., Sanchez-Sotelo J. Short-stem uncemented primary reverse shoulder arthroplasty: clinical and radiological outcomes. Bone Joint J. 2014;96-B:526–529. doi: 10.1302/0301-620x.96b3.32702. [DOI] [PubMed] [Google Scholar]
- 88.Gobezie R., Shishani Y., Lederman E., Denard P.J. Can a functional difference be detected in reverse arthroplasty with 135° versus 155° prosthesis for the treatment of rotator cuff arthropathy: a prospective randomized study. J Shoulder Elbow Surg. 2019;28:813–818. doi: 10.1016/j.jse.2018.11.064. [DOI] [PubMed] [Google Scholar]
- 89.Grammont P.M., Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–68. doi: 10.3928/0147-7447-19930101-11. [DOI] [PubMed] [Google Scholar]
- 90.Greiner S.H., Back D.A., Herrmann S., Perka C., Asbach P. Degenerative changes of the deltoid muscle have impact on clinical outcome after reversed total shoulder arthroplasty. Arch Orthop Trauma Surg. 2010;130:177–183. doi: 10.1007/s00402-009-1001-y. [DOI] [PubMed] [Google Scholar]
- 91.Groh G.I., Groh G.M. Complications rates, reoperation rates, and the learning curve in reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:388–394. doi: 10.1016/j.jse.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 92.Grubhofer F., Wieser K., Meyer D.C., Catanzaro S., Beeler S., Riede U. Reverse total shoulder arthroplasty for acute head-splitting, 3- and 4-part fractures of the proximal humerus in the elderly. J Shoulder Elbow Surg. 2016;25:1690–1698. doi: 10.1016/j.jse.2016.02.024. [DOI] [PubMed] [Google Scholar]
- 93.Grubhofer F., Wieser K., Meyer D.C., Catanzaro S., Schürholz K., Gerber C. Reverse total shoulder arthroplasty for failed open reduction and internal fixation of fractures of the proximal humerus. J Shoulder Elbow Surg. 2017;26:92–100. doi: 10.1016/j.jse.2016.05.020. [DOI] [PubMed] [Google Scholar]
- 94.Gupta A., Thussbas C., Koch M., Seebauer L. Management of glenoid bone defects with reverse shoulder arthroplasty-surgical technique and clinical outcomes. J Shoulder Elbow Surg. 2018;27:853–862. doi: 10.1016/j.jse.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 95.Gupta A.K., Chalmers P.N., Rahman Z., Bruce B., Harris J.D., McCormick F. Reverse total shoulder arthroplasty in patients of varying body mass index. J Shoulder Elbow Surg. 2014;23:35–42. doi: 10.1016/j.jse.2013.07.043. [DOI] [PubMed] [Google Scholar]
- 96.Hamid N., Connor P.M., Fleischli J.F., D'Alessandro D.F. Acromial fracture after reverse shoulder arthroplasty. Am J Orthop (Belle Mead NJ) 2011;40:E125–E129. [PubMed] [Google Scholar]
- 97.Hamilton M.A., Diep P., Roche C., Flurin P.H., Wright T.W., Zuckerman J.D. Effect of reverse shoulder design philosophy on muscle moment arms. J Orthop Res. 2015;33:605–613. doi: 10.1002/jor.22803. [DOI] [PubMed] [Google Scholar]
- 98.Harmsen S., Casagrande D., Norris T. "Shaped" humeral head autograft reverse shoulder arthroplasty: treatment for primary glenohumeral osteoarthritis with significant posterior glenoid bone loss (B2, B3, and C type) Orthopade. 2017;46:1045–1054. doi: 10.1007/s00132-017-3497-0. [DOI] [PubMed] [Google Scholar]
- 99.Harmsen S.M., Norris T.R. Radiographic changes and clinical outcomes associated with an adjustable diaphyseal press-fit humeral stem in primary reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1589–1597. doi: 10.1016/j.jse.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 100.Hartel B.P., Alta T.D., Sewnath M.E., Willems W.J. Difference in clinical outcome between total shoulder arthroplasty and reverse shoulder arthroplasty used in hemiarthroplasty revision surgery. Int J Shoulder Surg. 2015;9:69–73. doi: 10.4103/0973-6042.161426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hartzler R.U., Steen B.M., Hussey M.M., Cusick M.C., Cottrell B.J., Clark R.E. Reverse shoulder arthroplasty for massive rotator cuff tear: risk factors for poor functional improvement. J Shoulder Elbow Surg. 2015;24:1698–1706. doi: 10.1016/j.jse.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 102.Hasan S.S., Gordon M.P., Ramsey J.A., Levy M.S. Reverse shoulder arthroplasty using an implant with a lateral center of rotation: outcomes, complications, and the influence of experience. Am J Orthop (Belle Mead NJ) 2014;43:E194–E199. [PubMed] [Google Scholar]
- 103.Hasler A., Fornaciari P., Jungwirth-Weinberger A., Jentzsch T., Wieser K., Gerber C. Reverse shoulder arthroplasty in the treatment of glenohumeral instability. J Shoulder Elbow Surg. 2019;28:1587–1594. doi: 10.1016/j.jse.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 104.Hatta T., Werthel J.D., Wagner E.R., Itoi E., Steinmann S.P., Cofield R.H. Effect of smoking on complications following primary shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1–6. doi: 10.1016/j.jse.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 105.Hattrup S.J. The influence of postoperative acromial and scapular spine fractures on the results of reverse shoulder arthroplasty. Orthopedics. 2010;33 doi: 10.3928/01477447-20100329-04. [DOI] [PubMed] [Google Scholar]
- 106.Hattrup S.J., Sanchez-Sotelo J., Sperling J.W., Cofield R.H. Reverse shoulder replacement for patients with inflammatory arthritis. J Hand Surg Am. 2012;37:1888–1894. doi: 10.1016/j.jhsa.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 107.Hattrup S.J., Waldrop R., Sanchez-Sotelo J. Reverse total shoulder arthroplasty for posttraumatic sequelae. J Orthop Trauma. 2016;30:e41–e47. doi: 10.1097/bot.0000000000000416. [DOI] [PubMed] [Google Scholar]
- 108.Hernandez N.M., Chalmers B.P., Wagner E.R., Sperling J.W., Cofield R.H., Sanchez-Sotelo J. Revision to reverse total shoulder arthroplasty restores stability for patients with unstable shoulder prostheses. Clin Orthop Relat Res. 2017;475:2716–2722. doi: 10.1007/s11999-017-5429-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hess F., Zettl R., Smolen D., Knoth C. Anatomical reconstruction to treat acromion fractures following reverse shoulder arthroplasty. Int Orthop. 2018;42:875–881. doi: 10.1007/s00264-017-3710-0. [DOI] [PubMed] [Google Scholar]
- 110.Holcomb J.O., Hebert D.J., Mighell M.A., Dunning P.E., Pupello D.R., Pliner M.D. Reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Shoulder Elbow Surg. 2010;19:1076–1084. doi: 10.1016/j.jse.2009.11.049. [DOI] [PubMed] [Google Scholar]
- 111.Holschen M., Franetzki B., Witt K.A., Liem D., Steinbeck J. Conversions from anatomic shoulder replacements to reverse total shoulder arthroplasty: do the indications for initial surgery influence the clinical outcome after revision surgery? Arch Orthop Trauma Surg. 2017;137:167–172. doi: 10.1007/s00402-016-2595-5. [DOI] [PubMed] [Google Scholar]
- 112.Holschen M., Franetzki B., Witt K.A., Liem D., Steinbeck J. Is reverse total shoulder arthroplasty a feasible treatment option for failed shoulder arthroplasty? A retrospective study of 44 cases with special regards to stemless and stemmed primary implants. Musculoskelet Surg. 2017;101:173–180. doi: 10.1007/s12306-017-0467-y. [DOI] [PubMed] [Google Scholar]
- 113.Holschen M., Siemes M.K., Witt K.A., Steinbeck J. Five-year outcome after conversion of a hemiarthroplasty when used for the treatment of a proximal humeral fracture to a reverse total shoulder arthroplasty. Bone Joint J. 2018;100-B:761–766. doi: 10.1302/0301-620x.100b6.Bjj-2017-1280.R1. [DOI] [PubMed] [Google Scholar]
