Abstract
Objectives
To identify the consequences of the coronavirus 2019 (COVID-19) pandemic for individuals with traumatic brain injury (TBI), with particular attention to unique effects for individuals with chronic disability.
Design
Individuals with and without a history of TBI completed a web-based survey.
Setting
Participants were recruited from the Vanderbilt Brain Injury Patient Registry in Nashville, TN, and completed the survey from their homes between May and June 2020, during social distancing related to the COVID-19 pandemic.
Participants
Participants (N=47) in the chronic phase of moderate-severe TBI (>6mo postinjury) and 51 noninjured comparison (NC) peers completed the survey.
Interventions
Not applicable.
Main Outcome Measures
Participants, or respondents, answered a mix of multiple choice and free text questions about how the COVID-19 pandemic has affected their work, education, medical care, social communication, sources of information and decision making, and mental and physical well-being. Individuals with TBI also answered questions about how TBI has affected their experiences of the pandemic.
Results
As a group, respondents with TBI reported less pandemic-related behavior change (eg, daily habits, virtual social visits, and masking) than NC peers. Both NCs and respondents with TBI identified health care providers as trusted sources of public health information. One-third of individuals with TBI indicated that brain injury has made coping with the pandemic more difficult, and respondents identified mental health challenges and social isolation as key barriers.
Conclusions
These results suggest that health care providers should look for ways to provide tailored education and reduce social isolation for individuals with disability during the ongoing COVID-19 pandemic. We discuss several direct suggestions from participant responses.
Keywords: Brain injuries, traumatic; COVID-19; Rehabilitation
List of abbreviations: COVID-19, coronavirus disease 2019; NC, noninjured comparison; TBI, traumatic brain injury
In early 2020, the coronavirus disease 2019 (COVID-19) pandemic swept the globe, bringing with it widespread societal disruption. The pandemic has affected all facets of public life, but certain groups may be more vulnerable to the virus itself or to related changes in safety protocols, health care services, and social infrastructure. Specifically, there is increasing concern that individuals with disability may be disproportionately affected by the pandemic and related reductions in accessibility of supportive services and networks.1, 2, 3, 4, 5
Approximately 6.2 million Americans currently live with disability related to traumatic brain injury (TBI),6 which may result in broad impairments in cognition, communication, mobility, sensory domains, and/or behavior or mental health.7, 8, 9, 10, 11, 12 TBI is often called an “invisible injury” because individuals with TBI may not exhibit a physical disability but instead struggle to remember important details, to solve problems, or to communicate effectively with others.10 Consequently, it may be difficult for individuals with TBI to reintegrate to the community after injury.11 People with a history of TBI are at increased risk for unemployment,13, 14, 15 housing insecurity,16 interpersonal violence,17 and interactions with the legal system.18 In addition to these potential sources of social and economic vulnerability, many individuals with TBI feel socially isolated or have smaller support networks than their peers due to impairments in social communication or misunderstanding of the injury’s consequences.19, 20, 21, 22 Taken together, injury-related deficits, social isolation, and increased need for medical and support services may place individuals with TBI at increased risk for negative consequences from the COVID-19 pandemic.
We conducted a survey of individuals with a history of moderate-severe TBI to better understand how the pandemic has affected individuals with TBI, how individuals with TBI make decisions about their own health, and how health care providers and policy makers might best support individuals with TBI during the pandemic.
Methods
Participants
Participants, or respondents, were 47 individuals with moderate-severe TBI (24 women) and 51 noninjured comparison (NC) participants (27 women). The mean ages ± SD for respondents with TBI and NCs were 38.34±9.73 and 36.41±10.31, respectively, and did not differ statistically (t(96)=.950; P=.344). Mean years of education attained ± SD for respondents with TBI and NC participants were 15.00±2.67 and 15.22±2.23, respectively, and did not differ statistically (t(96)=1.16; P=.247).
NC participants were recruited from Nashville, TN, and the surrounding areas and had no history of neurologic or cognitive disability. Individuals with TBI were recruited through the Vanderbilt Brain Injury Patient Registry and did not have a history of neurologic or cognitive disability prior to the qualifying brain injury. All individuals with TBI were in the chronic phase of injury (>6mo postinjury; mean time since onset ± SD, 69.19±62.04mo) and sustained their injuries in adulthood. Injury-related information was collected from available medical records and semistructured participant interviews. Injury etiologies included motor vehicle collisions (n=20), falls (n=9), motorcycle or snowmobile accidents (n=6), being struck by a vehicle while walking or biking (n=4), assault (n=3), nonmotorized vehicle accidents (eg, longboard accident; n=3), and being struck by a moving object (n=2). TBI severity was determined using the Mayo Classification System,23 and injuries were classified as moderate-severe if at least 1 of the following criteria were met: (1) Glasgow Coma Scale score less than 13 within 24 hours of acute care admission, (2) positive neuroimaging findings (acute computed tomographic findings or lesions visible on chronic magnetic resonance imaging), (3) loss of consciousness for 30 minutes or longer, or (4) posttraumatic amnesia for 24 hours or longer.
