Abstract
Diabetes and hyperglycemia occurring during COVID-19 era have implications for COVID-19 related morbidity/mortality. In this brief review, we have attempted to categorise and classify such heterogenous hyperglycemic states. During COVID-19 pandemic broadly two types of hyperglycemia were seen: one in patients without COVID-19 infection and second in patients with COVID-19 infection. Patients not inflicted with COVID-19 infection and diagnosed with either type 2 diabetes mellitus (T2DM) or type 1 diabetes mellitus (T1DM) show more severe hyperglycemia and more ketoacidosis, respectively. In former, it could be attributed to weight gain, decreased exercise, stress and in both type of diabetes, due to delayed diagnosis during lockdown and pandemic. In patients with COVID-19 and associated pneumonia, altered glucose metabolism leading to hyperglycemia could be due to corticosteroids, cytokine storm, damage to pancreatic beta cells, or combination of these factors. Some of these patients present with diabetic ketoacidosis, hyperglycemic hyperosmolar state or both. We have provided a framework for categorisation of hyperglycemic states, which could be consolidated/revised in future based on new research data.
Keywords: COVID-19, Diabetes, Diabetic ketoacidosis, Stress, Weight gain
Hyperglycemia has emerged as one of the risk factors for adverse outcomes and mortality of SARS-CoV-2 virus infection (COVID-19) [[1], [2], [3]]. Further, bidirectional relationship of hyperglycemia and COVID-19 has been well recognised [4]. It must be realised that any magnitude of hyperglycemia is associated with poor prognosis in COVID-19 [3,5,6]. However, the timing and extent of hyperglycemia varies according to several factors: pre-existing diabetes or pre-diabetes [1,2], age (5), presence of obesity [7], other co-morbidities and stress [8], severity of infection, type of treatment given, and beta cells capacity during times of COVID-19 infection. Many of these factors have been researched, while knowledge regarding others is limited. During the times of COVID-19, knowledge of presentation of hyperglycemia and its relationship with morbidity and mortality has increased [9]. Indeed, varied presentations of hyperglycemia have been reported. A synthesis of this knowledge and categorisation of types of hyperglycemia has not been done so far. Aim of this short review is to propose classification of various categories of hyperglycemia during times of COVID-19.
A literature search was performed with Medline (PubMed), Scopus, and Google Scholar electronic databases till January 2021, using relevant keywords; COVID-19 induced diabetes; COVID-19 and type 1 diabetes; COVID-19 and type 2 diabetes; COVID-19 induced diabetic ketoacidosis; new-onset diabetes after SARS-CoV-2 infection, to extract relevant studies describing relationship between COVID-19 and hyperglycemia.
Upon literature review and according to recently published data till now, we propose the following classification of hyperglycemia taking recourse to current literature. We hope that an enhanced understanding of hyperglycemia would be attained with this proposed classification.
1. Proposed categories of hyperglycemia during times of COVID-19
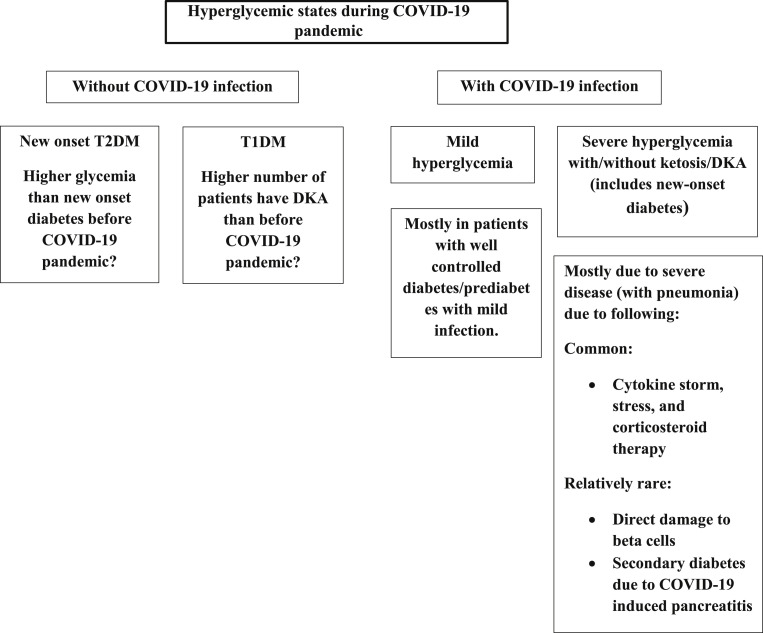
Fig. 1 lists a simplified classification. Discussion and further details have been provided below.
