Abstract
Objectives
Baduanjin exercise is a form of Qigong exercise therapy that has become increasingly popular worldwide. The aims of the current systematic review were to summarize reported adverse events potentially associated with Baduanjin exercise based on currently available literature and to evaluate the quality of the methods used to monitor adverse events in the trials assessed.
Methods
The English databases PubMed, Cochrane library, and EMbase were searched from inception to October 2020 using the keywords “Baduanjin” or “eight session brocade.” Only studies that included Baduanjin exercise therapy were included.
Results
Forty-seven trials with a total of 3877 participants were included in this systematic review. Twenty-two studies reported protocols for monitoring adverse events, and two studies reported the occurrence of adverse events during training. The adverse events reported included palpitation, giddiness, knee pain, backache, fatigue, nervousness, dizziness, shoulder pain, chest tightness, shortness of breath, and muscle ache.
Conclusions
Only two studies reported adverse events that were potentially caused by Baduanjin exercise. Adverse events related to Baduanjin exercise in patients with chronic fatigue syndrome may include muscle ache, palpitation, giddiness, knee pain, backache, fatigue, nervousness, dizziness, shoulder pain, chest tightness, and shortness of breath. Further studies conducted in accordance with the Consolidated Standards of Reporting Trials statement guideline incorporating monitoring of adverse events are recommended. Additional clinical trials in which Baduanjin exercise is used as a main intervention are needed, and further meta-analysis may be required to assess its safety and reach more informed conclusions in this regard in the future.
1. Introduction
Qigong exercise is a core part of traditional Chinese medicine therapy that has existed for more than 2000 years [1]. Baduanjin is one of the traditional Chinese Qigong exercise therapies of mild to moderate intensity, and it is considered to be an effective approach to promoting health [2]. It emphasizes the mind-body connection, slow movements while breathing deeply, and muscle stretching with mental concentration; it also has profound therapeutic effects in patients with various medical conditions [3–8]. Although Baduanjin has been practiced for thousands of years in China, globally it is not as popular as Tai Chi [1, 9]. To date, no review has systematically investigated the safety of Baduanjin.
The reporting of adverse events (AEs) is vital when introducing and evaluating a new therapy. An AE has been defined as any unwanted experience during a study regardless of whether the AE was directly related to an intervention [10]. Standard reporting of AEs is suggested in the Consolidated Standards of Reporting Trials (CONSORT) statement [11]. It is strongly recommended that AEs should be described in the Results sections of published reports [12]. Despite existing guidelines on the reporting of AEs [11], the degrees to which AEs are described in experimental studies are still inadequate [13, 14]. Insufficient reporting of AEs may lead to skepticism, criticism, and even rejection of a therapy.
To address the above-described research gaps with respect to Baduanjin exercise, a systematic review of the available evidence on its safety is needed. Accordingly, the main purpose of the present systematic review was to investigate and summarize the AEs reported in previous studies that included Baduanjin exercise. A secondary aim was to evaluate the quality of the methods used to monitor AEs in the studies assessed.
2. Methods
2.1. Guideline Adherence and Eligibility Criteria
The current analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Only studies published in English were included. Studies involving patients with medical conditions and studies using healthy participants were included. No restrictions on sociodemographic characteristics were applied. Experimental studies that included any type of Baduanjin exercise were included. No restrictions on the types of Baduanjin interventions or control interventions were applied.
2.2. Types of Outcome Measures
The definition of an AE was any undesirable experience during the study period. AEs were categorized as serious, non-serious, and intervention-related using a prior meta-analytic review as a guide [15]. Serious AEs were defined as those associated with hospitalization or medical or surgical needs, and those that were potentially life-threatening or resulted in death. Other AEs were defined as non-serious.
2.3. Search Methods
The PubMed, Cochrane library, and Embase electronic databases from inception to October 2020 were searched. The search string used to search PubMed and Embase was Baduanjin [Title/Abstract] OR eight session brocade [Title/Abstract]. The search string used to search the Cochrane library was Baduanjin [Title/Abstract/Keyword] OR eight session brocade [Title/Abstract/Keyword].
Initial screening to exclude duplicate and irrelevant studies based on article titles was conducted by the first author (Fang). The abstracts of the remaining studies were then independently reviewed by two authors (Fang and Zhang). The remaining full texts were then reviewed by two different independent authors with reference to the eligibility criteria (Wu and Ye). Only research articles that met the selection criteria were included in the subsequent review and assessment. The References sections of relevant articles were also reviewed by the authors. Consensus was reached via discussion if there were disagreements between two reviewers. Only reports published in English were included in the analysis [16].
2.4. Data Extraction and Management
Data extraction from the reports identified included characteristics of the timing, frequency, and types of AEs reported based on the Extension of the CONSORT statement [11], and it was performed by both Fang and Zhang independently. All authors participated in discussion to reach a consensus in cases of disagreements. In two cases in which researchers had not clearly described AEs in their published articles, we emailed the corresponding authors seeking further details on intervention-related AE data and baseline data. Only one of these corresponding authors emailed us back in response to our questions. All of the authors of the current study discussed the AEs that remained unclear in the second study due to the lack of a response from the corresponding author, and made collective judgments with respect to those AEs.
3. Results
3.1. Reports Identified
A total of 322 records were initially identified. Of these, 112 full-text articles were subsequently obtained based on the predetermined selection criteria, and a total of 47 articles were ultimately included in the current review. The flow of the literature search is presented in Figure 1.
Figure 1.
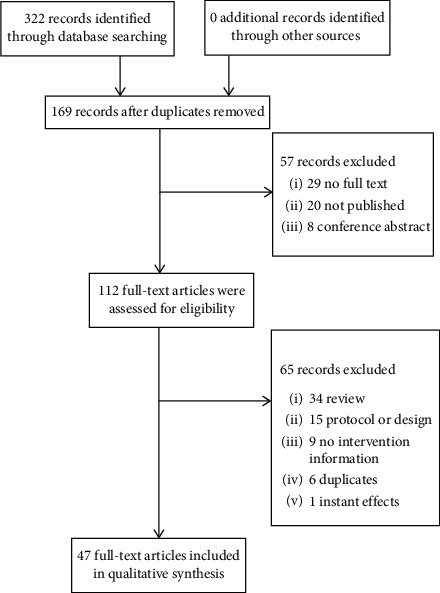
The flow of the literature search.