Survey
A survey consisting of 84 questions (a mix of multiple choice and free response) formed the basis of data collection (see supplemental appendix, available online only at http://archives-pmr.org/). In some cases, questions only appeared if respondents had previously selected a given response. For example, questions about changes to work routines only appeared for respondents who indicated that they were employed. The survey included questions about pandemic-related changes in employment or academics (eg, remote work or learning) and how those affected job or school difficulty; changes to family and caring responsibilities; changes to medical care, access to medications, and telehealth; changes to social communication, preferred communication methods, and how the pandemic has affected social relationships; sources of pandemic-related information and decision making; changes to daily life, habits, and mental and physical well-being during the pandemic. Individuals with TBI also answered questions about how TBI has affected their experiences and provided suggestions for supporting individuals with TBI during the pandemic.
Procedures
Procedures for this study were approved by the Human Research Protections Program at Vanderbilt University Medical Center. Participants received a link to complete the survey online via the Research Electronic Data Capture System (REDCapa).24 Two individuals who do not use e-mail completed paper versions of the survey and returned them by mail. The survey took approximately 30 to 45 minutes to complete.
All respondents completed the survey during a constrained 1-month period, between May 21 and June 21, 2020. During the response window, Tennessee was under a state of emergency due to the COVID-19 pandemic.25 Although both the Centers for Disease Control and Prevention and the local Nashville government recommended masks in public,26 , 27 there was no mask mandate in Tennessee or Davidson County during the response window. Nashville was in Phase 1 of its COVID-19 reopening plan,26 with retail stores, bars, and restaurants open at 50% capacity. Masking and social distancing were encouraged, gatherings were limited to 10 or fewer people, and individuals designated as having a higher risk of coronavirus complications (ie, those ≥65y or with pre-existing medical conditions) were asked to stay home.
Analysis and interpretation
The goal of this study was to provide a snapshot of how individuals with and without a history of TBI responded to the COVID-19 pandemic during a specific phase and in a specific geographic region. Consistent with this goal, and because this is the first exploration of pandemic response for individuals with TBI, we report descriptive statistics alone, without testing specific hypotheses about responses based on group membership. We expect that these data will provide a baseline as to how individuals with TBI are responding to the pandemic and will begin a derivation chain informing future hypothesis-driven research in this area.28
Results
Responding to individual questions was voluntary, and not all respondents completed all questions. The number of individuals who responded to a given question is listed in parentheses. Response percentages for each group are listed for multiple choice questions; percentages are not listed for free text responses. On some questions, respondents could choose more than 1 option, and total percentages reported for those questions may exceed 100%. In this section, we focus our reporting on those responses most relevant to the COVID-19 pandemic and on select free response questions (eg, those related to medical appointments) from participants with TBI. However, for comprehensiveness, the entire survey and each group’s response rates for all quantitative questions are available in the supplemental appendix (available online only at http://www.archives-pmr.org/).
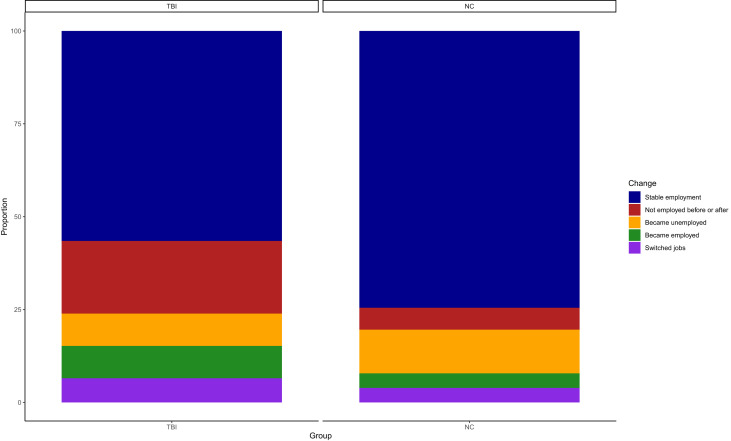
Employment, academics, and caring responsibilities during the pandemic
Overall, 72.34% (34 of 47) of respondents with TBI reported that they were currently employed, compared with 82.35% (42 of 51) of NCs. Of note, respondents with TBI reported more frequently than NCs that they were classified as essential workers (eg, retail worker, nurse). This designation applied to 70.59% of respondents with TBI (24 of 34), relative to 45.24% of NCs (19 of 42). Figure 1 shows how participants’ employment status had changed since the start of the pandemic.
Fig 1.
Changes in employment status since the start of the pandemic.
