Abstract
Objective
To document the level of physical function in patients with coronavirus disease 2019 (COVID-19) recovering from acute respiratory failure and investigate which patient clinical characteristics could predict physical function assessed by the Short Physical Performance Battery (SPPB) test.
Design
Cross-sectional study.
Setting
Subacute unit of a Rehabilitation Institute.
Participants
Patients with COVID-19 (N=184; aged 18 years or older) who were admitted to a subacute unit to stabilize their condition and recover from acute respiratory failure due to COVID-19.
Interventions
Not applicable.
Main Outcome Measures
At admission patients underwent the SPPB test, represented by the sum of 3 functional tests, standing balance, 4-meter gait speed, and 5-repetition sit-to-stand motion. Comparisons between 2 SPPB score groups were performed by an unpaired t test; multivariate stepwise linear regression analysis was employed to detect predictors of the SPPB score considering several clinical parameters.
Results
Participants were 74±12 years old, 52% were men and with more than 2 comorbidities in 43% of cases. SPPB score was 3.02±3.87 denoting patients’ profound physical dysfunction. Normal physical function was detected in only 12% of patients, whereas low, intermediate, and severe impairment was found in 65%, 13%, and 10%, respectively. Age, both invasive and noninvasive ventilation use, and the presence of previous disability were significant predictors of SPPB. Patients without any comorbidities (8%) also exhibited low function (SPPB: 5.67±1.12).
Conclusions
The majority of survivors after COVID-19 experienced acute respiratory failure due to pneumonia and exhibited substantial physical dysfunction influenced by age, mechanical ventilation need, and previous disability. Further studies are needed to evaluate the role of rehabilitation to promote recovery and community reintegration in this population.
Keywords: Coronavirus, Disability evaluation, Outcome assessment, Physical therapy modalities, Rehabilitation
List of abbreviations: ARF, acute respiratory failure; CIRS, Cumulative Illness Rating Scale; COVID-19, coronavirus disease 2019; CPAP, continuous positive airways pressure; FiO2, inspiratory fraction of oxygen; IMV, invasive mechanical ventilation; NIV, noninvasive ventilation; SpO2, percentage of oxygen saturation; SPPB, Short Physical Performance Battery; 4-MGS, 4-meter gait speed; 5-STS, 5-repetition sit-to-stand
Studies describe a wide variety of clinical presentations for COVID-19 infectious disease, ranging from absence of symptoms to pneumonia with acute respiratory failure (ARF).1 , 2 ARF is associated with prolonged functional impairment in many individuals and the recovery from this critical illness is fraught with challenges.3 Local unpublished data estimate that approximately 40% of patients with COVID-19 present ARF, with or without need for hospitalization. A recent study by Belli et al4 showed that 75% of patients entering a COVID-19 ward after acute hospitalization exhibited very low physical functioning and experienced impaired performance of daily physical activities. Further improvement in our understanding of the factors that influence physical function recovery after critical illness may help survivors and inform of the challenges and milestones of their recovery period,5 along with the appropriate prescription of rehabilitation interventions.6
The aim of this pragmatic cross-sectional study was to show the level of physical function in a cohort of patients with COVID-19 with ARF due to pneumonia, who were admitted to a subacute unit to stabilize their condition. The secondary aim was to investigate which clinical characteristics during hospitalization could predict physical function, assessed by the Short Physical Performance Battery (SPPB) test.7
Methods
Consecutive patients recovering from ARF due to COVID-19 pneumonia were admitted from the Emergency Area of several acute hospitals to a subacute Unit of the Clinical Scientific Maugeri Institute of Lumezzane from March 10, 2020 to April 30, 2020. The change of hospital policy was because of the emergency situation of the COVID-19 pandemic in Italy. This was a retrospective study approved by the Local Review Board and Ethics Committee (EC2440, May 26, 2020).
At the point of admission, patients underwent the SPPB test—a standardized, objective, rapid, and simple tool to conduct assessment.7 The SPPB represents the sum of results from 3 functional tests, standing balance, 4-meter gait speed (4-MGS), and 5-repetition sit-to-stand (5-STS) maneuver. Each component is scored based on a subscale, and the 3 subscores are added to obtain a summary score.7 Scores between 0 and 3 denote severe physical function disability, 4 to 6 low function, 7 to 9 intermediate function, and 10 to 12 normal function.7 Predicted values for the SPPB were calculated using normative values for total SPPB score and a European population aged ≥40 years, stratified for age and sex.8
SPPB scores have been previously shown to be highly predictive of disability, hospitalization, institutionalization, and mortality in older patients.9 The Cumulative Illness Rating Scale10 score was used to assess the number of comorbidities, whereas cognitive deficits were defined using a Mini Mental State Examination score <20 points. We defined the presence of previous disability as the inability to walk without assistance or a walking aid for at least 45 meters before COVID-19 infection.