3.2. Characteristics of Participants and Settings
A combined total of 3877 participants were included in the trials assessed in the final analysis, 2343 women and 1234 men; 3 studies did not report the exact number of males and females [17–19]. The mean ages in individual studies ranged from 20.8 to 83.0 years, and the median mean age was 60.1 years (interquartile range 49.9–65.5 years). The percentages of female participants in the studies ranged from 0% to 100%, and the median was 66.1% (interquartile range 38.7–80.2%).
The sample sizes in the reports ranged from 1 to 271, and the median was 68 (interquartile range 42–110). Most of the studies were conducted in China, including ten in Fujian [20–29], six in Beijing [19, 30–34], five in Taiwan [35–39], five in Guangdong [7, 40–43], four in Hong Kong [6, 44–46], three in Shanghai [18, 47, 48], two in each of Hebei [49, 50], Jiangsu [51, 52], Sichuan [53, 54], and Hubei [17, 55], and one in each of Tianjin [4], Shanxi [56], Jiangxi [57], and Macau [58]. One study was conducted in Singapore [59], and one study was conducted in the USA [60].
Eleven trials included healthy participants only [17, 20, 22, 30, 33, 36, 37, 39, 49, 55, 60], and the remaining 36 included participants with a variety of physical and mental health conditions [4, 6, 7, 18, 19, 21, 23–29, 31, 32, 34, 35, 38, 40–48, 50–54, 56–59].
3.3. Characteristics of Intervention Groups and Control Groups
The Baduanjin exercise regimes used in the studies varied in content, frequency, duration, and intensity. The majority of studies used standing Baduanjin exercises as an intervention [4, 6, 17–39, 41–59], two studies used a mixed model including standing and sitting Baduanjin exercises [40, 60], and one study used sitting Baduanjin exercises only [7]. The duration of Baduanjin exercise ranged from 12 minutes to 120 minutes. The frequency of sessions varied from once per week to 14 times per week, with overall exercise programs lasting from 8 weeks to 1 year. Five studies did not report the qualifications of instructors [17, 34, 40, 57, 58].
Of the 47 eligible studies, 8 evidently did not include controls [7, 28, 38, 39, 48, 58–60], and 5 used more than two control groups [21–24, 49]. Three studies used walking as a control [34, 42, 54], and other control measures used in single studies were muscle relaxation training [30], reading [6], physical therapy [19], and an aerobic exercise [43]. Twenty-seven studies used non-interventional controls, including usual care [4, 17, 18, 20, 25–27, 29, 31–33, 35–37, 40, 41, 44–47, 50–53, 55–57]. Further details of the characteristics of the studies are presented in Table 1.
Table 1.
Characteristics of included studies.
| Source | Area | Average age (age range) | Study population | No. of men/women | Intervention group | Control group |
|---|---|---|---|---|---|---|
| An et al. [47] | Shanghai | 65 ± 7.36 | Patients with KOA | 0/28 | N = 14 Baduanjin 30 min; 5 times/w; 8 w | N = 14 keep routine as usual 8 w |
|
| ||||||
| An et al. [48] | Shanghai | 65.2 ± 7.3 | Patients with KOA | 3/19 | N = 22 Baduanjin 30 min; 5 times/w; 1y | — |
|
| ||||||
| Bao et al. [60] | American | 83 | Older adults | 3/13 | N = 16 Baduanjin (mixed) 45–50 min; 12 w | — |
|
| ||||||
| Chan et al. [44] | HK | 39 ± 7.93 | Women with chronic fatigue syndrome-like illness | 42/108 | N = 75 Baduanjin 90 min; 16 times/9 w (group training) + ≥30 min; 7 times/w; 9 w (self- practice) | N = 75 keep routine as usual 9 w |
|
| ||||||
| Chan et al. [45] | HK | 32.5–47.0 | Persons with chronic fatigue syndrome-like illness | 0/108 | N = 46 Baduanjin 90 min; 16 times/9 w (group training) + ≥30 min; 7 times/w; 9 w (self-practice) | N = 62 keep routine as usual 9 w |
|
| ||||||
| Chen et al. [36] | Taiwan | 45.16 ± 5.78 | Healthy middle-aged women | 0/87 | N = 44 Baduanjin 3 times/w; 12 w | N = 43 keep routine as usual 12 w |
|
| ||||||
| Chen et al. [37] | Taiwan | 71.75 ± 8.13 | Community-dwelling older people | 19/36 | N = 27 Baduanjin 30 min; 3 times/w; 12 w | N = 28 keep routine as usual 12 w |
|
| ||||||
| Chen et al. [53] | Sichuan | 60.10 ± 7.06 | Patients with chronic obstructive pulmonary disease | 147/85 | N = 117 usual care + Baduanjin 30 min; 7 times/w; 3 m | N = 115 usual care 3 m |
|
| ||||||
| Chen et al. [7] | Guangdong | 62 | Patients with dysfunctional ventilatory weaning response | 1/0 | N = 1 usual care + Baduanjin (sitting Baduanjin) 30 min; 2 times/d; 19 d | — |
|
| ||||||
| Chen et al. [38] | Taiwan | 38.9 ± 9.6 | People with severe mental illness | 8/3 | N = 11 Baduanjin 90 min; 2 times/w; 8 w | — |
|
| ||||||
| Chen et al. [30] | Beijing | 22.5 ± 2.0 | Healthy college students | 16/26 | N = 21 Baduanjin 90 min; 5 times/w; 8 w | N = 21 muscle relaxation training 90 min; 5times/w; 8 w |
|
| ||||||
| Chen et al. [35] | Taiwan | 70.29 ± 13.53 | Patients with stable heart failure | 42/38 | N = 39 Baduanjin 35 min; 3 times/w; 12 w | N = 41 keep routine as usual 12 w |
|
| ||||||
| Chen et al. [40] | Guangdong | 60.7 ± 11.12 | Patients with AMI after PCI | 59/23 | N = 43 usual care + Baduanjin (mixed) 30 min; 2 times/d; 3 d (sitting Baduanjin) 30 min; 5 times/w; 4 d-24 w (standing Baduanjin) | N = 39 keep routine as usual 24 w |
|
| ||||||
| Cheung et al. [46] | HK | 41.75 ± 8.99 | Women survivors of intimate partner violence | 0/271 | N = 136 Baduanjin 120 min; 2 times/w; 6 w (group training) + 60 min; 1 time/w; 7–22 w (group follow-up) +30 min; 7 times/w; 1–22 w (self-practice) | N = 135 keep routine as usual 22 w |
|
| ||||||
| Dong et al. [57] | Jiangxi | 30–65 | Patients with phlegm-dampness hypertension | 26/21 | N = 23 Baduanjin 60 min; 5 times/w; 16 w | N = 24 usual care 16 w |
|
| ||||||