Of those respondents who had retained the same position since the start of the pandemic, respondents with TBI reported stable job duties and schedule (38.46%, 10 of 26) more frequently than NCs (18.42%, 7 of 38). Respondents with TBI reported that they had transitioned to working from home full time since the start of the pandemic (15.38%, 4 of 26) less frequently than NCs (42.11%, 16 of 38).
Respondents with TBI reported that COVID-related changes had affected the difficulty of their jobs less frequently than NCs (see supplemental appendix, available online only at http://archives-pmr.org/). Respondents with TBI and NCs were comparable in changes to their family and caring responsibilities since the start of the pandemic (see supplemental appendix, available online only at http://archives-pmr.org/).
Medical care during the pandemic
Only 1 participant in this study (an NC) had been diagnosed with COVID-19 since the start of the pandemic. We asked respondents about how they managed scheduled medical appointments during the pandemic. Of those who had appointments scheduled, 60.72% (17 of 28) of respondents with TBI had attended their appointments in person, compared with 50.00% (11 of 22) of NCs. Respondents with TBI who attended appointments in person cited the essential nature of those appointments (n=11), the need for hands-on care (n=5), and acute medical incidents (n=5) as primary reasons. In contrast, 28.57% of respondents with TBI (8 of 28) compared with 40.91% of NCs (9 of 22) had attended their appointments via telehealth.
Social communication during the pandemic
Respondents with TBI and NCs were comparable in their household structures (see supplemental appendix, available online only at http://archives-pmr.org/). Both respondents with TBI (72.34%, 34 of 47) and NCs (76.47%, 39 of 51) reported a reduction in in-person social visits with nonhousehold members since the start of the pandemic. Respondents with TBI reported an increase in virtual social visits (53.19%, 25 of 47) less frequently than NCs (72.55%, 37 of 51). About half of respondents with TBI (51.06%, 24 of 47) and 43.14% (22 of 51) of NCs reported staying in touch with the same number of people as before the pandemic. Both respondents with TBI and NCs reported an increase in their overall use of socially distanced communication (ie, communicating by phone, e-mail, text, video call), although NCs more frequently reported increasing their use of some methods (fig 2 ).
Fig 2.
Self-rated changes in use of communication tools since start of pandemic. Only respondents who endorsed using a given tool are included. Social, social media; Text, text or messaging app; Video, video call.
We asked respondents to rank communication modalities by ease of communication (table 1 ). Both respondents with TBI (84.78%, 39 of 46) and NCs (74.51%, 38 of 51) found virtual social visits to be less successful than in-person social visits. Respondents with TBI listed the impersonal feeling of virtual social visits (n=20) and communication challenges (eg, difficulty reading body language or expressions virtually; n=4) as primary barriers. Respondents with TBI (61.54%, 16 of 26) and NCs (68.89%, 31 of 45) also found social interactions wearing a mask to be less successful than those without a mask. Respondents with TBI cited reduced visibility of facial expressions (n=9) and hearing loss or difficulty hearing (n=6) as primary barriers.
Table 1.
Ranking of communication tools by ease of use
| Communication Tool | Rated Easiest, % |
Rated at All, % |
||
|---|---|---|---|---|
| TBI (n=47) | NC (n=51) | TBI (n=47) | NC (n=51) | |
| In person | 51.06 | 56.86 | 93.62 | 98.04 |
| 14.89 | 7.84 | 87.23 | 88.24 | |
| Phone call | 0.00 | 5.88 | 89.36 | 96.08 |
| Text or messaging | 14.89 | 19.61 | 93.62 | 98.04 |
| Video call | 17.02 | 5.88 | 85.11 | 98.04 |
NOTE. Respondents only rated tools that they use.
In both groups, approximately half of respondents (51.06% [24 of 27] of respondents with TBI and 51.02% [25 of 49] of NCs) reported no changes to the quality of their social relationships due to social distancing (see supplemental appendix, available online only at http://archives-pmr.org/).
Sources of pandemic-related public health information
Fewer respondents with TBI (27.66%, 13 of 47) than NCs (41.18%, 21 of 51) reported an increase in news consumption since the start of the pandemic. We asked respondents to rank the trustworthiness of sources of pandemic-related information (table 2 ). Respondents with TBI reported more frequently than NCs that they perceived government and media pandemic responses as overreactions (table 3 ).
Table 2.
Ranking of trustworthiness for sources of public health information
| Source of Public Health Information | Rated Most Trustworthy, % |
Rated at All, % |
||
|---|---|---|---|---|
| TBI (n=46) | NC (n=51) | TBI (n=46) | NC (n=51) | |
| Conversation with friends and family | 19.57 | 3.92 | 86.96 | 94.12 |
| Conversation with medical professionals | 32.61 | 41.18 | 86.96 | 98.04 |
| Government news briefings | 10.87 | 11.76 | 80.43 | 96.08 |
| Government websites | 4.35 | 7.84 | 84.78 | 96.08 |
| Newspaper or newspaper websites | 2.17 | 7.84 | 80.43 | 94.12 |
| News radio | 0.00 | 7.84 | 80.43 | 92.16 |
| Social media | 10.87 | 9.80 | 91.30 | 94.12 |
| Television news or network website | 6.52 | 5.88 | 95.65 | 98.04 |
NOTE. Respondents only rated news sources that they use.