Comparisons between groups were performed using an unpaired t test. Stepwise multivariate linear regression analysis was employed to investigate predictors of physical function captured by the SPPB score, from patient demographic and clinical characteristics (sex, age, BMI, number of comorbidities, Fio 2 and SpO2 at admission, use of invasive ventilation, use of noninvasive ventilation or continuous positive airway pressure, presence of tracheostomy, hospital length of stay, and previous disability). P<.05 was considered statistically significant.
Results
Table 1 shows demographic and clinical data of all 184 consecutive patients hospitalized in the subacute unit.
Table 1.
Patient Characteristics in All Population and in Subgroups of Patients With SPPB Score ≤3.0 and SPPB Score >3.0
| Variables | All (N=184) | SPPB ≤3.0 (n=118) | SPPB >3.0 (n=66) | P |
|---|---|---|---|---|
| Male, % | 51.63 | 46.61 | 60.61 | .068 |
| Age, y | 74±12 | 78±11 | 69±11 | .001 |
| Patients with age <60 y, % | 11.96 | 22.73 | 5.93 | .001 |
| Patients with age >85 y, % | 17.39 | 25.42 | 3.03 | .001 |
| CIRS score | 3.44±2.16 | 4.08±2.35 | 2.29±1.75 | .001 |
| BMI score | 26.24±4.80 | 26.23±5.10 | 26.27±4.36 | .9601 |
| Absence of any comorbidities, % | 8.15 | 5.93 | 12.12 | .001 |
| More than 2 comorbidities, % | 43.48 | 57.63 | 18.18 | .001 |
| Previous disability, % | 32.61 | 44.07 | 12.12 | .001 |
| Cognitive deficits, % | 10.87 | 16.10 | 1.52 | .002 |
| Length of acute hospital stay, d | 14±10 | 15±11 | 13±8 | .096 |
| Tracheotomy, % of patients | 4.35 | 5.93 | 1.52 | .159 |
| Only NIV/CPAP, % of patients | 21.74 | 23.73 | 18.18 | .382 |
| NIV+IMV, % of patients | 8.70 | 11.02 | 4.55 | .135 |
| FiO2, % | 28.5±11.72 | 28.39±12.46 | 26.68±10.35 | .875 |
| SpO2, % | 94.97±2.17 | 94.76±2.22 | 95.35±2.06 | .079 |
| SpO2/FiO2 | 370±98 | 372±99 | 365±97 | .627 |
NOTE. Values are presented as mean ± SD or as a percentage.
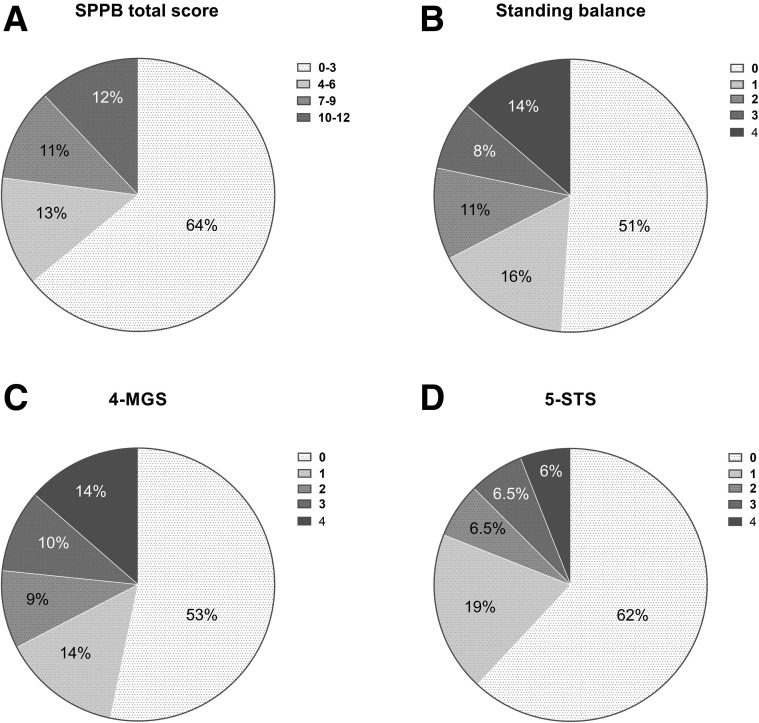
The total SPPB score was 3.1±3.9 (26.8± 33.4% predicted normal), with 64% of patients exhibiting SPPB scores ≤3.0. Mean values for the balance score was 1.2±1.5, 1.2±1.5 for the 4-MGS score, and 0.8±1.2 for the 5-STS score. The 4-MGS duration was 7.7±3.8 seconds and the 5-STS duration was 17.76±6.71 seconds.