| Fan et al. [41] | Shenzhen | 71.1 ± 6.3 | Elderly patients with sleep disturbances | 34/105 | N = 67 Baduanjin 45 min; 5 times/w; 24 w | N = 72 keep routine as usual 24 w |
|
| ||||||
| Han et al. [31] | Beijing | 56 ± 8.86 | Postoperative non-small cell lung cancer patients | 28/32 | N = 30 Baduanjin 60 min; 3 times/w; 1 w (training); 30 min; 10 times/w; 2 w-3 m (self-practise) | N = 30 keep routine as usual 3 m |
|
| ||||||
| Hsu et al. [39] | Taiwan | 49.93 ± 4.38 | Middle-aged women | 0/31 | N = 31 Baduanjin 20 min; 3 times/w; 12 w | — |
|
| ||||||
| Jin et al. [17] | Wuhan | 34.2 ± 14.57 | Physically healthy people | Not mentioned | N = 55 Baduanjin 30–60 min; ≥3 times/w; 16 w | N = 55 keep routine as usual 16 w |
|
| ||||||
| Jing et al. [49] | Tangshan | 75.08 ± 5.26 | Elderly housebound | 40/78 | N = 39 Baduanjin 60–90 min; 2 times/m; 3 m 1times/m; 3–6 m | N = 79 control group1: CBT 6 m control group2: Baduanjin + CBT 60–90 min; 2 times/m; 3 m 1 time/m; 3–6 m |
|
| ||||||
| Li et al. [55] | Wuhan | 34.2 ± 14.6 | Physically healthy adults | 36/74 | N = 55 Baduanjin 30–60 min; 3 times/w; 16 w | N = 55 keep routine as usual 16 w |
|
| ||||||
| Li et al. [20] | Fuzhou | 20.78 ± 1.1 | Healthy college students | 36/170 | N = 101 Baduanjin 60 min; 5 times/w; 12w | N = 105 keep routine as usual 12w |
|
| ||||||
| Li et al. [54] | Sichuan | 50.98 ± 7.76 | Patients with schizophrenia | 47/14 | N = 30 Baduanjin 40 min; 5 times/w; 24 w | N = 31 brisk walking 40 min; 5 times/w; 24 w |
|
| ||||||
| Liang et al. [42] | Guangdong | 55.25 ± 9.38 | Patients with essential hypertensive | 38/22 | N = 30 usual care + Baduanjin 20 min; 10 times/w; 6 m | N = 30 usual care + walking 20 min; 10 times/w; 6 m |
|
| ||||||
| Liao et al. [32] | Beijing | 18–60 | People with fatigue- Predominant subhealth | 33/96 | N = 62 Baduanjin 30 min; 14 times/w; 6 w | N = 67 keep routine as usual 6 w |
|
| ||||||
| Liu et al. [56] | Shanxi | 57.2 ± 5.4 | Women with diabetes | 0/35 | N = 17 Baduanjin 90 min; 6 times/w; 24 w | N = 18 keep routine as usual 24 w |
|
| ||||||
| Liu et al. [21] | Fuzhou | 59.17 ± 7.36 | Patients with KOA | 25/83 | N = 29 Baduanjin 60 min; 5 times/w; 12 w | N = 79 control group1: Taichi 60 min; 5 times/w; 12 w control group2: cycling 60 min; 5 times/w; 12 w control group3: health education 60 min; 1 time/w; 12 w |
|
| ||||||
| Liu et al. [59] | Singapore | 77.1 ± 5.9 | Frail older adults | 3/9 | N = 12 Baduanjin 90 min; 2 times/w; 4 w (training) 90 min; 3 times/w; 5–16 w (self-practise) | — |
|
| ||||||
| Lu et al. [51] | Nanjing | 55.11 ± 11.51 | Patients with colorectal cancer undergoing chemotherapy | 56/31 | N = 43 Baduanjin 20–40 min; ≥5 times/w; 24 w | N = 44 usual care 24 w |
|
| ||||||
| Mao et al. [43] | Beijing | 60.86 ± 10.63 | Patients after acute myocardial infarction | 73/37 | N = 56 Baduanjin 30 min; 2 times/w; 12 w | N = 54 aerobic exercise 30 min; 2 times/w; 12 w |
|
| ||||||
| Tao et al. [22] | Fuzhou | 61.29 ± 4.85 | Older adults | 20/41 | N = 15 Baduanjin 60 min; 5 times/w; 12 w | N = 46 control group1: Taichi 60 min; 5 times/w; 12w control group2: keep routine as usual 12 w |
|
| ||||||
| Tao et al. [23] | Fuzhou | 65.55 ± 4.40 | Patients with mild cognitive impairment | 18/39 | N = 20 Baduanjin 60 min; 3 times/w; 24 w | N = 37 control group1: brisk walking 60 min; 3 times/w; 24w control group2: health education 30 min/w; 24 w |
|
| ||||||
| Tsang et al. [6] | HK | 80.11 ± 5.63 | Chinese depressed elders with chronic illness | 12/26 | N = 21 Baduanjin 45 min; 3 times/w; 12w | N = 17 reading 45 min; 3 times/w; 12 w |
|
| ||||||
| Wang [33] | Beijing | 59.35 ± 1.6 | Old people | 42/71 | N = 55 Baduanjin 60 min; 5–7 times/w; 6 m | N = 58 keep routine as usual 6 m |
|
| ||||||
| Wang et al. [18] | Shanghai | 65.19 ± 4.88 | Patients with essential hypertensive | Not mentioned | N = 61 usual care + Baduanjin 20–30 min; 4-5 times/w; 1 y | N = 61 usual care 1 y |
|
| ||||||
| Wang et al. [4] | Tianjin | 54.09 ± 7.76 | Breast cancer survivors | 0/86 | N = 46 Baduanjin ≥20 min; 7 times/w; 6 m | N = 40 Keep routine as usual 6 m |
|
| ||||||
| Xia et al. [24] | Fuzhou | 65.51 ± 4.35 | Older adults with mild cognitive impairment | 23/46 | N = 23 Baduanjin + health education Baduanjin:60 min; 3 times/w; 24w + Health education:30 min; 1 time/8 w; 24 w | N = 46 control group1: brisk walking + health education brisk walking:60 min; 3 times/w; 24w + health education:30 min; 1 time/8 w; 24 w control group2: keep routine as usual + health education 30 min; 1 time/8 w; 24 w |
|
| ||||||
| Xiao et al. [19] | Beijing | 67.8 ± 9.4 | Patients with Parkinson's disease | Not mentioned | N = 35 Baduanjin 60 min; 4 times/w; 6 m | N = 33 physical therapy 6 m |
|
| ||||||
| Xiao et al. [34] | Beijing | 67.53 ± 8.56 | Patients with idiopathic Parkinson's disease | 67/29 | N = 48 Baduanjin + walk Baduanjin:12–15 min; 4 times/w; 6m + walk: ≥30 min; 7 times/w; 6 m | N = 48 walk ≥30 min; 7 times/w; 6 m |
|
| ||||||
| Xiao et al. [50] | Hebei | Not mentioned | Adults with cardiovascular diseases | 50/79 | N = 66 Baduanjin 24 min; 5 times/w; 16 w | N = 63 Keep routine as usual 16 w |
|
| ||||||
| Xie et al. [52] | Nanjing | 37.39 ± 11.35 | Patients with ankylosing spondylitis | 35/11 | N = 23 Baduanjin 2times/w; 4 w (instruction) ≥3 times/w; 5–12 w (self-practise) | N = 23 Keep routine as usual 12 w |
|
| ||||||
| Ye et al. [25] | Fuzhou | 63.78 ± 6.39 | Patients with KOA | 25/25 | N = 25 Baduanjin 40 min; 3 times/w; 12 w | N = 25 Keep routine as usual 12 w |
|
| ||||||
| Ye et al. [26] | Fuzhou | 64.36 ± 5.34 | Older adults with KOA | 19/37 | N = 28 Baduanjin 40 min; 3 times/w; 12 w | N = 28 Keep routine as usual 12 w |
|
| ||||||
| Zhang et al. [58] | Macau | 24 ± 7 | Women with premenstrual syndrome | 0/40 | N = 40 Baduanjin (8 sessions) 14 times/w; 3consecutive menstrual cycles | — |