Table 3.
Ratings of pandemic reactions from government and news media
| Group Reacting to Pandemic | Underreaction, % |
Appropriate Reaction, % |
Overreaction, % |
|||
|---|---|---|---|---|---|---|
| TBI | NC | TBI | NC | TBI | NC | |
| Federal government (TBI, n=46; NC, n=51) | 39.13 | 56.86 | 36.96 | 39.22 | 23.91 | 3.92 |
| Local government (TBI, n=47; NC, n=51) | 21.28 | 29.41 | 51.06 | 58.82 | 27.66 | 11.77 |
| News media (TBI, n=47; NC, n=51) | 10.64 | 4.00 | 27.66 | 44.00 | 61.70 | 52.00 |
Decision making about the pandemic
Respondents with TBI reported less frequently than NCs that they were staying home more when not at work. A total of 65.22% (30 of 46) of respondents with TBI reported a reduction in nonwork outings, compared with 88.00% (44 of 50) of NCs. Fewer respondents with TBI (55.32%, 26 of 47) than NCs (90.20%, 46 of 51) reported wearing a mask when in public. Approximately three quarters (76.60%) of respondents with TBI (36 of 47), compared with 66.67% of NCs (34 of 51), reported that they did not have difficulty making decisions as to when to leave the house. Respondents with TBI cited the necessity (n=18) and safety (n=5) of an outing as key decision factors. Nine respondents with TBI, compared with 3 NCs, reported that the pandemic does not play a role in their decisions about leaving the house.
Mental and physical well-being during the pandemic
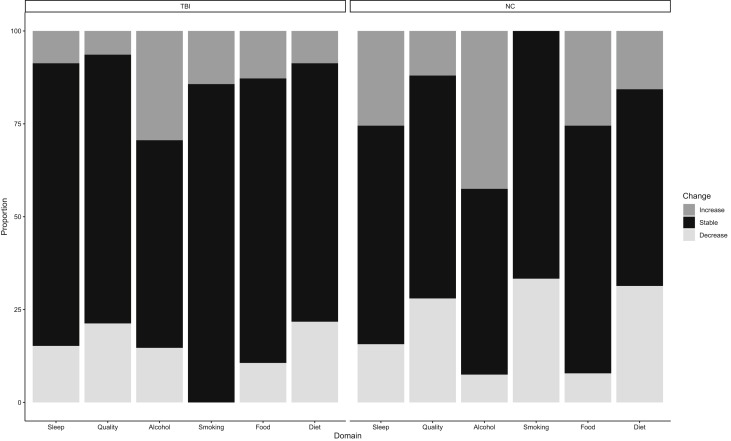
Fewer respondents with TBI (57.45%, 27 of 47) than NCs (76.47%, 39 of 51) reported that the pandemic had significantly affected their daily lives. Respondents with TBI reported more frequently than NCs that their perception of time and planning for the future had remained stable since the start of the pandemic (see supplemental appendix, available online only at http://archives-pmr.org/). Fewer respondents with TBI (51.06%, 24 of 47) than NCs (66.67%, 34 of 51) reported that the pandemic has affected their sense of mental and physical well-being. Respondents with TBI who had not experienced changes to their well-being cited limited changes to daily life (n=8), a sense of being fortunate relative to others (n=5), a refusal to live in fear (n=3), and a strong support system (n=2) as major factors. Respondents with TBI who experienced changes to well-being since the start of the pandemic cited mental health challenges (n=13), a sense of isolation (n=4), and an inability to go to the gym or exercise (n=4) as playing a role. Respondents with TBI reported less frequently than NCs that they had experienced a decrease in life satisfaction (TBI: 17.78%, 8 of 45; NC: 29.41%, 15 of 51) or reduced feeling that one’s activities are worthwhile (TBI: 10.64%, 5 of 47; NC: 23.53%, 12 of 51) since the start of the pandemic. Respondents with TBI reported being more stable in their daily habits than NCs (fig 3 ).
Fig 3.
Self-rated changes in daily habits during the week before survey completion, relative to the start of the pandemic. For smoking and alcohol consumption, only respondents who regularly engage in these habits are included. Sleep, amount of sleep; Quality, quality of sleep; Alcohol, alcohol consumption; Food, frequency of eating; Diet, diet health.