-
1.
Mild Hyperglycemia:
Fig. 1.
Proposed classification of hyperglycemic states during COVID-19 pandemic.
Mild hyperglycemia could be seen in following category of patients;
-
a.
Patients of T2DM with previously controlled glycemia. Subsequent to mild COVID-19 infection these patients may have minimal changes in their glycemic status. Upon mild COVID-19 infection, these patients can be managed at home. Mostly these patients are continued on their previous diabetes treatment.
-
b.
Patients with pre-existing prediabetes: Upon mild COVID-19 infection, these patients either remain in prediabetes category or covert to diabetes. Most of these can be managed with oral anti-hyperglycemic drugs.
-
c.
Patients with mild hyperglycemia detected for the first time at admission for COVID -19 infections. This category of patients have been researched. A retrospective analysis was done on 605 patients without known diabetes in two hospitals based in Wuhan, China. These authors showed that the odds ratio for 28-day in-hospital complications in those with fasting blood glucose >/ = 7.0 mmol/l and 6.1–6.9 mmol/l vs. <6.1 mmol/l was 3.99 (95% CI 2.71, 5.88) and 2.61 (95% CI 1.64, 4.41), respectively [10]. Such mild hyperglycemia without previous history of diabetes could also occur during home quarantine with mild COVID-19 infections, however, it is detected only in those who have glucose meter at home or upon subsequent visit to laboratory [11].
-
2.Severe hyperglycemia with or without ketosis/ketoacidosis with COVID-19 or during COVID-19 era:
-
A.Severe hyperglycemia without ketosis/ketoacidosis in patient with T2DM:
- a.
-
b.Patients with T2DM/prediabetes having moderate-severe COVID-19 infection requiring hospitalization:
- Patients with T2DM/prediabetes who receive corticosteroids for COVID-19 infection experience acute rise in blood glucose levels, which are difficult to control and need high doses of insulin. Even without steroids, infection and stress may increase blood glucose levels.
-
c.Patients with no prior history of diabetes or pre-diabetes presenting with new-onset diabetes:
-
i.With COVID-19 Infection: Mostly these patients have severe COVID-19 infection with pneumonia, cytokine storm and most are treated with corticosteroids [3,4,16]. Some patients acutely present with ketoacidosis suggesting acute insulinopenia, as described later (refer point c). In addition, we have also described patients with new-onset diabetes who are COVID-19 antibody positive but were asymptomatic [11]. In such cases relationship of hyperglycemia with asymptomatic COVID-19 antibody positivity remains unclear.
-
ii.Patients without COVID-19 Infection:
-
1.Type 2DM: These patients develop hyperglycemia due to altered lifestyle during COVID19 era; change in food habits, decrease in exercise, weight gain [17,18], and excessive stress [11,18]. We have recently reported that glycemic parameters (fasting blood glucose, post prandial blood glucose, and glycosylated hemoglobin levels) in patients with new-onset diabetes during COVID-19 era were far more adverse than patients with new onset diabetes before COVID-19 era(11). It is possible that patients with new-onset diabetes during COVID-19 era delayed their visit to physician or for blood testing, causing delay in diagnosis and consequent inordinate rise of blood glucose levels. Such data have only been reported from India and should be researched in other countries.