|
| ||||||
| Zheng et al. [28] | Fuzhou | 60 | Elderly Population at risk for Ischemic stroke | 11/9 | N = 20 Baduanjin 30 min; 3-5 times/w; 12 w | |
|
| ||||||
| Zheng et al. [27] | Fuzhou | 60.14 ± 6.3 | Community adults at risk of ischamic stroke | 61/109 | N = 85 Baduanjin 60 min; 5 times/w; 12 w | N = 85 keep routine as usual 12 w |
|
| ||||||
| Zheng et al. [29] | Fuzhou | 62.19 ± 7.87 | Patients with post-stroke cognitive impairment | 41/7 | N = 24 usual care + Baduanjin 40 min; 3 times/w; 24 w | N = 24 usual care 24 w |
HK: Hong Kong; KOA: knee osteoarthritis; CBT: cognitive behavioral therapy; min: minutes; w: week; m: month; y: year; N/No: number; AMI: acute myocardial infarction; PCI: percutaneous coronary intervention.
3.4. Patterns of AEs
Of the 47 studies assessed, 22 reported protocols used to monitor AEs [4, 6, 17, 20, 21, 26, 27, 29, 32, 35, 37, 38, 40, 41, 43, 44, 46–48, 52, 55, 59], but only 2 reported the actual occurrence of AEs during the trial [44, 52]. Of these two studies, one reported muscle ache only [52] and the other reported muscle ache, palpitation, giddiness, knee pain, backache, fatigue, nervousness, dizziness, shoulder pain, chest tightness, and shortness of breath [44] (Table 2).
Table 2.
The types of adverse events in both groups.
| Source | Tre | Tse | Tnon | Cre | Cse | Cnon | Tdropout | Cdropout | F-U |
|---|---|---|---|---|---|---|---|---|---|
| An et al. [47] | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 4 | 4 m |
| An et al. [48] | 0 | 0 | 0 | — | — | — | 6 | — | No |
| Bao et al. [60] | Unclear | Unclear | Unclear | — | — | — | 9 | — | No |
| Chan et al. [44] | 24 muscle ache | 0 | 4 palpitation; 3 giddiness; 2 knee pain; 2 backache; 2 fatigue; 2 nervousness; 2 dizziness; 1 shoulder pain; 1 chest tightness; 1 shortness of breath | 0 | 0 | 0 | 18 | 17 | No |
| Chan et al. [45] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 0 | 0 | 3 m |
| Chen et al. [17] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 1 | 2 | No |
| Chen et al. [37] | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | No |
| Chen et al. [53] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 3 | 5 | No |
| Chen et al. [7] | — | — | — | — | — | — | — | — | No |
| Chen et al. [38] | 0 | 0 | 0 | — | — | — | 5 | — | 8 w |
| Chen et al. [30] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 0 | 0 | No |
| Chen et al. [35] | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 8 | No |
| Chen et al. [40] | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 9 | No |
| Cheung et al. [46] | 0 | 0 | 0 | 0 | 0 | 0 | 16 | 8 | No |
| Dong et al. [57] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 2 | 3 | No |
| Fan et al. [41] | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 9 | No |
| Han et al. [31] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | No | No | No |
| Hsu et al. [39] | Unclear | Unclear | Unclear | — | — | — | 0 | — | No |
| Jin et al. [17] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | No |
| Jing et al. [49] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 1 | 1 | No |
| Li et al. [55] | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 0 | No |
| Li et al. [20] | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 4 | 12 w |
| Li et al. [54] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 0 | 0 | 0 |
| Liang et al. [42] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | No | No | No |
| Liao et al. [32] | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 12 |
| Liu et al. [56] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 3 | 2 | No |
| Liu et al. [21] | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 26 | No |
| Liu et al. [59] | 0 | 0 | 0 | — | — | — | 1 | — | No |
| Lu et al. [51] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 2 | 1 | No |
| Mao et al. [43] | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 3 | No |
| Tao et al. [22] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 10 | 4 | No |
| Tao et al. [23] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 3 | 9 | No |
| Tsang et al. [6] | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | No |
| Wang [33] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | No | No | No |
| Wang et al. [18] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | No | No | No |
| Wang et al. [4] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | No |
| Xia et al. [24] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 3 | 6 | No |
| Xiao et al. [19] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 14 | 16 | No |
| Xiao et al. [34] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 3 | 4 | No |
| Xiao et al. [50] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 1 | 4 | No |
| Xie et al. [52] | 7 muscle ache | 0 | 0 | 0 | 0 | 0 | 7 | 7 | No |
| Ye et al. [25] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | 0 | 0 | No |
| Ye et al. [26] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | No |
| Zhang et al. [58] | Unclear | Unclear | Unclear | — | — | — | 9 | — | No |
| Zheng et al. [28] | Unclear | Unclear | Unclear | — | — | — | 0 | — | No |
| Zheng et al. [27] | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 16 | No |
| Zheng et al. [29] | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 8 | 4 w |
Abbreviations. Tre: related adverse events of intervention group; Tse: serious adverse events of intervention group; Tnon: non-serious adverse events of intervention group; Cre: related adverse events of control group; Cse: serious adverse events of control group; Cnon: non-serious adverse events of control group; Tdropout: dropouts of intervention group; Cdropout: dropouts of control group; F-U: follow-up; m: month; w: week.