Effect of TBI history on perceptions of the pandemic
Approximately one-third (30.43%, 14 of 46) of respondents with TBI indicated that their injury history has made the pandemic more challenging. Some respondents who did not find that TBI has affected their experience of the pandemic indicated that they do not perceive any lingering effects of injury (n=6) or that they do not see how TBI would make a difference (n=6). Respondents who did report TBI-related changes in their experiences of the pandemic cited mental health concerns (n=9) and increased cognitive challenges (n=5) as key factors.
We asked respondents with TBI to provide suggestions as to how health care providers might improve supports for individuals with TBI during the COVID-19 pandemic. The most frequent suggestions were an increase in reassuring checkins to combat isolation (n=6) and opportunities to meet or engage in support with other people who have had a TBI (n=4).
Discussion
We conducted a survey of individuals with a chronic history of moderate-severe TBI and noninjured peers about changes to daily life, decision making, and support needs during the pandemic. The results from this survey provide a snapshot of how individuals with TBI are coping with the pandemic and may inform future efforts to tailor support during this evolving public health crisis. A number of key observations emerged.
Respondents with TBI reported more stability in daily pandemic life
Individuals with and without a history of TBI reported broad changes resulting from the COVID-19 pandemic. However, respondents with TBI reported less frequently than NCs that they had experienced significant alterations to daily life. Individuals with TBI reported fewer pandemic-related changes to their mental and physical well-being or ability to plan for the future than NCs. Individuals with TBI also reported more stable daily habits (eg, sleep, diet) since the start of the pandemic than NCs.
Some of the reported stability in habits and perceived well-being for respondents with TBI may result from reduced external changes relative to NCs. For example, NCs reported more frequently that they had transitioned to working from home, whereas individuals with TBI were more likely to have been unemployed since before the pandemic or to be classified as essential workers. As some of the consequences of the pandemic (eg, reductions in social interactions) mimic the consequences of TBI alone, individuals with TBI may have experienced fewer changes overall.
It is also worth considering that TBI-related disability may play a role in reported behavioral stability and pandemic-related decision making. The goal of this study was to document the effects of the COVID-19 pandemic on individuals with TBI, rather than to determine causal links between TBI and pandemic-related behaviors. That said, the results here suggest that some individuals with TBI-related disability may be less likely to make behavioral adjustments in response to the pandemic or other large-scale crises. For example, as a group, respondents with TBI reported fewer behavioral changes consistent with pandemic-related public health recommendations, such as staying home more or wearing a mask in public, than NCs. Although respondents with TBI and NCs were consistent in reducing in-person social visits, respondents with TBI reported increasing virtual social interactions, which may be protective against social isolation, less frequently than NCs. This lack of behavior change may place some individuals with TBI at risk for disproportionate negative outcomes from the pandemic.
Cognitive-communication deficits may make it difficult for some individuals to adjust behavior in response to the pandemic or to adapt to recommended pandemic-related changes. For example, cognitive-communication deficits may place additional burdens on those who reported that social interactions while wearing a mask were more difficult in part due to reduced visual cues (eg, facial expressions or lip reading when they cannot hear their communication partners). Some respondents with TBI also noted that pandemic-related changes have exacerbated existing cognitive-communication deficits (eg, memory deficits), or that TBI has made it more difficult to cope with mental health challenges during the pandemic.
We do not know the reason for reported behavioral stability in the group of respondents with TBI. It may be because of baseline lifestyle differences, differing sources of public health information during an evolving crisis, cognitive-communication deficits or, speculatively, because maintaining stable behavior patterns may feel protective in the face of vast uncertainty and change. However, this area of study is ripe for discovery in understanding the factors that drive behavioral stability or change in individuals with TBI. Understanding these factors, as well as sources of variability across individuals, may drive decision making in the context of the evolving pandemic and in response to a range of health care decisions and recommendations.
Health care providers are a trusted source of public health information
Given that our understanding of COVID-19 is dynamic with evolving public health recommendations, it is critical for health care providers and policy makers to consider how best to provide timely, accurate, and useful public health information to individuals with TBI. Respondents with TBI, as a group, did not report increasing their news consumption since the start of the pandemic at the same rate as NCs. Respondents with TBI also reported more frequuently than NCs that they receive trustworthy public health information from family and friends. However, both respondents with TBI and NCs rated health care providers as the most trustworthy source of public health information. In this context, health care providers and public health officials should consider how best to provide information to individuals with TBI in a way that is accessible and obtainable. For example, some individuals with TBI-related cognitive-communication deficits would benefit from information provided through multiple modalities (eg, verbal and written) and without complex language.10 , 29 In cases in which public health recommendations may be less accessible (eg, require additional or novel use of technology), some individuals with TBI may benefit from additional support to use those modalities. In addition, when asked how health care providers may best support individuals with TBI during the pandemic, respondents noted that checkins from providers or opportunities to interact with other individuals with TBI would reduce their feelings of social isolation. A combination of tailored information and regular contact may be critical in supporting some individuals with TBI in making behavioral adjustments for increased safety and social connectedness during the COVID-19 pandemic.