-
2.Type 1DM: Interestingly, presentation of patients of T1DM appears apperas to have changed during COVID-19 era. Data from several pediatric care centres in Italy showed that, as compared with 2019, there was a 23% reduction in new diabetes cases in 2020 (n,160; only 8 patients SARS-CoV-2 RT-PCR positive). Further, the authors show that among those newly diagnosed patients who presented in a state of DKA, the proportion with severe DKA was 44.3% in 2020 vs. 36.1% in 2019 (p = 0.03) [19]. Similarly, data from Australia shows that the number of new diagnoses of type 1 diabetes was comparable in the pandemic period and pre-pandemic periods, but the frequency of severe diabetic ketoacidosis was significantly higher in the pandemic period as compared to the pre-pandemic periods (45% vs 5%; P < 0.003), odds ratio 16.7 (95% CI 2.0, 194.7) [20].
-
1.
-
i.
-
B.Severe hyperglycemia with ketosis/ketoacidosis with/without hyperglycemic hyperosmolar state (HHS) in patients with T2DM (includes new-onset diabetes):
- This type of presentation has been reported by many authors [3,[21], [22], [23], [24], [25], [26]] [27] but its prevalence and features remain poorly researched. A retrospective cohort of 35 patients with COVID-19 (T2DM; 28, T1DM; 5, new presentation; 2), presenting with DKA (31·4%), mixed DKA and HHS (37·1%), HHS (5·7%), or hyperglycaemic ketosis (25·7%) were evaluated in a study reported from UK [21]. According to authors, acute insulinopenia in patients with COVID-19 and with type 2 diabetes, which persisted up until the time of discharge in 30% of patients previously not insulin-treated, was an uncommonly described feature. Further, in a study of 658 hospitalised patients from China, 42 (6.4%, one had T1DM) developed ketosis/ketoacidosis. Interestingly, 27/42 patients had non-diabetic ketoacidosis [22]. A series of 3 cases who developed severe COVID-19 infection with acute onset diabetes, DKA and marked increase in cytokines [23,24] has been described from India. These patients responded well to treatment including intravenous fluids and insulin. The requirement of insulin gradually diminished after about 4–6 weeks of diagnosis and then hyperglycemia was controlled with oral anti-hyperglycemic drugs alone [23,24]. Another, albeit rarer variety of patients are those who present with new-onset marked hyperglycemia with ketonuria after very mild COVID-19 infection [25,26]. Such a patient, recently reported by us was managed on small doses of oral anti-hyperglycemic treatment [25]. Euglycemic ketoacidosis, due to Sodium- glucose Cotransporter-2 inhibitor drugs should also be considered in patients presenting with ketoacidosis.
“Diabetogenic effects’ of COVID-19 infection have been debated but remain sparsely researched. Apart from ‘stress’, direct and possibly destructive effects of cytokine storm or SARS-CoV-19 virus itself (likely via attachment using ACE-2 receptors) on pancreatic beta cells have been speculated(4, 9). Nature (Type1, Type 2, or mixed) of diabetes in such patients and its course remains unclear. -
C.Patients of type 1 diabetes with COVID-19 infection presenting with diabetic ketoacidosis, or new onset T1DM. A multicentre study from the UK showed an apparent increase in new-onset T1DM in children, with evidence of SARS-CoV-2 infection or exposure in some of these. Seventy per cent (21/30) children presented with DKA and 52% (11/21) had severe DKA. Of the five children with positive results (2 of 21 tested were SARS-CoV-2 PCR positive and 3 of 16 tested were SARS-CoV-2 IgG positive), three presented with severe DKA and refractory hypokalaemia, and one PCR positive child suffered a hypokalaemia-related cardiac arrest but recovered fully [28]. The series of patients presenting with DKA, described previously in UK based cohort (see point 2 (B)), comprised of a mixture of patients with T1DM and T2DM [22]. New onset diabetes with DKA has also been described in a child who was having COVID-19 antibody positive with multisystem inflammatory syndrome [29]. The natural history of such patients with T1DM remains unclear and required further follow up research.
