Abstract
A Coronavirus Disease 2019 (COVID-19)–specific Hospital-at-Home was implemented in a 400-bed tertiary hospital in Barcelona, Spain. Senior or immune-compromised physicians oversaw patient care. The alternative to inpatient care more than doubled beds available for hospitalization and decreased the risk of transmission among patients and health care professionals. Mild cases from either the emergency department or after hospital discharge were deemed suitable for admission to the Hospital-at-Home. More than half of all patients had pneumonia. Standardized protocols and management criteria were provided. Only 6% of cases required referral for inpatient hospitalization. These results are promising and may provide valuable insight for centers undertaking Hospital-at-Home initiatives or in the case of new COVID-19 outbreaks.
Keywords: COVID-19, Hospital-at-Home, telemedicine
The Coronavirus Disease 2019 (COVID-19) pandemic posed as an unprecedented challenge for health systems. At its peak, hospitals experienced a shortage of beds, doctors, and supplies. Similarly, senior physicians, whose experience and decision-making skills would prove essential during the health crisis, faced a high risk of developing a COVID-19 infection because of their age.1 Lack of personal protective equipment and overcrowding in hospital facilities further increased their exposure to the virus.2
The cumulative result led to difficulties in providing quality patient care while minimizing the risk of transmission of COVID-19 among patients and health care professionals.
The city of Barcelona recorded its first cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) between February 22 and 29, 2020. Peak incidence occurred 5 weeks later between March 23 and 29, 2020. In the area served by our hospital, peak incidence of new cases per week was 178.5 per 100,000 inhabitants. After 15 weeks, the total number of cases in our area was 3642, with a cumulative incidence of 1146 per 100,000 inhabitants (http://www.aisbcn.cat/wp-content/uploads/2020/06/20200605_QC-EPI.pdf).
Given that COVID-19 infections would create a burden on our center, especially with respect to risk of transmission and availability of hospital beds and resources, we established a COVID-19–specific Hospital-at-Home (COVID-HaH). Our center has overseen a Hospital-at-Home program since 2000. It can currently attend 30 patients and has a staff composed of 7 nurses, 3 doctors, 1 clerical worker, and 1 social worker. It has maintained a positive relationship with primary care services. Therefore, to take advantage of their experience and logistical resources, we quickly built a new section called the COVID-HaH. Hospital-at-Home is defined by Bruce Leff3 as a community-based provision of services that is usually associated with acute inpatient care and executed with different models. The main objective of Hospital-at-Home is to prevent patients from being exposed to adverse events, such as nosocomial infections, associated with inpatient hospital care.4 Essentially, patients admitted to Hospital-at-Home are those who received traditional acute hospital care and will complete intravenous infusions or orthopedic programs with multidisciplinary interventions, as well as patients with conditions such as infections, heart failure, chronic obstructive pulmonary disease, and stroke.
In the past few years, implementation of Hospital-at-Home has risen in frequency after reductions in mortality and complications and, conversely, increases in patient satisfaction and cost-efficiency were demonstrated.5 , 6 Several Hospital-at-Home models have been carried out, from exclusive support for conventional hospitalization to reduce length of stay, to direct care of emergency room patients to prevent a collapse in the system. However, admission criteria are restricted to patients with specific conditions. Patients eligible include all those who reside in specified geographic reference areas; live with family members, caretakers, or in a nursing home; and who (or whose family member) provides consent for their admission and medication administration at home.3 The most important reasons that Hospital-at-Home has been implemented progressively within the past 20 years have been that it has demonstrated to be a great tool for reductions in emergency department visits, hospitalizations, and costs.7 The challenge that Hospital-at-Home faces is how to adapt to new situations or diseases and integrate technological or medical advances effectively for optimal patient care.8
Here we report the deployment and methodology of a Hospital-at-Home initiative during a public health emergency and highlight its importance as a complementary structure to such a crisis.