Figure 1 depicts the SPPB score distribution in relation to severity levels. Differences between patients with a SPPB score ≤3.0 (bedbound patients) and those with SPPB >3.0 were significant for age, the number of comorbidities, absence of any reported comorbidities, cognitive deficits, and the presence of previous disabilities (see table 1).
Fig 1.
Physical function disability evaluated by SPPB (as total score, panel A) and for each component of SPPB test (panels B-D). Fractional representation of patients (N=184) relative to the total SPPB score (A), the standing balance score (B), the 4-MGS score (C), and the 5-STS score (D).
On the basis of stepwise linear regression analysis including all baseline variables, a better functional status (higher SPPB score) was inversely related to previous disability (B= –2.9839, SE=0.494, P<.001), age (B= –0.1916, SE=0.021, P<.001), invasive mechanical ventilation (B= –3.8802, SE=0.9035, P<.001), use of noninvasive mechanical ventilation (NIV/CPAP) (B=–2.3928, SE=0.6061, P=.001) (R 2 of regression model was 0.4292). Nevertheless, patients with comorbidities (n=169, 91.85%) show highest physical impairment (SPPB 2.86 [3.78], 25 [32.58] % predicted normal) when compared with patients without comorbidities (n=15, 8.15%) (SPPB score 5.67±1.12 [47.2 ±36.3%] predicted normal) (P<.001).
When compared with patients with comorbidities, patients without any comorbidities were younger (56.47±10.32 vs 76.05±10.48 years, P<.001) but with longer length of hospital stay (19.73±10.74 vs 13.87±9.59 days, P=.0263), having undergone tracheostomy (26.67% vs 2.37%, P=.001), and required more invasive mechanical ventilation (46.67% vs 5.33%, P=.001) and noninvasive ventilation (46.67% vs 19.53%, P=.015).
Discussion
This pragmatic study highlights that physical function disability is highly prevalent in patients recovering from ARF after COVID-19 infection, being present in approximately two-thirds of patients admitted to a dedicated subacute COVID-19 Unit. The study confirms recent data from the literature,4 demonstrating that age, mechanical ventilation need, and previous disability may strongly influence this functional impairment.
In non-COVID ARF survivors with SPPB scores ≤3.0, physical function either does not recover within 6 months, or it improves initially but survivors remain functionally disabled by 6 months.3 Similarly to patients recovering from severe influenza A,11 those with an acute COVID event may have functional damage both in the short- and long-term periods after discharge. Undoubtedly, patients with comorbidities usually take longer to return to their former condition.3
The findings of impaired physical function status in our study population, encompassing severely compromised strength, balance, and walking function, validate relevant recommendations on referral to rehabilitation services for survivors after COVID-19. As the effect of muscle activity associated with viral agents is not known, active mobilization and low intensity exercise are indicated in this postacute phase, when safe to do so, to improve physical capacity and prevent the development of persistent disability.12
Variables predicting a pathologic SPPB score include age, invasive ventilation and noninvasive ventilation use and physical function status in ARF survivors.3, 4, 5 Interestingly, our study suggests that comorbidities are also predominant in patients with COVID-19 with ARF, with significant physical function disability, whereas absence of any comorbidity is associated with better functional status, albeit not completely eliminating the risk of suffering profound functional limitations. Accordingly, alert protocols for the early detection of deterioration in physical performance and early physiotherapy interventions should be considered for all patients, but particularly for those with comorbidities.
Importantly, our study confirms the value of the SPPB instrument to stratify physical function as part of the onward referral process to rehabilitation services, in the absence of more sophisticated testing due to infection risk. The routine bedside use of a simple and well documented test, such as the SPPB test, has been well accepted and deemed useful in this population.