-
A.
-
3.Other Categories:
-
a.Hyperglycemia with pancreatitis after COVID-19 infection. Hyperglycemia following pancreatitis associated with COVID-19 infection (presumably due to direct effect of SARS-CoV-19 virus on pancreatic beta cells) has been described [30]. Pancreatitis after COVID-19 infection in an established case of diabetes has been described by us previously [31]. Overall, prevalence and natural course of such ‘secondary diabetes’ remains unknown.
-
b.Gestational diabetes with/without COVID-19 infection: This issue has been less researched. As shown for patients with type 2 diabetes, lockdown during COVID-19 could lead to worsening of glycemia [32]. In a meta-analysis 128176 non-pregnant patients (228 studies) and 10000 pregnant patients (121 studies) with confirmed COVID-19 were included. The most common complication in pregnant patients with COVID-19, as compared to general population was diabetes [33]. Euglycemic ketoacidosis in a case of GDM and COVID-19 has been reported [34]. Clearly, more research is needed.
-
a.
2. Conclusions
There is considerable heterogeneity in the effect of COVID-19 on alteration of glucose metabolism, ranging from mild or no effect to severe hyperglycemia and ketoacidosis. These effects are because of the cytokine storm, steroids used in treatment and possibly the direct beta cell injury by virus. In addition, the psycho-socio-economic effects of the pandemic have resulted in altered glucose metabolism manifesting as worsening of glycemic control in people with pre-existing diabetes and in new onset diabetes. Importantly, association of altered glucose metabolism and severe COVID-19, as shown in many studies, indicate that SARS-CoV-2 infection involves an interplay with glucose metabolism. Exploration of heterogenous pathways by which SARS-CoV-2 dysregulates glucose metabolism is important for understanding proper diagnosis, monitoring and therapy [3].
Recognition of these different clinical categories of hyperglycemia will lead to a better understanding of the effect of COVID-19 in patients with diabetes and will help in formulating appropriate treatment plans. Further research may lead to modification of these proposed categories.
References
- 1.Gupta R., Hussain A., Misra A. Diabetes and COVID-19: evidence, current status and unanswered research questions. Eur J Clin Nutr. 2020 Jun;74(6):864–870. doi: 10.1038/s41430-020-0652-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta R., Misra A. COVID19 in South Asians/Asian Indians: heterogeneity of data and implications for pathophysiology and research. Diabetes Res Clin Pract. 2020 Jun 10;165:108267. doi: 10.1016/j.diabres.2020.108267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith S.M., Boppana A., Traupman J.A., Unson E., Maddock D.A., Chao K. Impaired glucose metabolism in patients with diabetes, prediabetes, and obesity is associated with severe COVID-19. J Med Virol. 2020 Jun 26 doi: 10.1002/jmv.26227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubino F., Amiel S.A., Zimmet P., Alberti G., Bornstein S., Eckel R.H. New-onset diabetes in Covid-19. N Engl J Med. 2020 Jun 12;383(8):789–790. doi: 10.1056/NEJMc2018688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang I., Lim M.A., Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia - a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 2020 Jul - Aug;14(4):395–403. doi: 10.1016/j.dsx.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh A.K., Gupta R., Misra A. Comorbidities in COVID-19: outcomes in hypertensive cohort and controversies with renin angiotensin system blockers. Diabetes Metab Syndr. 2020 Apr 9;14(4):283–287. doi: 10.1016/j.dsx.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jayawardena R., Jeyakumar D.T., Misra A., Hills A.P., Ranasinghe P. Obesity: a potential risk factor for infection and mortality in the current COVID-19 epidemic. Diabetes Metab Syndr. 