Methods
Our hospital is a 400-bed tertiary center in Barcelona, Spain. The COVID-HaH was implemented on March 16, 2020. The Internal Medicine Department established the initiative and oversaw all decisions pertaining to its execution. Recently retired senior physicians and all other physicians who were either immunosuppressed or undergoing immunosuppressive therapy and presented with an increased risk of infection were asked to volunteer. Participating physicians then worked remotely from home with access to the hospital's electronic health records. A standardized questionnaire for follow-up, as well as a common protocol, including criteria of clinical alarms, were provided to doctors.
Patients with COVID-19 infection who visited the emergency department were classified as mild, intermediate or severe according to clinical, respiratory and radiological criteria (Table 1 ). Mild cases were discharged for follow-up by family physicians. When isolation at home was not a viable option, those patients with mild infection were referred to a medicalized hotel. Patients with severe infection were hospitalized. Patients with intermediate infection were considered eligible for admission to the COVID-HaH when the following criteria (Table 2 ) were met: (1) not severely ill; (2) no respiratory insufficiency (basal SaO2 >94% or > 90% after exercise); (3) hemodynamic stability; and (4) adequate housing conditions that could allow for home isolation. Similarly, patients discharged from the hospital were candidates for COVID-HaH admission.
Table 1.
Criteria for Classifying COVID-19 Severity at the Emergency Department
| Mild |
| Covid-19 symptoms without pneumonia |
| Mild pneumonia confirmed by x-ray or CT scan CURB-65 <1 |
| Oxygen saturation >90% |
| Intermediate |
| Respiratory rate <30 |
| MEWS score <3 |
| With chronic diseases, eg, COPD, CKD, obesity, diabetes, age >65 years |
| Severe |
| Pneumonia confirmed by x-ray or CT scan CURB-65 >2 |
| Oxygen saturation <90% |
| Respiratory rate >30 per minute |
| MEWS score 3–4 |
CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; CT, computed tomography; disease severity scoring CURB-65, the combination of Confusion, Urea, Respiratory rate, Blood pressure, and Age ≥65; MEWS, Modified Early Warning Score consists of 5 physiological parameters, which include systolic blood pressure, pulse rate, respiratory rate, temperature, and level of consciousness.
Table 2.
Standard Criteria for Patients in the COVID-HaH
| Admission to the HaH |
| Age ≤75 years |
| Chronic disease stability, if exists |
| Not severely ill |
| Temperature <38.5°C |
| No hemoptysis |
| No diarrhea |
| No chest pain |
| Basal saturation O2 >94% |
| Saturation O2 post exercise >90%∗ |
| Hemodynamic stability, systolic blood pressure >110 mm Hg |
| Adequate housing conditions that could allow for home isolation, few co-inhabitants, possibility of single room, good air circulation, non-vulnerable persons living at home |
| Referral from the COVID-HaH back to the hospital |
| Dyspnea† |
| Persistent fever >38.5°C |
| Severe vomiting or diarrhea |
| Other complications (cardiovascular, metabolic)‡ |
Walking 4 m back and forth.
Dyspnea at minimal exercise or worsening.
Based on clinical criteria.
On admission, all patients were provided with written information on isolation and hygiene etiquette and practice, as well as emergency numbers to contact nurse and doctor coordinators (Table 3 ). Moreover, a verbal informed consent was obtained from patient or their families for the admission. Depending on patients' conditions, calls were made either once or twice a day to monitor clinical course. Twice a day, by telephone, patients were asked about temperature, muscular pain, headaches, diarrhea, and vomiting, as well as respiratory difficulty. A pulse oximeter was provided to patients with dyspnea, and saturation values were collected based on patient reporting. In cases in which physicians considered an in-person visit necessary, nurses and doctors were provided with personal protection equipment at that time to perform such visits. In cases of clinical worsening, a fast-track system for transferring patients to the hospital was created (Table 2). Samples for laboratory tests were obtained at the patients' home when necessary. In addition, drugs were delivered to patients’ homes when obtaining medication from the pharmacy was not possible. Consultations with specialists were held virtually. Team members maintained constant communication via WhatsApp, e-mails, and telephone.