- 114.Huri G., Familiari F., Salari N., Petersen S.A., Doral M.N., McFarland E.G. Prosthetic design of reverse shoulder arthroplasty contributes to scapular notching and instability. World J Orthop. 2016;7:738–745. doi: 10.5312/wjo.v7.i11.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hussey M.M., Hussey S.E., Mighell M.A. Reverse shoulder arthroplasty as a salvage procedure after failed internal fixation of fractures of the proximal humerus: outcomes and complications. Bone Joint J. 2015;97-B:967–972. doi: 10.1302/0301-620x.97b7.35713. [DOI] [PubMed] [Google Scholar]
- 116.Iacobellis C., Berizzi A., Biz C., Camporese A. Treatment of proximal humeral fractures with reverse shoulder arthroplasty in elderly patients. Musculoskelet Surg. 2015;99:39–44. doi: 10.1007/s12306-014-0331-2. [DOI] [PubMed] [Google Scholar]
- 117.Jehan S., Eltayeb M., Javaid M.M. Delta reverse polarity shoulder replacement: single surgeon experience with a minimum 2-year follow-up. Clin Orthop Surg. 2015;7:359–364. doi: 10.4055/cios.2015.7.3.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Jeong J.J., Kong C.G., Park S.E., Ji J.H., Whang W.H., Choi B.S. Non-fracture stem vs fracture stem of reverse total shoulder arthroplasty in complex proximal humeral fracture of asian elderly. Arch Orthop Trauma Surg. 2019;139:1649–1657. doi: 10.1007/s00402-019-03190-y. [DOI] [PubMed] [Google Scholar]
- 119.Ji J.H., Jeong J.Y., Song H.S., Ok J.H., Yang S.J., Jeon B.K. Early clinical results of reverse total shoulder arthroplasty in the Korean population. J Shoulder Elbow Surg. 2013;22:1102–1107. doi: 10.1016/j.jse.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 120.Jobin C.M., Brown G.D., Bahu M.J., Gardner T.R., LU Bigliani, Levine W.N. Reverse total shoulder arthroplasty for cuff tear arthropathy: the clinical effect of deltoid lengthening and center of rotation medialization. J Shoulder Elbow Surg. 2012;21:1269–1277. doi: 10.1016/j.jse.2011.08.049. [DOI] [PubMed] [Google Scholar]
- 121.Johnson C.C., Sodha S., Garzon-Muvdi J., Petersen S.A., McFarland E.G. Does preoperative American Society of Anesthesiologists score relate to complications after total shoulder arthroplasty? Clin Orthop Relat Res. 2014;472:1589–1596. doi: 10.1007/s11999-013-3400-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Jones R.B., Wright T.W., Roche C.P. Bone grafting the glenoid versus use of augmented glenoid baseplates with reverse shoulder arthroplasty. Bull Hosp Jt Dis (2013) 2015;73(Suppl 1):S129–S135. [PubMed] [Google Scholar]
- 123.Jones R.B., Wright T.W., Zuckerman J.D. Reverse total shoulder arthroplasty with structural bone grafting of large glenoid defects. J Shoulder Elbow Surg. 2016;25:1425–1432. doi: 10.1016/j.jse.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 124.Jonušas J., Banytė R., Ryliškis S. Clinical and radiological outcomes after reverse shoulder arthroplasty with less medialized endoprosthesis after mean follow-up time of 45 months. Arch Orthop Trauma Surg. 2017;137:1201–1205. doi: 10.1007/s00402-017-2751-6. [DOI] [PubMed] [Google Scholar]
- 125.Kaisidis A., Pantos P.G., Heger H., Bochlos D., Selimas S., Oikonomoulas V. Reverse shoulder arthroplasty for the treatment of three and four part fractures of the proximal humerus in patients older than 75 years old. Acta Orthop Belg. 2014;80:99–105. [PubMed] [Google Scholar]
- 126.Kang J.R., Dubiel M.J., Cofield R.H., Steinmann S.P., Elhassan B.T., Morrey M.E. Primary reverse shoulder arthroplasty using contemporary implants is associated with very low reoperation rates. J Shoulder Elbow Surg. 2019;28:S175–S180. doi: 10.1016/j.jse.2019.01.026. [DOI] [PubMed] [Google Scholar]
- 127.Katz D., Valenti P., Kany J., Elkholti K., Werthel J.D. Does lateralisation of the centre of rotation in reverse shoulder arthroplasty avoid scapular notching? Clinical and radiological review of one hundred and forty cases with forty five months of follow-up. Int Orthop. 2016;40:99–108. doi: 10.1007/s00264-015-2976-3. [DOI] [PubMed] [Google Scholar]
- 128.Kelly J.D., 2nd, Zhao J.X., Hobgood E.R., Norris T.R. Clinical results of revision shoulder arthroplasty using the reverse prosthesis. J Shoulder Elbow Surg. 2012;21:1516–1525. doi: 10.1016/j.jse.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 129.Kempton L.B., Ankerson E., Wiater J.M. A complication-based learning curve from 200 reverse shoulder arthroplasties. Clin Orthop Relat Res. 2011;469:2496–2504. doi: 10.1007/s11999-011-1811-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kennon J.C., Lu C., McGee-Lawrence M.E., Crosby L.A. Scapula fracture incidence in reverse total shoulder arthroplasty using screws above or below metaglene central cage: clinical and biomechanical outcomes. J Shoulder Elbow Surg. 2017;26:1023–1030. doi: 10.1016/j.jse.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 131.Kiet T.K., Feeley B.T., Naimark M., Gajiu T., Hall S.L., Chung T.T. Outcomes after shoulder replacement: comparison between reverse and anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:179–185. doi: 10.1016/j.jse.2014.06.039. [DOI] [PubMed] [Google Scholar]
- 132.King J.J., Dalton S.S., Gulotta L.V., Wright T.W., Schoch B.S. How common are acromial and scapular spine fractures after reverse shoulder arthroplasty? A systematic review. Bone Joint J. 2019;101-B:627–634. doi: 10.1302/0301-620X.101B6.BJJ-2018-1187.R1. [DOI] [PubMed] [Google Scholar]
- 133.King J.J., Farmer K.W., Struk A.M., Wright T.W. Uncemented versus cemented humeral stem fixation in reverse shoulder arthroplasty. Int Orthop. 2015;39:291–298. doi: 10.1007/s00264-014-2593-6. [DOI] [PubMed] [Google Scholar]
- 134.Kirzner N., Paul E., Moaveni A. Reverse shoulder arthroplasty vs BIO-RSA: clinical and radiographic outcomes at short term follow-up. J Orthop Surg Res. 2018;13:256. doi: 10.1186/s13018-018-0955-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Klein S.M., Dunning P., Mulieri P., Pupello D., Downes K., Frankle M.A. Effects of acquired glenoid bone defects on surgical technique and clinical outcomes in reverse shoulder arthroplasty. J Bone Joint Surg Am. 2010;92:1144–1154. doi: 10.2106/jbjs.I.00778. [DOI] [PubMed] [Google Scholar]
- 136.Klug A., Wincheringer D., Harth J., Schmidt-Horlohé K., Hoffmann R., Gramlich Y. Complications after surgical treatment of proximal humerus fractures in the elderly—an analysis of complication patterns and risk factors for reverse shoulder arthroplasty and angular-stable plating. J Shoulder Elbow Surg. 2019;28:1674–1684. doi: 10.1016/j.jse.2019.02.017. [DOI] [PubMed] [Google Scholar]
- 137.Kohan E.M., Chalmers P.N., Salazar D., Keener J.D., Yamaguchi K., Chamberlain A.M. Dislocation following reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1238–1245. doi: 10.1016/j.jse.2016.12.073. [DOI] [PubMed] [Google Scholar]
- 138.Kurowicki J., Triplet J.J., Momoh E., Moor M.A., Levy J.C. Reverse shoulder prosthesis in the treatment of locked anterior shoulders: a comparison with classic reverse shoulder indications. J Shoulder Elbow Surg. 2016;25:1954–1960. doi: 10.1016/j.jse.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 139.Lädermann A., Denard P.J., Tirefort J., Collin P., Nowak A., Schwitzguebel A.J. Subscapularis- and deltoid-sparing vs traditional deltopectoral approach in reverse shoulder arthroplasty: a prospective case-control study. J Orthop Surg Res. 2017;12:112. doi: 10.1186/s13018-017-0617-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lädermann A., Edwards T.B., Walch G. Arm lengthening after reverse shoulder arthroplasty: a review. Int Orthop. 2014;38:991–1000. doi: 10.1007/s00264-013-2175-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ladermann A., Walch G., Denard P.J., Collin P., Sirveaux F., Favard L. Reverse shoulder arthroplasty in patients with pre-operative impairment of the deltoid muscle. Bone Joint J. 2013;95-B:1106–1113. doi: 10.1302/0301-620X.95B8.31173. [DOI] [PubMed] [Google Scholar]