Pandemic experiences of individuals with chronic disability
Individuals with disability in general,30, 31, 32, 33 and those with TBI in particular,34 are often overlooked when considering population-level preparedness for large-scale disasters. This may be even more challenging in TBI, when disability may not be easily visible or identified even by the individuals themselves, especially years after injury. However, some of the specific challenges of TBI (eg, cognitive-communication deficits or mental health challenges) may be exacerbated by crises, even in individuals who do not typically endorse TBI-related changes to daily life. Many of the experiences reported by individuals with TBI on this survey are consistent with early pandemic reporting from individuals with other physical35 and neurologic disabilities (eg, multiple sclerosis).36 , 37 Our disaster response should be inclusive of individuals with both physical and cognitive disabilities.1 , 34 , 38 , 39 Given increased interest in disability preparedness for large-scale crises such as pandemics and natural disasters,30, 31, 32, 33, 34 the results from this survey suggest that health care providers and policy makers may need to take an increased role in both increasing health care access during the pandemic and providing information and support that is accessible and tailored to the needs of specific disability populations.
Although we report differences in group trends between respondents with TBI and NC peers, there was considerable variability in behavior and perceptions within each group. This variability is unsurprising given the vast range of behavioral and functional outcomes after TBI.11 As such, in addition to considering the needs of specific disability populations, providers should continue to take the needs of each individual with TBI into consideration when providing pandemic-related support.
Of course, this type of recommendation may be difficult to implement in our current medical model for TBI. Service delivery is often front-loaded to acute care and rehabilitation settings, despite the fact that TBI is a chronic disability in which individuals would benefit from a range of services, intermittently, across the lifespan. Any comprehensive disaster response must consider individuals with chronic but stable disability, such as TBI, in addition to those with developmental or degenerative disorders who may receive more consistent health care follow-up. As an increasing number of individuals experience prolonged neurologic disability caused by COVID-1940 and scientists warn that we are at risk for an increase in large-scale disasters, this is an ideal time to reimagine our service delivery models for individuals with chronic disability. We hope the findings from this survey provide some baseline data that will inform increased discussion and support for such endeavors to meet ongoing needs of individuals with TBI and other chronic disabilities and to better anticipate their unique needs during crises.
Study limitations
Results from this survey provide a snapshot of how a group of individuals with TBI in a specific geographic region responded during a constrained phase of the COVID-19 pandemic. It is possible that there are factors beyond brain injury that differ systematically between groups that contribute to the results here. We believe, however, that the close demographic matching of the groups significantly reduces this concern. Furthermore, the restricted region and timescale allowed for controlled variability in regional pandemic circumstances, as participants from both groups were drawn from the same metropolitan area. Given that the pandemic is evolving, there will also be a need for ongoing surveillance as to how to support individuals with TBI at each stage and across different geographic regions.
As this is the first study assessing how individuals with TBI are responding to the pandemic, we did not test specific hypotheses and instead provide baseline data that may form the first link in a derivation chain for future hypothesis-driven research in this area.28 In developing a TBI-specific pandemic response, and in rehabilitation research more broadly, it is critical that stakeholders with disabilities have a guiding voice.41 Our participants provided initial responses as to how we might improve health care services for individuals with TBI, but further studies may build upon these results to request feedback on specific intervention options. Additional studies with larger sample sizes will also allow for informed hypotheses and direct statistical tests of between-group differences in pandemic response.
Conclusions
As the COVID-19 pandemic affects all facets of daily life, it is critical to consider the pandemic’s differential effects on individuals with TBI and chronic disability. We reported results from a survey that provide a snapshot of how individuals with TBI are responding to the COVID-19 pandemic. Results from this survey suggest that some individuals with TBI may benefit from tailored and ongoing public health education, as well as support in making behavioral adjustments for increased safety and social connectedness during the COVID-19 pandemic. Considering how the pandemic has affected individuals with TBI may also allow for more proactive planning for supporting individuals with chronic disability during future large-scale crises.
Supplier
-
a.
REDCap; Vanderbilt University.
Footnotes
Supported by National Institutes of Health, National Institute of Neurological Disorders and Stroke (grant no. R01 110661 to M.C.D.).
Disclosures: none.