2020 Nov-Dec;14(6):2199–2203. doi: 10.1016/j.dsx.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scheen A.J., Marre M., Thivolet C. Prognostic factors in patients with diabetes hospitalized for COVID-19: findings from the CORONADO study and other recent reports. Diabetes Metab. 2020 Sep;46(4):265–271. doi: 10.1016/j.diabet.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strict glycemic control is needed in times of COVID19 epidemic in India: a Call for action for all physicians. Diabetes Metab Syndr. 2020 Sep - Oct;14(5):1579–1581. doi: 10.1016/j.dsx.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang S., Ma P., Zhang S., Song S., Wang Z., Ma Y. Fasting blood glucose at admission is an independent predictor for 28-day mortality in patients with COVID-19 without previous diagnosis of diabetes: a multi-centre retrospective study. Diabetologia. 2020 Jul 10;63(10):2102–2111. doi: 10.1007/s00125-020-05209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghosh A., Anjana R.M., Shanthi Rani C.S., Jeba Rani S., Gupta R., Jha A. Glycemic parameters in patients with new-onset diabetes during COVID-19 pandemic are more severe than in patients with new-onset diabetes before the pandemic: NOD COVID India Study. Diabetes Metab Syndr. 2020 Dec 29;15(1):215–220. doi: 10.1016/j.dsx.2020.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karatas S., Yesim T., Beysel S. Impact of lockdown COVID-19 on metabolic control in type 2 diabetes mellitus and healthy people. Prim Care Diabetes. 2021 Jan 9 doi: 10.1016/j.pcd.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruissen M.M., Regeer H., Landstra C.P., Schroijen M., Jazet I., Nijhoff M.F. Increased stress, weight gain and less exercise in relation to glycemic control in people with type 1 and type 2 diabetes during the COVID-19 pandemic. BMJ Open Diabetes Res Care. 2021 Jan;9(1) doi: 10.1136/bmjdrc-2020-002035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ruiz-Roso M.B., Knott-Torcal C., Matilla-Escalante D.C., Garcimartin A., Sampedro-Nunez M.A., Davalos A. COVID-19 lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with type 2 diabetes mellitus. Nutrients. 2020 Aug 4;12(8) doi: 10.3390/nu12082327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Onmez A., Gamsizkan Z., Ozdemir S., Kesikbas E., Gokosmanoglu F., Torun S. The effect of COVID-19 lockdown on glycemic control in patients with type 2 diabetes mellitus in Turkey. Diabetes Metab Syndr. 2020 Nov-Dec;14(6):1963–1966. doi: 10.1016/j.dsx.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gianchandani R., Esfandiari N.H., Ang L., Iyengar J., Knotts S., Choksi P. Managing hyperglycemia in the COVID-19 inflammatory storm. Diabetes. 2020 Oct;69(10):2048–2053. doi: 10.2337/dbi20-0022. [DOI] [PubMed] [Google Scholar]
- 17.Ghosh A., Arora B., Gupta R., Anoop S., Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab Syndr. 2020 Sep - Oct;14(5):917–920. doi: 10.1016/j.dsx.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pellegrini M., Ponzo V., Rosato R., Scumaci E., Goitre I., Benso A. Changes in weight and nutritional habits in adults with obesity during the "lockdown" period caused by the COVID-19 virus emergency. Nutrients. 2020 Jul 7;12(7) doi: 10.3390/nu12072016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rabbone I., Schiaffini R., Cherubini V., Maffeis C., Scaramuzza A. Has COVID-19 delayed the diagnosis and worsened the presentation of type 1 diabetes in children? Diabetes Care. 2020;43(11):2870–2872. doi: 10.2337/dc20-1321. [DOI] [PubMed] [Google Scholar]