4. Discussion
Baduanjin exercise is becoming increasingly popular around the world as it has been associated with therapeutic benefits for various medical conditions. It is now offered in hospital and community settings across China to reduce clinical symptoms and improve quality of life. The risk of harm from Baduanjin exercise may be minor, as suggested by the current systematic review, and older adults or patients with chronic illness are more likely to experience benefits associated with its clinical effects and affordability.
In the present systematic review, the reporting of AEs in Baduanjin exercise studies was insufficient, and this limits the conclusions that can be drawn to date about its safety [10]. A total of 47 studies with a combined total of 3877 participants were included in the current systematic review. Of the 47 studies, 22 reported the utilization of protocols to monitor AEs, and 2 reported the actual occurrence of AEs. The AEs reported included palpitation, giddiness, knee pain, backache, fatigue, nervousness, dizziness, shoulder pain, chest tightness, shortness of breath, and muscle ache. Some studies reported AEs at the end of the study, which may have resulted in recall bias. More frequent measures to identify AEs, and the incorporation of multiple modalities via which to report AEs throughout the study (interviews, questionnaires, and tests), may contribute to the generation of more reliable evidence [12].
None of the studies in the current systematic review reported any serious AEs. The most commonly reported AE related to Baduanjin exercise was muscle ache [44, 52], which is consistent with previous observations in other exercise studies [61–65]. Notably, some Baduanjin exercises entail a semi-squat position, for example, “Session 2, Open the Arms as an Archer Shooting Both Left- and Right-Handed”; “Session 5, Sway the Head and Shake the Tail”; and “Session 7, Grip the Palms to Improve Strength” [25]. In such sessions, participants are required to coordinately move upper limbs and trunks while in a semi-squat position, which may greatly improve muscle strength, particularly that of the lower extremities. These types of Baduanjin exercises may have contributed to the mild muscle aches reported during the first 2 weeks of practice [44, 52].
In one trial that included participants with chronic fatigue syndrome (CFS), 24 AEs were reported after Baduanjin exercise [44], which is consistent with other physical exercise studies in individuals with CFS [66]. This suggests that patients with CFS may experience some non-serious AEs after standard Baduanjin exercises. Notably however, that report [44] only mentions the monitoring of AEs in the intervention group, and there is no information regarding AEs in the control group. Further research is needed that incorporates the monitoring and reporting of all AEs in both intervention and control groups based on the CONSORT statement, to facilitate informative conclusions in patients with CFS.
The current study had several limitations. Only reports published in English were included. Additional potentially relevant studies may have been conducted that were published in other languages. Secondly, the number of trials included in the review was small, and they only employed descriptive statistics and summaries of AEs. Further meta-analyses assessing AEs potentially associated with Baduanjin exercise may be conducted.
5. Conclusion
Estimation of any potential harm related to a novel therapy is a vital consideration when promoting that therapy. Poor reporting of AEs may substantially limit the conclusions that can be drawn relating to Baduanjin exercise. The number of trials with strict reporting of AEs is small. One of the studies in the current analysis suggests that AEs related to Baduanjin exercise in patients with CFS may include muscle ache, palpitation, giddiness, knee pain, backache, fatigue, nervousness, dizziness, shoulder pain, chest tightness, and shortness of breath. It is recommended that in future studies AEs are rigorously monitored and strictly reported in accordance with the CONSORT guideline. Further meta-analysis may enhance understanding of the safety of Baduanjin exercise in the future.
Acknowledgments
This work was supported by Central Guide to Local Science and Technology Development (Grant No. 2018L3009).
Contributor Information
Jiajia Ye, Email: ye.j.ye@connect.polyu.hk.
Shuhe Cai, Email: 13706989977@139.com.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Disclosure
The funder had no role during the entire process of this study.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Authors' Contributions
Jiajia Ye, Fangzhen Wu, and Shuhe Cai contributed to conceptualization; Jianqi Fang, Fangzhen Wu, and Liying Zhang contributed to data curation; Jianqi Fang and Fangzhen Wu contributed to formal analysis; Jiajia Ye and Shuhe Cai contributed to funding acquisition; Jiajia Ye and Liying Zhang contributed to investigation; Jianqi Fang and Liying Zhang contributed to methodology; Jiajia Ye and Shuhe Cai contributed to project administration; Jiajia Ye and Shuhe Cai contributed to resources; Jianqi Fang and Fangzhen Wu contributed to software; Jiajia Ye, Xiaowen Lian, and Shuhe Cai contributed to supervision; Jiajia Ye, Xiaowen Lian, and Shuhe Cai contributed to validation; Jiajia Ye and Shuhe Cai contributed to visualization; Jianqi Fang and Jiajia Ye prepared original draft; Jiajia Ye, Liying Zhang, Xiaowen Lian, and Shuhe Cai partcicpated in review and editing.
Supplementary Materials
The supplementary data file includes the comparison list of PRISMA Checklist.