Table 3.
Instructions on Isolation and Hygiene Practice Provided to Hospital-at-Home Patients With COVID-19
| Single room for isolation, keep door closed at all times |
| Maintain at least 2 m of distance with co-inhabitants |
| Wash hands with soap or an alcoholic solution before leaving the room |
| Wear a mask outside of the room |
| Good air circulation in the isolation room and all other shared spaces |
| Wash the bathroom with bleach frequently |
| Individual tools for cleanliness |
| Individual bin with plastic bag fastener |
| Discard gloves and mask in individual bin |
| Wash clothes between 60° and 90°; do not shake clothing before placing it into the washing machine |
| Wash dishes and utensils with soap and hot water |
| Wash hands before handling food and after touching trash |
| Clean surfaces frequently (nightstand, bed, room furniture, and bathroom) with a solution of 10 mL bleach/1000 mL water |
| 14 days of isolation |
Results
A total of 24 physicians comprised the COVID-HaH staff. Specialties of these physicians were as follows: internal medicine, anesthesia, gastroenterology, emergency care, pediatrics, rheumatology, epidemiology and pharmacy. None of these individuals developed a SARS-CoV-2 infection while serving in the Hospital-at-Home.
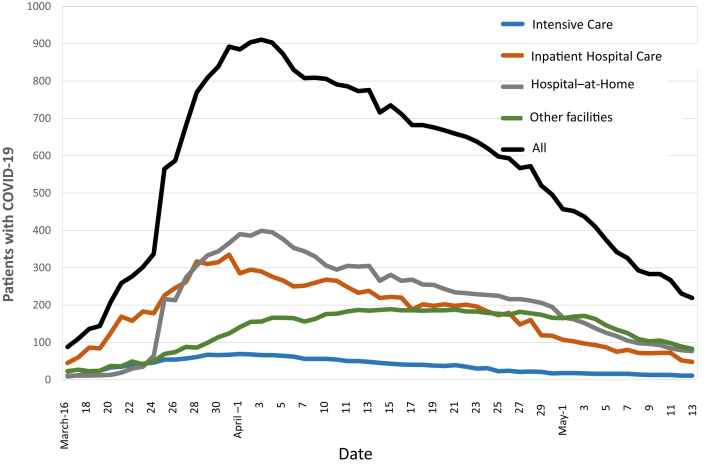
Overall, 917 patients (526 women and 391 men) were admitted to the COVID-HaH between March 16 and May 13, 2020 (Figure 1 ). Of those, 687 were referred from the emergency department and 230 after hospital discharge. The maximum number of simultaneous cases was 424 on April 5. The average length of stay was 13.4 (8.4) days. Pneumonia was diagnosed in 474 (51.7%) patients.
Fig. 1.
Number of patients with COVID-19 infection admitted to the hospital between March 13 and May 13, 2020. Other facilities include a rehabilitation center, geriatrics center, and a medicalized hotel.
Of all patients admitted to the COVID-HaH, 57 (6.2%) were referred back to the emergency department due to clinical worsening; 10 of those patients were re-admitted to conventional wards. Only 1 patient died while in the COVID-HaH: a 75-year-old woman who had presented with pneumonia experienced sudden death. Patients were monitored until no major symptoms, such as fever or dyspnea, were present and always within at least 14 days of symptom onset. Patients were recommended to respect quarantine and referred thereafter to their primary care physician with a discharge report.
Furthermore, between March 16 and May 13, 2020, a total of 12,297 bed-days were added to hospital capacity. During demand peak, the 424 patients admitted to the COVID-HaH accounted for 56.6% of all beds designated for patients with COVID-19 in our center.