- 142.Lanzone R., Carbone S., Albino P., Cassio J.B., Métais P. Retroverted glenoid reconstruction using glenoid plate in reverse shoulder arthroplasty. Musculoskelet Surg. 2017;101:121–127. doi: 10.1007/s12306-017-0481-0. [DOI] [PubMed] [Google Scholar]
- 143.Leathers M.P., Ialenti M.N., Feeley B.T., Zhang A.L., Ma C.B. Do younger patients have better results after reverse total shoulder arthroplasty? J Shoulder Elbow Surg. 2018;27:S24–S28. doi: 10.1016/j.jse.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 144.Lehtimäki K., Rasmussen J.V., Mokka J., Salomonsson B., Hole R., Jensen S.L. Risk and risk factors for revision after primary reverse shoulder arthroplasty for cuff tear arthropathy and osteoarthritis: a Nordic Arthroplasty Register Association study. J Shoulder Elbow Surg. 2018;27:1596–1601. doi: 10.1016/j.jse.2018.02.060. [DOI] [PubMed] [Google Scholar]
- 145.Lenarz C., Shishani Y., McCrum C., Nowinski R.J., Edwards T.B., Gobezie R. Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop Relat Res. 2011;469:3324–3331. doi: 10.1007/s11999-011-2055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Leonidou A., Virani S., Buckle C., Yeoh C., Relwani J. Reverse shoulder arthroplasty with a cementless short metaphyseal humeral prosthesis without a stem: survivorship, early to mid-term clinical and radiological outcomes in a prospective study from an independent centre. Eur J Orthop Surg Traumatol. 2020;30:89–96. doi: 10.1007/s00590-019-02531-2. [DOI] [PubMed] [Google Scholar]
- 147.Leung B., Horodyski M., Struk A.M., Wright T.W. Functional outcome of hemiarthroplasty compared with reverse total shoulder arthroplasty in the treatment of rotator cuff tear arthropathy. J Shoulder Elbow Surg. 2012;21:319–323. doi: 10.1016/j.jse.2011.05.023. [DOI] [PubMed] [Google Scholar]
- 148.Levy J.C., Anderson C., Samson A. Classification of postoperative acromial fractures following reverse shoulder arthroplasty. J Bone Joint Surg Am. 2013;95:e104. doi: 10.2106/JBJS.K.01516. [DOI] [PubMed] [Google Scholar]
- 149.Levy J.C., Berglund D., Vakharia R., DeVito P., Tahal D.S., Mijc D. Primary monoblock inset reverse shoulder arthroplasty resulted in decreased pain and improved function. Clin Orthop Relat Res. 2019;477:2097–2108. doi: 10.1097/corr.0000000000000761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Levy O., Narvani A., Hous N., Abraham R., Relwani J., Pradhan R. Reverse shoulder arthroplasty with a cementless short metaphyseal humeral implant without a stem: clinical and radiologic outcomes in prospective 2- to 7-year follow-up study. J Shoulder Elbow Surg. 2016;25:1362–1370. doi: 10.1016/j.jse.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 151.Levy O., Walecka J., Arealis G., Tsvieli O., Della Rotonda G., Abraham R. Bilateral reverse total shoulder arthroplasty—functional outcome and activities of daily living. J Shoulder Elbow Surg. 2017;26:e85–e96. doi: 10.1016/j.jse.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 152.Lindbloom B.J., Christmas K.N., Downes K., Simon P., McLendon P.B., Hess A.V., 2nd Is there a relationship between preoperative diagnosis and clinical outcomes in reverse shoulder arthroplasty? An experience in 699 shoulders. J Shoulder Elbow Surg. 2019;28:S110–S117. doi: 10.1016/j.jse.2019.04.007. [DOI] [PubMed] [Google Scholar]
- 153.Lopiz Y., Alcobía-Díaz B., Galán-Olleros M., García-Fernández C., Picado A.L., Marco F. Reverse shoulder arthroplasty versus nonoperative treatment for 3- or 4-part proximal humeral fractures in elderly patients: a prospective randomized controlled trial. J Shoulder Elbow Surg. 2019;28:2259–2271. doi: 10.1016/j.jse.2019.06.024. [DOI] [PubMed] [Google Scholar]
- 154.Lopiz Y., García-Coiradas J., Serrano-Mateo L., García-Fernández C., Marco F. Reverse shoulder arthroplasty for acute proximal humeral fractures in the geriatric patient: results, health-related quality of life and complication rates. Int Orthop. 2016;40:771–781. doi: 10.1007/s00264-015-3085-z. [DOI] [PubMed] [Google Scholar]
- 155.Lopiz Y., García-Fernández C., Arriaza A., Rizo B., Marcelo H., Marco F. Midterm outcomes of bone grafting in glenoid defects treated with reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1581–1588. doi: 10.1016/j.jse.2017.01.017. [DOI] [PubMed] [Google Scholar]
- 156.Lópiz Y., Rodríguez-González A., García-Fernández C., Marco F. Scapula insufficiency fractures after reverse total shoulder arthroplasty in rotator cuff arthropathy: what is their functional impact? Rev Esp Cir Ortop Traumatol. 2015;59:318–325. doi: 10.1016/j.recot.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 157.Luciani P., Farinelli L., Procaccini R., Verducci C., Gigante A. Primary reverse shoulder arthroplasty for acute proximal humerus fractures: A 5-year long term retrospective study of elderly patients. Injury. 2019;50:1974–1977. doi: 10.1016/j.injury.2019.09.019. [DOI] [PubMed] [Google Scholar]
- 158.Lunden L.K., Kleggetveit I.P., Jorum E. Delayed diagnosis and worsening of pain following orthopedic surgery in patients with complex regional pain syndrome (CRPS) Scand J Pain. 2016;11:27–33. doi: 10.1016/j.sjpain.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 159.Mahure S., Mollon B., Quien M., Karia R., Zuckerman J., Kwon Y. Impact of diabetes on perioperative complications in patients undergoing elective total shoulder arthroplasty. Bull Hosp Jt Dis (2013) 2017;75:173–179. [PubMed] [Google Scholar]
- 160.Mahylis J.M., Puzzitiello R.N., Ho J.C., Amini M.H., Iannotti J.P., Ricchetti E.T. Comparison of radiographic and clinical outcomes of revision reverse total shoulder arthroplasty with structural versus nonstructural bone graft. J Shoulder Elbow Surg. 2019;28:e1–e9. doi: 10.1016/j.jse.2018.06.026. [DOI] [PubMed] [Google Scholar]
- 161.Mangano T., Cerruti P., Repetto I., Felli L., Ivaldo N., Giovale M. Reverse shoulder arthroplasty in older patients: is it worth it? A subjective functional outcome and quality of life survey. Aging Clin Exp Res. 2016;28:925–933. doi: 10.1007/s40520-015-0493-2. [DOI] [PubMed] [Google Scholar]
- 162.Mangold D.R., Wagner E.R., Cofield R.H., Sanchez-Sotelo J., Sperling J.W. Reverse shoulder arthroplasty for rheumatoid arthritis since the introduction of disease-modifying drugs. Int Orthop. 2019;43:2593–2600. doi: 10.1007/s00264-019-04373-3. [DOI] [PubMed] [Google Scholar]
- 163.Martinez A.A., Bejarano C., Carbonel I., Iglesias D., Gil-Albarova J., Herrera A. The treatment of proximal humerus nonunions in older patients with reverse shoulder arthroplasty. Injury. 2012;43(Suppl 2):S3–S6. doi: 10.1016/s0020-1383(13)70172-4. [DOI] [PubMed] [Google Scholar]
- 164.Martinez A.A., Calvo A., Bejarano C., Carbonel I., Herrera A. The use of the Lima reverse shoulder arthroplasty for the treatment of fracture sequelae of the proximal humerus. J Orthop Sci. 2012;17:141–147. doi: 10.1007/s00776-011-0185-5. [DOI] [PubMed] [Google Scholar]