References
- 1.Koh T. C. Baduanjin—an ancient Chinese exercise. The American Journal of Chinese Medicine. 1982;10(1—4):14–21. doi: 10.1142/s0192415x8200004x. [DOI] [PubMed] [Google Scholar]
- 2.Zou L., Pan Z., Yeung A., et al. A review study on the beneficial effects of baduanjin. The Journal of Alternative and Complementary Medicine. 2018;24(4):324–335. doi: 10.1089/acm.2017.0241. [DOI] [PubMed] [Google Scholar]
- 3.Zou L., Wang C., Chen X., Wang H. Baduanjin exercise for stroke rehabilitation: a systematic review with meta-analysis of randomized controlled trials. Int J Environ Res Public Health. 2018;15(4) doi: 10.3390/ijerph15040600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ying W., Min Q. W., Lei T., Na Z. X., Li L., Jing L. The health effects of Baduanjin exercise (a type of qigong exercise) in breast cancer survivors: a randomized, controlled, single-blinded trial. European Journal of Oncology Nursing. 2019;39:90–97. doi: 10.1016/j.ejon.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 5.Zou L., Yeung A., Quan X., et al. Mindfulness-based baduanjin exercise for depression and anxiety in people with physical or mental illnesses: a systematic review and meta-analysis. International Journal of Environmental Research and Public Health. 2018;15(2) doi: 10.3390/ijerph15020321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsang H. W. H., Tsang W. W. N., Jones A. Y. M., et al. Psycho-physical and neurophysiological effects of qigong on depressed elders with chronic illness. Aging & Mental Health. 2013;17(3):336–348. doi: 10.1080/13607863.2012.732035. [DOI] [PubMed] [Google Scholar]
- 7.Chen M., Zeng R. X., Liang X., et al. Seated-baduanjin as an adjuvant rehabilitation treatment for dysfunctional ventilatory weaning response: a case report. Medicine. 2018;97(34) doi: 10.1097/md.0000000000011854.e11854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zou L., Yeung A., Quan X., Boyden S. D., Wang H. A systematic review and meta-analysis of mindfulness-based (baduanjin) exercise for alleviating musculoskeletal pain and improving sleep quality in people with chronic diseases. International Journal of Environmental Research and Public Health. 2018;15(2) doi: 10.3390/ijerph15020206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu J., Chen L., Tu Y., et al. Different exercise modalities relieve pain syndrome in patients with knee osteoarthritis and modulate the dorsolateral prefrontal cortex: a multiple mode MRI study. Brain, Behavior, and Immunity. 2019;82:253–263. doi: 10.1016/j.bbi.2019.08.193. [DOI] [PubMed] [Google Scholar]
- 10.Wayne P. M., Berkowitz D. L., Litrownik D. E., Buring J. E., Yeh G. Y. What do we really know about the safety of tai chi?: a systematic review of adverse event reports in randomized trials. Archives of Physical Medicine and Rehabilitation. 2014;95(12):2470–2483. doi: 10.1016/j.apmr.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Altman D. G., Schulz K. F., Moher D., et al. The revised consort statement for reporting randomized trials: explanation and elaboration. Annals of Internal Medicine. 2001;134(8):663–694. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- 12.Ioannidis J. P. A., Evans S. J. W., Gøtzsche P. C., et al. Better reporting of harms in randomized trials: an extension of the consort statement. Annals Of Internal Medicine. 2004;141(10):781–788. doi: 10.7326/0003-4819-141-10-200411160-00009. [DOI] [PubMed] [Google Scholar]
- 13.Ioannidis J. P. A., Chew P., Lau J. Standardized retrieval of side effects data for meta-analysis of safety outcomes. Journal of Clinical Epidemiology. 2002;55(6):619–626. doi: 10.1016/s0895-4356(02)00393-1. [DOI] [PubMed] [Google Scholar]
- 14.Papanikolaou P. N., Churchill R., Wahlbeck K., Ioannidis J. P. A., The EU-PSI Project P. Safety reporting in randomized trials of mental health interventions. American Journal of Psychiatry. 2004;161(9):1692–1697. doi: 10.1176/appi.ajp.161.9.1692. [DOI] [PubMed] [Google Scholar]
- 15.Cramer H., Ward L., Saper R., Fishbein D., Dobos G., Lauche R. The safety of yoga: a systematic review and meta-analysis of randomized controlled trials. American Journal of Epidemiology. 2015;182(4):281–293. doi: 10.1093/aje/kwv071. [DOI] [PubMed] [Google Scholar]
- 16.Ye J., Cheung W. M., Tsang H. W. H. The neuroscience of nonpharmacological traditional chinese therapy (NTCT) for major depressive disorder: a systematic review and meta-analysis. evidence-based complementary and alternative medicine. Evidence-Based Complementary and Alternative Medicine. 2019;2019:13. doi: 10.1155/2019/2183403.2183403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jin L., Li R., Chen J., Xue Q. B., Yang Y. Q. Surface electromyography Analysis of the lower extremities of subjects participating in baduanjin exercises. Evidence-Based Complementary and Alternative Medicine. 2017;2017:5. doi: 10.1155/2017/1304190.1304190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Q., Ai J. The effect of anti-hypertension gongfa for recovering and treating essential hypertension in the community. China Journal of Pharmaceutical Economics. 2013;8(3):184–186. [Google Scholar]
- 19.Xiao C., Zhuang Y., Kang Y. Effect of health qigong baduanjin on fall prevention in individuals with parkinson’s disease. Journal of the American Geriatrics Society. 2016;64(11):e227–e228. doi: 10.1111/jgs.14438. [DOI] [PubMed] [Google Scholar]
- 20.Li M., Fang Q., Li J., et al. The effect of Chinese traditional exercise-baduanjin on physical and psychological well-being of college students: a randomized controlled trial. PLoS One. 2015;10(7) doi: 10.1371/journal.pone.0130544.e0130544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu J., Chen L., Chen X., et al. Modulatory effects of different exercise modalities on the functional connectivity of the periaqueductal grey and ventral tegmental area in patients with knee osteoarthritis: a randomised multimodal magnetic resonance imaging study. British Journal of Anaesthesia. 2019;123(4):p. 506. doi: 10.1016/j.bja.2019.06.017. [DOI] [PubMed] [Google Scholar]