In addition, 634 patients were admitted to inpatient hospital care (IHC) with moderate or severe pneumonia (Table 4). These patients were older than those in HaH and prevalence of at least 1 comorbidity being present was 48.5%. Hypertension was the most frequent comorbidity (49%), followed by chronic kidney disease (41%) and diabetes (18%).
Table 4.
Clinical Characteristics and Outcomes of Patients in HaH and Patients in IHC
| HaH n = 917 | IHC n = 634 | P | |
|---|---|---|---|
| Mean age (SD) | 46.2 (14.3) | 64.5 (17.6) | <.001 |
| Female sex (%) | 526 (57.3) | 353 (55.6) | .634 |
| Pneumonia (%) | 474 (51.6) | 634 (100) | <.001 |
| Length of stay (SD) all | 13.4 (8.4) | 12.4 (11.9) | .504 |
| Length of stay (SD) pneumonia | 10.2 (5.6) | 12.4 (11.9) | <.001 |
| ICU admission (%) | 0 (0) | 100 (15) | <.001 |
| Death (%) | 1 (0.1) | 88 (13) | <.001 |
ICU, intensive care unit.
Discussion
A COVID-specific Hospital-at-Home expanded the total bed capacity in our hospital by up to 106%, ratifying it as a formidable solution to overloaded health systems during the COVID-19 pandemic.9 , 10 In our experience, this specific structure has proffered several advantages: (1) to alleviate burdens placed on hospital structure through the avoidance of admissions to conventional or expanded wards located on hospital premises; (2) to continue the essential work and contributions of senior or immunologically compromised clinicians without risk exposure to COVID-19 infection; (3) to provide flexibility with regard to the number of patients admitted to the COVID-HaH; (4) to prevent a concentration of patients in an already overcrowded hospital and decrease the risk of transmission among health personnel and patients11; and (5) to facilitate the availability of beds in the emergency department, which often faces a critical bottleneck. Finally, it is important to highlight that due to the use of tools like the telephone and Internet in telemedicine, implementation of this Hospital-at-Home initiative incurred minimal costs.
The COVID- HaH is, in fact, an adaptation of home health care due to challenges posed by an unprecedented pandemic. Patients admitted to COVID-HaH were clearly less severe than inpatients in hospital wards, as admission criteria were different. The main objectives of COVID-HaH were to manage the overwhelming wave of patients visiting the emergency department, select the appropriated cases, and facilitate hospital discharge. At that time, inpatient hospital bed capacity was limited, even though there were 4.8 times more intensive care beds and 11 times more beds in the infectious disease department. That stated, patients with pneumonia in COVID-HaH were younger and presented with milder clinical cases.
In addition, it would prove relevant for monitoring patients at home in case of acute changes in clinical conditions and the need for immediate transfers to the hospital. For example, acute respiratory distress syndrome (ARDS) is a common immunopathological event arising in SARS-CoV-2, SARS-CoV, and Middle East Respiratory Syndrome (MERS)-CoV infections.12 ARDS is a consequence of the cytokine storm that often occurs between day 5 and 13 after illness onset.13, 14, 15 It is crucial to know both the time and symptoms (persistent fever, cough, and dyspnea) so physicians can become aware of a possible unfavorable evolution of the disease.16 Some authors have published that age >70 years and chronic disease instability, among other factors, were prognostic factors related to poor prognosis and death in patients admitted to the hospital.17 In our center, the overall mortality reported for patients with COVID-19 was lower than other Spanish centers.18, 19, 20 However, mortality was higher in the group >75 years, increasing to 28.3% in patients aged between 80 and 89 years and to 40% in patients aged 90 years or older.21 The prevalence of at least 1 comorbidity as hypertension, chronic kidney disease, or diabetes was associated with worse prognosis and essentially when these comorbidities were not well controlled or stable.21 In defining inclusion criteria for COVID-HaH admission, age <75 years and chronic disease stability were 2 important aspects to have, so as to minimize the likelihood of patients returning to the emergency room and relieve pressure being placed on IHC.