Supplementary data
References
- 1.Leocani L., Diserens K., Moccia M., Caltagirone C. Disability through COVID-19 pandemic: neurorehabilitation cannot wait. Eur J Neurol. 2020;27:e50–e51. doi: 10.1111/ene.14320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyle C.A., Fox M.H., Havercamp S.M., Zubler J. The public health response to the COVID-19 pandemic for people with disabilities. Disabil Health J. 2020;13:100943. doi: 10.1016/j.dhjo.2020.100943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Armitage R., Nellums L.B. The COVID-19 response must be disability inclusive. Lancet Public Health. 2020;5:e257. doi: 10.1016/S2468-2667(20)30076-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Nations Human Rights Office of the High Commissioner . In: COVID-19 and the rights of persons with disabilities. United Nations Human Rights Office of the High Commissioner; Geneva: 2020. What is the impact of COVID-19 on the right to health of persons with disabilities? pp. 1–11. [Google Scholar]
- 5.Lund E.M. Interpersonal violence against people with disabilities: additional concerns and considerations in the COVID-19 pandemic. Rehabil Psychol. 2020;65:199–205. doi: 10.1037/rep0000347. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; Atlanta: 2015. Report to Congress on traumatic brain injury in the United States: epidemiology and rehabilitation. [DOI] [PubMed] [Google Scholar]
- 7.Ylvisaker M. Context-sensitive cognitive rehabilitation after brain injury: theory and practice. Brain Impair. 2003;4:1–16. [Google Scholar]
- 8.Ylvisaker M., Hanks R., Johnson-Green D. Rehabilitation of children and adults with cognitive-communication disorders after brain injury. ASHA Suppl. 2003;23:59–72. [Google Scholar]
- 9.Ylvisaker M., Turkstra L.S., Coelho C. Behavioral and social interventions for individuals with traumatic brain injury: a summary of the research with clinical implications. Semin Speech Lang. 2005;26:256–267. doi: 10.1055/s-2005-922104. [DOI] [PubMed] [Google Scholar]
- 10.MacDonald S. Introducing the model of cognitive-communication competence: a model to guide evidence-based communication interventions after brain injury. Brain Inj. 2017;31:1760–1780. doi: 10.1080/02699052.2017.1379613. [DOI] [PubMed] [Google Scholar]
- 11.Dahdah M.N., Barnes S., Buros A., et al. Variations in inpatient rehabilitation functional outcomes across centers in the traumatic brain injury model systems study and the influence of demographics and injury severity on patient outcomes. Arch Phys Med Rehabil. 2016;97:1821–1831. doi: 10.1016/j.apmr.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Rabinowitz A.R., Levin H.S. Cognitive sequelae of traumatic brain injury. Psychiatr Clin North Am. 2014;37:1–11. doi: 10.1016/j.psc.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gormley M., Devanaboyina M., Andelic N., Røe C., Seel R.T., Lu J. Long-term employment outcomes following moderate to severe traumatic brain injury: a systematic review and meta-analysis. Brain Inj. 2019;33:1567–1580. doi: 10.1080/02699052.2019.1658222. [DOI] [PubMed] [Google Scholar]
- 14.Todis B., Glang A., Bullis M., Ettel D., Hood D. Longitudinal investigation of the post-high school transition experiences of adolescents with traumatic brain injury. J Head Trauma Rehabil. 2011;26:138–149. doi: 10.1097/HTR.0b013e3181e5a87a. [DOI] [PubMed] [Google Scholar]
- 15.Ylvisaker M., Adelson P.D., Braga L.W., et al. Rehabilitation and ongoing support after pediatric TBI: twenty years of progress. J Head Trauma Rehabil. 2005;20:95–109. doi: 10.1097/00001199-200501000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Stubbs J.L., Thornton A.E., Sevick J.M., et al. Traumatic brain injury in homeless and marginally housed individuals: a systematic review and meta-analysis. Lancet Public Health. 2020;5:e19–e32. doi: 10.1016/S2468-2667(19)30188-4. [DOI] [PubMed] [Google Scholar]
- 17.St Ivany A., Schminkey D. Intimate partner violence and traumatic brain injury: state of the science and next steps. Fam Community Health. 2016;39:129–137. doi: 10.1097/FCH.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 18.McIsaac K.E., Moser A., Moineddin R., et al. Association between traumatic brain injury and incarceration: a population-based cohort study. CMAJ Open. 2016;4:E746–E753. doi: 10.9778/cmajo.20160072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finset A., Dyrnes S., Krogstad J.M., Berstad J. Self-reported social networks and interpersonal support 2 years after severe traumatic brain injury. Brain Inj. 1995;9:141–150. doi: 10.3109/02699059509008187. [DOI] [PubMed] [Google Scholar]
- 20.Tomberg T., Toomela A., Pulver A., Tikk A. Coping strategies, social support, life orientation and health-related quality of life following traumatic brain injury. Brain Inj. 2005;19:1181–1190. doi: 10.1080/02699050500150153. [DOI] [PubMed] [Google Scholar]
- 21.Rigon A., Duff M.C., Beadle J. Lonely but not alone: neuroticism mediates the relationship between social network size and loneliness in individuals with traumatic brain injury. J Int Neuropsychol Soc. 2019;25:285–292. doi: 10.1017/S1355617718001108. [DOI] [PubMed] [Google Scholar]
- 22.Morton M.V., Wehman P. Psychosocial and emotional sequelae of individuals with traumatic brain injury: a literature review and recommendations. Brain Inj. 1995;9:81–92. doi: 10.3109/02699059509004574. [DOI] [PubMed] [Google Scholar]
- 23.Malec J.F., Brown A.W., Leibson C.L., et al. The Mayo classification system for traumatic brain injury severity. J Neurotrauma. 2007;24:1417–1424. doi: 10.1089/neu.2006.0245. [DOI] [PubMed] [Google Scholar]
- 24.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tennessee state of emergency extended, runs until June 30th. News 4 Nashville. May 12, 2020 [Google Scholar]
- 26.Alund N.N. What to know about phase one and the plan to reopen Nashville: restaurant rules, what can happen next. Nashville Tennessean. May 11, 2020. https://www.tennessean.com/story/news/2020/05/11/nashville-reopening-phase-one-what-to-know-restaurant-rules-shops/3107239001/ Available at: Accessed September 20, 2020.