- 22.Tao J., Chen X., Liu J., et al. Tai chi chuan and baduanjin mind-body training changes resting-state low-frequency fluctuations in the frontal lobe of older adults: a resting-state fMRI study. Frontiers in Human Neuroscience. 2017;11 doi: 10.3389/fnhum.2017.00514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tao J., Liu J., Chen X., et al. Mind-body exercise improves cognitive function and modulates the function and structure of the hippocampus and anterior cingulate cortex in patients with mild cognitive impairment. NeuroImage: Clinical. 2019;23 doi: 10.1016/j.nicl.2019.101834.101834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xia R., Qiu P., Lin H., et al. The effect of traditional Chinese mind-body exercise (baduanjin) and brisk walking on the dorsal attention network in older adults with mild cognitive impairment. Frontiers in Psychology. 2019;10:p. 2075. doi: 10.3389/fpsyg.2019.02075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ye J., Simpson M. W., Liu Y., et al. The effects of baduanjin qigong on postural stability, proprioception, and symptoms of patients with knee osteoarthritis: a randomized controlled trial. Frontiers in Medicine. 2019;6:p. 307. doi: 10.3389/fmed.2019.00307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ye J., Zheng Q., Zou L., et al. Mindful exercise (baduanjin) as an adjuvant treatment for older adults (60 years old and over) of knee osteoarthritis: a randomized controlled trial. Evidence-Based Complementary and Alternative Medicine. 2020;2020:9. doi: 10.1155/2020/9869161.9869161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zheng G., Chen B., Fang Q., Lin Q., Tao J., Chen L. Baduanjin exercise intervention for community adults at risk of ischamic stroke: a randomized controlled trial. Scientific Reports. 2019;9(1):p. 1240. doi: 10.1038/s41598-018-37544-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zheng G., Fang Q., Chen B., Yi H., Lin Q., Chen L. Qualitative evaluation of baduanjin (traditional Chinese qigong) on health promotion among an elderly community population at risk for ischemic stroke. Evidence-Based Complementary and Alternative Medicine. 2015;2015:10. doi: 10.1155/2015/893215.893215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zheng G., Zheng Y., Xiong Z., Ye B. Effect of baduanjin exercise on cognitive function in patients with post-stroke cognitive impairment: a randomized controlled trial. Clinical Rehabilitation. 2020;34(8):1028–1039. doi: 10.1177/0269215520930256. [DOI] [PubMed] [Google Scholar]
- 30.Chen T., Yue G. H., Tian Y., Jiang C. Baduanjin mind-body intervention improves the executive control function. Frontiers in Psychology. 2016;7 doi: 10.3389/fpsyg.2016.02015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Han R., Lin H. S. A clinical study on therapeutic effects of fitness qigong baduanjin on pulmonary function and quality of life of post-operative non-small cell lung cancer patients. Tianjin Journal of Traditional Chinese Medicine. 2016;33(12):715–718. [Google Scholar]
- 32.Liao Y., Lin Y., Zhang C., et al. Intervention effect of baduanjin exercise on the fatigue state in people with fatigue-predominant subhealth: a cohort study. The Journal of Alternative and Complementary Medicine. 2015;21(9):554–562. doi: 10.1089/acm.2014.0395. [DOI] [PubMed] [Google Scholar]
- 33.Wang S. T. Effect of baduanjin on physiological age of intelligence for old people. Journal of Clinical Rehabilitative Tissue Engineering Research. 2007;11(39):7910–7913. [Google Scholar]
- 34.Xiao C.-M., Zhuang Y.-C. Effect of health baduanjin qigong for mild to moderate parkinson’s disease. Geriatrics & Gerontology International. 2016;16(8):911–919. doi: 10.1111/ggi.12571. [DOI] [PubMed] [Google Scholar]
- 35.Chen D.-M., Yu W.-C., Hung H.-F., Tsai J.-C., Wu H.-Y., Chiou A.-F. The effects of Baduanjin exercise on fatigue and quality of life in patients with heart failure: a randomized controlled trial. European Journal of Cardiovascular Nursing. 2018;17(5):456–466. doi: 10.1177/1474515117744770. [DOI] [PubMed] [Google Scholar]
- 36.Chen H.-H., Yeh M.-L., Lee F.-Y. The effects of baduanjin qigong in the prevention of bone loss for middle-aged women. The American Journal of Chinese Medicine. 2006;34(5):741–747. doi: 10.1142/s0192415x06004259. [DOI] [PubMed] [Google Scholar]
- 37.Chen M.-C., Liu H.-E., Huang H.-Y., Chiou A.-F. The effect of a simple traditional exercise programme (baduanjin exercise) on sleep quality of older adults: a randomized controlled trial. International Journal of Nursing Studies. 2012;49(3):265–273. doi: 10.1016/j.ijnurstu.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 38.Chen M.-D., Yeh Y.-C., Tsai Y.-J., Chang Y.-C., Yu J.-W., Hsu C.-H. Efficacy of baduanjin exercise and feasibility of mobile text reminders on follow-up participation in people with severe mental illness. Journal of Psychiatric Practice. 2016;22(3):241–249. doi: 10.1097/pra.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 39.Hsu M.-C., Wang T.-S., Liu Y.-P., Liu C.-F. Effects of baduanjin exercise on oxidative stress and antioxidant status and improving quality of life among middle-aged women. The American Journal of Chinese Medicine. 2008;36(5):815–826. doi: 10.1142/s0192415x08006260. [DOI] [PubMed] [Google Scholar]
- 40.Chen M. G., Liang X., Kong L., et al. Effect of baduanjin sequential therapy on the quality of life and cardiac function in patients with AMI after PCI: a randomized controlled trial. Evidence-Based Complementary and Alternative Medicine. 2020;2020:10. doi: 10.1155/2020/8171549.8171549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fan B., Song W., Zhang J., et al. The efficacy of mind-body (baduanjin) exercise on self-reported sleep quality and quality of life in elderly subjects with sleep disturbances: a randomized controlled trial. Sleep and Breathing. 2020;24(2) doi: 10.1007/s11325-019-01999-w. [DOI] [PubMed] [Google Scholar]
- 42.Liang Y. H., Liao S. Q., Han C. L., Wang H., Peng Y. Effect of the Baduanjin intervention on blood pressure and fat of essential hypertensive patients. Henan Traditional Chinese Medicine. 2014;34(12) [Google Scholar]
- 43.Mao S., Zhang X., Chen M., et al. Beneficial effects of baduanjin exercise on left ventricular remodelling in patients after Acute myocardial infarction: an exploratory clinical trial and proteomic analysis. Cardiovascular Drugs and Therapy. 2020;35 doi: 10.1007/s10557-020-07047-0. [DOI] [PubMed] [Google Scholar]