Similar experience has been published in Australia; however, investigators described fewer patients and inclusion criteria varied.22 Results, in comparison with those reported by our COVID-HaH experience, were worse: 7 of 23 patients required a visit to the hospital, and a 91-year-old patient died after returning to the hospital. Reasons for these results include (1) patients aged >70 years were eligible for admission, and (2) comorbidities were present in 73.9% of patients. However, it is important to add that in our COVID-HaH experience, a woman who met the age criteria limit did die during care. That all stated, data provided by those investigators and our experience support the decision to define inclusion criteria for their admission (eg, patients aged <75 years, as such).
Last, when reflecting on our COVID-HaH experience, the participation of retired senior physicians and other experienced physicians was important. At that time, little was known about COVID-19; however, physicians’ skillsets were adequate enough to learn quickly from the abundant literature published during those days and identify alarm signals in patients via telemedicine tools.23 In this study, there are, however, limitations and potential caveats. There were no direct observations of patients; the involvement of highly experienced senior clinicians aimed to assuage this concern. Pictures taken of only dermatological conditions allowed for teleconsultations with a dermatologist. Notwithstanding, in all other cases of necessary laboratory or imaging tests, or during clinical deterioration, patients were referred back to the hospital. This occurrence was observed in only 6% of all patients, and the established fast-track system streamlined responses in such cases. In addition, proper adherence to home isolation required careful advice and follow-up. Finally, this is a single-center experience and the model at hand may need to be adjusted to meet the specific demands and needs of varying locations and health systems.
Implications for Practice, Policy, and/or Research
A COVID-19–specific Hospital-at-Home can prove valuable and cost-efficient, should further SARS-CoV-2 outbreaks occur or other highly transmittable infectious disease epidemics arise. It is a good opportunity to record data from specific patients and analyze post–COVID-19 clinical manifestations.
Acknowledgments
We thank all 24 nurses, senior physicians and other doctors who volunteered their time in the COVID-19-specific Hospital-at-Home.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Buerhaus P.I., Auerbach D.I., Staiger D.O. Older clinicians and the surge in novel Coronavirus Disease 2019 (COVID-19) JAMA. 2020;323:1777–1778. doi: 10.1001/jama.2020.4978. [DOI] [PubMed] [Google Scholar]
- 2.Rosenbaum L. Facing Covid-19 in Italy — ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020;382:1873–1875. doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 3.Leff B. Defining and disseminating the hospital-at-home model. CMAJ. 2009;180:156–157. doi: 10.1503/cmaj.081891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caplan G.A., Brown A., Crowe P.J. Reengineering the elective surgical service of a tertiary hospital:a historical controlled trial. Med J Aust. 1998;169:247–251. [PubMed] [Google Scholar]
- 5.Mas M.À., Santaeugènia S.J., Tarazona-Santabalbina F.J. Effectiveness of a hospital-at-home integrated care program as alternative resource for medical crises care in older adults with complex chronic conditions. J Am Med Dir Assoc. 2018;19:860–863. doi: 10.1016/j.jamda.2018.06.013. [DOI] [PubMed] [Google Scholar]
- 6.Shepperd S., Doll H., Angus R.M. Avoiding hospital admission through provision of hospital care at home: A systematic review and meta-analysis of individual patient data. CMAJ. 2009;180:175–182. doi: 10.1503/cmaj.081491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stall N., Nowaczynski M., Sinha S.K. Systematic review of outcomes from home-based primary care programs for homebound older adults. J Am Geriatr Soc. 2014;62:2243–2251. doi: 10.1111/jgs.13088. [DOI] [PubMed] [Google Scholar]