- 27.Dwyer C., Aubrey A. CDC now recommends Americans consider wearing cloth face coverings in public. National Public Radio. April 3, 2020. https://www.npr.org/sections/coronavirus-live-updates/2020/04/03/826219824/president-trump-says-cdc-now-recommends-americans-wear-cloth-masks-in-public Available at: Accessed September 20, 2020.
- 28.Scheel A.M., Tiokhin L., Isager P.M., Lakens D. Why hypothesis testers should spend less time testing hypotheses. Perspect Psychol Sci. 2020 Dec 16 doi: 10.1177/1745691620966795. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ylvisaker M., Feeney T.J. Singular Publishing Group; San Diego: 1998. Collaborative brain injury intervention: positive everyday routines. [Google Scholar]
- 30.Bethel J.W., Foreman A.N., Burke S.C. Disaster preparedness among medically vulnerable populations. Am J Prev Med. 2011;40:139–143. doi: 10.1016/j.amepre.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 31.Bloodworth D.M., Kevorkian C.G., Rumbaut E., Chiou-Tan F.Y. Impairment and disability in the Astrodome after Hurricane Katrina: lessons learned about the needs of the disabled after large population movements. Am J Phys Med Rehabil. 2007;86:770–775. doi: 10.1097/PHM.0b013e31813e0439. [DOI] [PubMed] [Google Scholar]
- 32.Eisenman D.P., Zhou Q., Ong M., Asch S., Gilk D., Long A. Variations in disaster preparedness by mental health, perceived general health, and disability status. Disaster Med Public Health Prep. 2009;3:33–41. doi: 10.1097/DMP.0b013e318193be89. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention CDC’s disaster planning goal: protect vulnerable older adults. https://www.cdc.gov/aging/pdf/disaster_planning_goal.pdf Available at: Accessed September 20, 2020.
- 34.Shapiro L.T., Jimenez V., Espinel Z., Galea S., Kossin J.P., Shultz J.M. Preparing survivors of traumatic brain injury for catastrophic hurricanes in the time of climate change. J Head Trauma Rehabil. 2020;35:439–442. doi: 10.1097/HTR.0000000000000571. [DOI] [PubMed] [Google Scholar]
- 35.Lebrasseur A., Fortin-Bédard N., Lettre J., et al. Impact of COVID-19 on people with physical disabilities: a rapid review. Disabil Health J. 2021;14:101014. doi: 10.1016/j.dhjo.2020.101014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chiaravalloti N.D., Amato M.P., Brichetto G., et al. The emotional impact of the COVID-19 pandemic on individuals with progressive multiple sclerosis. J Neurol. 2020 Aug 19 doi: 10.1007/s00415-020-10160-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stojanov A., Malobabic M., Milosevic V., et al. Psychological status of patients with relapsing-remitting multiple sclerosis during coronavirus disease-2019 outbreak. Mult Scler Relat Disord. 2020;45:102407. doi: 10.1016/j.msard.2020.102407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health OrganizationDisability considerations during the COVID-19 outbreak. Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-Disability-2020-1. Accessed September 20, 2020.
- 39.Courtenay K., Perera B. COVID-19 and people with intellectual disability: impacts of a pandemic. Ir J Psychol Med. 2020;37:231–236. doi: 10.1017/ipm.2020.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ramage A.E. Potential for cognitive communication impairment in COVID-19 survivors: a call to action for speech-language pathologists. Am J Speech Lang Pathol. 2020;12:1821–1832. doi: 10.1044/2020_AJSLP-20-00147. [DOI] [PubMed] [Google Scholar]
- 41.Ehde D.M., Wegener S.T., Williams R.M., et al. Developing, testing, and sustaining rehabilitation interventions via participatory action research. Arch Phys Med Rehabil. 2013;94(1 Suppl):S30–S42. doi: 10.1016/j.apmr.2012.10.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.