- 165.Matsuki K., King J.J., Wright T.W., Schoch B.S. Outcomes of reverse shoulder arthroplasty in small- and large-stature patients. J Shoulder Elbow Surg. 2018;27:808–815. doi: 10.1016/j.jse.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 166.Matthews C.J., Wright T.W., Farmer K.W., Struk A.M., Vasilopoulos T., King J.J. Outcomes of primary reverse total shoulder arthroplasty in patients younger than 65 years old. J Hand Surg Am. 2019;44:104–111. doi: 10.1016/j.jhsa.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 167.Mattiassich G., Marcovici L.L., Krifter R.M., Ortmaier R., Wegerer P., Kroepfl A. Delta III reverse shoulder arthroplasty in the treatment of complex 3- and 4-part fractures of the proximal humerus: 6 to 42 months of follow up. BMC Musculoskelet Disord. 2013;14:231. doi: 10.1186/1471-2474-14-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Mayne I.P., Bell S.N., Wright W., Coghlan J.A. Acromial and scapular spine fractures after reverse total shoulder arthroplasty. Shoulder Elbow. 2016;8:90–100. doi: 10.1177/1758573216628783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.McFarland E.G., Huri G., Hyun Y.S., Petersen S.A., Srikumaran U. Reverse total shoulder arthroplasty without bone-grafting for severe glenoid bone loss in patients with osteoarthritis and intact rotator cuff. J Bone Joint Surg Am. 2016;98:1801–1807. doi: 10.2106/jbjs.15.01181. [DOI] [PubMed] [Google Scholar]
- 170.Melis B., Bonnevialle N., Neyton L., Lévigne C., Favard L., Walch G. Glenoid loosening and failure in anatomical total shoulder arthroplasty: is revision with a reverse shoulder arthroplasty a reliable option? J Shoulder Elbow Surg. 2012;21:342–349. doi: 10.1016/j.jse.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 171.Mellano C.R., Kupfer N., Thorsness R., Chalmers P.N., Feldheim T.F., O'Donnell P. Functional results of bilateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:990–996. doi: 10.1016/j.jse.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 172.Merolla G., Tartarone A., Sperling J.W., Paladini P., Fabbri E., Porcellini G. Early clinical and radiological outcomes of reverse shoulder arthroplasty with an eccentric all-polyethylene glenosphere to treat failed hemiarthroplasty and the sequelae of proximal humeral fractures. Int Orthop. 2017;41:141–148. doi: 10.1007/s00264-016-3188-1. [DOI] [PubMed] [Google Scholar]
- 173.Merolla G., Wagner E., Sperling J.W., Paladini P., Fabbri E., Porcellini G. Revision of failed shoulder hemiarthroplasty to reverse total arthroplasty: analysis of 157 revision implants. J Shoulder Elbow Surg. 2018;27:75–81. doi: 10.1016/j.jse.2017.06.038. [DOI] [PubMed] [Google Scholar]
- 174.Merolla G., Walch G., Ascione F., Paladini P., Fabbri E., Padolino A. Grammont humeral design versus onlay curved-stem reverse shoulder arthroplasty: comparison of clinical and radiographic outcomes with minimum 2-year follow-up. J Shoulder Elbow Surg. 2018;27:701–710. doi: 10.1016/j.jse.2017.10.016. [DOI] [PubMed] [Google Scholar]
- 175.Michael Wiater J., Carpenter S., Koueiter D.M., Marcantonio D., Wiater B.P. Influence of body mass index on clinical outcomes in reverse total shoulder arthroplasty. J Surg Orthop Adv. 2017;26:134–142. [PubMed] [Google Scholar]
- 176.Middleton C., Uri O., Phillips S., Barmpagiannis K., Higgs D., Falworth M. A reverse shoulder arthroplasty with increased offset for the treatment of cuff-deficient shoulders with glenohumeral arthritis. Bone Joint J. 2014;96-B:936–942. doi: 10.1302/0301-620x.96b7.32946. [DOI] [PubMed] [Google Scholar]
- 177.Mizuno N., Denard P.J., Raiss P., Walch G. The clinical and radiographical results of reverse total shoulder arthroplasty with eccentric glenosphere. Int Orthop. 2012;36:1647–1653. doi: 10.1007/s00264-012-1539-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Mizuno N., Denard P.J., Raiss P., Walch G. Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Joint Surg Am. 2013;95:1297–1304. doi: 10.2106/jbjs.L.00820. [DOI] [PubMed] [Google Scholar]
- 179.Moeini S., Rasmussen J.V., Salomonsson B., Domeij-Arverud E., Fenstad A.M., Hole R. Reverse shoulder arthroplasty has a higher risk of revision due to infection than anatomical shoulder arthroplasty: 17 730 primary shoulder arthroplasties from the Nordic Arthroplasty Register Association. Bone Joint J. 2019;101-B:702–707. doi: 10.1302/0301-620x.101b6.Bjj-2018-1348.R1. [DOI] [PubMed] [Google Scholar]
- 180.Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. W264. [DOI] [PubMed] [Google Scholar]
- 181.Mollon B., Mahure S.A., Roche C.P., Zuckerman J.D. Impact of glenosphere size on clinical outcomes after reverse total shoulder arthroplasty: an analysis of 297 shoulders. J Shoulder Elbow Surg. 2016;25:763–771. doi: 10.1016/j.jse.2015.10.027. [DOI] [PubMed] [Google Scholar]
- 182.Mollon B., Mahure S.A., Roche C.P., Zuckerman J.D. Impact of scapular notching on clinical outcomes after reverse total shoulder arthroplasty: an analysis of 476 shoulders. J Shoulder Elbow Surg. 2017;26:1253–1261. doi: 10.1016/j.jse.2016.11.043. [DOI] [PubMed] [Google Scholar]
- 183.Moroder P., Ernstbrunner L., Zweiger C., Schatz M., Seitlinger G., Skursky R. Short to mid-term results of stemless reverse shoulder arthroplasty in a selected patient population compared to a matched control group with stem. Int Orthop. 2016;40:2115–2120. doi: 10.1007/s00264-016-3249-5. [DOI] [PubMed] [Google Scholar]
- 184.Morris B.J., Haigler R.E., Cochran J.M., Laughlin M.S., Elkousy H.A., Gartsman G.M. Obesity has minimal impact on short-term functional scores after reverse shoulder arthroplasty for rotator cuff tear arthropathy. Am J Orthop (Belle Mead NJ) 2016;45:E180–E186. [PubMed] [Google Scholar]
- 185.Muh S.J., Streit J.J., Wanner J.P., Lenarz C.J., Shishani Y., Rowland D.Y. Early follow-up of reverse total shoulder arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2013;95:1877–1883. doi: 10.2106/jbjs.L.10005. [DOI] [PubMed] [Google Scholar]
- 186.Mulieri P., Dunning P., Klein S., Pupello D., Frankle M. Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg Am. 2010;92:2544–2556. doi: 10.2106/jbjs.I.00912. [DOI] [PubMed] [Google Scholar]
- 187.Müller A.M., Born M., Jung C., Flury M., Kolling C., Schwyzer H.K. Glenosphere size in reverse shoulder arthroplasty: is larger better for external rotation and abduction strength? J Shoulder Elbow Surg. 2018;27:44–52. doi: 10.1016/j.jse.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 188.Natera L., Bruguera J., Atoun E., Levy O. Revision shoulder arthroplasty from resurfacing to non-cemented short-stem reverse prosthesis. Rev Esp Cir Ortop Traumatol. 2016;60:175–183. doi: 10.1016/j.recot.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 189.Naveed M.A., Kitson J., Bunker T.D. The Delta III reverse shoulder replacement for cuff tear arthropathy: a single-centre study of 50 consecutive procedures. J Bone Joint Surg Br. 2011;93:57–61. doi: 10.1302/0301-620x.93b1.24218. [DOI] [PubMed] [Google Scholar]