- 8.Siu A.L., Zimbroff R.M., Federman A.D. The effect of adapting Hospital at Home to facilitate implementation and sustainment on program drift or voltage drop. BMC Health Serv Res. 2019;19:264. doi: 10.1186/s12913-019-4063-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arias-de la Torre J., Alonso J., Martín V., Valderas J.M. Hospital-at-home as an alternative to release the overload of healthcare systems during the severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) pandemic. J Am Med Dir Assoc. 2020;21:990–991. doi: 10.1016/j.jamda.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hick J.L., Biddinger P.D. Novel coronavirus and old lessons —preparing the health system for the pandemic. N Engl J Med. 2020;382:e55. doi: 10.1056/NEJMp2005118. [DOI] [PubMed] [Google Scholar]
- 11.Dzau V.J., Kirch N.T. Preventing a parallel pandemic — a national strategy to protect clinicians’ well-being. N Engl J Med. 2020;383:513–515. doi: 10.1056/NEJMp2011027. [DOI] [PubMed] [Google Scholar]
- 12.Peiris J.S., Guan Y., Yuen K.Y. Severe acute respiratory syndrome. Nat Med. 2004;10:S88–S97. doi: 10.1038/nm1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang L., Liu S., Liu J. COVID-19: Immunopathogenesis and immunotherapeutics. Signal Transduct Target Ther. 2020;5:128. doi: 10.1038/s41392-020-00243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sinha P., Matthay M.A., Calfee C.S. Is a “cytokine storm” relevant to COVID-19? JAMA Intern Med. 2020;180:1152–1154. doi: 10.1001/jamainternmed.2020.3313. [DOI] [PubMed] [Google Scholar]
- 16.Borges do Nascimento I.J., von Groote T.C., O'Mathúna D.P. International Task Force Network of Coronavirus Disease 2019 (InterNetCOVID-19). Clinical, laboratory and radiological characteristics and outcomes of novel coronavirus (SARS-CoV-2) infection in humans: A systematic review and series of meta-analyses. PLoS One. 2020;15:e0239235. doi: 10.1371/journal.pone.0239235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maguire D., Woods M., Richards C. Prognostic factors in patients admitted to an urban teaching hospital with COVID-19 infection. J Transl Med. 2020;18:354. doi: 10.1186/s12967-020-02524-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mostaza J.M., García-Iglesias F., González-Alegre T. Clinical course and prognostic factors of COVID-19 infection in an elderly hospitalized population. Arch Gerontol Geriatr. 2020;91:104204. doi: 10.1016/j.archger.2020.104204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Casas-Rojo J.M., Antón-Santos J.M., Millán-Núñez-Cortés J. Grupo SEMI-COVID-19 Network. Clinical characteristics of patients hospitalized with COVID-19 in Spain: Results from the SEMI-COVID-19 Registry. Rev Clin Esp. 2020;220:480–494. doi: 10.1016/j.rce.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iftimie S., López-Azcona A.F., Vicente-Miralles M. Risk factors associated with mortality in hospitalized patients with SARS-CoV-2 infection. A prospective, longitudinal, unicenter study in Reus, Spain. PLoS One. 2020;15:e0234452. doi: 10.1371/journal.pone.0234452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Posso M., Comas M., Román M. Comorbidities and mortality in patients with COVID-19 aged 60 years and older in a university hospital in Spain. Arch Bronconeumol. 2020;56:756–758. doi: 10.1016/j.arbr.2020.06.010. [DOI] [PubMed] [Google Scholar]
- 22.Lwin N., Burgess J., Johnston C. Hospital-in-the-home experience of first 23 COVID-19 patients at a regional NSW hospital. Intern Med J. 2020;50:1271–1273. doi: 10.1111/imj.15016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bos L.D.J., Brodie D., Calfee C.S. Severe COVID-19 infections-knowledge gained and remaining questions. JAMA Intern Med. 2021;181:9–11. doi: 10.1001/jamainternmed.2020.6047. [DOI] [PubMed] [Google Scholar]