- 20.Lawrence C., Seckold R., Smart C., King B.R., Howley P., Feltrin R. Increased paediatric presentations of severe diabetic ketoacidosis in an Australian tertiary centre during the COVID-19 pandemic. Diabet Med. 2021 Jan;38(1) doi: 10.1111/dme.14417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Armeni E., Aziz U., Qamar S., Nasir S., Nethaji C., Negus R. Protracted ketonaemia in hyperglycaemic emergencies in COVID-19: a retrospective case series. Lancet Diabetes Endocrinol. 2020 Aug;8(8):660–663. doi: 10.1016/S2213-8587(20)30221-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li J., Wang X., Chen J., Zuo X., Zhang H., Deng A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes Metab. 2020 Oct;22(10):1935–1941. doi: 10.1111/dom.14057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reddy P.K., Kuchay M.S., Mehta Y., Mishra S.K. Diabetic ketoacidosis precipitated by COVID-19: a report of two cases and review of literature. Diabetes Metab Syndr. 2020 Sep - Oct;14(5):1459–1462. doi: 10.1016/j.dsx.2020.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuchay M.S., Reddy P.K., Gagneja S., Mathew A., Mishra S.K. Short term follow-up of patients presenting with acute onset diabetes and diabetic ketoacidosis during an episode of COVID-19. Diabetes Metab Syndr. 2020 Oct 21;14(6):2039–2041. doi: 10.1016/j.dsx.2020.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghosh A., Misra A. Marked hyperglycemia and ketosis in a non-obese patient with new onset diabetes and very mild COVID-19 symptoms: a case report. Diabetes Metab Syndr. 2020 Dec 25;15(1):213–214. doi: 10.1016/j.dsx.2020.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suwanwongse K., Shabarek N. Newly diagnosed diabetes mellitus, DKA, and COVID-19: causality or coincidence? A report of three cases. J Med Virol. 2020 Jul 24;93(2):1150–1153. doi: 10.1002/jmv.26339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Croft A., Bucca A., Jansen J.H., Motzkus C., Herbert A., Wang A. First-time diabetic ketoacidosis in type 2 diabetics with Covid-19 infection: a novel case series. J Emerg Med. 2020 Nov;59(5):e193–e197. doi: 10.1016/j.jemermed.2020.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Unsworth R., Wallace S., Oliver N.S., Yeung S., Kshirsagar A., Naidu H. New-onset type 1 diabetes in children during COVID-19: multicenter regional findings in the U.K. Diabetes Care. 2020 Nov;43(11):e170–e171. doi: 10.2337/dc20-1551. [DOI] [PubMed] [Google Scholar]
- 29.Naguib M.N., Raymond J.K., Vidmar A.P. New onset diabetes with diabetic ketoacidosis in a child with multisystem inflammatory syndrome due to COVID-19. J Pediatr Endocrinol Metab. 2020 Nov 12;34(1) doi: 10.1515/jpem-2020-0426. [DOI] [PubMed] [Google Scholar]
- 30.Wang F., Wang H., Fan J., Zhang Y., Zhao Q. Pancreatic injury patterns in patients with Coronavirus disease 19 pneumonia. Gastroenterology. 2020 Jul;159(1):367–370. doi: 10.1053/j.gastro.2020.03.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ghosh A., Gupta V., Misra A. COVID19 induced acute pancreatitis and pancreatic necrosis in a patient with type 2 diabetes. Diabetes Metab Syndr. 2020 Oct 10;14(6):2097–2098. doi: 10.1016/j.dsx.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghesquiere L., Garabedian C., Drumez E., Lemaitre M., Cazaubiel M., Bengler C. Effects of COVID-19 pandemic lockdown on gestational diabetes mellitus: a retrospective study. Diabetes Metab. 2020 Oct 15 doi: 10.1016/j.diabet.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jafari M., Pormohammad A., Sheikh Neshin S.A., Ghorbani S., Bose D., Alimohammadi S. Clinical characteristics and outcomes of pregnant women with COVID-19 and comparison with control patients: a systematic review and meta-analysis. Rev Med Virol. 2021 Jan 2 doi: 10.1002/rmv.2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smati S., Mahot P., Bourdiol A., Ploteau S., Hadjadj S., Cariou B. Euglycaemic ketoacidosis during gestational diabetes with concomitant COVID-19 infection. Diabetes Metab. 2020 Jul 29 doi: 10.1016/j.diabet.2020.07.008. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]