- 190.Neyton L., Erickson J., Ascione F., Bugelli G., Lunini E., Walch G. Grammont Award 2018: Scapular fractures in reverse shoulder arthroplasty (Grammont style): prevalence, functional, and radiographic results with minimum 5-year follow-up. J Shoulder Elbow Surg. 2019;28:260–267. doi: 10.1016/j.jse.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 191.Nolan B.M., Ankerson E., Wiater J.M. Reverse total shoulder arthroplasty improves function in cuff tear arthropathy. Clin Orthop Relat Res. 2011;469:2476–2482. doi: 10.1007/s11999-010-1683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Ohl X., Bonnevialle N., Gallinet D., Ramdane N., Valenti P., Decroocq L. How the greater tuberosity affects clinical outcomes after reverse shoulder arthroplasty for proximal humeral fractures. J Shoulder Elbow Surg. 2018;27:2139–2144. doi: 10.1016/j.jse.2018.05.030. [DOI] [PubMed] [Google Scholar]
- 193.Ortmaier R., Mattiassich G., Pumberger M., Hitzl W., Moroder P., Auffarth A. Comparison between reverse shoulder arthroplasty and Humerusblock in three- and four-part proximal humerus fractures in elderly patients. Int Orthop. 2015;39:335–342. doi: 10.1007/s00264-014-2433-8. [DOI] [PubMed] [Google Scholar]
- 194.Ortmaier R., Resch H., Matis N., Blocher M., Auffarth A., Mayer M. Reverse shoulder arthroplasty in revision of failed shoulder arthroplasty-outcome and follow-up. Int Orthop. 2013;37:67–75. doi: 10.1007/s00264-012-1742-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Otto R.J., Clark R.E., Frankle M.A. Reverse shoulder arthroplasty in patients younger than 55 years: 2- to 12-year follow-up. J Shoulder Elbow Surg. 2017;26:792–797. doi: 10.1016/j.jse.2016.09.051. [DOI] [PubMed] [Google Scholar]
- 196.Otto R.J., Virani N.A., Levy J.C., Nigro P.T., Cuff D.J., Frankle M.A. Scapular fractures after reverse shoulder arthroplasty: evaluation of risk factors and the reliability of a proposed classification. J Shoulder Elbow Surg. 2013;22:1514–1521. doi: 10.1016/j.jse.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 197.Pastor M.F., Kieckbusch M., Kaufmann M., Ettinger M., Wellmann M., Smith T. Reverse shoulder arthroplasty for fracture sequelae: clinical outcome and prognostic factors. J Orthop Sci. 2019;24:237–242. doi: 10.1016/j.jos.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 198.Patel D.N., Young B., Onyekwelu I., Zuckerman J.D., Kwon Y.W. Reverse total shoulder arthroplasty for failed shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21:1478–1483. doi: 10.1016/j.jse.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 199.Poon P.C., Chou J., Young S.W., Astley T. A comparison of concentric and eccentric glenospheres in reverse shoulder arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2014;96:e138. doi: 10.2106/jbjs.M.00941. [DOI] [PubMed] [Google Scholar]
- 200.Puskas B., Harreld K., Clark R., Downes K., Virani N.A., Frankle M. Isometric strength, range of motion, and impairment before and after total and reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:869–876. doi: 10.1016/j.jse.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 201.Puskas G.J., Catanzaro S., Gerber C. Clinical outcome of reverse total shoulder arthroplasty combined with latissimus dorsi transfer for the treatment of chronic combined pseudoparesis of elevation and external rotation of the shoulder. J Shoulder Elbow Surg. 2014;23:49–57. doi: 10.1016/j.jse.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 202.Raiss P., Alami G., Bruckner T., Magosch P., Habermeyer P., Boileau P. Reverse shoulder arthroplasty for type 1 sequelae of a fracture of the proximal humerus. Bone Joint J. 2018;100-B:318–323. doi: 10.1302/0301-620x.100b3.Bjj-2017-0947.R1. [DOI] [PubMed] [Google Scholar]
- 203.Raiss P., Edwards T.B., Collin P., Bruckner T., Zeifang F., Loew M. Reverse shoulder arthroplasty for malunions of the proximal part of the humerus (type-4 fracture sequelae) J Bone Joint Surg Am. 2016;98:893–899. doi: 10.2106/jbjs.15.00506. [DOI] [PubMed] [Google Scholar]
- 204.Raiss P., Edwards T.B., da Silva M.R., Bruckner T., Loew M., Walch G. Reverse shoulder arthroplasty for the treatment of nonunions of the surgical neck of the proximal part of the humerus (type-3 fracture sequelae) J Bone Joint Surg Am. 2014;96:2070–2076. doi: 10.2106/JBJS.N.00405. [DOI] [PubMed] [Google Scholar]
- 205.Raiss P., Schnetzke M., Wittmann T., Kilian C.M., Edwards T.B., Denard P.J. Postoperative radiographic findings of an uncemented convertible short stem for anatomic and reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28:715–723. doi: 10.1016/j.jse.2018.08.037. [DOI] [PubMed] [Google Scholar]
- 206.Rhee Y.G., Cho N.S., Moon S.C. Effects of humeral component retroversion on functional outcomes in reverse total shoulder arthroplasty for cuff tear arthropathy. J Shoulder Elbow Surg. 2015;24:1574–1581. doi: 10.1016/j.jse.2015.03.026. [DOI] [PubMed] [Google Scholar]
- 207.Roberson T.A., Shanley E., Griscom J.T., Granade M., Hunt Q., Adams K.J. Subscapularis repair is unnecessary after lateralized reverse shoulder arthroplasty. JB JS Open Access. 2018;3:e0056. doi: 10.2106/JBJS.OA.17.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Rojas J., Familiari F., Borade A.U., Joseph J., Deune E.G., Ingari J.V. Exposure of the brachial plexus in complex revisions to reverse total shoulder arthroplasty. Int Orthop. 2019;43:2789–2797. doi: 10.1007/s00264-019-04349-3. [DOI] [PubMed] [Google Scholar]
- 209.Ross M., Hope B., Stokes A., Peters S.E., McLeod I., Duke P.F. Reverse shoulder arthroplasty for the treatment of three-part and four-part proximal humeral fractures in the elderly. J Shoulder Elbow Surg. 2015;24:215–222. doi: 10.1016/j.jse.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 210.Routman H.D., Flurin P.H., Wright T.W., Zuckerman J.D., Hamilton M.A., Roche C.P. Reverse shoulder arthroplasty prosthesis design classification system. Bull Hosp Jt Dis (2013) 2015;73(Suppl 1):S5–S14. [PubMed] [Google Scholar]
- 211.Russo R., Della Rotonda G., Cautiero F., Ciccarelli M. Reverse shoulder prosthesis to treat complex proximal humeral fractures in the elderly patients: results after 10-year experience. Musculoskelet Surg. 2015;99(Suppl 1):S17–S23. doi: 10.1007/s12306-015-0367-y. [DOI] [PubMed] [Google Scholar]
- 212.Sadoghi P., Vavken P., Leithner A., Hochreiter J., Weber G., Pietschmann M.F. Impact of previous rotator cuff repair on the outcome of reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20:1138–1146. doi: 10.1016/j.jse.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 213.Saier T., Cotic M., Kirchhoff C., Feucht M.J., Minzlaff P., Glanzmann M.C. Early results after modular non-cemented reverse total shoulder arthroplasty: a prospective single-centre study of 38 consecutive cases. J Orthop Sci. 2015;20:830–836. doi: 10.1007/s00776-015-0734-4. [DOI] [PubMed] [Google Scholar]
- 214.Saltzman B.M., Chalmers P.N., Gupta A.K., Romeo A.A., Nicholson G.P. Complication rates comparing primary with revision reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1647–1654. doi: 10.1016/j.jse.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 215.Samuelsen B.T., Wagner E.R., Houdek M.T., Elhassan B.T., Sánchez-Sotelo J., Cofield R. Primary reverse shoulder arthroplasty in patients aged 65 years or younger. J Shoulder Elbow Surg. 2017;26:e13–e17. doi: 10.1016/j.jse.2016.05.026. [DOI] [PubMed] [Google Scholar]
- 216.Sanchez-Sotelo J., Wagner E.R., Sim F.H., Houdek M.T. Allograft-prosthetic composite reconstruction for massive proximal humeral bone loss in reverse shoulder arthroplasty. J Bone Joint Surg Am. 2017;99:2069–2076. doi: 10.2106/jbjs.16.01495. [DOI] [PubMed] [Google Scholar]