Study limitations
The main limitations of our report are (1) the possible low external validity, as the study only included patients who needed an intermediate care setting, therefore only representing a partial picture of the COVID-19 population discharged from an acute context (we did not take into account patients who remained in a high-intensity care setting and patients with mild illness who were discharged home); (2) the limited number of variables we included in our regression analysis (due to the lack of other clinical information such as drug therapy performed in the Emergency Area and social status) may limit the amount of valuable information that we could gather from our results; and (3) the emergency situation in which the study was conducted affecting hospital capacity, patient increase, resources, and so on, which could have had a negative effect on patient autonomy.
Conclusions
The majority of survivors after COVID-19 who experienced ARF due to pneumonia exhibit substantial physical dysfunction, influenced by age, mechanical ventilation need, and previous disability. Screening rehabilitation needs in the acute and subacute setting should be performed through simple functional and disability assessments. Future studies on rehabilitation interventions are mandatory in order to define the role rehabilitation could play in those recovering from COVID-19 pneumonia, as severe dysfunction is observed among these patients.
Acknowledgments
We thank all physiotherapists of Istituti Clinici Scientifici Maugeri IRCCS, Respiratory Rehabilitation of the Institute of Lumezzane (BS) and Veruno (NO), who treated the patients enrolled in this study, and Laura Comini PhD for technical assistance and editing.
Footnotes
Supported by the “Ricerca Corrente” funding scheme of the Italian Ministry of Health.
Disclosures: none.
References
- 1.Lian J., Jin X., Hao S., et al. Analysis of epidemiological and clinical features in older patients with corona virus disease 2019 (COVID-19) out of Wuhan. Clin Infect Dis. 2020;71:740–747. doi: 10.1093/cid/ciaa242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C.Y., Calfee C.S., Paul D.W., et al. One-year mortality and predictors of death among hospital survivors of acute respiratory distress syndrome. Intensive Care Med. 2014;40:388–396. doi: 10.1007/s00134-013-3186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gandotra S., Lovato J., Case D., et al. Physical function trajectories in survivors of acute respiratory failure. Ann Am Thorac Soc. 2019;16:471–477. doi: 10.1513/AnnalsATS.201806-375OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belli S., Balbi B., Prince I., et al. Low physical functioning and impaired performance of activities of daily life in COVID-19 patients who survived the hospitalisation. Eur Respir J. 2020;56:2002096. doi: 10.1183/13993003.02096-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Herridge M.S., Chu L.M., Matte A., et al. RECOVER Program Investigators (Phase 1: towards RECOVER); Canadian Critical Care Trials Group. The RECOVER program: disability risk groups and 1-year outcome after 7 or more days of mechanical ventilation. Am J Respir Crit Care Med. 2016;194:831–844. doi: 10.1164/rccm.201512-2343OC. [DOI] [PubMed] [Google Scholar]
- 6.Brown S.M., Wilson E.L., Presson A.P., et al. Understanding patient outcomes after acute respiratory distress syndrome. Identifying subtypes of physical, cognitive and mental health outcomes. Thorax. 2017;72:1094–1103. doi: 10.1136/thoraxjnl-2017-210337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guralnik J.M., Simonsick E.M., Ferrucci L., et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 8.Bergland A., Strand B. Norwegian reference values for the Short Physical Performance Battery (SPPB): the Tromsø Study. BMC Geriatr. 2019;19:216. doi: 10.1186/s12877-019-1234-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Studenski S., Perera S., Wallace D., et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322. doi: 10.1046/j.1532-5415.2003.51104.x. [DOI] [PubMed] [Google Scholar]
- 10.Salvi F., Miller M.D., Grilli A., et al. A manual of guidelines to score the modified Cumulative Illness Rating Scale and its validation in acute hospitalized elderly patients. J Am Geriatr Soc. 2008;56:1926–1931. doi: 10.1111/j.1532-5415.2008.01935.x. [DOI] [PubMed] [Google Scholar]
- 11.Luyt C.E., Combes A., Becquemin M.H., et al. Long-term outcomes of pandemic 2009 influenza A(H1N1)-associated severe ARDS. Chest. 2012;142:583–592. doi: 10.1378/chest.11-2196. [DOI] [PubMed] [Google Scholar]
- 12.Vitacca M., Carone M., Clini E.M., et al. Joint statement on the role of respiratory rehabilitation in the COVID-19 crisis: the Italian position paper. Respiration. 2020;99:493–499. doi: 10.1159/000508399. [DOI] [PMC free article] [PubMed] [Google Scholar]