- 44.Chan J. S., Ho R. T., Chung K. F., et al. Qigong exercise alleviates fatigue, anxiety, and depressive symptoms, improves sleep quality, and shortens sleep latency in persons with chronic fatigue syndrome-like illness. Evidence-Based Complementary and Alternative Medicine. 2014;2014:10. doi: 10.1155/2014/106048.106048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chan J. S. M., Li A., Ng S.-M., et al. Adiponectin potentially contributes to the antidepressive effects of baduanjin qigong exercise in women with chronic fatigue syndrome-like illness. Cell Transplantation. 2017;26(3):493–501. doi: 10.3727/096368916x694238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cheung D. S. T., Deng W., Tsao S. W., et al. Effect of a qigong intervention on telomerase activity and mental health in Chinese women survivors of intimate partner violence: a randomized clinical trial. JAMA Network Open. 2019;2(1) doi: 10.1001/jamanetworkopen.2018.6967.e186967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.An B., Dai K., Zhu Z., et al. Baduanjin alleviates the symptoms of knee osteoarthritis. The Journal of Alternative and Complementary Medicine. 2008;14(2):167–174. doi: 10.1089/acm.2007.0600. [DOI] [PubMed] [Google Scholar]
- 48.An B.-C., Wang Y., Jiang X., et al. Effects of Baduanjin (八段锦) exercise on knee osteoarthritis: a one-year study. Chinese Journal of Integrative Medicine. 2013;19(2):p. 143. doi: 10.1007/s11655-012-1211-y. [DOI] [PubMed] [Google Scholar]
- 49.Jing L., Jin Y., Zhang X., Wang F., Song Y., Xing F. The effect of baduanjin qigong combined with CBT on physical fitness and psychological health of elderly housebound. Medicine. 2018;97(51) doi: 10.1097/md.0000000000013654.e13654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xiao X., Wang J., Gu Y., Cai Y., Ma L. Effect of community based practice of baduanjin on self-efficacy of adults with cardiovascular diseases. PLoS One. 2018;13(7) doi: 10.1371/journal.pone.0200246.e0200246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lu Y., Qu H.-Q., Chen F.-Y., et al. Effect of baduanjin qigong exercise on cancer-related fatigue in patients with colorectal cancer undergoing chemotherapy: a randomized controlled trial. Oncology Research and Treatment. 2019;42(9):431–439. doi: 10.1159/000501127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Xie Y., Guo F., Lu Y., et al. A 12-week baduanjin qigong exercise improves symptoms of ankylosing spondylitis: a randomized controlled trial. Complementary Therapies in Clinical Practice. 2019;36:113–119. doi: 10.1016/j.ctcp.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 53.Chen Y. F., Liu S. R., Li R., et al. Effect of health qigong baduanjin on the pulmonary function of patients with chronic obstructive pulmonary disease in stable period. Chinese Medicine Modern Distance Education of China. 2015;13(17):16–18. [Google Scholar]
- 54.Li M., Fang J., Gao Y., et al. Baduanjin mind-body exercise improves logical memory in long-term hospitalized patients with schizophrenia: a randomized controlled trial. Asian Journal of Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102046.102046 [DOI] [PubMed] [Google Scholar]
- 55.Li R., Jin L., Hong P., et al. The effect of baduanjin on promoting the physical fitness and health of adults. Evidence-Based Complementary and Alternative Medicine. 2014;2014:8. doi: 10.1155/2014/784059.784059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu T., Bai S., Zhang R. C. Effects of health qigong baduanjin on diabetes related indexes in middle-aged obese women. Zhongguo Ying Yong Sheng Li Xue Za Zhi. 2018;34(1):19–22. doi: 10.12047/j.cjap.5484.2018.006. [DOI] [PubMed] [Google Scholar]
- 57.Dong D. G., Yu Z., Yu Z. S. Effects of fitness qigong baduanjin on phlegm-dampness hypertension. Zhongguo Ying Yong Sheng Li Xue Za Zhi. 2020;36(2):157–160. doi: 10.12047/j.cjap.5924.2020.035. [DOI] [PubMed] [Google Scholar]
- 58.Zhang H., Zhu M., Song Y., Kong M. Baduanjin exercise improved premenstrual syndrome symptoms in Macau women. Journal of Traditional Chinese Medicine. 2014;34(4):460–464. doi: 10.1016/s0254-6272(15)30047-9. [DOI] [PubMed] [Google Scholar]
- 59.Liu X., Seah J. W. T., Pang B. W. J., et al. A single-arm feasibility study of community-delivered baduanjin (qigong practice of the eight brocades) training for frail older adults. Pilot Feasibility Stud. 2020;6:p. 105. doi: 10.1186/s40814-020-00649-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bao X., Qiu Q. X., Shao Y. J., Quiben M., Liu H. Effect of sitting ba-duan-jin exercises on balance and quality of life among older adults: a preliminary study. Rehabil Nurs. 2020;45(5):p. E17. doi: 10.1097/rnj.0000000000000219. [DOI] [PubMed] [Google Scholar]
- 61.Cramer H., Lauche R., Hohmann C., et al. Randomized-controlled trial comparing yoga and home-based exercise for chronic neck pain. The Clinical Journal of Pain. 2013;29(3):216–223. doi: 10.1097/ajp.0b013e318251026c. [DOI] [PubMed] [Google Scholar]
- 62.Crow E., Jeannot E., Trewhela A. Effectiveness of Iyengar yoga in treating spinal (back and neck) pain: a systematic review. International Journal of Yoga. 2015;8(1):3–14. doi: 10.4103/0973-6131.146046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Song R., Lee E. O., Lam P., Bae S. C. Effects of tai chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: a randomized clinical trial. The Journal of Rheumatology. 2003;30(9):2039–2044. [PubMed] [Google Scholar]
- 64.Taylor D., Hale L., Schluter P., et al. Effectiveness of tai chi as a community-based falls prevention intervention: a randomized controlled trial. Journal of the American Geriatrics Society. 2012;60(5):841–848. doi: 10.1111/j.1532-5415.2012.03928.x. [DOI] [PubMed] [Google Scholar]
- 65.Wayne P. M., Kiel D. P., Buring J. E., et al. Impact of tai chi exercise on multiple fracture-related risk factors in post-menopausal osteopenic women: a pilot pragmatic, randomized trial. BMC Complementary and Alternative Medicine. 2012;12:p. 7. doi: 10.1186/1472-6882-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.White P., Goldsmith K., Johnson A., et al. Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (pace): a randomised trial. The Lancet. 2011;377(9768):823–836. doi: 10.1016/s0140-6736(11)60096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The supplementary data file includes the comparison list of PRISMA Checklist.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.