- 217.Santana F., Alentorn-Geli E., Guirro P., Torrens C. Reverse shoulder arthroplasty for fracture sequelae: how the initial fracture treatment influences the outcomes of joint replacement. Acta Orthop Traumatol Turc. 2019;53:278–281. doi: 10.1016/j.aott.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Schirren M., Siebenbürger G., Fleischhacker E., Biermann N., Helfen T., Böcker W. Anterior fracture dislocation of the proximal humerus. Obere Extremität. 2019;14:103–109. doi: 10.1007/s11678-019-0509-1. [DOI] [Google Scholar]
- 219.Schliemann B., Theisen C., Kösters C., Raschke M.J., Weimann A. Reverse total shoulder arthroplasty for type I fracture sequelae after internal fixation of proximal humerus fractures. Arch Orthop Trauma Surg. 2017;137:1677–1683. doi: 10.1007/s00402-017-2789-5. [DOI] [PubMed] [Google Scholar]
- 220.Schneeberger A.G., Müller T.M., Steens W., Thür C. Reverse total shoulder arthroplasty after failed deltoid flap reconstruction. Arch Orthop Trauma Surg. 2014;134:317–323. doi: 10.1007/s00402-013-1908-1. [DOI] [PubMed] [Google Scholar]
- 221.Schnetzke M., Preis A., Coda S., Raiss P., Loew M. Anatomical and reverse shoulder replacement with a convertible, uncemented short-stem shoulder prosthesis: first clinical and radiological results. Arch Orthop Trauma Surg. 2017;137:679–684. doi: 10.1007/s00402-017-2673-3. [DOI] [PubMed] [Google Scholar]
- 222.Schoch B., Aibinder W., Walters J., Sperling J., Throckmorton T., Sanchez-Sotelo J. Outcomes of uncemented versus cemented reverse shoulder arthroplasty for proximal humerus fractures. Orthopedics. 2019;42:e236–e241. doi: 10.3928/01477447-20190125-03. [DOI] [PubMed] [Google Scholar]
- 223.Sebastiá-Forcada E., Cebrián-Gómez R., Lizaur-Utrilla A., Gil-Guillén V. Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J Shoulder Elbow Surg. 2014;23:1419–1426. doi: 10.1016/j.jse.2014.06.035. [DOI] [PubMed] [Google Scholar]
- 224.Sebastia-Forcada E., Lizaur-Utrilla A., Cebrian-Gomez R., Miralles-Muñoz F.A., Lopez-Prats F.A. Outcomes of reverse total shoulder arthroplasty for proximal humeral fractures: primary arthroplasty versus secondary arthroplasty after failed proximal humeral locking plate fixation. J Orthop Trauma. 2017;31:e236–e240. doi: 10.1097/bot.0000000000000858. [DOI] [PubMed] [Google Scholar]
- 225.Sershon R.A., Van Thiel G.S., Lin E.C., McGill K.C., Cole B.J., Verma N.N. Clinical outcomes of reverse total shoulder arthroplasty in patients aged younger than 60 years. J Shoulder Elbow Surg. 2014;23:395–400. doi: 10.1016/j.jse.2013.07.047. [DOI] [PubMed] [Google Scholar]
- 226.Shafritz A.B., Flieger S. Reverse total shoulder arthroplasty: early results of forty-one cases and a review of the literature. Hand Clin. 2012;28:469–479. doi: 10.1016/j.hcl.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 227.Shah S.S., Gentile J., Chen X., Kontaxis A., Dines D.M., Warren R.F. Influence of implant design and parasagittal acromial morphology on acromial and scapular spine strain after reverse total shoulder arthroplasty: a cadaveric and computer based biomechanical analysis [Epub ahead of print] J Shoulder Elbow Surg. 2020 doi: 10.1016/j.jse.2020.04.004. [DOI] [PubMed] [Google Scholar]
- 228.Shannon S.F., Wagner E.R., Houdek M.T., Cross W.W., 3rd, Sánchez-Sotelo J. Reverse shoulder arthroplasty for proximal humeral fractures: outcomes comparing primary reverse arthroplasty for fracture versus reverse arthroplasty after failed osteosynthesis. J Shoulder Elbow Surg. 2016;25:1655–1660. doi: 10.1016/j.jse.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 229.Sheth M.M., Sholder D., Getz C.L., Williams G.R., Namdari S. Revision of failed hemiarthroplasty and anatomic total shoulder arthroplasty to reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28:1074–1081. doi: 10.1016/j.jse.2018.10.026. [DOI] [PubMed] [Google Scholar]
- 230.Shi L.L., Cahill K.E., Ek E.T., Tompson J.D., Higgins L.D., Warner J.J. Latissimus dorsi and teres major transfer with reverse shoulder arthroplasty restores active motion and reduces pain for posterosuperior cuff dysfunction. Clin Orthop Relat Res. 2015;473:3212–3217. doi: 10.1007/s11999-015-4433-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Shields E., Wiater J.M. Patient outcomes after revision of anatomic total shoulder arthroplasty to reverse shoulder arthroplasty for rotator cuff failure or component loosening: a matched cohort study. J Am Acad Orthop Surg. 2019;27:e193–e198. doi: 10.5435/jaaos-d-17-00350. [DOI] [PubMed] [Google Scholar]
- 232.Shields E.J.W., Koueiter D.M., Maerz T., Schwark A., Wiater J.M. Previous rotator cuff repair is associated with inferior clinical outcomes after reverse total shoulder arthroplasty. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117730311. 2325967117730311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Simovitch R., Flurin P.H., Wright T.W., Zuckerman J.D., Roche C. Impact of scapular notching on reverse total shoulder arthroplasty midterm outcomes: 5-year minimum follow-up. J Shoulder Elbow Surg. 2019;28:2301–2307. doi: 10.1016/j.jse.2019.04.042. [DOI] [PubMed] [Google Scholar]
- 234.Simovitch R.W., Gerard B.K., Brees J.A., Fullick R., Kearse J.C. Outcomes of reverse total shoulder arthroplasty in a senior athletic population. J Shoulder Elbow Surg. 2015;24:1481–1585. doi: 10.1016/j.jse.2015.03.011. [DOI] [PubMed] [Google Scholar]
- 235.Singh A., Yian E.H., Dillon M.T., Takayanagi M., Burke M.F., Navarro R.A. The effect of surgeon and hospital volume on shoulder arthroplasty perioperative quality metrics. J Shoulder Elbow Surg. 2014;23:1187–1194. doi: 10.1016/j.jse.2013.11.017. [DOI] [PubMed] [Google Scholar]
- 236.Somerson J.S., Hsu J.E., Neradilek M.B., Matsen F.A., 3rd Analysis of 4063 complications of shoulder arthroplasty reported to the US Food and Drug Administration from 2012 to 2016. J Shoulder Elbow Surg. 2018;27:1978–1986. doi: 10.1016/j.jse.2018.03.025. [DOI] [PubMed] [Google Scholar]
- 237.Statz J.M., Wagner E.R., Houdek M.T., Cofield R.H., Sanchez-Sotelo J., Elhassan B.T. Outcomes of primary reverse shoulder arthroplasty in patients with morbid obesity. J Shoulder Elbow Surg. 2016;25:e191–e198. doi: 10.1016/j.jse.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 238.Stechel A., Fuhrmann U., Irlenbusch L., Rott O., Irlenbusch U. Reversed shoulder arthroplasty in cuff tear arthritis, fracture sequelae, and revision arthroplasty. Acta Orthop. 2010;81:367–372. doi: 10.3109/17453674.2010.487242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Steen B.M., Cabezas A.F., Santoni B.G., Hussey M.M., Cusick M.C., Kumar A.G. Outcome and value of reverse shoulder arthroplasty for treatment of glenohumeral osteoarthritis: a matched cohort. J Shoulder Elbow Surg. 2015;24:1433–1441. doi: 10.1016/j.jse.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 240.Stephens B.C., Simon P., Clark R.E., Christmas K.N., Stone G.P., Lorenzetti A.J. Revision for a failed reverse: a 12-year review of a lateralized implant. J Shoulder Elbow Surg. 2016;25:e115–e124. doi: 10.1016/j.jse.2015.09.027. [DOI] [PubMed] [Google Scholar]
- 241.Stephens S.P., Paisley K.C., Giveans M.R., Wirth M.A. The effect of proximal humeral bone loss on revision reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:1519–1526. doi: 10.1016/j.jse.2015.02.020. [DOI] [PubMed] [Google Scholar]
- 242.Stevens C.G., Murphy M.R., Stevens T.D., Bryant T.L., Wright T.W. Bilateral scapular fractures after reverse shoulder arthroplasties. J Shoulder Elbow Surg. 2015;24:e50–e55. doi: 10.1016/j.jse.2014.09.045. [DOI] [PubMed] [Google Scholar]
- 243.Stevens C.G., Struk A.M., Wright T.W. The functional impact of bilateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1341–1348. doi: 10.1016/j.jse.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 244.Streit J.J., Clark J.C., Allert J., Clark R., Christmas K.N., Mighell M.A. Ten years of reverse total shoulder arthroplasty performed for osteoarthritis and intact rotator cuff: indications and outcomes. J Shoulder Elbow Surg. 2017;26:e159. doi: 10.1016/j.jse.2016.12.031. [DOI] [Google Scholar]
- 245.Tashjian R.Z., Broschinsky K., Stertz I., Chalmers P.N. Structural glenoid allograft reconstruction during reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2020;29:534–540. doi: 10.1016/j.jse.2019.07.011. [DOI] [PubMed] [Google Scholar]
- 246.Tashjian R.Z., Martin B.I., Ricketts C.A., Henninger H.B., Granger E.K., Chalmers P.N. Superior baseplate inclination is associated with instability after reverse total shoulder arthroplasty. Clin Orthop Relat Res. 2018;476:1622–1629. doi: 10.1097/CORR.0000000000000340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Taylor S.A., Shah S.S., Chen X., Gentile J., Gulotta L.V., Dines J.S. Scapular ring preservation: coracoacromial ligament transection increases scapular spine strains following reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2020;102:1358–1364. doi: 10.2106/JBJS.19.01118. [DOI] [PubMed] [Google Scholar]
- 248.Teissier P., Teissier J., Kouyoumdjian P., Asencio G. The TESS reverse shoulder arthroplasty without a stem in the treatment of cuff-deficient shoulder conditions: clinical and radiographic results. J Shoulder Elbow Surg. 2015;24:45–51. doi: 10.1016/j.jse.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 249.Teusink M.J., Otto R.J., Cottrell B.J., Frankle M.A. What is the effect of postoperative scapular fracture on outcomes of reverse shoulder arthroplasty? J Shoulder Elbow Surg. 2014;23:782–790. doi: 10.1016/j.jse.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 250.Theivendran K., Varghese M., Large R., Bateman M., Morgan M., Tambe A. Reverse total shoulder arthroplasty using a trabecular metal glenoid base plate: functional and radiological outcomes at two to five years. Bone Joint J. 2016;98-B:969–975. doi: 10.1302/0301-620x.98b7.37688. [DOI] [PubMed] [Google Scholar]
- 251.Torrens C., Alentorn-Geli E., Mingo F., Gamba C., Santana F. Reverse shoulder arthroplasty for the treatment of acute complex proximal humeral fractures: influence of greater tuberosity healing on the functional outcomes. J Orthop Surg (Hong Kong) 2018;26 doi: 10.1177/2309499018760132. 2309499018760132. [DOI] [PubMed] [Google Scholar]
- 252.Triplet J.J., Everding N.G., Levy J.C., Formaini N.T., O'Donnell K.P., Moor M.A. Anatomic and reverse total shoulder arthroplasty in patients older than 80 years. Orthopedics. 2015;38:e904–e910. doi: 10.3928/01477447-20151002-58. [DOI] [PubMed] [Google Scholar]
- 253.Uri O., Beckles V., Higgs D., Falworth M., Middleton C., Lambert S. Increased-offset reverse shoulder arthroplasty for the treatment of failed post-traumatic humeral head replacement. J Shoulder Elbow Surg. 2014;23:401–408. doi: 10.1016/j.jse.2013.07.041. [DOI] [PubMed] [Google Scholar]
- 254.Valenti P., Kilinc A.S., Sauzières P., Katz D. Results of 30 reverse shoulder prostheses for revision of failed hemi- or total shoulder arthroplasty. Eur J Orthop Surg Traumatol. 2014;24:1375–1382. doi: 10.1007/s00590-013-1332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Valenti P., Sekri J., Kany J., Nidtahar I., Werthel J.D. Benefits of a metallic lateralized baseplate prolonged by a long metallic post in reverse shoulder arthroplasty to address glenoid bone loss. Int Orthop. 2019;43:2131–2139. doi: 10.1007/s00264-018-4249-4. [DOI] [PubMed] [Google Scholar]
- 256.van Ochten J.H.M., van der Pluijm M., Pouw M., Felsch Q.T.M., Heesterbeek P., de Vos M.J. Long-term survivorship and clinical and radiological follow-up of the primary uncemented Delta III reverse shoulder prosthesis. J Orthop. 2019;16:342–346. doi: 10.1016/j.jor.2019.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Verhofste B., Decock T., Van Tongel A., De Wilde L. Heterotopic ossification after reverse total shoulder arthroplasty. Bone Joint J. 2016;98-B:1215–1221. doi: 10.1302/0301-620X.98B9.37761. [DOI] [PubMed] [Google Scholar]
- 258.Villacis D., Sivasundaram L., Pannell W.C., Heckmann N., Omid R., Hatch G.F., 3rd Complication rate and implant survival for reverse shoulder arthroplasty versus total shoulder arthroplasty: results during the initial 2 years. J Shoulder Elbow Surg. 2016;25:927–935. doi: 10.1016/j.jse.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 259.Villodre-Jiménez J., Estrems-Díaz V., Diranzo-García J., Bru-Pomer A. Reverse shoulder arthroplasty in 3 and 4 part proximal humeral fractures in patients aged more than 65 years: results and complications. Rev Esp Cir Ortop Traumatol. 2017;61:43–50. doi: 10.1016/j.recot.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 260.Virk M., Yip M., Liuzza L., Abdelshahed M., Paoli A., Grey S. Clinical and radiographic outcomes with a posteriorly augmented glenoid for Walch B2, B3, and C glenoids in reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2020;29:e196–e204. doi: 10.1016/j.jse.2019.09.031. [DOI] [PubMed] [Google Scholar]
- 261.Vourazeris J.D., Wright T.W., Struk A.M., King J.J., Farmer K.W. Primary reverse total shoulder arthroplasty outcomes in patients with subscapularis repair versus tenotomy. J Shoulder Elbow Surg. 2017;26:450–457. doi: 10.1016/j.jse.2016.09.017. [DOI] [PubMed] [Google Scholar]
- 262.Wagner E., Houdek M.T., Griffith T., Elhassan B.T., Sanchez-Sotelo J., Sperling J.W. Glenoid bone-grafting in revision to a reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2015;97:1653–1660. doi: 10.2106/jbjs.N.00732. [DOI] [PubMed] [Google Scholar]
- 263.Wagner E.R., Chang M.J., Welp K.M., Solberg M.J., Hunt T.J., Woodmass J.M. The impact of the reverse prosthesis on revision shoulder arthroplasty: analysis of a high-volume shoulder practice. J Shoulder Elbow Surg. 2019;28:e49–e56. doi: 10.1016/j.jse.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 264.Wagner E.R., Hevesi M., Houdek M.T., Cofield R.H., Sperling J.W., Sanchez-Sotelo J. Can a reverse shoulder arthroplasty be used to revise a failed primary reverse shoulder arthroplasty? Revision reverse shoulder arthroplasty for failed reverse prosthesis. Bone Joint J. 2018;100-B:1493–1498. doi: 10.1302/0301-620x.100b11.Bjj-2018-0226. [DOI] [PubMed] [Google Scholar]
- 265.Wagner E.R., Houdek M.T., Elhassan B.T., Sanchez-Sotelo J., Cofield R.H., Sperling J.W. What are risk factors for intraoperative humerus fractures during revision reverse shoulder arthroplasty and do they influence outcomes? Clin Orthop Relat Res. 2015;473:3228–3234. doi: 10.1007/s11999-015-4448-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Wagner E.R., Houdek M.T., Hernandez N.M., Cofield R.H., Sánchez-Sotelo J., Sperling J.W. Cement-within-cement technique in revision reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1448–1453. doi: 10.1016/j.jse.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 267.Wagner E.R., Statz J.M., Houdek M.T., Cofield R.H., Sánchez-Sotelo J., Sperling J.W. Use of a shorter humeral stem in revision reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1454–1461. doi: 10.1016/j.jse.2017.01.016. [DOI] [PubMed] [Google Scholar]
- 268.Wahlquist T.C., Hunt A.F., Braman J.P. Acromial base fractures after reverse total shoulder arthroplasty: report of five cases. J Shoulder Elbow Surg. 2011;20:1178–1783. doi: 10.1016/j.jse.2011.01.029. [DOI] [PubMed] [Google Scholar]
- 269.Walch G., Bacle G., Lädermann A., Nové-Josserand L., Smithers C.J. Do the indications, results, and complications of reverse shoulder arthroplasty change with surgeon's experience? J Shoulder Elbow Surg. 2012;21:1470–1477. doi: 10.1016/j.jse.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 270.Walker M., Willis M.P., Brooks J.P., Pupello D., Mulieri P.J., Frankle M.A. The use of the reverse shoulder arthroplasty for treatment of failed total shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21:514–522. doi: 10.1016/j.jse.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 271.Weber-Spickschen T.S., Alfke D., Agneskirchner J.D. The use of a modular system to convert an anatomical total shoulder arthroplasty to a reverse shoulder arthroplasty: Clinical and radiological results. Bone Joint J. 2015;97-B:1662–1667. doi: 10.1302/0301-620x.97b12.35176. [DOI] [PubMed] [Google Scholar]
- 272.Wellmann M., Struck M., Pastor M.F., Gettmann A., Windhagen H., Smith T. Short and midterm results of reverse shoulder arthroplasty according to the preoperative etiology. Arch Orthop Trauma Surg. 2013;133:463–471. doi: 10.1007/s00402-013-1688-7. [DOI] [PubMed] [Google Scholar]
- 273.Werner B.C., Gulotta L.V., Dines J.S., Dines D.M., Warren R.F., Craig E.V. Acromion compromise does not significantly affect clinical outcomes after reverse shoulder arthroplasty: a matched case-control study. HSS J. 2019;15:147–152. doi: 10.1007/s11420-018-9653-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Werner B.C., Wong A.C., Mahony G.T., Craig E.V., Dines D.M., Warren R.F. Clinical outcomes after reverse shoulder arthroplasty with and without subscapularis repair: the importance of considering glenosphere lateralization. J Am Acad Orthop Surg. 2018;26:e114–e119. doi: 10.5435/jaaos-d-16-00781. [DOI] [PubMed] [Google Scholar]
- 275.Werner B.S., Abdelkawi A.F., Boehm D., Hudek R., Plumhoff P., Burkhart K.J. Long-term analysis of revision reverse shoulder arthroplasty using cemented long stems. J Shoulder Elbow Surg. 2017;26:273–278. doi: 10.1016/j.jse.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 276.Werner B.S., Boehm D., Gohlke F. Revision to reverse shoulder arthroplasty with retention of the humeral component. Acta Orthop. 2013;84:473–478. doi: 10.3109/17453674.2013.842433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Werner B.S., Böhm D., Abdelkawi A., Gohlke F. Glenoid bone grafting in reverse shoulder arthroplasty for long-standing anterior shoulder dislocation. J Shoulder Elbow Surg. 2014;23:1655–1661. doi: 10.1016/j.jse.2014.02.017. [DOI] [PubMed] [Google Scholar]
- 278.Werthel J.D., Schoch B.S., van Veen S.C., Elhassan B.T., An K.N., Cofield R.H. Acromial fractures in reverse shoulder arthroplasty: a clinical and radiographic analysis. J Shoulder Elbow Arthroplasty. 2018;2 doi: 10.1177/2471549218777628. 2471549218777628. [DOI] [Google Scholar]
- 279.Whatley A.N., Fowler R.L., Warner J.J., Higgins L.D. Postoperative rupture of the anterolateral deltoid muscle following reverse total shoulder arthroplasty in patients who have undergone open rotator cuff repair. J Shoulder Elbow Surg. 2011;20:114–122. doi: 10.1016/j.jse.2010.04.049. [DOI] [PubMed] [Google Scholar]
- 280.Wiater B.P., Boone C.R., Koueiter D.M., Wiater J.M. Early outcomes of staged bilateral reverse total shoulder arthroplasty: a case-control study. Bone Joint J. 2013;95-B:1232–1238. doi: 10.1302/0301-620x.95b9.31445. [DOI] [PubMed] [Google Scholar]
- 281.Wiater J.M., Moravek J.E., Jr., Budge M.D., Koueiter D.M., Marcantonio D., Wiater B.P. Clinical and radiographic results of cementless reverse total shoulder arthroplasty: a comparative study with 2 to 5 years of follow-up. J Shoulder Elbow Surg. 2014;23:1208–1214. doi: 10.1016/j.jse.2013.11.032. [DOI] [PubMed] [Google Scholar]
- 282.Wieser K., Borbas P., Ek E.T., Meyer D.C., Gerber C. Conversion of stemmed hemi- or total to reverse total shoulder arthroplasty: advantages of a modular stem design. Clin Orthop Relat Res. 2015;473:651–660. doi: 10.1007/s11999-014-3985-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Willis M., Min W., Brooks J.P., Mulieri P., Walker M., Pupello D. Proximal humeral malunion treated with reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21:507–513. doi: 10.1016/j.jse.2011.01.042. [DOI] [PubMed] [Google Scholar]
- 284.Wong M.T., Langohr G.D.G., Athwal G.S., Johnson J.A. Implant positioning in reverse shoulder arthroplasty has an impact on acromial stresses. J Shoulder Elbow Surg. 2016;25:1889–1895. doi: 10.1016/j.jse.2016.04.011. [DOI] [PubMed] [Google Scholar]
- 285.Wright J.O., Ho A., Kalma J., Koueiter D., Esterle J., Marcantonio D. Uncemented reverse total shoulder arthroplasty as initial treatment for comminuted proximal humerus fractures. J Orthop Trauma. 2019;33:e263–e269. doi: 10.1097/bot.0000000000001465. [DOI] [PubMed] [Google Scholar]
- 286.Wright M.A., Keener J.D., Chamberlain A.M. Comparison of clinical outcomes after anatomic total shoulder arthroplasty and reverse shoulder arthroplasty in patients 70 years and older with glenohumeral osteoarthritis and an intact rotator cuff. J Am Acad Orthop Surg. 2020;28:e222–e229. doi: 10.5435/JAAOS-D-19-00166. [DOI] [PubMed] [Google Scholar]
- 287.Wright T.W., Roche C.P., Wright L., Flurin P.H., Crosby L.A., Zuckerman J.D. Reverse shoulder arthroplasty augments for glenoid wear. Comparison of posterior augments to superior augments. Bull Hosp Jt Dis (2013) 2015;73(Suppl 1):S124–S128. [PubMed] [Google Scholar]
- 288.Yoon J.P., Seo A., Kim J.J., Lee C.H., Baek S.H., Kim S.Y. Deltoid muscle volume affects clinical outcome of reverse total shoulder arthroplasty in patients with cuff tear arthropathy or irreparable cuff tears. PLoS One. 2017;12:e0174361. doi: 10.1371/journal.pone.0174361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Youn S.M., Deo S., Poon P.C. Functional and radiologic outcomes of uncemented reverse shoulder arthroplasty in proximal humeral fractures: cementing the humeral component is not necessary. J Shoulder Elbow Surg. 2016;25:e83–e89. doi: 10.1016/j.jse.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 290.Young A.A., Smith M.M., Bacle G., Moraga C., Walch G. Early results of reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93:1915–1923. doi: 10.2106/JBJS.J.00300. [DOI] [PubMed] [Google Scholar]
- 291.Zafra M., Uceda P., Flores M., Carpintero P. Reverse total shoulder replacement for nonunion of a fracture of the proximal humerus. Bone Joint J. 2014;96-B:1239–1243. doi: 10.1302/0301-620x.96b9.33157. [DOI] [PubMed] [Google Scholar]
- 292.Zilber S., Camana E., Lapner P., Haritinian E., Nove Josserand L. Reverse total shoulder arthroplasty using helical blade to optimize glenoid fixation and bone preservation: preliminary results in thirty five patients with minimum two year follow-up. Int Orthop. 2018;42:2159–2164. doi: 10.1007/s00264-018-3891-1. [DOI] [PubMed] [Google Scholar]
- 293.Zumstein M.A., Pinedo M., Old J., Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20:146–157. doi: 10.1016/j.jse.2010.08.001. [DOI] [PubMed] [Google Scholar]